Sex Differences in Complex Posttraumatic Stress Disorder Network among Chinese Young Adults
Abstract
:1. Introduction
2. Methods
2.1. Participants and Procedure
2.2. Measurements
2.2.1. CPTSD
2.2.2. Childhood Trauma
2.3. Data Analysis
2.3.1. Network Estimation
2.3.2. Centrality Estimation
2.3.3. Network Stability
2.3.4. Network Comparison
2.3.5. Bayesian Network Estimation
3. Results
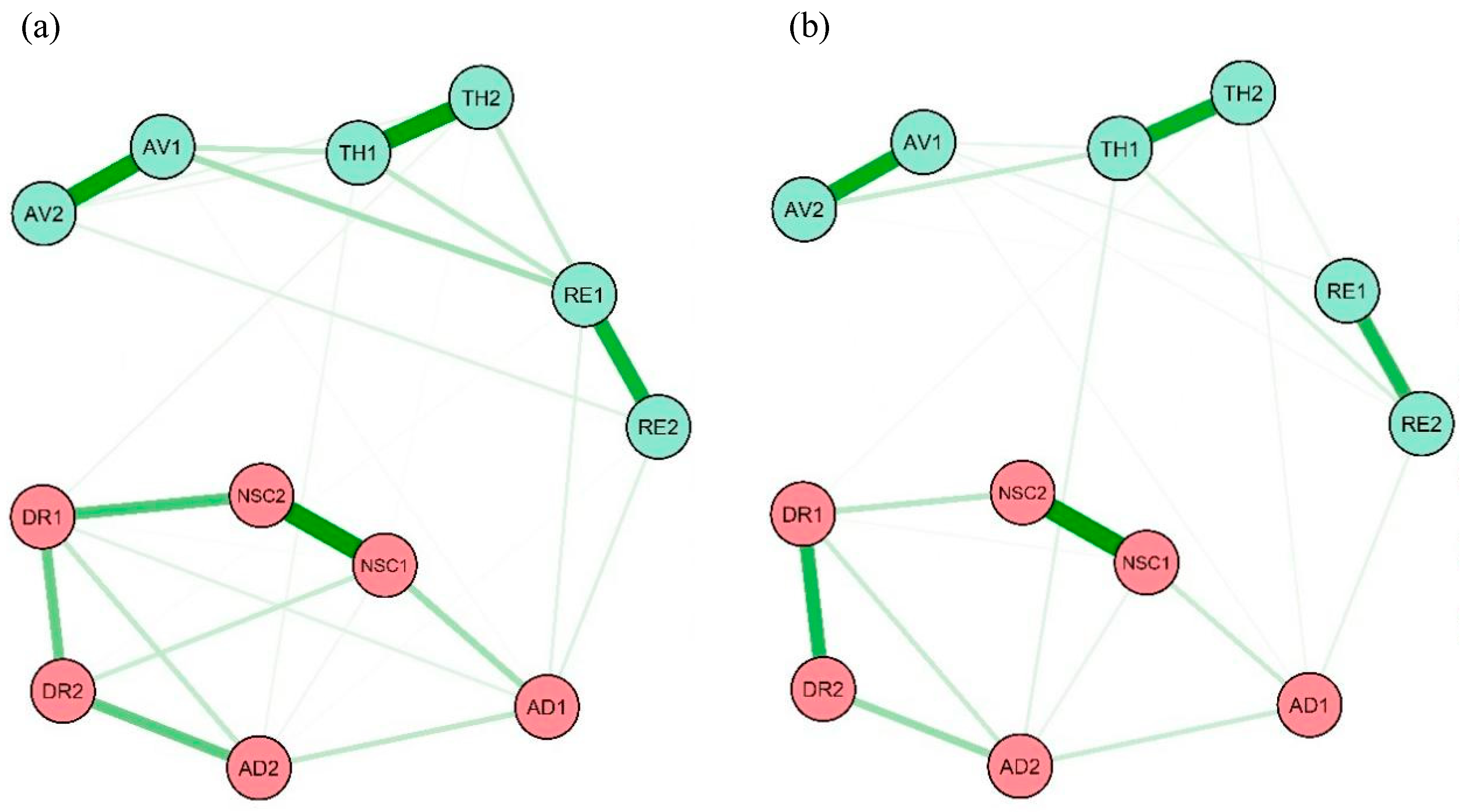
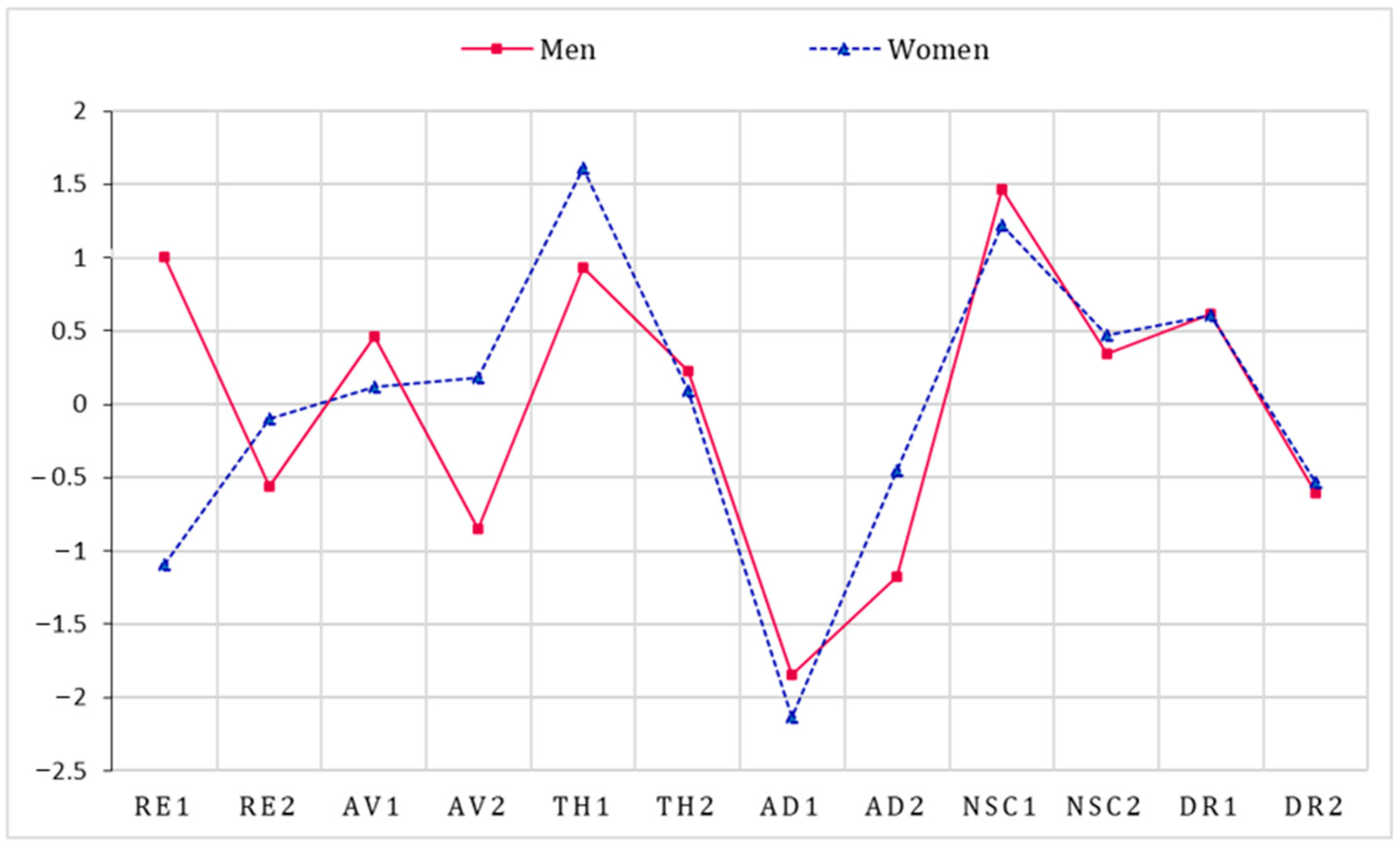
3.1. Networks and Centrality Estimation
