Social Network Characteristics and Depressive Symptoms of Italian Public Health Medical Residents: The Public Health Residents’ Anonymous Survey in Italy (PHRASI)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Social Network Characteristics
2.3. Assessment of Depressive Symptoms
2.4. Covariates
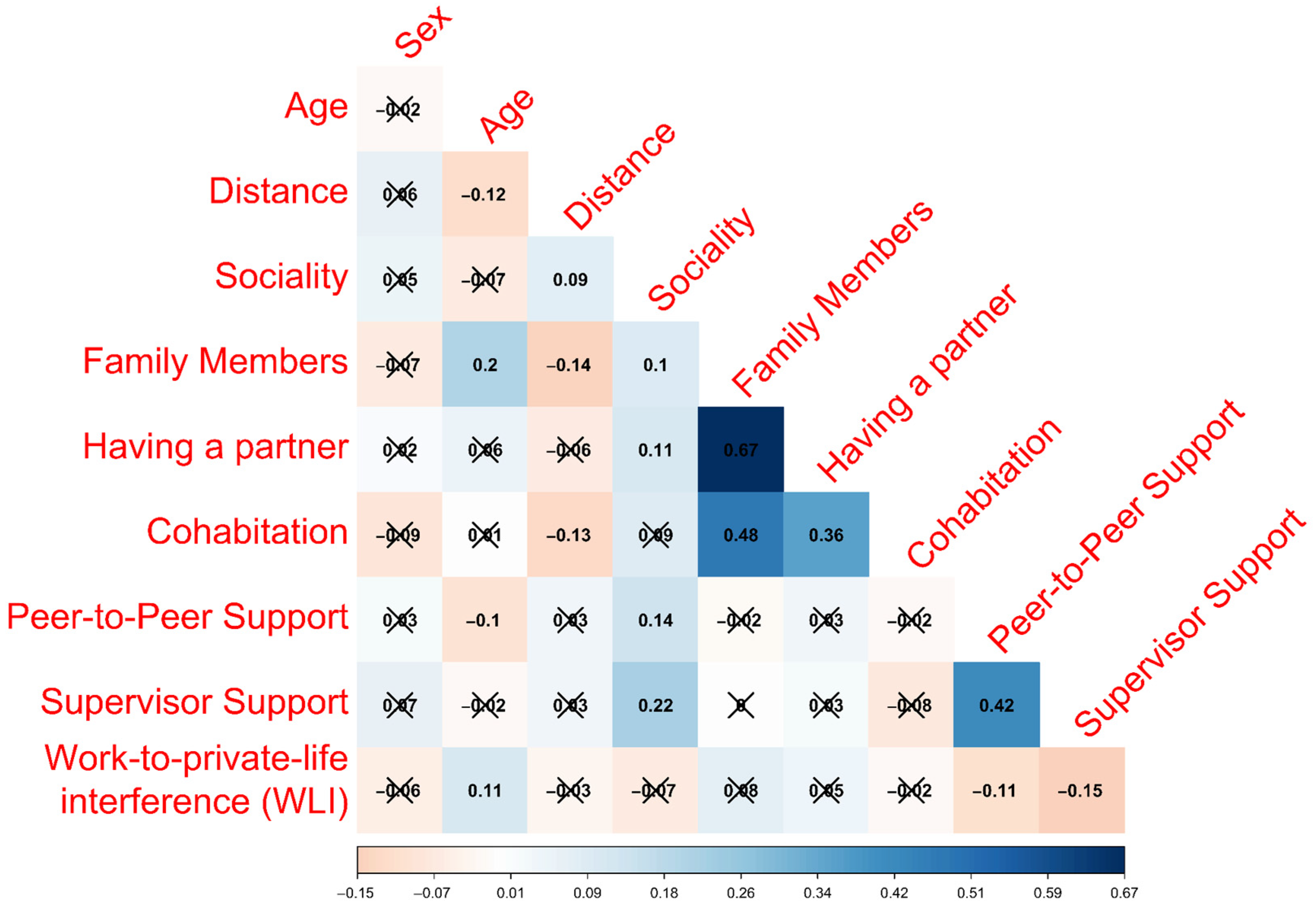
2.5. Statistical Analysis
2.6. Ethical Approval
3. Results
3.1. Descriptive Characteristics of the Sample
3.2. Social Network Characteristics and Depressive Symptoms
3.3. Social Network Characteristics and Clinically Relevant Depressive Symptoms
4. Discussion
4.1. Implication and Practices for Public Health Policies
4.2. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2019 Diseases and Injuries Collaborators. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Mental Disorders. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 30 March 2023).
