Parental-Bonding and Alexithymia in Adolescents with Anorexia Nervosa, Their Parents, and Siblings
Abstract
:1. Introduction
Psychological Mechanisms
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Statistical Analyses
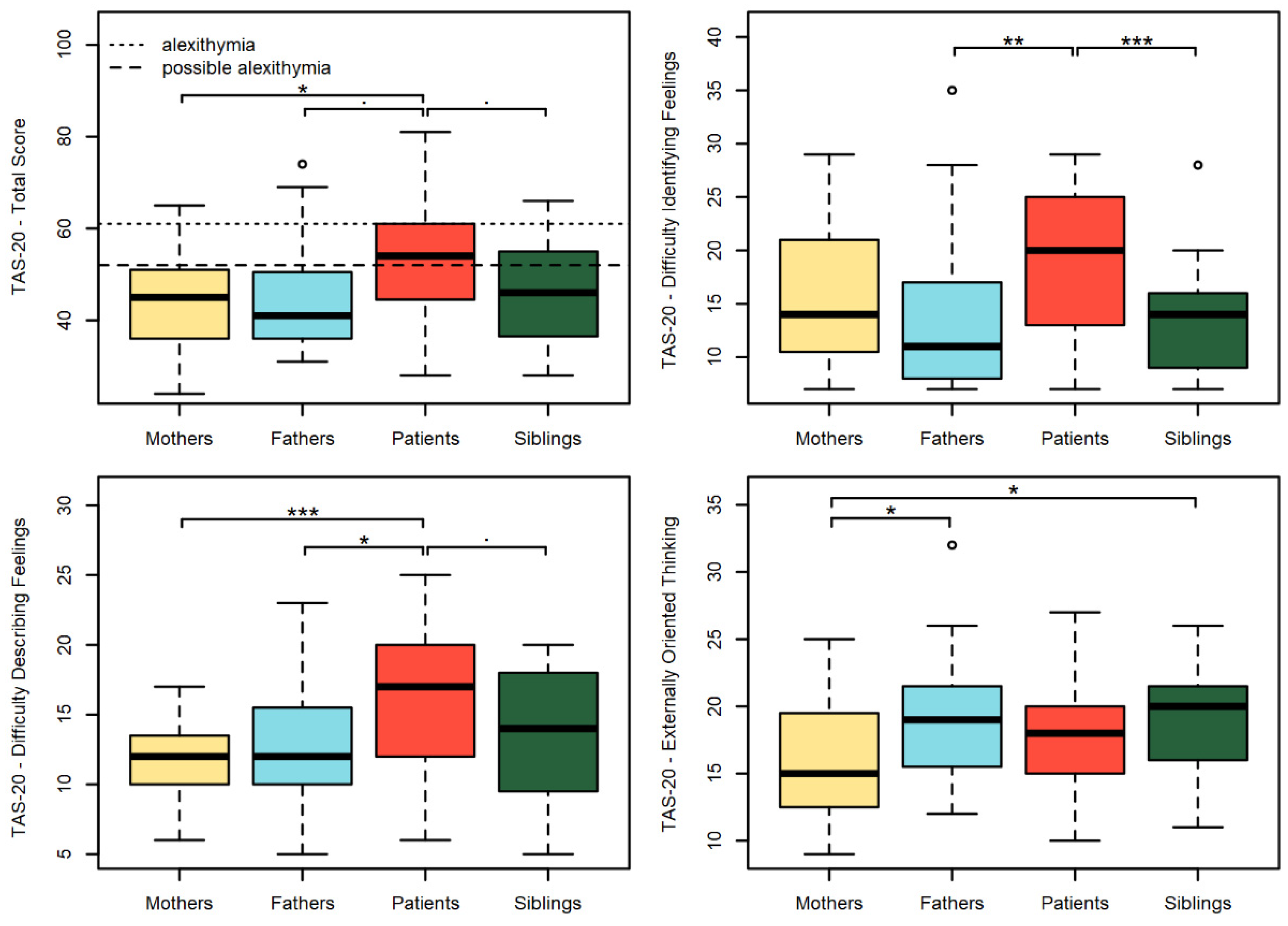
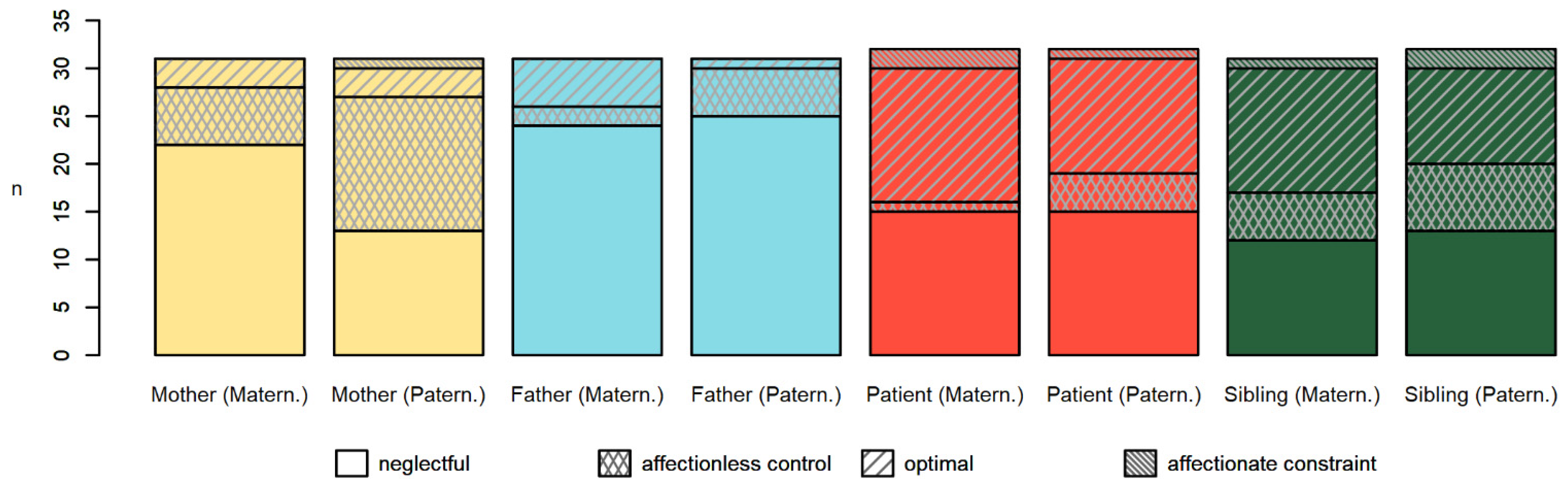
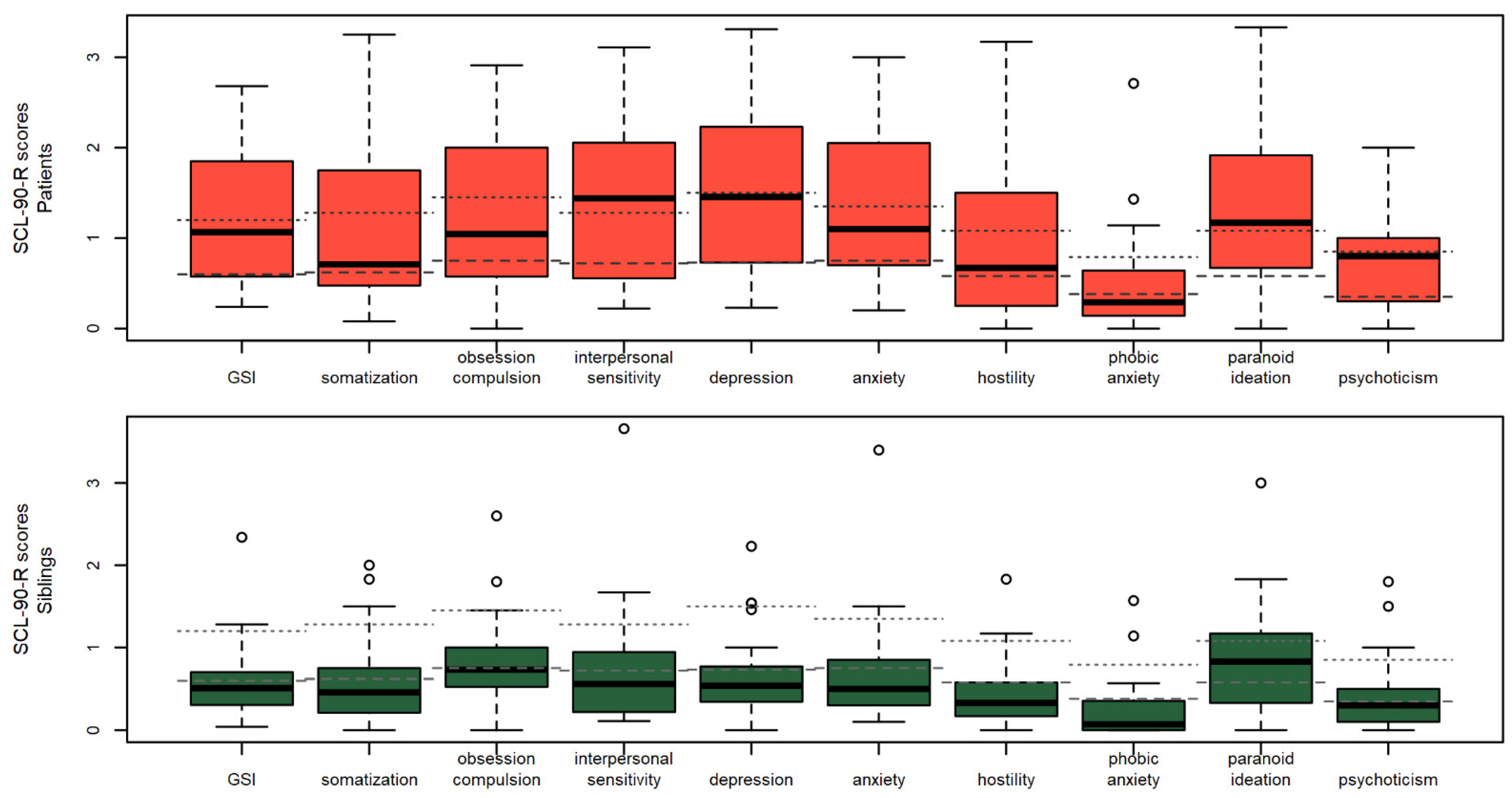
3. Results
Trait Interactions in Patients and Siblings
4. Discussion
4.1. Findings of the Current Study
4.2. Strengths and Limitations
4.3. Clinical Implications
4.4. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smink, F.R.; Van Hoeken, D.; Hoek, H.W. Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Curr. Psychiatry Rep. 2012, 14, 406–414. [Google Scholar] [CrossRef] [Green Version]
- Arcelus, J.; Mitchell, A.J.; Wales, J.; Nielsen, S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Arch. Gen. Psychiatry 2011, 68, 724–731. [Google Scholar] [CrossRef] [Green Version]
- Crow, S.J.; Peterson, C.B.; Swanson, S.A.; Raymond, N.C.; Specker, S.; Eckert, E.D.; Mitchell, J.E. Increased mortality in bulimia nervosa and other eating disorders. Am. J. Psychiatry 2009, 166, 1342–1346. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Harrison, P.J. Eating disorders. Lancet 2003, 361, 407–416. [Google Scholar] [CrossRef]
- Hay, P. A systematic review of evidence for psychological treatments in eating disorders: 2005–2012. Int. J. Eat. Disord. 2013, 46, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Tauro, J.L.; Wearne, T.A.; Belevski, B.; Filipčíková, M.; Francis, H.M. Social cognition in female adults with Anorexia Nervosa: A systematic review. Neurosci. Biobehav. Rev. 2022, 132, 197–210. [Google Scholar] [CrossRef]
- Sibeoni, J.; Orri, M.; Colin, S.; Valentin, M.; Pradère, J.; Revah-Levy, A. The lived experience of anorexia nervosa in adolescence, comparison of the points of view of adolescents, parents, and professionals: A metasynthesis. Int. J. Nurs. Stud. 2017, 65, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Meule, A.; Richard, A.; Schnepper, R.; Reichenberger, J.; Georgii, C.; Naab, S.; Voderholzer, U.; Blechert, J. Emotion regulation and emotional eating in anorexia nervosa and bulimia nervosa. Eat. Disord. 2021, 29, 175–191. [Google Scholar] [CrossRef] [Green Version]