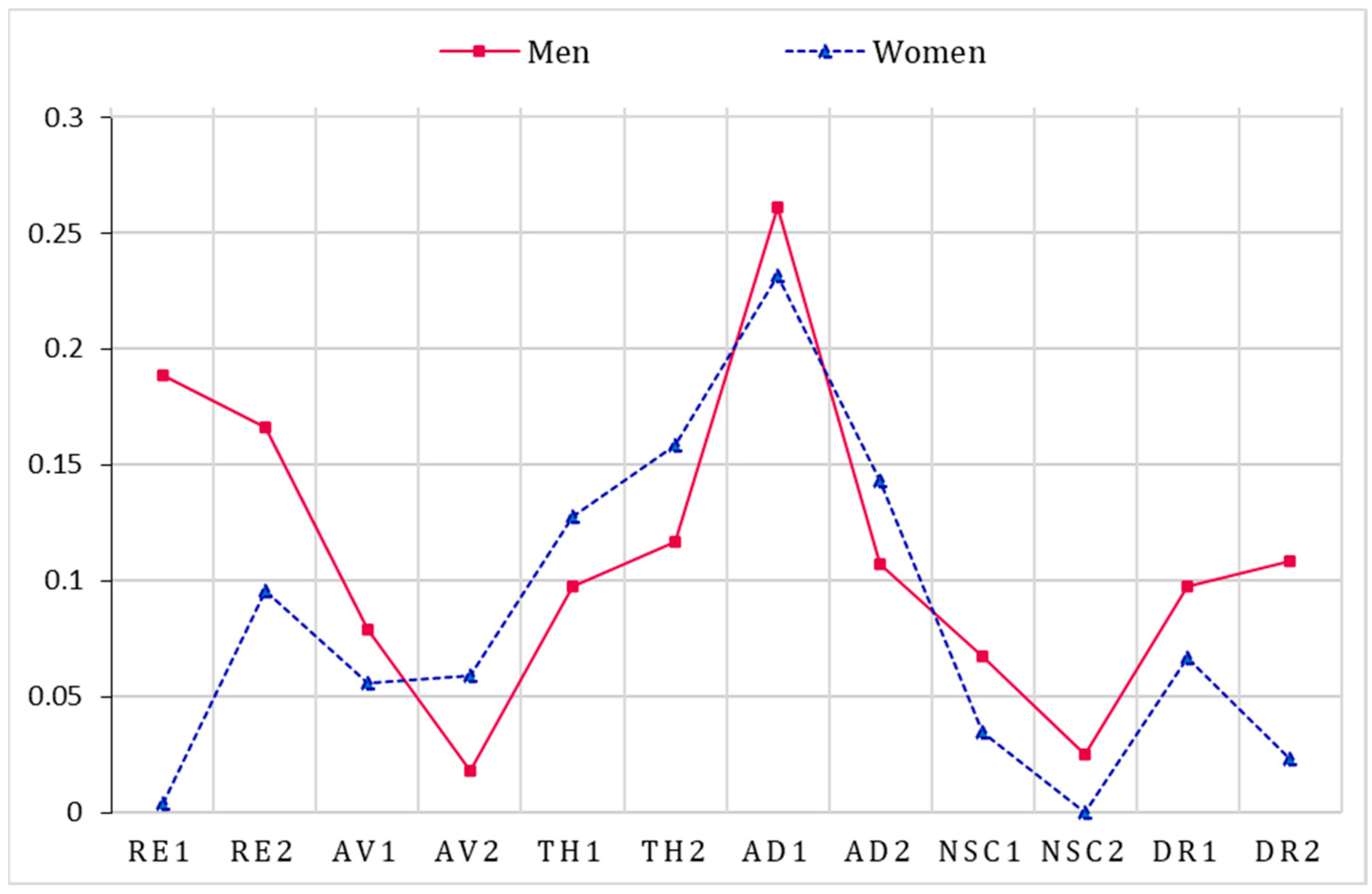
3.2. Network Accuracy and Stability
3.3. Network Comparison
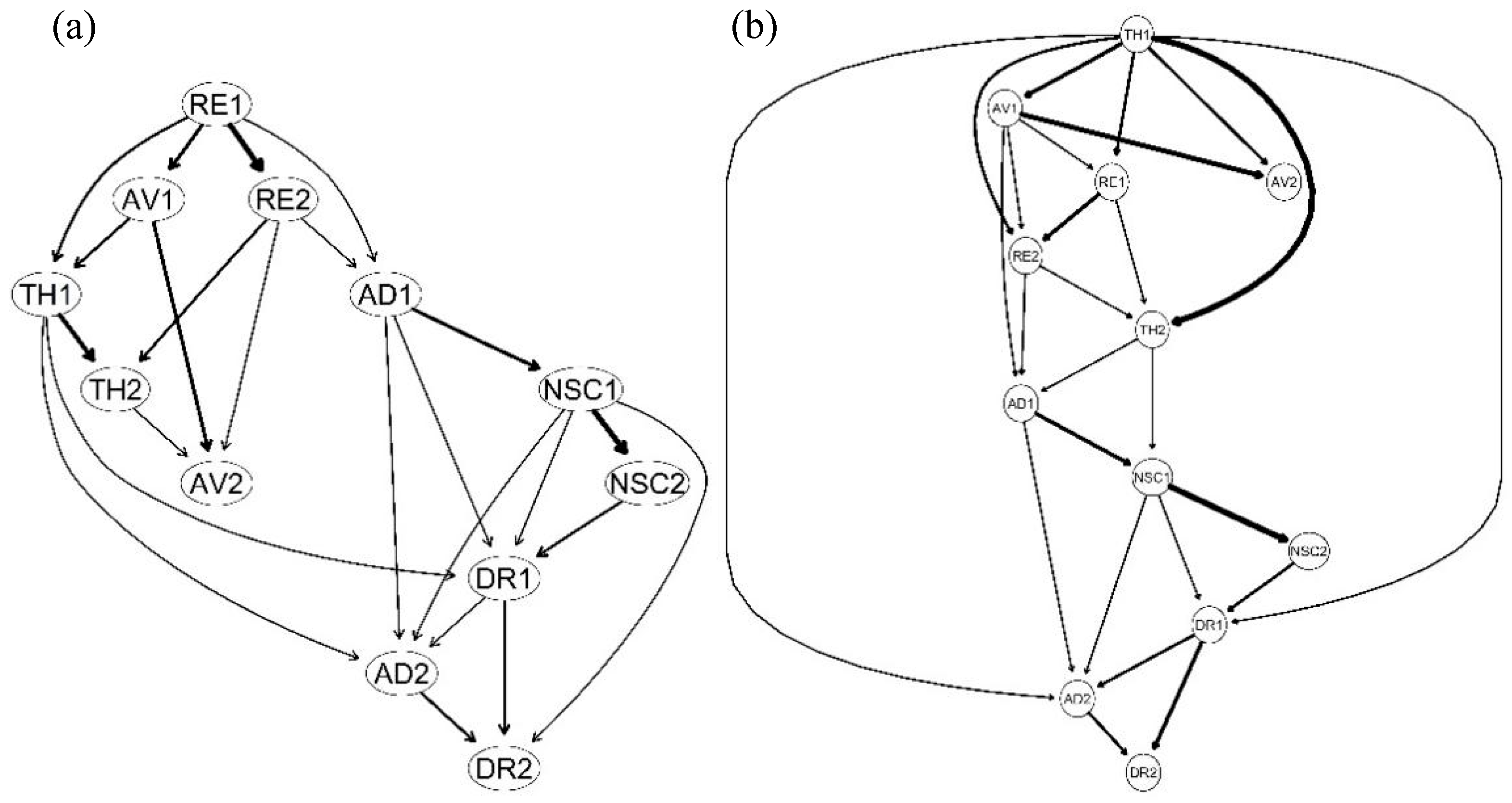
3.4. Bayesian Network
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Herman, J.L. Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. J. Trauma. Stress 1992, 5, 377–391. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Diseases-11 the Version (ICD-11). Available online: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/585833559 (accessed on 13 October 2022).
