A Systematic Review on the Role of Substance Consumption in Work-Related Road Traffic Crashes Reveals the Importance of Biopsychosocial Factors in Prevention
Abstract
:1. Introduction
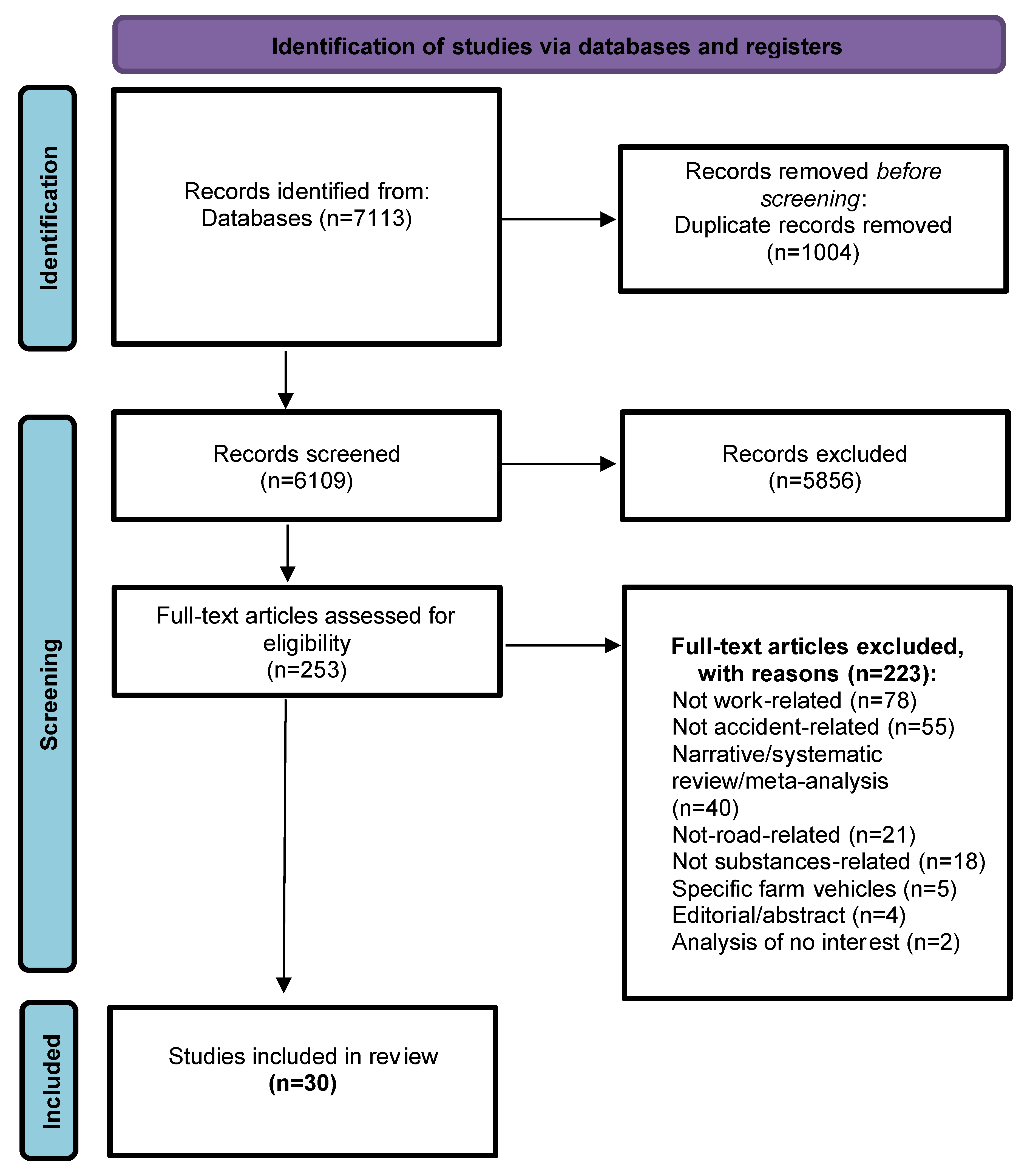
2. Methods
Study Design and Search Strategy
3. Results
3.1. Flow Diagram
3.2. Study Selection and Characteristics
3.3. Synthetized Findings
3.3.1. Impact of Alcohol in Work-Related Road Traffic Crashes
3.3.2. Impact of Recreational Drugs in Work-Related Road Traffic Crashes
