Futurization of Aging: Subjective Beliefs and Effects
Abstract
1. Introduction
1.1. Futurization of Aging
1.2. Resources of Aging
2. Materials and Methods
2.1. Data Collection and Research Design
- (1)
- To what extent are people in the transition period between adulthood and aging aware of strategies that could help them to form resources for a better life in aging?
- (2)
- How often were strategies of aging formation used by our participants 10 years ago?
- (3)
- Could subjective beliefs affect the reported performance of the formation of strategies of aging?
- Our study is exploratory, so we had no predictions about the extent to which our participants would be familiar with the formation of strategies of aging, but we expected that those who were more familiar would demonstrate higher scores on reported performance as well.
- Transferring the idea that more knowledge about aging in general, and particularly about stereotypes of aging, leads to better self-understanding and better mental functioning [40], we supposed that more knowledge about the formation of strategies of aging would also lead to a higher use of these strategies.
2.2. Measures
- (1)
- control over different types of fats (based on consultations with doctors);
- (2)
- going in for sports or fitness;
- (3)
- continued learning;
- (4)
- participation in social events;
- (5)
- the ability to not be nervous about minor negative events;
- (6)
- the ability to not think about problems when going to sleep;
- (7)
- intentional control over one’s sleep schedule;
- (8)
- intentional refusal to use gadgets before going to sleep;
- (9)
- following a healthy diet;
- (10)
- watching one’s water balance;
- (11)
- intention to solve complex problems (brain activity);
- (12)
- reading;
- (13)
- learning foreign languages;
- (14)
- acquiring new impressions;
- (15)
- driving;
- (16)
- thinking about how one’s own memory, attention, and cognitive abilities work;
- (17)
- thinking about how different processes (mental, emotional, physiological) work;
- (18)
- striving to regulate one’s own emotions;
- (19)
- self-analysis;
- (20)
- generativity;
- (21)
- a desire to help others;
- (22)
- control of one’s quality of sleep.
2.3. Statistical Analysis
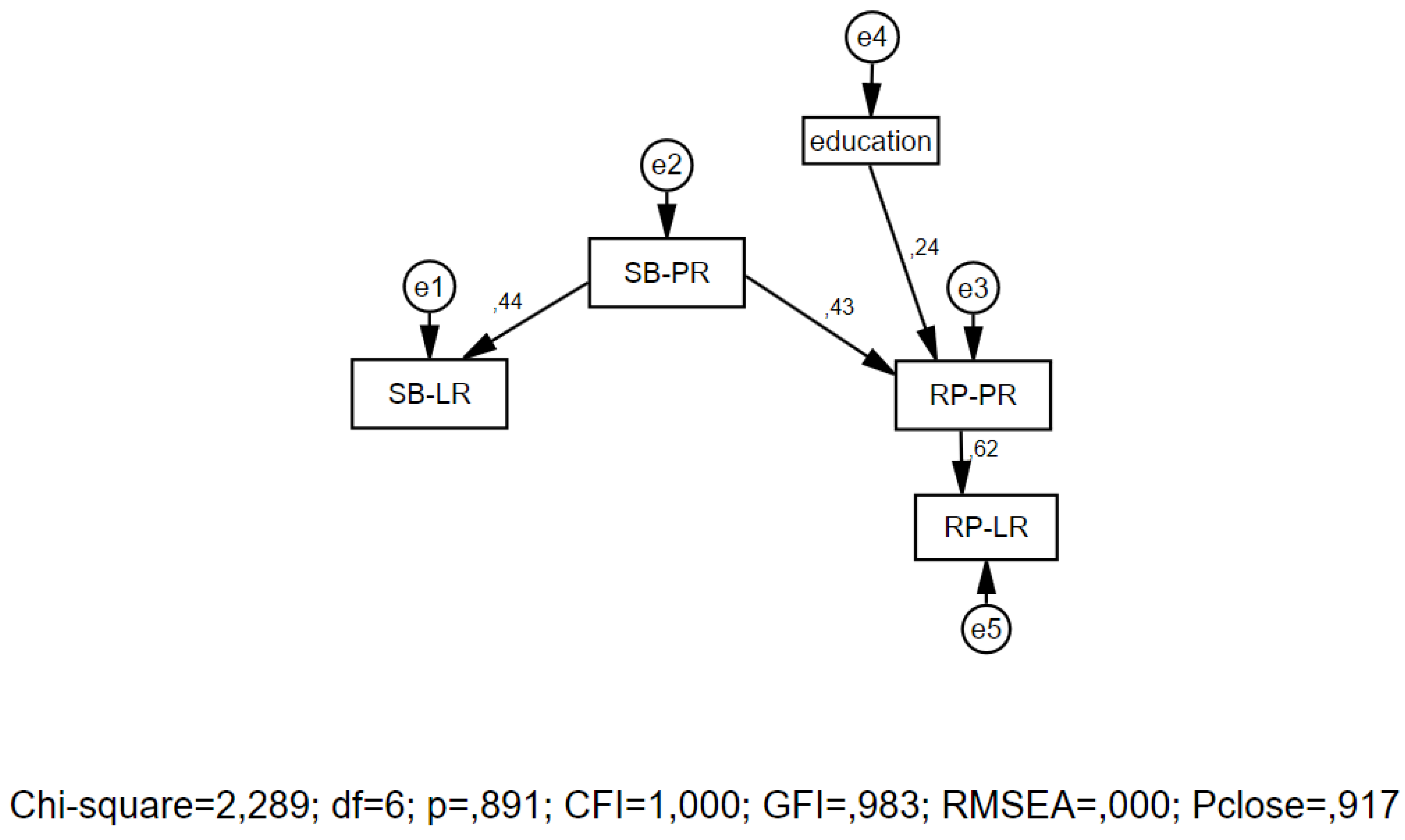
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rowe, J.W.; Kahn, R.L. Successful Aging 2.0: Conceptual Expansions for the 21st Century. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2015, 70, 593–596. [Google Scholar] [CrossRef] [PubMed]