- Hyland, P.; Murphy, J.; Shevlin, M.; Vallières, F.; McElroy, E.; Elklit, A.; Christoffersen, M.; Cloitre, M. Variation in post-traumatic response: The role of trauma type in predicting ICD-11 PTSD and CPTSD symptoms. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 727–736. [Google Scholar] [CrossRef] [PubMed]
- Daniunaite, I.; Cloitre, M.; Karatzias, T.; Shevlin, M.; Thoresen, S.; Zelviene, P.; Kazlauskas, E. PTSD and complex PTSD in adolescence: Discriminating factors in a population-based cross-sectional study. Eur. J. Psychotraumatol. 2021, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Brewin, C.R.; Cloitre, M.; Hyland, P.; Shevlin, M.; Maercker, A.; Bryant, R.A.; Humayun, A.; Jones, L.M.; Kagee, A.; Rousseau, C.; et al. A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clin. Psychol. Rev. 2017, 58, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Cloitre, M. ICD-11 complex post-traumatic stress disorder: Simplifying diagnosis in trauma populations. Br. J. Psychiatry 2020, 216, 129–131. [Google Scholar] [CrossRef]
- Chiu, H.T.S.; Alberici, A.; Claxton, J.; Meiser-Stedman, R. The prevalence, latent structure and psychosocial and cognitive correlates of complex post-traumatic stress disorder in an adolescent community sample. J. Affect. Disord. 2023, 340, 482–489. [Google Scholar] [CrossRef]
- Hyland, P.; Shevlin, M.; Brewin, C.R. The Memory and Identity Theory of ICD-11 Complex Posttraumatic Stress Disorder. Psychol. Rev. 2023, 130, 1044–1065. [Google Scholar] [CrossRef]
- Borsboom, D. Psychometric perspectives on diagnostic systems. J. Clin. Psychol. 2008, 64, 1089–1108. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef]
- Bringmann, L.F.; Albers, C.; Bockting, C.; Borsboom, D.; Ceulemans, E.; Cramer, A.; Epskamp, S.; Eronen, M.I.; Hamaker, E.; Kuppens, P. Psychopathological networks: Theory, methods and practice. Behav. Res. Ther. 2022, 149, 104011. [Google Scholar] [CrossRef]
- Strauss, G.P.; Esfahlani, F.Z.; Kirkpatrick, B.; Allen, D.N.; Gold, J.M.; Visser, K.F.; Sayama, H. Network analysis reveals which negative symptom domains are most central in schizophrenia vs bipolar disorder. Schizophr. Bull. 2019, 45, 1319–1330. [Google Scholar] [CrossRef] [PubMed]
- Beard, C.; Millner, A.J.; Forgeard, M.J.; Fried, E.I.; Hsu, K.J.; Treadway, M.; Leonard, C.V.; Kertz, S.; Björgvinsson, T. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol. Med. 2016, 46, 3359–3369. [Google Scholar] [CrossRef]
- Karatzias, T.; Shevlin, M.; Hyland, P.; Ben-Ezra, M.; Cloitre, M.; Owkzarek, M.; McElroy, E. The network structure ofICD-11 complex post-traumatic stress disorder across different traumatic life events. World Psychiatry 2020, 19, 400–401. [Google Scholar] [CrossRef]
- Knefel, M.; Karatzias, T.; Ben-Ezra, M.; Cloitre, M.; Lueger-Schuster, B.; Maercker, A. The replicability of ICD-11 complex post-traumatic stress disorder symptom networks in adults. Br. J. Psychiatry 2019, 214, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Knefel, M.; Lueger-Schuster, B.; Bisson, J.; Karatzias, T.; Kazlauskas, E.; Roberts, N.P. A cross-cultural comparison of icd-11 complex posttraumatic stress disorder symptom networks in Austria, the United Kingdom, and Lithuania. J. Trauma. Stress 2020, 33, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Levin, Y.; Hyland, P.; Karatzias, T.; Shevlin, M.; Bachem, R.; Maercker, A.; Ben-Ezra, M. Comparing the network structure of ICD-11 PTSD and complex PTSD in three African countries. J. Psychiatr. Res. 2021, 136, 80–86. [Google Scholar] [CrossRef] [PubMed]
- McElroy, E.; Shevlin, M.; Murphy, S.; Roberts, B.; Makhashvili, N.; Javakhishvili, J.; Bisson, J.; Ben-Ezra, M.; Hyland, P. ICD-11 PTSD and complex PTSD: Structural validation using network analysis. World Psychiatry 2019, 18, 236–237. [Google Scholar] [CrossRef]