- Vos, T.; Barber, R.M.; Bell, B.; Bertozzi-Villa, A.; Biryukov, S.; Bolliger, I.; Charlson, F.; Davis, A.; Degenhardt, L.; Dicker, D.; et al. Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 301 Acute and Chronic Diseases and Injuries in 188 Countries, 1990–2013: A Systematic Analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar] [CrossRef] [PubMed]
- Cuijpers, P.; Vogelzangs, N.; Twisk, J.; Kleiboer, A.; Li, J.; Penninx, B.W. Comprehensive Meta-Analysis of Excess Mortality in Depression in the General Community Versus Patients With Specific Illnesses. Am. J. Psychiatry 2014, 171, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Laursen, T.M.; Musliner, K.L.; Benros, M.E.; Vestergaard, M.; Munk-Olsen, T. Mortality and Life Expectancy in Persons with Severe Unipolar Depression. J. Affect. Disord. 2016, 193, 203–207. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). The Global Burden of Disease: 2004 Update. Available online: http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/ (accessed on 30 March 2023).
- GBD 2019 Mental Disorders Collaborators. Global, Regional, and National Burden of 12 Mental Disorders in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Engel, G.L. The Need for a New Medical Model: A Challenge for Biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef]
- Taquet, M.; Holmes, E.A.; Harrison, P.J. Depression and Anxiety Disorders during the COVID-19 Pandemic: Knowns and Unknowns. Lancet 2021, 398, 1665–1666. [Google Scholar] [CrossRef]
- Gianfredi, V.; Provenzano, S.; Santangelo, O.E. What Can Internet Users’ Behaviours Reveal about the Mental Health Impacts of the COVID-19 Pandemic? A Systematic Review. Public Health 2021, 198, 44–52. [Google Scholar] [CrossRef]
- Wiwatkunupakarn, N.; Pateekhum, C.; Aramrat, C.; Jirapornchaoren, W.; Pinyopornpanish, K.; Angkurawaranon, C. Social Networking Site Usage: A Systematic Review of Its Relationship with Social Isolation, Loneliness, and Depression among Older Adults. Aging Ment. Health 2022, 26, 1318–1326. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Simpson, S.G. Psychological Consequences of Social Isolation during COVID-19 Outbreak. Front. Psychol. 2020, 11, 2201. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Berkman, L.F. Social Ties and Mental Health. J. Urban Health 2001, 78, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Jose, P.E.; Lim, B.T.L. Social Connectedness Predicts Lower Loneliness and Depressive Symptoms over Time in Adolescents. Open J. Depress. 2014, 3, 49192. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hawkley, L.C.; Norman, G.J.; Berntson, G.G. Social Isolation: Social Isolation. Ann. N. Y. Acad. Sci. 2011, 1231, 17–22. [Google Scholar] [CrossRef]
- Chao, S.F. Assessing Social Support and Depressive Symptoms in Older Chinese Adults: A Longitudinal Perspective. Aging Ment. Health 2011, 15, 765–774. [Google Scholar] [CrossRef]
- Levula, A.; Harré, M.; Wilson, A. The Association Between Social Network Factors with Depression and Anxiety at Different Life Stages. Community Ment. Health J. 2018, 54, 842–854. [Google Scholar] [CrossRef]
- Borgatti, S.P.; Mehra, A.; Brass, D.J.; Labianca, G. Network Analysis in the Social Sciences. Science 2009, 323, 892–895. [Google Scholar] [CrossRef]
- Schmälzle, R.; Brook O’Donnell, M.; Garcia, J.O.; Cascio, C.N.; Bayer, J.; Bassett, D.S.; Vettel, J.M.; Falk, E.B. Brain Connectivity Dynamics during Social Interaction Reflect Social Network Structure. Proc. Natl. Acad. Sci. USA 2017, 114, 5153–5158. [Google Scholar] [CrossRef]
- Rosenquist, J.N.; Fowler, J.H.; Christakis, N.A. Social Network Determinants of Depression. Mol. Psychiatry 2011, 16, 273–281. [Google Scholar] [CrossRef]
- Elmer, T.; Stadtfeld, C. Depressive Symptoms Are Associated with Social Isolation in Face-to-Face Interaction Networks. Sci. Rep. 2020, 10, 1444. [Google Scholar] [CrossRef]