- Beckmann, N.; Baumann, P.; Herpertz, S.; Trojan, J.; Diers, M. How the unconscious mind controls body movements: Body schema distortion in anorexia nervosa. Int. J. Eat. Disord. 2021, 54, 578–586. [Google Scholar] [CrossRef]
- Muratore, A.F.; Attia, E. Current therapeutic approaches to anorexia nervosa: State of the art. Clin. Ther. 2021, 43, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Pietrabissa, G.; Rossi, A.; Simpson, S.; Tagliagambe, A.; Bertuzzi, V.; Volpi, C.; Fava, G.; Manzoni, G.M.; Gravina, G.; Castelnuovo, G. Evaluation of the reliability and validity of the Italian version of the schema mode inventory for eating disorders: Short form for adults with dysfunctional eating behaviors. Eat. Weight Disord. 2020, 25, 553–565. [Google Scholar] [CrossRef] [PubMed]
- Simpson, S.G.; Pietrabissa, G.; Rossi, A.; Seychell, T.; Manzoni, G.M.; Munro, C.; Nesci, J.B.; Castelnuovo, G. Factorial Structure and Preliminary Validation of the Schema Mode Inventory for Eating Disorders (SMI-ED). Front. Psychol. 2018, 9, 600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mannarini, S.; Balottin, L.; Toldo, I.; Gatta, M. Alexithymia and psychosocial problems among Italian preadolescents. A latent class analysis approach. Scand. J. Psychol. 2016, 57, 473–481. [Google Scholar] [CrossRef]
- Mazzeo, S.E.; Espelage, D.L. Association between childhood physical and emotional abuse and disordered eating behaviors in female undergraduates: An investigation of the mediating role of alexithymia and depression. J. Couns. Psychol. 2002, 49, 86. [Google Scholar] [CrossRef]
- Taylor, G.J.; Bagby, R.M. New trends in alexithymia research. Psychother. Psychosom. 2004, 73, 68–77. [Google Scholar] [CrossRef]