- Schiess-Jokanovic, J.; Knefel, M.; Kantor, V.; Weindl, D.; Schafer, I.; Lueger-Schuster, B. The boundaries between complex posttraumatic stress disorder symptom clusters and post-migration living difficulties in traumatised Afghan refugees: A network analysis. Confl. Health 2022, 16, 10. [Google Scholar] [CrossRef]
- Afifi, M. Gender differences in mental health. Singap. Med. J. 2007, 48, 385. [Google Scholar]
- Hartung, C.M.; Widiger, T.A. Gender differences in the diagnosis of mental disorders: Conclusions and controversies of the DSM–IV. Psychol. Bull. 1998, 123, 260. [Google Scholar] [CrossRef]
- Cao, X.; Wang, L.; Cao, C.Q.; Fang, R.J.; Chen, C.; Hall, B.J.; Elhai, J.D. Sex differences in global and local connectivity of adolescent posttraumatic stress disorder symptoms. J. Child Psychol. Psychiatry 2019, 60, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.M.; Zhou, Y.Y.; Liu, Z.K. Traumatic experiences and posttraumatic stress disorder among Chinese rural-to-urban migrant children. J. Affect. Disord. 2019, 257, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Dückers, M.L.; Olff, M. Does the vulnerability paradox in PTSD apply to women and men? An exploratory study. J. Trauma. Stress 2017, 30, 200–204. [Google Scholar] [CrossRef] [PubMed]
- Breslau, N.; Anthony, J.C. Gender differences in the sensitivity to posttraumatic stress disorder: An epidemiological study of urban young adults. J. Abnorm. Psychol. 2007, 116, 607. [Google Scholar] [CrossRef] [PubMed]
- Pietrzak, R.H.; Feder, A.; Singh, R.; Schechter, C.B.; Bromet, E.J.; Katz, C.; Reissman, D.; Ozbay, F.; Sharma, V.; Crane, M. Trajectories of PTSD risk and resilience in World Trade Center responders: An 8-year prospective cohort study. Psychol. Med. 2014, 44, 205–219. [Google Scholar] [CrossRef]
- Priebe, S.; Grappasonni, I.; Mari, M.; Dewey, M.; Petrelli, F.; Costa, A. Posttraumatic stress disorder six months after an earthquake. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 393–397. [Google Scholar] [CrossRef]
- Hourani, L.; Williams, J.; Bray, R.; Kandel, D. Gender differences in the expression of PTSD symptoms among active duty military personnel. J. Anxiety Disord. 2015, 29, 101–108. [Google Scholar] [CrossRef]
- King, M.W.; Street, A.E.; Gradus, J.L.; Vogt, D.S.; Resick, P.A. Gender differences in posttraumatic stress symptoms among OEF/OIF veterans: An item response theory analysis. J. Trauma. Stress 2013, 26, 175–183. [Google Scholar] [CrossRef]
- Cloitre, M.; Hyland, P.; Bisson, J.I.; Brewin, C.R.; Roberts, N.P.; Karatzias, T.; Shevlin, M. ICD-11 Posttraumatic Stress Disorder and Complex Posttraumatic Stress Disorder in the United States: A Population-Based Study. J. Trauma. Stress 2019, 32, 833–842. [Google Scholar] [CrossRef]
- Karatzias, T.; Hyland, P.; Bradley, A.; Fyvie, C.; Logan, K.; Easton, P.; Thomas, J.; Philips, S.; Bisson, J.I.; Roberts, N.P. Is self-compassion a worthwhile therapeutic target for ICD-11 Complex PTSD (CPTSD)? Behav. Cognit. Psychther. 2019, 47, 257–269. [Google Scholar] [CrossRef]
- Cloitre, M.; Shevlin, M.; Brewin, C.R.; Bisson, J.I.; Roberts, N.P.; Maercker, A.; Karatzias, T.; Hyland, P. The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr. Scand. 2018, 138, 536–546. [Google Scholar] [CrossRef]
- Ho, G.W.K.; Karatzias, T.; Cloitre, M.; Chan, A.C.Y.; Bressington, D.; Chien, W.T.; Hyland, P.; Shevlin, M. Translation and validation of the Chinese ICD-11 International Trauma Questionnaire (ITQ) for the Assessment of Posttraumatic Stress Disorder (PTSD) and Complex PTSD (CPTSD). Eur. J. Psychotraumatol. 2019, 10, 10. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The Life Events Checklist for DSM-5 (LEC-5). Instrument Available from the National Center for PTSD. 2013. Available online: www.ptsd.va.gov (accessed on 13 October 2022).
