Cumulative Risk and Externalizing Behaviors during Infancy in a Predominantly Latine Sample
Abstract
1. Introduction
1.1. Parent–Child Interaction Therapy
1.2. Dropout and Differential Responses to PCIT
1.3. Individual Risk Factors of Intervention Response
1.4. Cumulative Risk and Intervention Outcomes
1.5. Current Study
2. Materials and Methods
2.1. Procedures
2.2. Participants
2.3. Risk Measures
2.4. Outcome Measures
2.5. Statistical Plan
3. Results
3.1. Descriptive Analyses
3.2. Cumulative Risk and Child Externalizing Behaviors
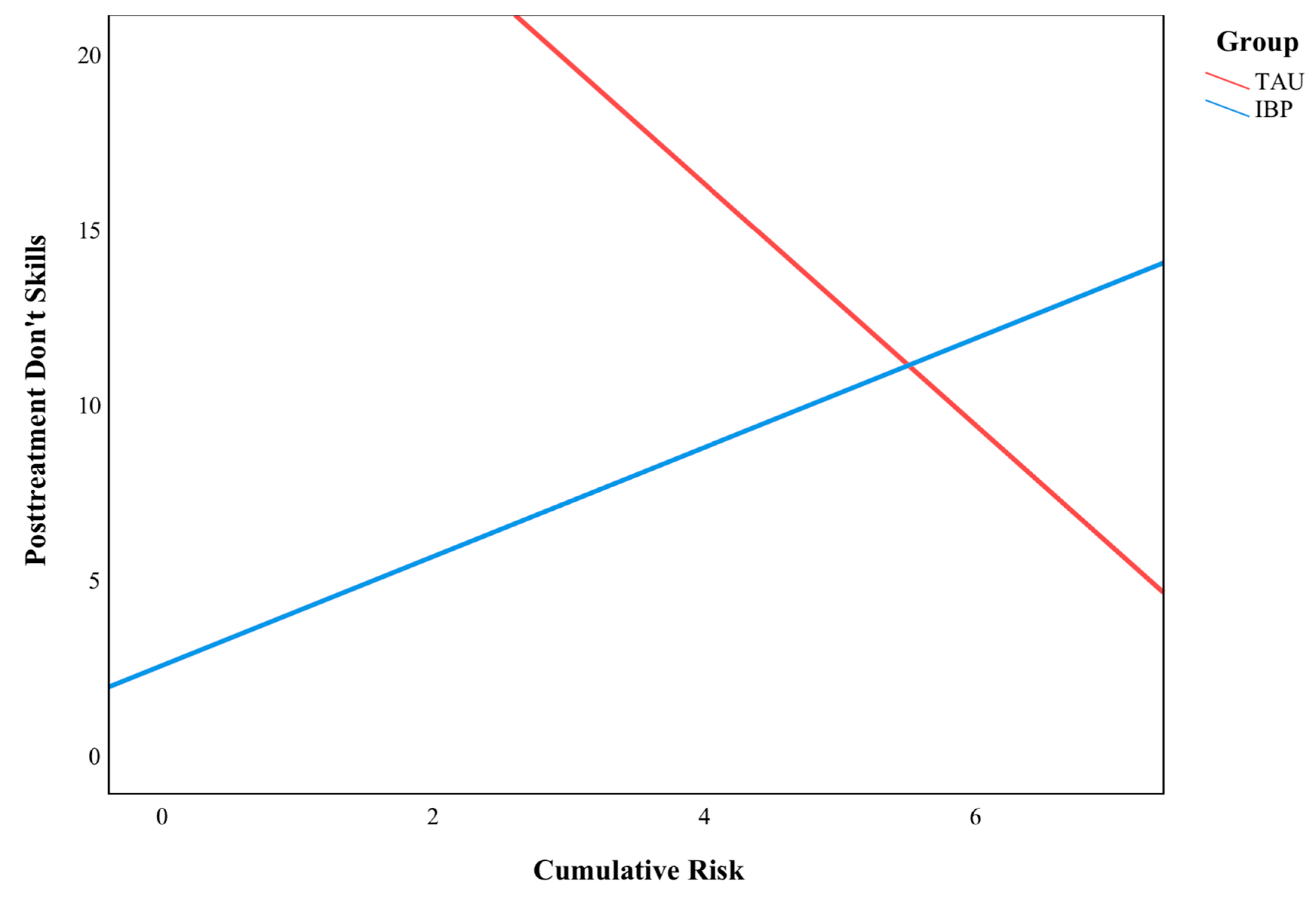
3.3. Cumulative Risk and Parenting Skills
3.4. Cumulative Risk and Dropout
4. Discussion
4.1. Child Externalizing Behaviors
4.2. Parenting Skills
4.3. Dropout
4.4. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Risk Score | Externalizing | Do Skills | Don’t Skills | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TAU | IBP | TAU | IBP | TAU | IBP | |||||||||||||
| n | M | SD | n | M | SD | n | M | SD | n | M | SD | n | M | SD | n | M | SD | |
| 1 | 0 | . | . | 1 | 0.64 | . | 0 | . | . | 1 | 27.00 | . | 0 | . | . | 1 | 9.00 | . |
| 2 | 1 | 0.77 | . | 0 | . | . | 2 | 5 | 3.54 | 0 | . | . | 2 | 30.50 | 22.63 | 0 | . | |
| 3 | 6 | 0.68 | 0.32 | 3 | 0.79 | 0.48 | 4 | 1.38 | 1.55 | 2 | 15.25 | 3.89 | 4 | 11.00 | 8.53 | 2 | 2.25 | 0.35 |
| 4 | 5 | 0.67 | 0.16 | 9 | 0.69 | 0.28 | 3 | 2.50 | 2.29 | 8 | 8.00 | 6.88 | 3 | 18.50 | 13.81 | 8 | 15.56 | 14.73 |
| 5 | 10 | 1.16 | 0.33 | 4 | 0.66 | 0.24 | 9 | 3.83 | 6.71 | 6 | 14.42 | 15.09 | 9 | 9.83 | 12.00 | 6 | 9.33 | 9.15 |
| 6 | 9 | 1.02 | 0.34 | 0 | . | . | 9 | 10.11 | 10.84 | 1 | 1.50 | . | 9 | 9.56 | 10.39 | 1 | 8.00 | . |
References
- Loeber, R.; Green, S.M.; Lahey, B.B.; Frick, P.J.; McBurnett, K. Findings on Disruptive Behavior Disorders from the First Decade of the Developmental Trends Study. Clin. Child Fam. Psychol. Rev. 2000, 3, 37–60. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Kazdin, A.E.; Hiripi, E.; Kessler, R.C. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National Comorbidity Survey Replication. Psychol. Med. 2006, 36, 699–710. [Google Scholar] [CrossRef] [PubMed]
- Erskine, H.E.; Norman, R.E.; Ferrari, A.J.; Chan GC, K.; Copeland, W.E.; Whiteford, H.A.; Scott, J.G. Long-Term Outcomes of Attention-Deficit/Hyperactivity Disorder and Conduct Disorder: A Systematic Review and Meta-Analysis. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 841–850. [Google Scholar] [CrossRef]