- Nowakowski, M.E.; McFarlane, T.; Cassin, S. Alexithymia and eating disorders: A critical review of the literature. J. Eat. Disord. 2013, 1, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Westwood, H.; Kerr-Gaffney, J.; Stahl, D.; Tchanturia, K. Alexithymia in eating disorders: Systematic review and meta-analyses of studies using the Toronto Alexithymia Scale. J. Psychosom. Res. 2017, 99, 66–81. [Google Scholar] [CrossRef] [Green Version]
- Erriu, M.; Cimino, S.; Cerniglia, L. The role of family relationships in eating disorders in adolescents: A narrative review. Behav. Sci. 2020, 10, 71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fjermestad, K.W.; Rø, A.E.; Espeland, K.E.; Halvorsen, M.S.; Halvorsen, I.M. “Do I exist in this world, really, or is it just her?” Youths’ perspectives of living with a sibling with anorexia nervosa. Eat. Disord. 2020, 28, 80–95. [Google Scholar] [CrossRef] [PubMed]
- Balottin, L.; Mannarini, S.; Mensi, M.M.; Chiappedi, M.; Gatta, M. Triadic Interactions in Families of Adolescents with Anorexia Nervosa and Families of Adolescents with Internalizing Disorders. Front. Psychol. 2017, 7, 2046. [Google Scholar] [CrossRef] [Green Version]
- Schaumberg, K.; Welch, E.; Breithaupt, L.; Hübel, C.; Baker, J.H.; Munn-Chernoff, M.A.; Yilmaz, Z.; Ehrlich, S.; Mustelin, L.; Ghaderi, A.; et al. The Science Behind the Academy for Eating Disorders’ Nine Truths About Eating Disorders. Eur. Eat. Disord. Rev. 2017, 25, 432–450. [Google Scholar] [CrossRef] [PubMed]
- Balottin, L.; Mannarini, S.; Mensi, M.M.; Chiappedi, M.; Balottin, U. Are family relations connected to the quality of the outcome in adolescent anorexia nervosa? An observational study with the Lausanne Trilogue Play. Clin. Psychol. Psychother. 2018, 25, 785–796. [Google Scholar] [CrossRef] [PubMed]
- Chinello, A.; Redaelli, M.; Parma, F.; Faraci, G.; Bertelli, S.; Zappa, L.E. The lack of a “Normative Male Alexithymia” in parents of daughters with anorexia nervosa: A pilot study by using the Reading the Mind in the Eyes test (RME) and the Toronto Alexithymia Scale TAS-20. Psicoter. Cogn. E Comport. 2020, 26, 13–21. [Google Scholar]