- Ojagbemi, A.; Gureje, O. Typology of Social Network Structures and Late-Life Depression in Low- and Middle-Income Countries. Clin. Pract. Epidemiol. Ment. Health 2019, 15, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Lau, Y.W.; Vaingankar, J.A.; Abdin, E.; Shafie, S.; Jeyagurunathan, A.; Zhang, Y.; Magadi, H.; Ng, L.L.; Chong, S.A.; Subramaniam, M. Social Support Network Typologies and Their Association with Dementia and Depression among Older Adults in Singapore: A Cross-Sectional Analysis. BMJ Open 2019, 9, e025303. [Google Scholar] [CrossRef] [PubMed]
- Werner-Seidler, A.; Afzali, M.H.; Chapman, C.; Sunderland, M.; Slade, T. The Relationship between Social Support Networks and Depression in the 2007 National Survey of Mental Health and Well-Being. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 1463–1473. [Google Scholar] [CrossRef] [PubMed]
- van den Brink, R.H.S.; Schutter, N.; Hanssen, D.J.C.; Elzinga, B.M.; Rabeling-Keus, I.M.; Stek, M.L.; Comijs, H.C.; Penninx, B.W.J.H.; Oude Voshaar, R.C. Prognostic Significance of Social Network, Social Support and Loneliness for Course of Major Depressive Disorder in Adulthood and Old Age. Epidemiol. Psychiatr. Sci. 2018, 27, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Brummett, B.H.; Mark, D.B.; Siegler, I.C.; Williams, R.B.; Babyak, M.A.; Clapp-Channing, N.E.; Barefoot, J.C. Perceived Social Support as a Predictor of Mortality in Coronary Patients: Effects of Smoking, Sedentary Behavior, and Depressive Symptoms. Psychosom. Med. 2005, 67, 40–45. [Google Scholar] [CrossRef]
- Glanz, K.; Rimer, B.K.; Viswanath, K. (Eds.) Health Behavior: Theory, Research, and Practice, 5th ed.; Jossey-Bass Public Health; Jossey-Bass: San Francisco, CA, USA, 2015; ISBN 978-1-118-62898-0. [Google Scholar]
- Devassy, S.M.; Scaria, L.; Cheguvera, N.; Thampi, K. Association of Depression and Anxiety with Social Network Types: Results from a Community Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 6120. [Google Scholar] [CrossRef]
- Monninger, M.; Aggensteiner, P.-M.; Pollok, T.M.; Reinhard, I.; Hall, A.S.M.; Zillich, L.; Streit, F.; Witt, S.-H.; Reichert, M.; Ebner-Priemer, U.; et al. Real-Time Individual Benefit from Social Interactions before and during the Lockdown: The Crucial Role of Personality, Neurobiology and Genes. Transl. Psychiatry 2022, 12, 28. [Google Scholar] [CrossRef]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of Mental Health Problems during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef]
- Catalini, A.; Mazza, C.; Cosma, C.; Minutolo, G.; De Nicolò, V.; Gallinoro, V.; Caminiti, M.; Ancona, A.; Stacchini, L.; Berselli, N.; et al. Public Health Residents’ Anonymous Survey in Italy (PHRASI): Study Protocol for a Cross-Sectional Study for a Multidimensional Assessment of Mental Health and Its Determinants. Int. J. Environ. Res. Public Health 2023, 20, 2003. [Google Scholar] [CrossRef]
- Charan, J.; Biswas, T. How to Calculate Sample Size for Different Study Designs in Medical Research? Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef]
- Silvestri, C.; Carpita, B.; Cassioli, E.; Lazzeretti, M.; Rossi, E.; Messina, V.; Castellini, G.; Ricca, V.; Dell’Osso, L.; Bolognesi, S.; et al. Prevalence Study of Mental Disorders in an Italian Region. Preliminary Report. BMC Psychiatry 2023, 23, 12. [Google Scholar] [CrossRef] [PubMed]
- Menichini, D.; Fanetti, O.; Molinazzi, M.T. Physical Activity in Low Risk Pregnant Women: A Cross-Sectional Study. Clin. Ter. 2020, 171, e328–e334. [Google Scholar] [CrossRef] [PubMed]