- Patel, R.S.; Amaravadi, N.; Bhullar, H.; Lekireddy, J.; Win, H. Understanding the Demographic Predictors and Associated Comorbidities in Children Hospitalized with Conduct Disorder. Syst. Res. Behav. Sci. 2018, 8, 80. [Google Scholar] [CrossRef]
- Bakermans-Kranenburg, M.J.; van IJzendoorn, M.H.; Juffer, F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychol. Bull. 2003, 129, 195–215. [Google Scholar] [CrossRef]
- Briggs-gowan, M.J.; Carter, A.S.; Bosson-heenan, J.; Guyer, A.E.; Horwitz, S.M. Are Infant-Toddler Social-Emotional and Behavioral Problems Transient? J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 849–858. [Google Scholar] [CrossRef] [PubMed]
- Eyberg, S.M.; Nelson, M.M.; Boggs, S.R. Evidence-Based Psychosocial Treatments for Children and Adolescents with Disruptive Behavior. J. Clin. Child Adolesc. Psychol. 2008, 37, 215–237. [Google Scholar] [CrossRef]
- Tully, L.A.; Hunt, C. Brief Parenting Interventions for Children at Risk of Externalizing Behavior Problems: A Systematic Review. J. Child Fam. Stud. 2016, 25, 705–719. [Google Scholar] [CrossRef]
- Mitchell, A.E.; Morawska, A.; Mihelic, M. A systematic review of parenting interventions for child chronic health conditions. J. Child Health Care 2020, 24, 603–628. [Google Scholar] [CrossRef]
- Prinz, R.J.; Miller, G.E. Family-Based Treatment for Childhood Antisocial Behavior: Experimental Influences on Dropout and Engagement. J. Consult. Clin. Psychol. 1994, 62, 645–650. [Google Scholar] [CrossRef]
- Bagner, D.M.; Graziano, P.A. Barriers to Success in Parent Training for Young Children with Developmental Delay the Role of Cumulative Risk. Behav. Modif. 2013, 37, 356–377. [Google Scholar] [CrossRef]
- Lieneman, C.C.; Quetsch, L.B.; Theodorou, L.L.; Newton, K.A.; McNeil, C.B. Reconceptualizing attrition in Parent-Child Interaction Therapy: “Dropouts” demonstrate impressive improvements. Psychol. Res. Behav. Manag. 2019, 12, 543–555. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.; Eyberg, S.M. Predicting Treatment and Follow-Up Attrition in Parent–Child Interaction Therapy. J. Abnorm. Child Psychol. 2009, 37, 431–441. [Google Scholar] [CrossRef] [PubMed]
- McCabe, K.M.; Yeh, M. Parent–Child Interaction Therapy for Mexican Americans: A Randomized Clinical Trial. J. Clin. Child Adolesc. Psychol. 2009, 38, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Ramos, G.; Giovanni Ramos Giovanni Ramos Blizzard, A.M.; Barroso, N.E.; Bagner, D.M. Parent Training and Skill Acquisition and Utilization among Spanish- and English-Speaking Latino Families. J. Child Fam. Stud. 2018, 27, 268–279. [Google Scholar] [CrossRef]