3.3.3. Impact of Medicines in Work-Related Road Traffic Crashes
3.3.4. Synthetized Findings from Studies Reporting Aggregated Data of Interest
3.3.5. Impact of Psychological, Medical, and Social Factors in Work-Related Road Traffic Crashes
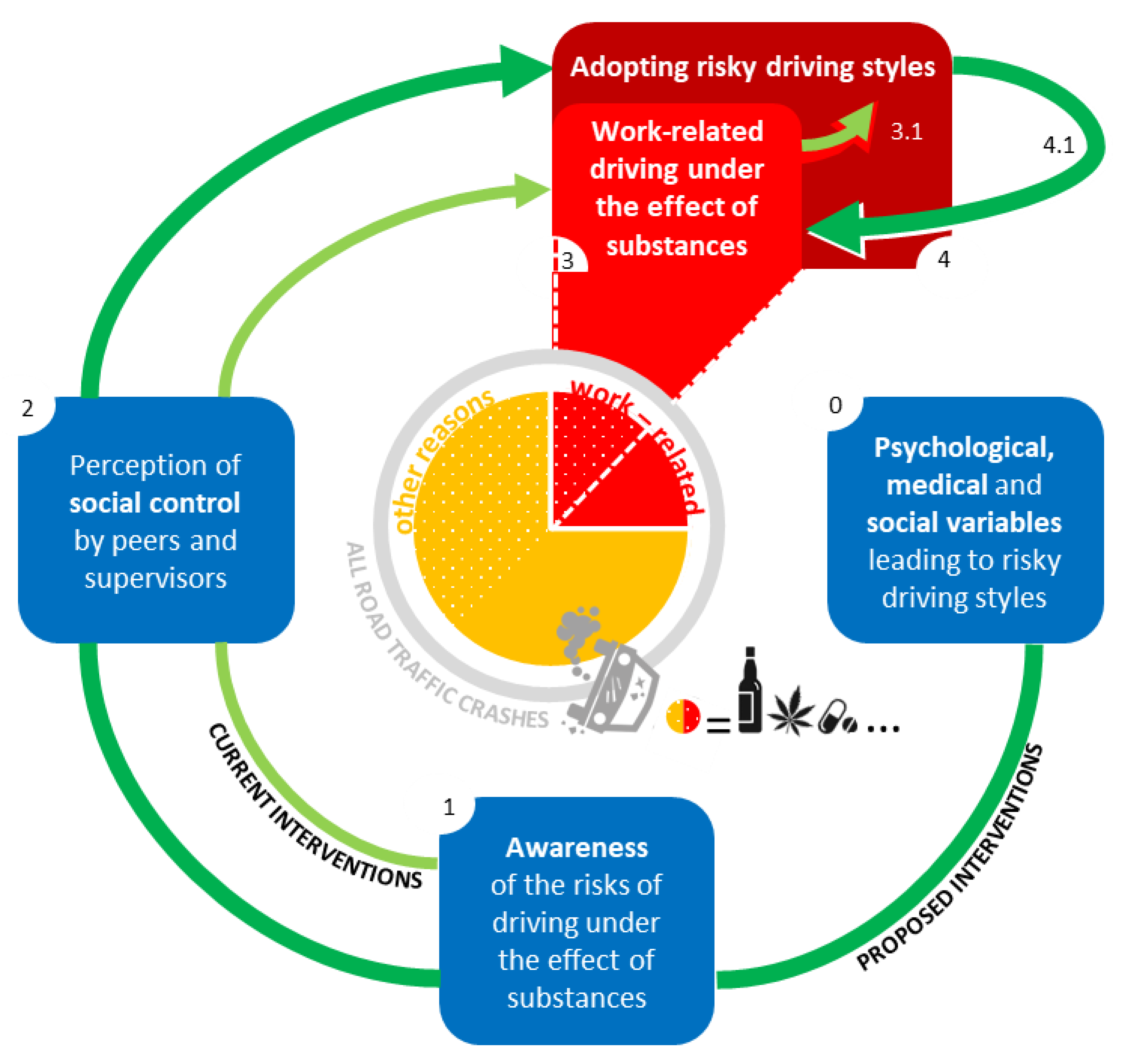
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- SafetyNet Final Activity Report. Available online: https://trimis.ec.europa.eu/sites/default/files/project/documents/20090206_184410_45024_SafetyNet_Final_Activity_Report_V3_Final.pdf (accessed on 24 January 2022).