- Balottin, L.; Nacinovich, R.; Bomba, M.; Mannarini, S. Alexithymia in parents and adolescent anorexic daughters: Comparing the responses to TSIA and TAS-20 scales. Neuropsychiatr. Dis. Treat. 2014, 10, 1941–1951. [Google Scholar]
- Gatta, M.; Balottin, L.; Mannarini, S.; Chesani, G.; Del Col, L.; Spoto, A.; Battistella, P.A. Familial factors relating to alexithymic traits in adolescents with psychiatric disorders. Clin. Psychol. 2017, 21, 252–262. [Google Scholar] [CrossRef]
- Parker, G.; Tupling, H.; Brown, L.B. Parental bonding instrument (PBI). Br. J. Med. Psychol. 1979, 52, 1–10. [Google Scholar] [CrossRef]
- Mannarini, S.; Balottin, L.; Palmieri, A.; Carotenuto, F. Emotion regulation and parental bonding in families of adolescents with internalizing and externalizing symptoms. Front. Psychol. 2018, 9, 1493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tasca, G.A. Attachment and eating disorders: A research update. Curr. Opin. Psychol. 2019, 25, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Balottin, L.; Mannarini, S.; Rossi, M.; Rossi, G.; Balottin, U. The parental bonding in families of adolescents with anorexia: Attachment representations between parents and offspring. Neuropsychiatr. Dis. Treat. 2017, 13, 319–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wunderlich, U.; Gerlinghoff, M.; Backmund, H. Eating disturbances in siblings of patients with eating disorders. Eat. Weight Disord.—Stud. Anorexia Bulim. Obes. 2004, 9, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Van Langenberg, T.; Duncan, R.E.; Allen, J.S.; Sawyer, S.M.; Le Grange, D.; Hughes, E.K. “They don’t really get heard”: A qualitative study of sibling involvement across two forms of family-based treatment for adolescent anorexia nervosa. Eat. Disord. 2018, 26, 373–387. [Google Scholar] [CrossRef] [PubMed]