- Heymann, P.; Heflin, B.H.; Bagner, D.M. Effect of Therapist Coaching Statements on Parenting Skills in a Brief Parenting Intervention for Infants. Behav. Modif. 2021, 46, 691–705. [Google Scholar] [CrossRef]
- Green Rosas, Y.; McCabe, K.M.; Zerr, A.; Yeh, M.; Gese, K.; Barnett, M.L. Examining English- and Spanish-Speaking Therapist Behaviors in Parent–Child Interaction Therapy. Int. J. Environ. Res. Public Health 2022, 19, 4474. [Google Scholar] [CrossRef]
- Danko, C.M.; Garbacz, L.L.; Budd, K.S. Outcomes of Parent–Child Interaction Therapy in an urban community clinic: A comparison of treatment completers and dropouts. Child. Youth Serv. Rev. 2016, 60, 42–51. [Google Scholar] [CrossRef]
- Fernandez, M.; Butler, A.M.; Eyberg, S.M. Treatment Outcome for Low Socioeconomic Status African American Families in Parent-Child Interaction Therapy: A Pilot Study. Child Fam. Behav. Ther. 2011, 33, 32–48. [Google Scholar] [CrossRef]
- Bagner, D.M.; Coxe, S.; Hungerford, G.M.; Garcia, D.; Barroso, N.E.; Hernandez, J.; Rosa-Olivares, J. Behavioral Parent Training in Infancy: A Window of Opportunity for High-Risk Families. J. Abnorm. Child Psychol. 2016, 44, 901–912. [Google Scholar] [CrossRef]
- Lavigne, J.V.; LeBailly, S.A.; Gouze, K.R.; Binns, H.J.; Keller, J.; Pate, L. Predictors and Correlates of Completing Behavioral Parent Training for the Treatment of Oppositional Defiant Disorder in Pediatric Primary Care. Behav. Ther. 2010, 41, 198–211. [Google Scholar] [CrossRef] [PubMed]
- Webster-Stratton, C. Predictors of treatment outcome in parent training for conduct disordered children. Behav. Ther. 1985, 16, 223–243. [Google Scholar] [CrossRef]
- Webster-Stratton, C.; Hammond, M.A. Predictors of treatment outcome in parent training for families with conduct problem children. Behav. Ther. 1990, 21, 319–337. [Google Scholar] [CrossRef]
- Barroso, N.E.; Mendez, L.; Graziano, P.A.; Bagner, D.M. Parenting Stress through the Lens of Different Clinical Groups: A Systematic Review & Meta-Analysis. J. Abnorm. Child Psychol. 2018, 46, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.H.; Call, T.A.; Wolford, S.N.; McWey, L.M. Parental Stress and Child Outcomes: The Mediating Role of Family Conflict. J. Child Fam. Stud. 2021, 30, 746–756. [Google Scholar] [CrossRef]
- Caravita, S.C.S.; Miragoli, S.; Balzarotti, S.; Camisasca, E.; Di Blasio, P. Parents’ perception of child behavior, parenting stress, and child abuse potential: Individual and partner influences. Child Abus. Negl. 2018, 84, 146–156. [Google Scholar] [CrossRef]