- Epskamp, S.; Fried, E.I. A tutorial on regularized partial correlation networks. Psychol. Methods 2018, 23, 617. [Google Scholar] [CrossRef] [PubMed]
- Epskamp, S.; Cramer, A.O.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. qgraph: Network visualizations of relationships in psychometric data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2008, 9, 432–441. [Google Scholar] [CrossRef]
- Van Borkulo, C.D.; Borsboom, D.; Epskamp, S.; Blanken, T.F.; Boschloo, L.; Schoevers, R.A.; Waldorp, L.J. A new method for constructing networks from binary data. Sci. Rep. 2014, 4, 5918. [Google Scholar] [CrossRef]
- Opsahl, T.; Agneessens, F.; Skvoretz, J. Node centrality in weighted networks: Generalizing degree and shortest paths. Soc. Netw. 2010, 32, 245–251. [Google Scholar] [CrossRef]
- Jones, P.J.; Ma, R.; McNally, R.J. Bridge Centrality: A Network Approach to Understanding Comorbidity. Multivar. Behav. Res. 2021, 56, 353–367. [Google Scholar] [CrossRef]
- Epskamp, S.; Fried, E.I. Package ‘bootnet’. R Package Version 1. 2020. Available online: https://mirror.las.iastate.edu/CRAN/web/packages/bootnet/bootnet.pdf (accessed on 13 October 2022).
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Pearl, J. From Bayesian networks to causal networks. In Mathematical Models for Handling Partial Knowledge in Artificial Intelligence; Springer: Berlin/Heidelberg, Germany, 1995; pp. 157–182. [Google Scholar]
- Moffa, G.; Catone, G.; Kuipers, J.; Kuipers, E.; Freeman, D.; Marwaha, S.; Lennox, B.R.; Broome, M.R.; Bebbington, P. Using directed acyclic graphs in epidemiological research in psychosis: An analysis of the role of bullying in psychosis. Schizophr. Bull. 2017, 43, 1273–1279. [Google Scholar] [CrossRef]
- Daly, R.; Shen, Q. Methods to accelerate the learning of bayesian network structures. In Proceedings of the 2007 UK Workshop on Computational Intelligence, London, UK, 23–24 July 2007. [Google Scholar]
- McNally, R.J. Networks and nosology in posttraumatic stress disorder. JAMA Psychiatry 2017, 74, 124–125. [Google Scholar] [CrossRef] [PubMed]
- Weindl, D.; Lueger-Schuster, B. Coming to terms with oneself: A mixed methods approach to perceived self-esteem of adult survivors of childhood maltreatment in foster care settings. BMC Psychol. 2018, 6, 47. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Cicchetti, D. Longitudinal trajectories of self-system processes and depressive symptoms among maltreated and nonmaltreated children. Child Dev. 2006, 77, 624–639. [Google Scholar] [CrossRef] [PubMed]
- Bryant, R.A.; Creamer, M.; O’Donnell, M.; Forbes, D.; McFarlane, A.C.; Silove, D.; Hadzi-Pavlovic, D. Acute and chronic posttraumatic stress symptoms in the emergence of posttraumatic stress disorder: A network analysis. JAMA Psychiatry 2017, 74, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Armour, C.; Fried, E.I.; Deserno, M.K.; Tsai, J.; Pietrzak, R.H. A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in US military veterans. J. Anxiety Disord. 2017, 45, 49–59. [Google Scholar] [CrossRef]
