Stress and Its Correlates in Migraine-Headache Patients with a Family History of Migraine
Abstract
:1. Introduction
2. Material and Methods
2.1. Participants and Procedure
2.2. Perceived Stress Scale (PSS-4)
2.3. Clinical History and Socio-Demographics
2.4. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Multivariate Analysis: Multiple Linear Regression
4. Discussion
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cohen, S.; Janicki-Deverts, D.; Miller, G.E. Psychological stress and disease. JAMA 2008, 298, 1685–1687. [Google Scholar] [CrossRef] [PubMed]
- Theeler, B.J.; Kenney, K.; Prokhorenko, O.A.; Fideli, U.S.; Campbell, W.; Erickson, J.C. Headache triggers in the US military. Headache 2010, 50, 790–794. [Google Scholar] [CrossRef] [PubMed]
- Kelman, L. The triggers or precipitants of the acute migraine attack. Cephalalgia 2007, 27, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Vives-Mestres, M.; Casanova, A.; Buse, D.C.; Donoghue, S.; Houle, T.T.; Lipton, R.B.; Mian, A.; Shulman, K.J.; Orr, S.L. Patterns of perceived stress throughout the migraine cycle: A longitudinal cohort study using daily prospective diary data. Headache 2021, 61, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Sauro, K.M.; Becker, W.J. The stress and migraine interaction. Headache 2009, 49, 1378–1386. [Google Scholar] [CrossRef]
- Rafique, N.; Al-Asoom, L.I.; Latif, R.; Alsunni, A.A.; Salem, A.M.; Alkhalifa, Z.H.; Almaharfi, R.M.; Alramadan, R.S.; Aldajani, Z.F.; Alghadeer, F.A.; et al. Prevalence of Migraine and its Relationship with Psychological Stress and Sleep Quality in Female University Students in Saudi Arabia. J. Pain Res. 2020, 3, 2423–2430. [Google Scholar] [CrossRef]
- Malone, C.D.; Bhowmick, A.; Wachholtz, A.B. Migraine: Treatments, comorbidities, and quality of life, in the USA. J. Pain Res. 2015, 8, 537–547. [Google Scholar] [CrossRef] [Green Version]