- Feisthamel, K.P.; Schwartz, R.C. Differences in Mental Health Counselors’ Diagnoses Based on Client Race: An Investigation of Adjustment, Childhood, and Substance-Related Disorders. J. Ment. Health Couns. 2009, 31, 47–59. [Google Scholar] [CrossRef]
- Schwartz, R.C.; Blankenship, D.M. Racial disparities in psychotic disorder diagnosis: A review of empirical literature. World J. Psychiatry 2014, 4, 133–140. [Google Scholar] [CrossRef]
- Shifrer, D. Clarifying the Social Roots of the Disproportionate Classification of Racial Minorities and Males with Learning Disabilities. Sociol. Q. 2018, 59, 384–406. [Google Scholar] [CrossRef]
- U.S. Census Bureau. Real Median Household Income by Race and Hispanic Origin: 1967 to 2020; U.S. Census Bureau: Suitland, MD, USA, 2021. Available online: https://www.census.gov/content/dam/Census/library/visualizations/2021/demo/p60-273/figure2.pdf (accessed on 4 February 2023).
- Timmins, C.L. The impact of language barriers on the health care of Latinos in the United States: A review of the literature and guidelines for practice. J. Midwifery Women’s Health 2002, 47, 80–96. [Google Scholar] [CrossRef]
- Gardner, F.; Connell, A.M.; Trentacosta, C.J.; Shaw, D.S.; Dishion, T.J.; Wilson, M.N. Moderators of outcome in a brief family-centered intervention for preventing early problem behavior. J. Consult. Clin. Psychol. 2009, 77, 543–553. [Google Scholar] [CrossRef]
- Ackerman, B.P.; Brown, E.D.; Izard, C.E. The Relations between Contextual Risk, Earned Income, and the School Adjustment of Children from Economically Disadvantaged Families. Dev. Psychol. 2004, 40, 204–216. [Google Scholar] [CrossRef]
- Shaw, D.S.; Winslow, E.B.; Owens, E.B.; Hood, N. Young children’s adjustment to chronic family adversity: A longitudinal study of low-income families. J. Am. Acad. Child Adolesc. Psychiatry 1998, 37, 545–553. [Google Scholar] [CrossRef]
- Carter, A.S.; Briggs-Gowan, M.J. ITSEA/BITSEA: Infant Toddler and Brief Infant Toddler Social and Emotional Assessment Examiner’s Manual; Harcourt Assessment: San Antonio, TX, USA, 2006. [Google Scholar]
- Pons, J.I.; Flores-Pabón, L.; Matías-Carrelo, L.; Rodríguez, M.; Rosario-Hernández, E.; Rodríguez, J.M.; Herrans, L.L.; Yang, J. Confiabilidad de la Escala de Inteligencia Wechsler para Adultos Versión III, Puerto Rico (EIWA-III). Rev. Puertorriqueña Psicol. 2008, 19, 112–132. [Google Scholar]
- Wechsler, D. Wechsler Abbreviated Scale of Intelligence; Pearson: London, UK, 1999. [Google Scholar]
- Miami-Dade County. 2022 HHS Federal Poverty Guidelines. 2022. Available online: https://www.miamidade.gov/grants/library/ryanwhite/federal-poverty-guidelines.pdf (accessed on 4 February 2023).