- Vincenty, T. Direct and inverse solutions of geodesics on the ellipsoid with application of nested equations. Surv. Rev. 1975, 23, 88–93. [Google Scholar] [CrossRef]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Mazzotti, E.; Fassone, G.; Picardi, A.; Sagoni, E.; Ramieri, L.; Lega, I.; Camaioni, D.; Abeni, D.; Pasquini, P. Il Patient Health Questionnaire (PHQ) per Lo Screening Dei Disturbi Psichiatrici: Uno Studio Di Validazione Nei Confronti Della Intervista Clinica Strutturata per Il DSM-IV Asse I (SCID-I) (The Patient Health Questionnaire (PHQ) for the Screening of Psychiatric Disorders: A Validation Study versus the Structured Clinical Interview for DSM-IV Axis I (SCID-I)). Ital. J. Psychopatol. 2003, 9, 235–242. [Google Scholar]
- Janssen, E.P.C.J.; Köhler, S.; Stehouwer, C.D.A.; Schaper, N.C.; Dagnelie, P.C.; Sep, S.J.S.; Henry, R.M.A.; Van Der Kallen, C.J.H.; Verhey, F.R.; Schram, M.T. The Patient Health Questionnaire-9 as a Screening Tool for Depression in Individuals with Type 2 Diabetes Mellitus: The Maastricht Study. J. Am. Geriatr. Soc. 2016, 64, e201–e206. [Google Scholar] [CrossRef]
- Bush, K. The AUDIT Alcohol Consumption Questions (AUDIT-C)An Effective Brief Screening Test for Problem Drinking. Arch. Intern. Med. 1998, 158, 1789. [Google Scholar] [CrossRef]
- Campbell, C.E.; Maisto, S.A. Validity of the AUDIT-C Screen for at-Risk Drinking among Students Utilizing University Primary Care. J. Am. Coll. Health 2018, 66, 774–782. [Google Scholar] [CrossRef]
- Mannocci, A.; Masala, D.; Mei, D.; Tribuzio, A.M.; Villari, P.; LA Torre, G. International Physical Activity Questionnaire for Adolescents (IPAQ A): Reliability of an Italian Version. Minerva Pediatr (Torino). Minerva Pediatr. 2021, 73, 383–390. [Google Scholar] [CrossRef]
- Schaeffer, M.S.; Levitt, E.E. Concerning Kendall’s Tau, a Nonparametric Correlation Coefficient. Psychol. Bull. 1956, 53, 338–346. [Google Scholar] [CrossRef]
- European Union. Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC (General Data Protection Regulation). Eur-Lex. Access to European Unione Law. 2016. Available online: https://eur-lex.europa.eu/eli/reg/2016/679/oj (accessed on 5 September 2023).
- Italia. Decreto Legislativo 10 Agosto 2018, n. 101. Disposizioni per L’adeguamento Della Normativa Nazionale Alle Disposizioni del Regolamento (UE) 2016/679 del Parlamento Europeo e del Consiglio, del 27 Aprile 2016, Relativo Alla Protezione Delle Persone Fisiche Con Riguardo al Trattamento dei Dati Personali, Nonché alla Libera Circolazione di Tali Dati e Che Abroga la Direttiva 95/46/CE (Regolamento Generale Sulla Protezione Dei Dati). Gazzetta Ufficiale Della Repubblica Italiana Serie Generale n. 159 del 4 September 2018. Available online: https://www.gazzettaufficiale.it/eli/id/2018/09/04/18G00129/sg (accessed on 5 September 2023).
- Italia. Decreto Legislativo 30 Giugno 2003, n. 196. Codice in Materia di Protezione dei Dati Personali. In Ministero della Giustizia—Ufficio Pubblicazioni Leggi e Decreti, Editor. Supplemento Ordinario alla “Gazzetta Ufficiale della Repubblica Italiana”; Serie Generale; Istituto Poligrafico e Zecca Dello Stato: Roma, Italy, 2003; Volume 123/L, pp. 11–207. Available online: https://www.gazzettaufficiale.it/eli/gu/2003/07/29/174/so/123/sg/pdf (accessed on 5 September 2023).
- Thoits, P.A. Mechanisms Linking Social Ties and Support to Physical and Mental Health. J. Health Soc. Behav. 2011, 52, 145–161. [Google Scholar] [CrossRef] [PubMed]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social Relationships and Mortality Risk: A Meta-Analytic Review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Thisted, R.A. Loneliness as a Specific Risk Factor for Depressive Symptoms: Cross-Sectional and Longitudinal Analyses. Psychol. Aging 2006, 21, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Gianfredi, V.; Beran, M.; Koster, A.; Eussen, S.J.; Odone, A.; Signorelli, C.; Schaper, N.C.; Köhler, S.; Bosma, H.; Dagnelie, P.C.; et al. Association between social network characteristics and prevalent and incident depression: The Maastricht Study. J. Affect. Disord. 