- Adeloye, D.; Thompson, J.Y.; Akanbi, M.A.; Azuh, D.; Samuel, V.; Omoregbe, N.; Ayo, C.K. The burden of road traffic crashes, injuries and deaths in Africa: A systematic review and meta-analysis. Bull. World Health Organ. 2016, 94, 510–521A. [Google Scholar] [CrossRef] [Green Version]
- Robb, G.; Sultana, S.; Ameratunga, S.; Jackson, R. A systematic review of epidemiological studies investigating risk factors for work-related road traffic crashes and injuries. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2008, 14, 51–58. [Google Scholar] [CrossRef]
- Ricci, G.; Majori, S.; Mantovani, W.; Zappaterra, A.; Rocca, G.; Buonocore, F. Prevalence of alcohol and drugs in urine of patients involved in road accidents. J. Prev. Med. Hyg. 2008, 49, 89–95. [Google Scholar]
- Czeisler, M.É. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1049. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addict. Abingdon Engl. 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Bush, K. The AUDIT Alcohol Consumption Questions (AUDIT-C): An Effective Brief Screening Test for Problem Drinking. Arch. Intern. Med. 1998, 158, 1789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; Liu, J.; Liu, P.; Qi, Y. Analysis of Factors Contributing to the Severity of Large Truck Crashes. Entropy 2020, 22, 1191. [Google Scholar] [CrossRef]
- Smailović, E.; Lipovac, K.; Pešić, D.; Antić, B. Factors associated with driving under the influence of alcohol. Traffic Inj. Prev. 2019, 20, 343–347. [Google Scholar] [CrossRef]
- Boufous, S.; Williamson, A. Work-related traffic crashes: A record linkage study. Accid. Anal. Prev. 2006, 38, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Brodie, L.; Lyndal, B.; Elias, I.J. Heavy vehicle driver fatalities: Learning’s from fatal road crash investigations in Victoria. Accid. Anal. Prev. 2009, 41, 557–564. [Google Scholar] [CrossRef] [PubMed]
- McNeilly, B.; Ibrahim, J.E.; Bugeja, L.; Ozanne-Smith, J. The prevalence of work-related deaths associated with alcohol and drugs in Victoria, Australia, 2001–2006. Inj. Prev. J. Int. Soc. Child Adolesc. Inj. Prev. 2010, 16, 423–428. [Google Scholar] [CrossRef]
- Chu, H.-C. Assessing factors causing severe injuries in crashes of high-deck buses in long-distance driving on freeways. Accid. Anal. Prev. 2014, 62, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Holizki, T.; McDonald, R.; Gagnon, F. Patterns of underlying causes of work-related traumatic fatalities—Comparison between small and larger companies in British Columbia. Saf. Sci. 2015, 71, 197–204. [Google Scholar] [CrossRef]
- Karakus, A.; İdiz, N.; Dalgiç, M.; Uluçay, T.; Sincar, Y. Comparison of the effects of two legal blood alcohol limits: The presence of alcohol in traffic accidents according to category of driver in Izmir, Turkey. Traffic Inj. Prev. 2015, 16, 440–442. [Google Scholar] [CrossRef]