- Abidin, R.R. Parenting Stress Index (PSI); Pediatric Psychology Press: Atlanta, GA, USA, 1990. [Google Scholar]
- Sarsour, K.; Sheridan, M.A.; Jutte, D.P.; Nuru-Jeter, A.; Hinshaw, S.P.; Boyce, W.T. Family socioeconomic status and child executive functions: The roles of language, home environment, and single parenthood. J. Int. Neuropsychol. Soc. 2011, 17, 120–132. [Google Scholar] [CrossRef]
- Eyberg, S.M.; Nelson, M.M.; Duke, M.; Boggs, S.R. Manual for the Dyadic Parent-Child Interaction Coding System, 3rd ed.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2004. [Google Scholar]
- Matos, M.; Torres, R.; Santiago, R.; Jurado, M.; Rodríguez, I. Adaptation of parent-child interaction therapy for Puerto Rican families: A preliminary study. Fam. Process 2006, 45, 205–222. [Google Scholar] [CrossRef]
- Parra Cardona, J.; Holtrop, K.; Córdova, J.D.; Escobar-Chew, A.R.; Horsford, S.; Tams, L.; Villarruel, F.A.; Villalobos, G.; Dates, B.; Anthony, J.C.; et al. “Queremos aprender”: Latino immigrants’ call to integrate cultural adaption with best practice knowledge in a parenting intervention. Fam. Process 2009, 48, 211–231. [Google Scholar] [CrossRef]
- Callahan, C.L.; Eyberg, S.M. Relations between Parenting Behavior and SES in a Clinical Sample: Validity of SES Measures. Child Fam. Behav. Ther. 2010, 32, 125–138. [Google Scholar] [CrossRef]
- Sultana, N.; Wong Lena, L.; Purdy Samanta, C. Natural Language Input: Maternal Education, Socioeconomic Deprivation, and Language Outcomes in Typically Developing Children. Lang. Speech Hear. Serv. Sch. 2020, 51, 1049–1070. [Google Scholar] [CrossRef]
- Bagner, D.M.; Berkovits, M.D.; Coxe, S.; Frech, N.; Garcia, D.; Golik, A.; Heflin, B.H.; Heymann, P.; Javadi, N.; Sanchez, A.L.; et al. Telehealth Treatment of Behavior Problems in Young Children with Developmental Delay: A Randomized Clinical Trial. JAMA Pediatr. 2023, 177, 231–239. [Google Scholar] [CrossRef]
- Gurwitch, R.H.; Salem, H.; Nelson, M.M.; Comer, J.S. Leveraging parent-child interaction therapy and telehealth capacities to address the unique needs of young children during the COVID-19 public health crisis. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S82–S84. [Google Scholar] [CrossRef] [PubMed]

| Measures | % Risk Factor |
|---|---|
| SES | 87.9 |
| Maternal Education | 69.0 |
| Maternal Intelligence | 82.8 |
| Marital Status | 31.0 |
| Parenting Stress | 50.0 |
| Child Ethnicity | 94.8 |
| Child Race | 17.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rowe, G.M.; Bagner, D.M.; Lorenzo, N.E. Cumulative Risk and Externalizing Behaviors during Infancy in a Predominantly Latine Sample. Behav. Sci. 2023, 13, 363. https://doi.org/10.3390/bs13050363
Rowe GM, Bagner DM, Lorenzo NE. Cumulative Risk and Externalizing Behaviors during Infancy in a Predominantly Latine Sample. Behavioral Sciences. 2023; 13(5):363. https://doi.org/10.3390/bs13050363
Chicago/Turabian StyleRowe, Greighson M., Daniel M. Bagner, and Nicole E. Lorenzo. 2023. "Cumulative Risk and Externalizing Behaviors during Infancy in a Predominantly Latine Sample" Behavioral Sciences 13, no. 5: 363. https://doi.org/10.3390/bs13050363
APA StyleRowe, G. M., Bagner, D. M., & Lorenzo, N. E. (2023). Cumulative Risk and Externalizing Behaviors during Infancy in a Predominantly Latine Sample. Behavioral Sciences, 13(5), 363. https://doi.org/10.3390/bs13050363