2021, 293, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Gariépy, G.; Honkaniemi, H.; Quesnel-Vallée, A. Social Support and Protection from Depression: Systematic Review of Current Findings in Western Countries. Br. J. Psychiatry 2016, 209, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Simmons, M.B.; Cartner, S.; MacDonald, R.; Whitson, S.; Bailey, A.; Brown, E. The Effectiveness of Peer Support from a Person with Lived Experience of Mental Health Challenges for Young People with Anxiety and Depression: A Systematic Review. BMC Psychiatry 2023, 23, 194. [Google Scholar] [CrossRef]
- Richard, J.; Rebinsky, R.; Suresh, R.; Kubic, S.; Carter, A.; Cunningham, J.E.A.; Ker, A.; Williams, K.; Sorin, M. Scoping Review to Evaluate the Effects of Peer Support on the Mental Health of Young Adults. BMJ Open 2022, 12, e061336. [Google Scholar] [CrossRef]
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender Differences in Depression in Representative National Samples: Meta-Analyses of Diagnoses and Symptoms. Psychol. Bull. 2017, 143, 783–822. [Google Scholar] [CrossRef]
- Abraham, A.; Chaabna, K.; Doraiswamy, S.; Bhagat, S.; Sheikh, J.; Mamtani, R.; Cheema, S. Depression among Healthcare Workers in the Eastern Mediterranean Region: A Systematic Review and Meta-Analysis. Hum. Resour. Health 2021, 19, 81. [Google Scholar] [CrossRef]
- Iglesias Martínez, E.; Roces García, J.; Jiménez Arberas, E.; Llosa, J.A. Difference between Impacts of COVID-19 on Women and Men’s Psychological, Social, Vulnerable Work Situations, and Economic Well-Being. Int. J. Environ. Res. Public Health 2022, 19, 8849. [Google Scholar] [CrossRef]
- Gao, Y.-Q.; Pan, B.-C.; Sun, W.; Wu, H.; Wang, J.-N.; Wang, L. Depressive Symptoms among Chinese Nurses: Prevalence and the Associated Factors: Depressive Symptoms in Chinese Nurses. J. Adv. Nurs. 2012, 68, 1166–1175. [Google Scholar] [CrossRef] [PubMed]
- Naidoo, T.; Tomita, A.; Paruk, S. Burnout, Anxiety and Depression Risk in Medical Doctors Working in KwaZulu-Natal Province, South Africa: Evidence from a Multi-Site Study of Resource-Constrained Government Hospitals in a Generalised HIV Epidemic Setting. PLoS ONE 2020, 15, e0239753. [Google Scholar] [CrossRef] [PubMed]
- Dormann, C.; Zapf, D. Social Support, Social Stressors at Work, and Depressive Symptoms: Testing for Main and Moderating Effects with Structural Equations in a Three-Wave Longitudinal Study. J. Appl. Psychol. 1999, 84, 874–884. [Google Scholar] [CrossRef] [PubMed]
- Padkapayeva, K.; Gilbert-Ouimet, M.; Bielecky, A.; Ibrahim, S.; Mustard, C.; Brisson, C.; Smith, P. Gender/Sex Differences in the Relationship between Psychosocial Work Exposures and Work and Life Stress. Ann. Work. Expo. Health 2018, 62, 416–425. [Google Scholar] [CrossRef]
- Rugulies, R.; Bültmann, U.; Aust, B.; Burr, H. Psychosocial Work Environment and Incidence of Severe Depressive Symptoms: Prospective Findings from a 5-Year Follow-up of the Danish Work Environment Cohort Study. Am. J. Epidemiol. 2006, 163, 877–887. [Google Scholar] [CrossRef]
- Keohane, A.; Richardson, N. Negotiating Gender Norms to Support Men in Psychological Distress. Am. J. Mens. Health 2018, 12, 160–171. [Google Scholar] [CrossRef] [PubMed]
- Magnusson Hanson, L.L.M.H.; Leineweber, C.L.; Chungkham, H.S.; Westerlund, H. Work–Home Interference and Its Prospective Relation to Major Depression and Treatment with Antidepressants. Scand. J. Work Environ. Health 2014, 40, 66–73. [Google Scholar] [CrossRef]
- Wang, J.; Patten, S.B.; Currie, S.; Sareen, J.; Schmitz, N. A Population-Based Longitudinal Study on Work Environmental Factors and the Risk of Major Depressive Disorder. Am. J. Epidemiol. 2012, 176, 52–59. [Google Scholar] [CrossRef]