- Bullitt, C.; Farber, B.A. Sex differences in the relationship between interpersonal problems and defensive style. Psychol. Rep. 2002, 91, 767–768. [Google Scholar] [CrossRef]
- Hammack, S.E.; Cooper, M.A.; Lezak, K.R. Overlapping neurobiology of learned helplessness and conditioned defeat: Implications for PTSD and mood disorders. Neuropharmacology 2012, 62, 565–575. [Google Scholar] [CrossRef]
- Jaworska-Andryszewska, P.; Rybakowski, J.K. Childhood trauma in mood disorders: Neurobiological mechanisms and implications for treatment. Pharmacol. Rep. 2019, 71, 112–120. [Google Scholar] [CrossRef]
- Ono, M.; Devilly, G.J.; Shum, D.H. A meta-analytic review of overgeneral memory: The role of trauma history, mood, and the presence of posttraumatic stress disorder. Psychol. Trauma 2016, 8, 157. [Google Scholar] [CrossRef]
| Event | Respondents | Percentage of the Sample |
|---|---|---|
| Natural disasters | 481 | 33.97% |
| Transportation accident | 572 | 40.40% |
| Physical assault | 605 | 42.73% |
| Life-threatening illness or injury | 343 | 24.22% |
| Unwanted or uncomfortable sexual experience | 326 | 23.02% |
| Causing serious injury or death to someone else | 314 | 22.18% |
| Assault with a weapon | 266 | 18.79% |
| Sudden accidental death | 156 | 11.02% |
| Fire or explosion | 268 | 18.93% |
| Sudden death to a loved one | 309 | 21.82% |
| Exposure to toxic substance | 100 | 7.06% |
| Sexual assault | 73 | 5.16% |
| Symptom | M | SD | Percentage |
|---|---|---|---|
| RE1 | 1.00 | 1.10 | 28.46% |
| RE2 | 1.14 | 1.19 | 36.51% |
| AV1 | 1.48 | 1.27 | 44.07% |
| AV2 | 1.41 | 1.31 | 41.81% |
| TH1 | 1.02 | 1.24 | 30.16% |
| TH2 | 1.05 | 1.21 | 30.37% |
| AD1 | 1.60 | 1.06 | 47.46% |
| AD2 | 1.25 | 1.22 | 37.50% |
| NSC1 | 1.20 | 1.25 | 35.88% |
| NSC2 | 0.97 | 1.21 | 28.46% |
| DR1 | 0.98 | 1.15 | 27.40% |
| DR2 | 1.42 | 1.30 | 36.51% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, Y.; Yang, L. Sex Differences in Complex Posttraumatic Stress Disorder Network among Chinese Young Adults. Behav. Sci. 2023, 13, 846. https://doi.org/10.3390/bs13100846
Liang Y, Yang L. Sex Differences in Complex Posttraumatic Stress Disorder Network among Chinese Young Adults. Behavioral Sciences. 2023; 13(10):846. https://doi.org/10.3390/bs13100846
Chicago/Turabian StyleLiang, Yiming, and Luxi Yang. 2023. "Sex Differences in Complex Posttraumatic Stress Disorder Network among Chinese Young Adults" Behavioral Sciences 13, no. 10: 846. https://doi.org/10.3390/bs13100846
APA StyleLiang, Y., & Yang, L. (2023). Sex Differences in Complex Posttraumatic Stress Disorder Network among Chinese Young Adults. Behavioral Sciences, 13(10), 846. https://doi.org/10.3390/bs13100846