- Pelzer, N.; Louter, M.A.; van Zwet, E.W.; Nyholt, D.R.; Ferrari, M.D.; van den Maagdenberg, A.M.; Haan, J.; Terwindt, G.M. Linking migraine frequency with family history of migraine. Cephalalgia 2019, 39, 229–236. [Google Scholar] [CrossRef]
- Eidlitz-Markus, T.; Haimi-Cohen, Y.; Zeharia, A. Association of age at onset of migraine with family history of migraine in children attending a pediatric headache clinic: A retrospective cohort study. Cephalalgia 2015, 35, 722–727. [Google Scholar] [CrossRef]
- Gasparini, G.F.; Sutherland, H.G.; Griffiths, L.R. Studies on the pathophysiology and genetic basis of migraine. Curr. Genom. 2013, 14, 300–315. [Google Scholar] [CrossRef]
- Sutherland, H.G.; Albury, C.L.; Griffiths, L.R. Advances in genetics of migraine. J. Headache Pain 2019, 20, 72. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Manzar, M.D.; Salahuddin, M.; Peter, S.; Alghadir, A.; Anwer, S.; Bahammam, A.S.; Pandi-Perumal, S.R. Psychometric properties of the perceived stress scale in Ethiopian university students. BMC Public Health 2019, 19, 41. [Google Scholar] [CrossRef] [PubMed]
- Answer, S.; Manzar, M.D.; Alghadir, A.H.; Salahuddin, M.; Hameed, U.A. Psychometric Analysis of the perceived stress scale among healthy university students. Neuropsychiatr. Dis. Treat. 2020, 16, 2389–2396. [Google Scholar] [CrossRef] [PubMed]
- Houle, T.T.; Butschek, R.A.; Turner, D.P.; Smitherman, T.A.; Rains, J.C.; Penzien, D.B. Stress and sleep duration predict headache severity in chronic headache sufferers. Pain 2012, 153, 2432–2440. [Google Scholar] [CrossRef] [Green Version]
- Sullivan, D.P.; Martin, P.R. Sleep and headaches: Relationships between migraine and non-migraine headaches and sleep duration, sleep quality, chronotype, and obstructive sleep apnoea risk. Aust. J. Psychol. 2017, 69, 210–217. [Google Scholar] [CrossRef]
- Schramm, S.; Tenhagen, I.; Schmidt, B.; Holle-Lee, D.; Naegel, S.; Katsarava, Z.; Jöckel, K.H.; Moebus, S. Prevalence and risk factors of migraine and non-migraine headache in older people–results of the Heinz Nixdorf Recall study. Cephalalgia 2021, 41, 649–664. [Google Scholar] [CrossRef]