- Cerrato, J.; Cifre, E. Gender Inequality in Household Chores and Work-Family Conflict. Front. Psychol. 2018, 9, 1330. [Google Scholar] [CrossRef]
- Carcedo, R.J.; Fernández-Rouco, N.; Fernández-Fuertes, A.A.; Martínez-Álvarez, J.L. Association between Sexual Satisfaction and Depression and Anxiety in Adolescents and Young Adults. Int. J. Environ. Res. Public Health 2020, 17, 841. [Google Scholar] [CrossRef]
- Olson, J.S.; Crosnoe, R. Are You Still Bringing Me Down?: Romantic Involvement and Depressive Symptoms from Adolescence to Young Adulthood. J. Health Soc. Behav. 2017, 58, 102–115. [Google Scholar] [CrossRef] [PubMed]
- Vasilenko, S.A. Age-Varying Associations between Nonmarital Sexual Behavior and Depressive Symptoms across Adolescence and Young Adulthood. Dev. Psychol. 2017, 53, 366–378. [Google Scholar] [CrossRef] [PubMed]
- Gustavson, K.; Røysamb, E.; von Soest, T.; Helland, M.J.; Karevold, E.; Mathiesen, K.S. Reciprocal Longitudinal Associations between Depressive Symptoms and Romantic Partners’ Synchronized View of Relationship Quality. J. Soc. Pers. Relatsh. 2012, 29, 776–794. [Google Scholar] [CrossRef]
- Joosten, D.H.J.; Nelemans, S.A.; Meeus, W.; Branje, S. Longitudinal Associations between Depressive Symptoms and Quality of Romantic Relationships in Late Adolescence. J. Youth Adolesc. 2022, 51, 509–523. [Google Scholar] [CrossRef] [PubMed]
- Vujeva, H.M.; Furman, W. Depressive Symptoms and Romantic Relationship Qualities from Adolescence Through Emerging Adulthood: A Longitudinal Examination of Influences. J. Clin. Child Adolesc. Psychol. 2011, 40, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Ragan, J.; Randall, P. Prospective Relations Between Social Support and Depression: Differential Direction of Effects for Parent and Peer Support? J. Abnorm. Psychol. 2004, 113, 155–159. [Google Scholar] [CrossRef]
- Coyne, J.C.; Burchill, S.A.L.; Stiles, W.B. An Interactional Perspective on Depression. In Handbook of Social and Clinical Psychology: The Health Perspective; Pergamon General Psychology Series; Pergamon Press: Elmsford, NY, USA, 1991; Volume 162, pp. 327–349. ISBN 0-08-036128-5. [Google Scholar]
- Boop, C.; Cahill, S.M.; Davis, C.; Dorsey, J.; Gibbs, V.; Herr, B.; Kearney, K.; Metzger, L.; Miller, J.; Owens, A.; et al. Occupational Therapy Practice Framework: Domain and Process—Fourth Edition. Am. J. Occup. Ther. 2020, 74, 7412410010p1–7412410010p87. [Google Scholar] [CrossRef]
- Wang, J.; Mann, F.; Lloyd-Evans, B.; Ma, R.; Johnson, S. Associations between Loneliness and Perceived Social Support and Outcomes of Mental Health Problems: A Systematic Review. BMC Psychiatry 2018, 18, 156. [Google Scholar] [CrossRef]
- Weziak-Bialowolska, D.; Bialowolski, P. Bidirectional Associations between Meaning in Life and the Health, Emotional Ill-Being and Daily Life Functioning Outcomes among Older Adults. Psychol. Health 2022, 1–17. [Google Scholar] [CrossRef]
- Joules, N.; Williams, D.M.; Thompson, A.W. Depression in Resident Physicians: A Systematic Review. Open J. Depress. 2014, 3, 48621. [Google Scholar] [CrossRef]
- Cedrone, F.; Berselli, N.; Stacchini, L.; De Nicolò, V.; Caminiti, M.; Ancona, A.; Minutolo, G.; Mazza, C.; Cosma, C.; Gallinoro, V.; et al. Depressive Symptoms of Public Health Medical Residents during the COVID-19 Pandemic, a Nation-Wide Survey: The PHRASI Study. Int. J. Environ. Res. Public Health 2023, 20, 5620. [Google Scholar] [CrossRef] [PubMed]
- Lasalvia, A.; Bonetto, C.; Porru, S.; Carta, A.; Tardivo, S.; Bovo, C.; Ruggeri, M.; Amaddeo, F. Psychological Impact of COVID-19 Pandemic on Healthcare Workers in a Highly Burdened Area of North-East Italy. Epidemiol. Psychiatr. Sci. 2021, 30, e1. [Google Scholar] [CrossRef]