- Rozenstein, M.H.; Latzer, Y.; Stein, D.; Eviatar, Z. Perception of emotion and bilateral advantage in women with eating disorders, their healthy sisters, and nonrelated healthy controls. J. Affect. Disord. 2011, 134, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Persico, A.; Grandclerc, S.; Giraud, C.; Moro, M.R.; Blanchet, C. “We Thought We Were Alone”: The Subjective Experience of the Siblings of Anorexic Adolescent Patients. Front. Psychiatry 2021, 12, 664517. [Google Scholar] [CrossRef] [PubMed]
- Karlstad, J.; Moe, C.F.; Wattum, M.; Adelsten Stokland, R.; Brinchmann, B.S. “Putting your own oxygen mask on first”: A qualitative study of siblings of adults with anorexia or bulimia. J. Eat. Disord. 2021, 9, 83. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The age of adolescence. Lancet Child Adolesc. Health 2018, 2, 223–228. [Google Scholar] [CrossRef]
- Bagby, R.M.; Taylor, G.J.; Parker, J.D. The Twenty-item Toronto Alexithymia Scale—II. Convergent, discriminant, and concurrent validity. J. Psychosom. Res. 1994, 38, 33–40. [Google Scholar] [CrossRef]
- Bressi, C.; Taylor, G.; Parker, J.; Bressi, S.; Brambilla, V.; Aguglia, E.; Allegranti, I.; Bongiorno, A.; Giberti, F.; Bucca, M.; et al. Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: An Italian multicenter study. J. Psychosom. Res. 1996, 41, 551–559. [Google Scholar] [CrossRef]
- Parker, G. Parental Overprotection: A Risk Factor in Psychosocial Development; Grune & Stratton: New York, NY, USA, 1983. [Google Scholar]
- Favaretto, E.; Torresani, S.; Zimmermann, C. Further results on the reliability of the Parental Bonding Instrument (PBI) in an Italian sample of schizophrenic patients and their parents. J. Clin. Psychol. 2001, 57, 119–129. [Google Scholar] [CrossRef]
- Derogatis, L.R. SCL-90-R: Administration, Scoring and Procedures Manual; National Computer Systems Inc.: Minneapolis, MN, USA, 1994. [Google Scholar]
- Prunas, A.; Sarno, I.; Preti, E.; Madeddu, F.; Perugini, M. Psychometric properties of the Italian version of the SCL-90-R: A study on a large community sample. Eur. Psychiatry 2012, 27, 591–597. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 6 July 2020).