- Baltes, P.B.; Baltes, M.M. Psychological Perspectives on Successful Aging: The Model of Selective Optimization with Compensation. In Successful Aging: Perspectives from the Behavioral Sciences; Baltes, P.B., Baltes, M.M., Eds.; Cambridge University Press: Cambridge, MA, USA, 1990; pp. 1–34. [Google Scholar]
- Olshansky, S.J.; Perry, D.; Miller, R.A.; Butler, R.N. Pursuing the Longevity Dividend. Ann. N. Y. Acad. Sci. 2007, 1114, 11–13. [Google Scholar] [CrossRef] [PubMed]
- Kirkwood, T.B.L. Why and how are we living longer? Exp. Physiol. 2017, 102, 1067–1074. [Google Scholar] [CrossRef] [PubMed]
- Fong, B.Y.F.; Chiu, W.-K.; Chan, W.F.M.; Lam, T.Y. A review study of a green diet and healthy ageing. Int. J. Environ. Res. Public Health 2021, 18, 8024. [Google Scholar] [CrossRef] [PubMed]
- Stessman, J.; Jacobs, J.M. Diabetes Mellitus, Physical Activity, and Longevity Between the Ages of 70 and 90. J. Am. Geriatr. Soc. 2014, 62, 1329–1334. [Google Scholar] [CrossRef]
- Kuzuya, M. Nutritional status related to poor health outcomes in older people: Which is better, obese or lean? Geriatr. Gerontol. Int. 2021, 21, 5–13. [Google Scholar] [CrossRef]
- Harris, K.; English, T.; Harms, P.D.; Gross, J.J.; Jackson, J.J. Why are Extraverts more satisfied? Personality, Social Experiences, And Subjective Well-Being In College. Eur. J. Personal. 2017, 31, 170–186. [Google Scholar] [CrossRef]
- Potter, S.; Drewelies, J.; Wagner, J.; Duezel, S.; Brose, A.; Demuth, I.; Steinhagen-Thiessen, E.; Lindenberger, U.; Wagner, G.G.; Gerstorf, D. Trajectories of multiple subjective well-being facets across old age: The role of health and personality. Psychol. Aging 2020, 35, 894–909. [Google Scholar] [CrossRef]
- Bjälkebring, P.; Henning, G.; Västfjäll, D.; Dickert, S.; Brehmer, Y.; Buratti, S.; Hansson, I.; Johansson, B. Helping Out or Helping Yourself? Volunteering and Life Satisfaction Across the Retirement Transition. Psychol. Aging 2021, 36, 119–130. [Google Scholar] [CrossRef]
- Shane, J.; Niwa, E.Y.; Heckhausen, J. Prosociality Across Adulthood: A Developmental and Motivational Perspective. Psychol. Aging 2021, 36, 22–35. [Google Scholar] [CrossRef]
- World Health Organization: Decade of Healthy Ageing 2020–2030” reported conceptualized. Available online: https://www.who.int/docs/default-source/documents/decade-of-health-ageing/decade-healthy-ageing-update-march-2019.pdf?sfvrsn=5a6d0e5c_2 (accessed on 14 November 2022).