- Santini, Z.I.; Koyanagi, A.; Tyrovolas, S.; Mason, C.; Haro, J.M. The association between social relationships and depression: A systematic review. J. Affect. Disord. 2015, 175, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Paulhus, D.L. Measurement and Control of Response Bias. In Measures of Personality and Social Psychological Attitudes; Measures of Social Psychological Attitudes; Academic Press: San Diego, CA, USA, 1991; Volume 1, pp. 17–59. ISBN 0-12-590241-7. [Google Scholar]
- Boruch, R.F. Assuring Confidentiality of Responses in Social Research: A Note on Strategies. Am. Sociol. 1971, 6, 308–311. [Google Scholar]
- Parker, G.; Brotchie, H. Gender Differences in Depression. Int. Rev. Psychiatry 2010, 22, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Asher, M.; Asnaani, A.; Aderka, I.M. Gender Differences in Social Anxiety Disorder: A Review. Clin. Psychol. Rev. 2017, 56, 1–12. [Google Scholar] [CrossRef]
- Cedrone, F.; Catalini, A.; Stacchini, L.; Berselli, N.; Caminiti, M.; Mazza, C.; Cosma, C.; Minutolo, G.; Di Martino, G. The Role of Gender in the Association between Mental Health and Potentially Preventable Hospitalizations: A Single-Center Retrospective Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 14691. [Google Scholar] [CrossRef]
| Characteristic | Overall | PHQ-9 Score ≥ 5 | PHQ-9 Score ≥ 10 | ||||
|---|---|---|---|---|---|---|---|
| n = 379 | No (n = 148) | Yes (n = 231) | p | No (n = 282) | Yes (n = 97) | p | |
| Sex | 0.453 1 | 0.802 1 | |||||
| Female | 219 (57.78%) | 82 (55.41%) | 137 (59.31%) | 164 (58.16%) | 55 (56.70%) | ||
| Male | 160 (42.22%) | 66 (44.59%) | 94 (40.69%) | 118 (41.84%) | 42 (43.30%) | ||
| Age | 30.00 (29.00, 34.00) | 30.00 (28.00, 34.00) | 31.00 (29.00, 33.00) | 0.446 2 | 30.00 (28.00, 34.00) | 31.00 (29.00, 33.00) | 0.134 2 |
| Functional characteristics of social network | |||||||
| Peer-to-Peer Support | 4.00 (3.00, 5.00) | 4.00 (4.00, 5.00) | 4.00 (3.00, 5.00) | <0.001 2 | 4.00 (4.00, 5.00) | 4.00 (3.00, 4.00) | 0.031 2 |
| Supervisor Support | 4.00 (3.00, 4.00) | 4.00 (3.00, 5.00) | 3.00 (3.00, 4.00) | <0.001 2 | 4.00 (3.00, 4.00) | 3.00 (2.00, 4.00) | <0.001 2 |
| WLI | 3.00 (2.00, 3.00) | 2.00 (2.00, 3.00) | 3.00 (2.00, 3.00) | <0.001 2 | 2.00 (2.00, 3.00) | 3.00 (2.00, 4.00) | <0.001 2 |
| Structural characteristics of social network | |||||||
| Distance | 0.00 (0.00, 122.29.0) | 0.00 (0.00, 201.27) | 0.00 (0.00, 0.00) | 0.026 2 | 0.00 (0.00, 137.52) | 0.00 (0.00, 111.21) | 0.786 2 |
| Family Members | 2.00 (2.00, 2.00) | 2.00 (2.00, 2.00) | 2.00 (2.00, 2.00) | 0.870 2 | 2.00 (2.00, 2.00) | 2.00 (2.00, 2.00) | 0.124 2 |
| Having a partner | 0.141 1 | 0.043 1 | |||||
| Yes | 276 (72.82%) | 114 (77.03%) | 162 (70.13%) | 213 (75.53%) | 34 (35.05%) | ||
| No | 103 (27.18%) | 34 (22.97% | 69 (29.87%) | 69 (24.47%) | 63 (64.95%) | ||
| Cohabitation | 0.760 1 | 0.433 1 | |||||
| Living Alone | 98 (25.86%) | 37 (25.00%) | 61 (26.41%) | 70 (25.0%) | 28 (29.0%) | ||
| With Others | 281 (74.14%) | 111 (75.00%) | 170 (73.59%) | 212 (75.0%) | 69 (71.0%) | ||
| Social participation | 3.00 (2.00, 3.00) | 3.00 (3.00, 4.00) | 2.00 (1.00, 3.00) | <0.001 2 | 3.0 (2.0, 4.0) | 1.0 (1.0, 2.0) | <0.001 2 |
| Characteristic | aβ | 95% CI 1 | p |
|---|---|---|---|
| Functional characteristics of social network | |||
| Peer-to-peer support | −1.01 | −1.52; −0.50 | <0.001 |
| Supervisor support | −1.20 | −1.67; −0.74 | <0.001 |
| Work-to-private life interference (WLI) | 1.24 | 0.74; 1.74 | <0.001 |
| Structural characteristics of social network | |||
| Distance | 0.00 | 0.00; 0.00 | 0.636 |
| Family members | −0.81 | −1.54; −0.08 | 0.031 |
| Having a partner (ref. = No) | −1.42 | −2.58; −0.25 | 0.017 |
| Cohabitation (ref. = Alone) | −1.13 | −2.32; 0.06 | 0.062 |
| Social participation | −2.13 | −2.49; −1.76 | <0.001 |
| PHQ-9 Score ≥ 10 | PHQ-9 Score ≥ 10 Sensitivity Analysis | |||||