- Hollingshead, A.A. Four-Factor Index of Social Status; Yale University: New Haven, CT, USA, 1975. [Google Scholar]
- Bagby, R.M.; Parker, J.D.; Taylor, G.J. Twenty-five years with the 20-item Toronto Alexithymia Scale. J. Psychosom. Res. 2020, 131, 109940. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, N.; Hartkamp, N.; Franke, G.H. Assessing clinically significant change: Application to the SCL-90-R. Psychol. Rep. 2000, 86, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Sfärlea, A.; Dehning, S.; Keller, L.K.; Schulte-Körne, G. Alexithymia predicts maladaptive but not adaptive emotion regulation strategies in adolescent girls with anorexia nervosa or depression. J. Eat. Disord. 2019, 7, 41. [Google Scholar] [CrossRef] [PubMed]
- Gramaglia, C.; Gambaro, E.; Zeppegno, P. Alexithymia and Treatment Outcome in Anorexia Nervosa: A Scoping Review of the Literature. Front. Psychiatry 2020, 10, 991. [Google Scholar] [CrossRef] [PubMed]
- Bourke, M.P.; Taylor, G.J.; Parker, J.D.; Bagby, R.M. Alexithymia in women with anorexia nervosa. A preliminary investigation. Br. J. Psychiatry 1992, 161, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Sexton, M.C.; Sunday, S.R.; Hurt, S.; Halmi, K.A. The relationship between alexithymia, depression, and axis II psychopathology in eating disorder inpatients. Int. J. Eat. Disord. 1998, 23, 277–286. [Google Scholar] [CrossRef]
- McCormack, C.; McCann, E. Caring for an adolescent with anorexia nervosa: Parent’s views and experiences. Arch. Psychiatr. Nurs. 2015, 29, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Cimino, S.; Cerniglia, L.; Dentale, F.; Capobianco, M.; Tambelli, R. Maternal Symptoms of Depression and Paranoid Ideation can be Predictive of the Onset of Eating Disorders in Early Adolescents Offspring: A Nine-year Longitudinal Study. Int. J. Psychol. Psychol. Ther. 2018, 18, 221–234. [Google Scholar]
- Hughes, E.K.; Burton, C.; Le Grange, D.; Sawyer, S.M. The Participation of Mothers, Fathers, and Siblings in Family-Based Treatment for Adolescent Anorexia Nervosa. J. Clin. Child Adolesc. Psychol. 2018, 47 (Suppl. S1), S456–S466. [Google Scholar] [CrossRef]
| Family Role | Age (Years) | Birth Order | Sex | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | I | II | III | IV | F | M | |
| Mothers | 50.1 | 4.52 | 41 | 58 | 31 | - | ||||
| Fathers | 52.9 | 4.73 | 41 | 64 | - | 31 | ||||
| Patients | 18.2 | 2.60 | 14 | 24 | 14 | 15 | 2 | 1 | 32 | - |
| Siblings | 18.4 | 4.00 | 12 | 25 | 15 | 13 | 4 | 0 | 18 | 14 |
| Patients | Siblings | |||
|---|---|---|---|---|
| r | p-Value | r | p-Value | |
| GSI | 0.574 | <0.001 *** | 0.399 | 0.024 * |
| Somatization | 0.511 | 0.003 ** | 0.352 | 0.048 * |
| Obsession–compulsion | 0.593 | <0.001 *** | 0.238 | 0.189 |
| Interpersonal sensitivity | 0.575 | <0.001 *** | 0.354 | 0.047 * |
| Depression | 0.504 | 0.003 ** | 0.339 | 0.057 |
| Anxiety | 0.487 | 0.005 ** | 0.448 | 0.01 * |
| Hostility | 0.282 | 0.118 | 0.331 | 0.064 |
| Phobic anxiety | 0.087 | 0.637 | 0.323 | 0.071 |
| Paranoid ideation | 0.624 | <0.001 *** | 0.420 | 0.017 * |
| Psychoticism | 0.494 | 0.004 ** | 0.356 | 0.045 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mannarini, S.; Kleinbub, J.R. Parental-Bonding and Alexithymia in Adolescents with Anorexia Nervosa, Their Parents, and Siblings. Behav. Sci. 2022, 12, 123. https://doi.org/10.3390/bs12050123
Mannarini S, Kleinbub JR. Parental-Bonding and Alexithymia in Adolescents with Anorexia Nervosa, Their Parents, and Siblings. Behavioral Sciences. 2022; 12(5):123. https://doi.org/10.3390/bs12050123
Chicago/Turabian StyleMannarini, Stefania, and Johann Roland Kleinbub. 2022. "Parental-Bonding and Alexithymia in Adolescents with Anorexia Nervosa, Their Parents, and Siblings" Behavioral Sciences 12, no. 5: 123. https://doi.org/10.3390/bs12050123
APA StyleMannarini, S., & Kleinbub, J. R. (2022). Parental-Bonding and Alexithymia in Adolescents with Anorexia Nervosa, Their Parents, and Siblings. Behavioral Sciences, 12(5), 123. https://doi.org/10.3390/bs12050123