- Pavlovic, J.M.; Akcali, D.; Bolay, H.; Bernstein, C.; Maleki, N. Sex-related influences in migraine. J. Neurosci. Res. 2017, 95, 587–593. [Google Scholar] [CrossRef] [Green Version]
- Rogers, D.G.; Bond, D.S.; Bentley, J.P.; Smitherman, T.A. Objectively Measured Physical Activity in Migraine as a Function of Headache Activity. Headache 2020, 60, 1930–1938. [Google Scholar] [CrossRef]
- McLean, G.; Mercer, S.W. Chronic migraine, comorbidity, and socioeconomic deprivation: Cross-sectional analysis of a large nationally representative primary care database. J. Comorb. 2017, 7, 89–95. [Google Scholar] [CrossRef] [Green Version]
- Chowdhary, K.; Enam, N. Post-traumatic Headaches After Traumatic Brain Injury: Current Clinical Approaches. Curr. Phys. Med. Rehabil. Rep. 2021, 9, 100–107. [Google Scholar] [CrossRef]
- Lateef, T.M.; Cui, L.; Nakamura, E.; Dozier, J.; Merikangas, K. Accuracy of family history reports of migraine in a community-based family study of migraine. Headache 2015, 55, 407–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedborg, K.; Anderberg, U.M.; Muhr, C. Stress in migraine: Personality-dependent vulnerability, life events, and gender are of significance. Upsala J. Med. Sci. 2011, 116, 187–199. [Google Scholar] [CrossRef]
- Sullivan, D.P.; Martin, P.R.; Boschen, M.J. Psychological Sleep Interventions for Migraine and Tension-Type Headache: A Systematic Review and Meta-Analysis. Sci. Rep. 2019, 9, 6411. [Google Scholar] [CrossRef]
- Silberstein, S.D.; Lipton, R.B.; Breslau, N. Migraine: Association with personality characteristics and psychopathology. Cephalalgia 1995, 15, 358–369. [Google Scholar] [CrossRef]
| Characteristics | Mean ± SD/Frequency (Percentage) |
|---|---|
| Headache clinical diagnosis | |
| Migraine with aura | 33 (24.1) |
| Migraine without aura | 91 (66.4) |
| Chronic-tension type headache | 13 (9.5) |
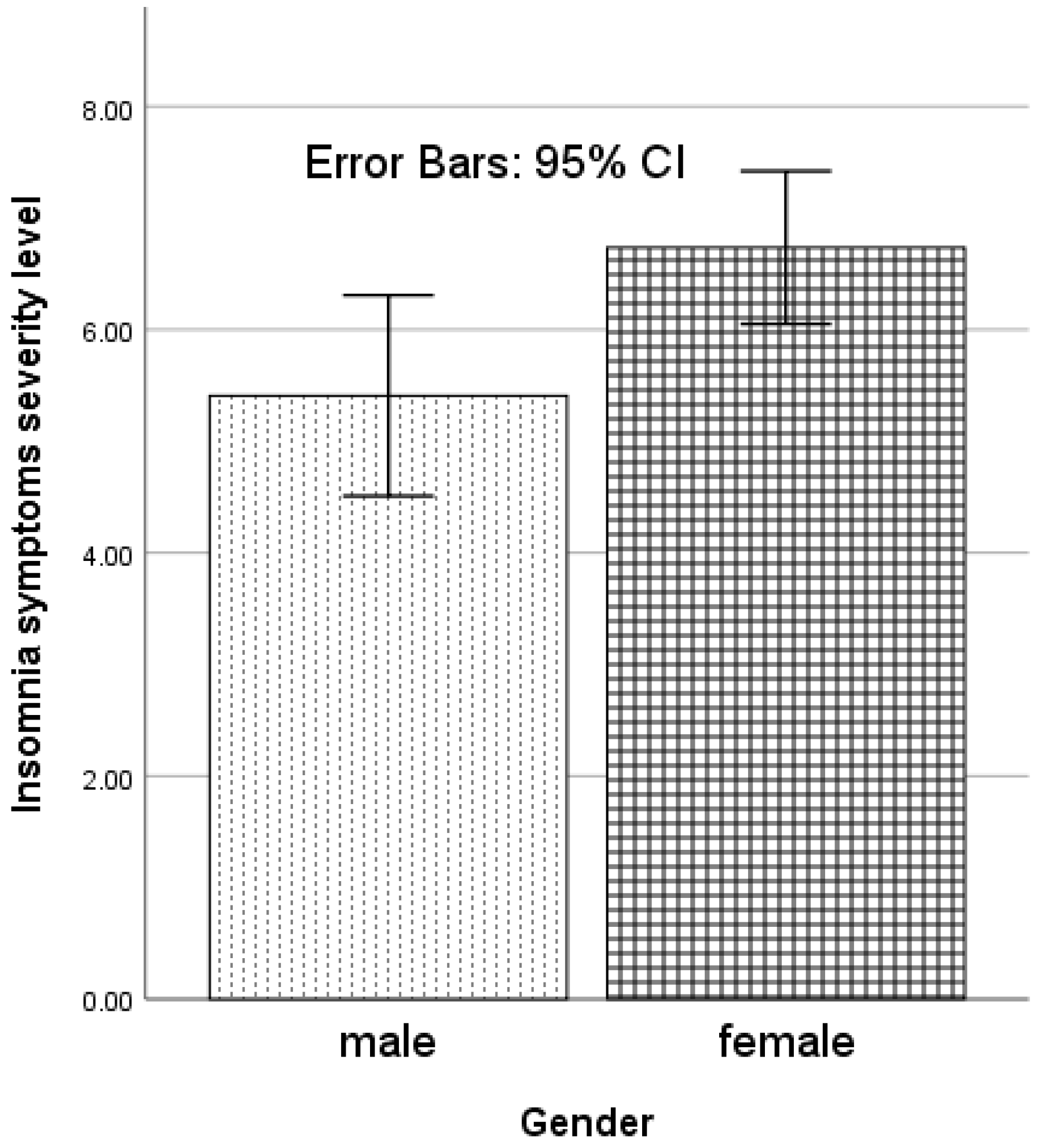
| Gender | |
| Male | 36 (26.3) |
| Female | 101 (73.7) |