- Strizhitskaya, O.Y.; Petrash, M.D. Construction of Productive Ageing: Biological, Psychological and Environmental Factors [Elektronnyi resurs]. Konsul’tativnaya Psikhologiya I Psikhoterapiya Couns. Psychol. Psychother. 2022, 30, 8–28. (In Russian) [Google Scholar] [CrossRef]
- Sircova, A. Futurization of Thinking and Behavior: Exploring People’s Imaginaries About the Future and Futurization. In Managing Screen Time in an Online Society; Oliveira, L., Ed.; Information Science Reference: Hershey, PA, USA, 2019; pp. 219–245. [Google Scholar]
- Nelson, M.E.; Jester, D.J.; Petkus, A.J.; Andel, R. Cognitive Reserve, Alzheimer’s Neuropathology, and Risk of Dementia: A Systematic Review and Meta-Analysis. Neuropsychol. Rev. 2021, 31, 233–250. [Google Scholar] [CrossRef] [PubMed]
- Häsler, R.; Venkatesh, G.; Tan, Q.; Flachsbart, F.; Sinha, A.; Rosenstiel, P.; Lieb, W.; Schreiber, S.; Christensen, K.; Christiansen, L.; et al. Genetic interplay between human longevity and metabolic pathways—A large-scale eQTL study. Aging Cell 2017, 16, 716–725. [Google Scholar] [CrossRef] [PubMed]
- Murabito, J.M.; Yuan, R.; Lunetta, K.L. The search for longevity and healthy aging genes: Insights from epidemiological studies and samples of long-lived individuals. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2021, 67, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, E.A.; Brunet, A. Lipid Profiles and Signals for Long Life. Trends Endocrinol. Metab. TEM 2015, 26, 589–592. [Google Scholar] [CrossRef] [PubMed]
- Zarulli, V.; Barthold Jones, J.A.; Oksuzyan, A.; Lindahl-Jacobsen, R.; Christensen, K.; Vaupel, J.W. Women live longer than men even during severe famines and epidemics. Proc. Natl. Acad. Sci. USA 2018, 115, E832–E840. [Google Scholar] [CrossRef]
- Jacobs, J.M.; Cohen, A.; Ein-Mor, E.; Stessman, J. Cholesterol, statins, and longevity from age 70 to 90 years. J. Am. Med. Dir. Assoc. 2013, 14, 883–888. [Google Scholar] [CrossRef]
- Samieri, C.; Jutand, M.A.; Feart, C.; Capuron, L.; Letenneur, L.; Barberger-Gateau, P. Dietary patterns derived by hybrid clus-tering method in older people: Association with cognition, mood, and self-rated health. J. Am. Diet. Assoc. 2008, 108, 1461–1471. [Google Scholar] [CrossRef]
- Fortes, C.; Mastroeni, S.; Sperati, A.; Pacifici, R.; Zuccaro, P.; Francesco, F.; Ebrahim, S. Walking four times weekly for at least 15min is associated with longevity in a Cohort of very elderly people. Maturitas 2013, 74, 246–251. [Google Scholar] [CrossRef]
- Cullell, N.; Cárcel-Márquez, J.; Gallego-Fábrega, C.; Muiño, E.; Llucià-Carol, L.; Lledós, M.; Amaut, K.E.U.; Krupinski, J.; Fer-nández-Cadenas, I. Sleep/wake cycle alterations as a cause of neurodegenerative diseases: A Mendelian randomization study. Neurobiol. Aging 2021, 106, 320.e1–320.e12. [Google Scholar] [CrossRef] [PubMed]
- Didikoglu, A.; Maharani, A.; Payton, A.; Pendleton, N.; Canal, M.M. Longitudinal change of sleep timing: Association between chronotype and longevity in older adults. Chronobiol. Int. 2019, 36, 1285–1300. [Google Scholar] [CrossRef] [PubMed]
- Zanjani, F.; Downer, B.G.; Kruger, T.M.; Willis, S.L.; Schaie, K.W. Alcohol effects on cognitive change in middle-aged and older adults. Aging Ment. Health 2013, 17, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Arntzen, K.A.; Schirmer, H.; Wilsgaard, T.; Mathiesen, E.B. Moderate wine consumption is associated with better cognitive test results: A 7 year follow up of 5033 subjects in the Tromsø Study. Acta Neurol. Scand. 2010, 122, 23–29. [Google Scholar] [CrossRef] [PubMed]