|---|---|---|---|---|---|---|
| Characteristic | aOR 1 | 95% CI | p | aOR 2 | 95% CI | p |
| Functional characteristics of social network | ||||||
| Peer-to-peer support | 0.72 | 0.58; 0.90 | 0.004 | 0.62 | 0.47; 0.83 | 0.001 |
| Supervisor support | 0.69 | 0.55; 0.85 | <0.001 | 0.49 | 0.36; 0.68 | <0.001 |
| Work-to-private-life interference (WLI) | 1.59 | 1.25; 2.01 | <0.001 | 1.77 | 1.28; 2.45 | <0.001 |
| Structural characteristics of social network | ||||||
| Distance | 1.00 | 1.00; 1.00 | 0.895 | 1.00 | 1.00; 1.00 | 0.816 |
| Family Members | 0.73 | 0.51; 1.03 | 0.075 | 0.73 | 0.51; 1.05 | 0.089 |
| Having a partner (ref. = No) | 0.59 | 0.36; 0.97 | 0.039 | 0.49 | 0.25; 0.96 | 0.036 |
| Cohabitation (ref. = Alone) | 0.82 | 0.49; 1.37 | 0.443 | 0.82 | 0.48; 1.40 | 0.466 |
| Social participation | 0.39 | 0.31; 0.50 | <0.001 | 0.38 | 0.29; 0.49 | <0.001 |
| Characteristic | Moderator | PHQ Score ≥ 10 | ||
|---|---|---|---|---|
| aOR 1 | 95% CI | p | ||
| Functional characteristics of social network | ||||
| Peer-to-peer support | Predictor | 0.63 | 0.48; 0.84 | 0.002 |
| Interaction | 1.42 | 0.89; 2.27 | 0.142 | |
| Supervisor support | Predictor | 0.52 | 0.38; 0.71 | <0.001 |
| Interaction | 1.77 | 1.11; 2.74 | 0.010 | |
| Work-to-private-life interference (WLI) | Predictor | 1.74 | 1.27; 2.38 | <0.001 |
| Interaction | 0.81 | 0.50; 1.30 | 0.375 | |
| Structural characteristics of social network | ||||
| Distance | Predictor | 1.00 | 1.00; 1.00 | 0.757 |
| Interaction | 1.00 | 1.00; 1.00 | 0.761 | |
| Family Members | Predictor | 0.80 | 0.55; 1.16 | 0.239 |
| Interaction | 1.02 | 0.55; 1.88 | 0.959 | |
| Having a partner (ref. = No) | Predictor | 0.47 | 0.25; 0.90 | 0.023 |
| Interaction | 1.74 | 0.63; 4.86 | 0.289 | |
| Cohabitation (ref. = Alone) | Predictor | 0.69 | 0.34; 1.40 | 0.310 |
| Interaction | 1.42 | 0.50; 4.00 | 0.513 | |
| Social participation | Predictor | 0.37 | 0.26; 0.51 | <0.001 |
| Interaction | 1.16 | 0.71; 1.90 | 0.555 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stacchini, L.; Catalini, A.; De Nicolò, V.; Cosma, C.; Gallinoro, V.; Ancona, A.; Berselli, N.; Caminiti, M.; Mazza, C.; Minutolo, G.; et al. Social Network Characteristics and Depressive Symptoms of Italian Public Health Medical Residents: The Public Health Residents’ Anonymous Survey in Italy (PHRASI). Behav. Sci. 2023, 13, 881. https://doi.org/10.3390/bs13110881
Stacchini L, Catalini A, De Nicolò V, Cosma C, Gallinoro V, Ancona A, Berselli N, Caminiti M, Mazza C, Minutolo G, et al. Social Network Characteristics and Depressive Symptoms of Italian Public Health Medical Residents: The Public Health Residents’ Anonymous Survey in Italy (PHRASI). Behavioral Sciences. 2023; 13(11):881. https://doi.org/10.3390/bs13110881
Chicago/Turabian StyleStacchini, Lorenzo, Alessandro Catalini, Valentina De Nicolò, Claudia Cosma, Veronica Gallinoro, Angela Ancona, Nausicaa Berselli, Marta Caminiti, Clara Mazza, Giuseppa Minutolo, and et al. 2023. "Social Network Characteristics and Depressive Symptoms of Italian Public Health Medical Residents: The Public Health Residents’ Anonymous Survey in Italy (PHRASI)" Behavioral Sciences 13, no. 11: 881. https://doi.org/10.3390/bs13110881
APA StyleStacchini, L., Catalini, A., De Nicolò, V., Cosma, C., Gallinoro, V., Ancona, A., Berselli, N., Caminiti, M., Mazza, C., Minutolo, G., Cedrone, F., Gianfredi, V., & on Behalf of the Working Group on Public Mental Health 2021/2022 of the Medical Residents’ Assembly of the Italian Society of Hygiene and Preventive Medicine. (2023). Social Network Characteristics and Depressive Symptoms of Italian Public Health Medical Residents: The Public Health Residents’ Anonymous Survey in Italy (PHRASI). Behavioral Sciences, 13(11), 881. https://doi.org/10.3390/bs13110881