| Age (year) | 27.3 ± 7.0 |
| Sports activity | |
| Yes | 60 (43.8) |
| No | 77 (56.2) |
| Currently under treatment for medical conditions | |
| Yes | 78 (56.9) |
| No | 58 (42.3) |
| Did not report | 1 (0.7) |
| Complaint of insufficient sleep | |
| No | 63 (46) |
| Yes | 74 (54) |
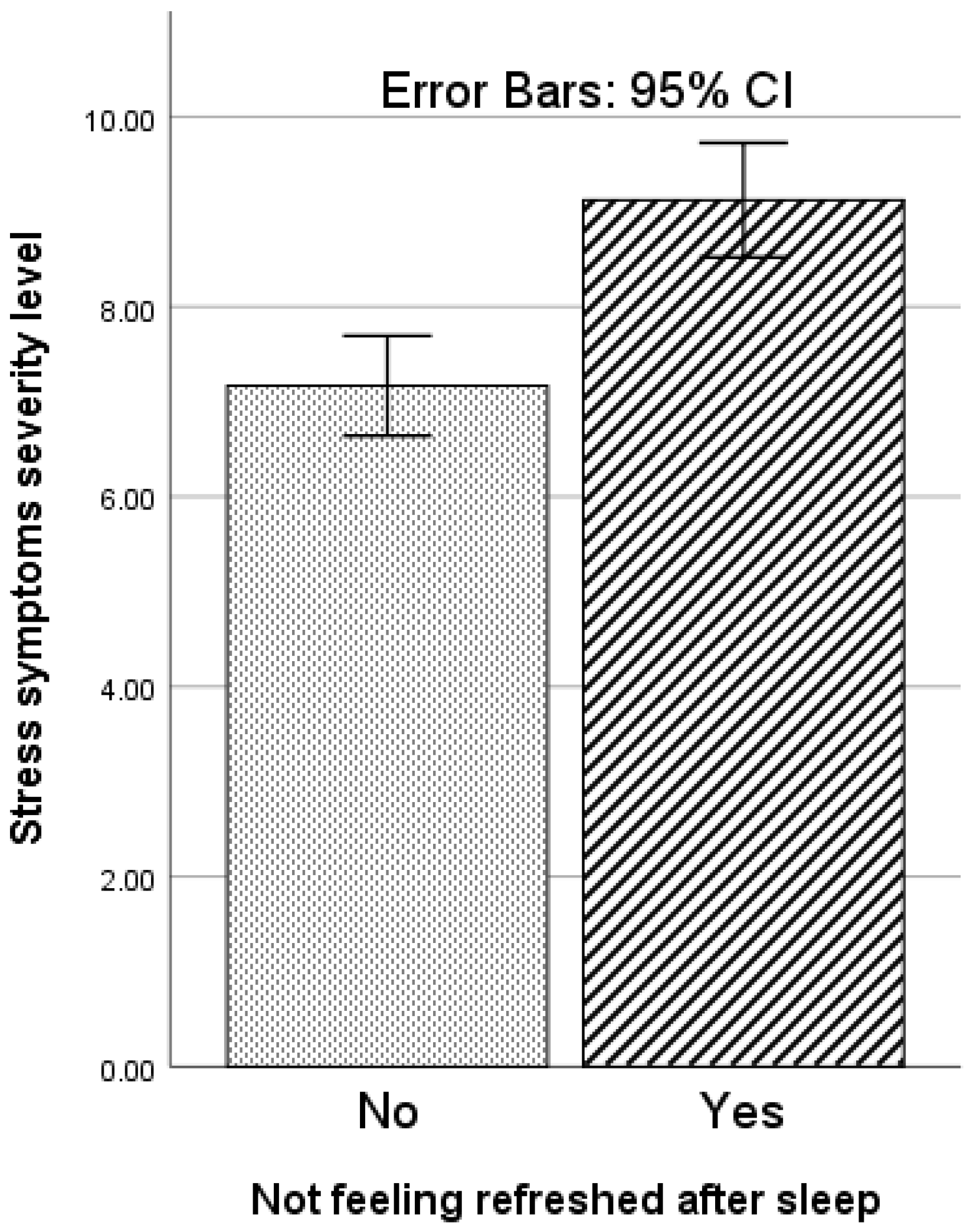
| Not feeling refreshed after sleep | |
| No | 72 (52.6) |
| Yes | 65 (47.4) |
| Traumatic incident in the family, e.g., death of a relative or close friend | |
| No | 68 (49.6) |
| Yes | 69 (50.4) |
| PSS-4 score | 8.1 ± 2.5 |
| Independent Variable | Beta Coefficient | Standard Error | T Values | p-Values | Model Unadjusted R2; Adjusted R2; p-Value |
|---|---|---|---|---|---|
| BMI | 0.19 | 0.11 | 1.97 | 0.05 | 0.17, 0.13, <0.01 |
| Age | 0.11 | 0.05 | 1.28 | 0.20 | |
| Gender | 0.25 | 0.70 | 2.81 | 0.01 | |
| Migraine with-without aura | 0.00 | 0.62 | 0.04 | 0.97 | |
| Sports activity | −0.06 | 0.58 | −0.77 | 0.44 | |
| History of head-neck injury | 0.05 | 0.58 | 0.62 | 0.54 | |
| Currently under treatment for other medical conditions | 0.16 | 0.61 | 1.91 | 0.06 | |
| Frequency of migraine medicine intake | 0.08 | 0.48 | 0.99 | 0.32 | |
| Intercept | −3.43 | 2.91 | −1.18 | 0.24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Quliti, K. Stress and Its Correlates in Migraine-Headache Patients with a Family History of Migraine. Behav. Sci. 2022, 12, 65. https://doi.org/10.3390/bs12030065
Al-Quliti K. Stress and Its Correlates in Migraine-Headache Patients with a Family History of Migraine. Behavioral Sciences. 2022; 12(3):65. https://doi.org/10.3390/bs12030065
Chicago/Turabian StyleAl-Quliti, Khalid. 2022. "Stress and Its Correlates in Migraine-Headache Patients with a Family History of Migraine" Behavioral Sciences 12, no. 3: 65. https://doi.org/10.3390/bs12030065
APA StyleAl-Quliti, K. (2022). Stress and Its Correlates in Migraine-Headache Patients with a Family History of Migraine. Behavioral Sciences, 12(3), 65. https://doi.org/10.3390/bs12030065