- McNaughton, S.A.; Dunstan, D.W.; Ball, K.; Shaw, J.; Crawford, D. Dietary quality is associated with diabetes and car-diometabolic risk factors. J. Nutr. 2009, 139, 734–742. [Google Scholar] [CrossRef] [PubMed]
- McNaughton, S.A.; Bates, C.J.; Mishra, G.D. Diet quality is associated with all-cause mortality in adults aged 65 years and older. J. Nutr. 2012, 142, 320–325. [Google Scholar] [CrossRef]
- Bourre, J.M. Effects of nutrients (in food) on the structure and function of the nervous system: Update on dietary requirements for brain. Part 2: Macronutrients. J. Nutr. Health Aging 2006, 10, 386–399. [Google Scholar]
- Bourre, J.M. Effects of nutrients (in food) on the structure and function of the nervous system: Update on dietary requirements for brain. Part 1: Micronutrients. J. Nutr. Health Aging 2006, 10, 377–385. [Google Scholar]
- Paterson, D.H.; Warburton, D.E. Physical activity and functional limitations in older adults: A systematic review related to Canada’s physical activity guidelines. Int. J. Behav. Nutr. Phys. Act. 2010, 11, 7–38. [Google Scholar] [CrossRef]
- Renner, B.; Spivak, Y.; Kwon, S.; Schwarzer, R. Does age make a difference? Predicting physical activity of South Koreans. Psychol. Aging 2007, 22, 482–493. [Google Scholar] [CrossRef]
- Simons, L.A.; Simons, J.; McCallum, J.; Friedlander, Y. Lifestyle factors and risk of dementia: Dubbo study of the elderly. Med. J. Aust. 2006, 184, 68–70. [Google Scholar] [CrossRef]
- Miller, D.I.; Taler, V.; Davidson, P.S.; Messier, C. Measuring the impact of exercise on cognitive aging: Methodological issues. Neurobiol. Aging 2012, 33, 622.e29–622.e43. [Google Scholar] [CrossRef] [PubMed]
- Shubert, T.E.; McCulloch, K.; Hartman, M.; Giuliani, C.A. The effect of an exercise-based balance intervention on physical and cognitive performance for older adults: A pilot study. J. Geriatr. Phys. Ther. 2010, 33, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Mather, M. The emotion paradox in the aging brain. Ann. N. Y. Acad. Sci. 2012, 1251, 33–49. [Google Scholar] [CrossRef]
- Scheibe, S.; Carstensen, L.L. Emotional Aging: Recent Findings and Future Trends. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2010, 65, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, T.; Shimotsukasa, T.; Oshio, A. Cross-sectional age differences in the Dark Triad traits in two Japanese samples. Psychol. Aging 2020, 35, 91–96. [Google Scholar] [CrossRef]
- Sparrow, E.P.; Swirsky, L.T.; Kudus, F.; Spaniol, J. Aging and Altruism: A Meta-Analysis. Psychol. Aging 2021, 36, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Townsend, B.G.; Chen, J.T.-H.; Wuthrich, V.M. Barriers and Facilitators to Social Participation in Older Adults: A Systematic Literature Review. Clin. Gerontol. 2021, 44, 359–380. [Google Scholar] [CrossRef]
- Nikitin, J.; Freund, A.M. Does Focusing on Others Enhance Subjective Well-Being? The Role of Age, Motivation, and Rela-tionship Closeness. Psychol. Aging 2021, 36, 69–82. [Google Scholar] [CrossRef]
- Levy, B.R.; Chang, E.-S.; Lowe, S.R.; Provolo, N.; Slade, M.D. Impact of Media-Based Negative and Positive Age Stereotypes on Older Individuals’ Mental Health. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2022, 7, e70–e75. [Google Scholar] [CrossRef]
| Strategies of Aging Formation (SAF) | SB-SAF | RP-SAF | Cor. | p | Bootstrap CI (95%) | |||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | Low Limit | High Limit | |||
| Psychological resources | ||||||||
| Continued learning | 3.27 | 1.10 | 3.29 | 1.34 | −0.126 | 0.312 | −0.484 | 0.409 |
| Participation in social events | 3.39 | 1.19 | 3.11 | 1.49 | 0.393 | 0.001 | −0.091 | 0.636 |
| Intention to solve complex problems | 4.24 | 0.86 | 3.27 | 1.20 | 0.189 | 0.129 | 0.652 | 1.258 |
| Learning foreign languages | 3.47 | 1.38 | 2.17 | 1.40 | 0.269 | 0.029 | 0.864 | 1.697 |
| Acquiring new impressions | 4.35 | 0.77 | 3.52 | 1.30 | 0.398 | 0.001 | 0.530 | 1.167 |
| Driving | 3.41 | 1.45 | 2.94 | 1.82 | 0.529 | 0.000 | 0.061 | 0.833 |
| Thinking about how own memory, attention, cognitive abilities work | 3.52 | 1.10 | 3.00 | 1.44 | 0.380 | 0.002 | 0.167 | 0.879 |
| Thinking about how different processes work | 3.52 | 1.13 | 2.59 | 1.40 | 0.291 | 0.018 | 0.545 | 1.287 |
| Self-analysis | 3.45 | 1.15 | 3.08 | 1.35 | 0.343 | 0.005 | 0.016 | 0.727 |
| Generativity | 3.91 | 0.99 | 3.53 | 1.29 | 0.400 | 0.001 | 0.061 | 0.682 |
| Desire to help others | 4.24 | 0.90 | 4.39 | 0.74 | 0.456 | 0.000 | −0.364 | 0.061 |
| Lifestyle resources | ||||||||
| Controlling fats | 3.27 | 1.38 | 1.67 | 1.00 | −0.022 | 0.858 | 1.197 | 2.015 |
| Going in for sports or fitness | 3.71 | 1.15 | 2.61 | 1.35 | 0.025 | 0.842 | 0.652 | 1.530 |
| Not being nervous about minor negative events | 4.12 | 0.95 | 3.05 | 1.23 | −0.096 | 0.441 | 0.652 | 1.484 |
| Not thinking about problems when going to sleep | 4.12 | 0.94 | 2.91 | 1.20 | −0.031 | 0.804 | 0.803 | 1.576 |
| Intentional control over sleep schedule | 4.14 | 1.01 | 2.73 | 1.38 | 0.216 | 0.081 | 1.061 | 1.757 |
| Intentional refusal to use gadgets before going to sleep | 3.98 | 0.98 | 2.47 | 1.32 | 0.291 | 0.018 | 1.152 | 1.848 |
| Following healthy diet | 4.35 | 0.89 | 2.89 | 1.25 | −0.119 | 0.343 | 1.076 | 1.818 |
| Watching water balance | 4.21 | 0.90 | 2.79 | 1.20 | 0.213 | 0.086 | 1.106 | 1.727 |
| Reading | 4.05 | 1.09 | 3.35 | 1.20 | 0.319 | 0.009 | 0.394 | 1.015 |
| Striving to regulate own emotions | 3.95 | 0.98 | 3.00 | 1.24 | 0.441 | 0.000 | 0.667 | 1.258 |
| Controlled of quality of sleep | 4.48 | 0.73 | 3.17 | 1.21 | 0.291 | 0.018 | 1.030 | 1.636 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strizhitskaya, O.; Petrash, M.; Golubitskaya, D.; Kuzmina, M.; Krupina, K.; Shchukin, A.; Engelgardt, E. Futurization of Aging: Subjective Beliefs and Effects. Behav. Sci. 2023, 13, 4. https://doi.org/10.3390/bs13010004
Strizhitskaya O, Petrash M, Golubitskaya D, Kuzmina M, Krupina K, Shchukin A, Engelgardt E. Futurization of Aging: Subjective Beliefs and Effects. Behavioral Sciences. 2023; 13(1):4. https://doi.org/10.3390/bs13010004
Chicago/Turabian StyleStrizhitskaya, Olga, Marina Petrash, Daria Golubitskaya, Maria Kuzmina, Kristina Krupina, Anton Shchukin, and Elena Engelgardt. 2023. "Futurization of Aging: Subjective Beliefs and Effects" Behavioral Sciences 13, no. 1: 4. https://doi.org/10.3390/bs13010004
APA StyleStrizhitskaya, O., Petrash, M., Golubitskaya, D., Kuzmina, M., Krupina, K., Shchukin, A., & Engelgardt, E. (2023). Futurization of Aging: Subjective Beliefs and Effects. Behavioral Sciences, 13(1), 4. https://doi.org/10.3390/bs13010004