- Rudisill, T.M.; Menon, S.; Hendricks, B.; Zhu, M.; Smith, G.S. Differences between occupational and non-occupational-related motor vehicle collisions in West Virginia: A cross-sectional and spatial analysis. PLoS ONE 2019, 14, e0227388. [Google Scholar] [CrossRef]
- Sam, E.F.; Daniels, S.; Brijs, K.; Brijs, T.; Wets, G. Modelling public bus/minibus transport accident severity in Ghana. Accid. Anal. Prev. 2018, 119, 114–121. [Google Scholar] [CrossRef]
- Thygerson, S.M.; Merrill, R.M.; Cook, L.J.; Thomas, A.M. Comparison of factors influencing emergency department visits and hospitalization among drivers in work and nonwork-related motor vehicle crashes in Utah, 1999-2005. Accid. Anal. Prev. 2011, 43, 209–213. [Google Scholar] [CrossRef]
- Bourdeau, M.; Guibert, N.; Fort, E.; Boulogne, S.; Lagarde, E.; Charbotel, B. Medicine consumptions and occupational road risk. Accid. Anal. Prev. 2021, 158, 106202. [Google Scholar] [CrossRef]
- Chen, M.; Chen, P.; Gao, X.; Yang, C. Examining injury severity in truck-involved collisions using a cumulative link mixed model. J. Transp. Health 2020, 19, 100942. [Google Scholar] [CrossRef] [PubMed]
- French, M.T.; Gumus, G. Death on the job: The Great Recession and work-related traffic fatalities. Soc. Sci. Med. 2021, 280, 113979. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Yang, M.; Guo, Y.; Rasouli, S.; Gan, Z.; Ren, Y. Risk factors associated with truck-involved fatal crash severity: Analyzing their impact for different groups of truck drivers. J. Saf. Res. 2021, 76, 154–165. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.J.; Bambach, M.R.; Friswell, R. Work and non-work-related vehicle crashes: The contribution of risky driving practices. Saf. Sci. 2014, 68, 65–72. [Google Scholar] [CrossRef]
- Bacchieri, G.; Barros, A.J.D.; Dos Santos, J.V.; Gigante, D.P. Cycling to work in Brazil: Users profile, risk behaviors, and traffic accident occurrence. Accid. Anal. Prev. 2010, 42, 1025–1030. [Google Scholar] [CrossRef]
- Asefa, N.G.; Ingale, L.; Shumey, A.; Yang, H. Prevalence and factors associated with road traffic crash among taxi drivers in Mekelle town, northern Ethiopia, 2014: A cross sectional study. PLoS ONE 2015, 10, e0118675. [Google Scholar] [CrossRef]
- Bamberger, P.A.; Cohen, A. Driven to the Bottle: Work- Related Risk Factors and Alcohol Misuse Among Commercial Drivers. J. Drug Issues 2015, 45, 180–201. [Google Scholar] [CrossRef]
- Lambrechts, M.-C.; Vandersmissen, L.; Godderis, L. Alcohol and other drug use among Belgian workers and job-related consequences. Occup. Environ. Med. 2019, 76, 652–659. [Google Scholar] [CrossRef] [Green Version]
- Thiese, M.S.; Ott, U.; Robbins, R.; Effiong, A.; Murtaugh, M.; Lemke, M.R.; Deckow-Schaefer, G.; Kapellusch, J.; Wood, E.; Passey, D.; et al. Factors Associated With Truck Crashes in a Large Cross Section of Commercial Motor Vehicle Drivers. J. Occup. Environ. Med. 2015, 57, 1098–1106. [Google Scholar] [CrossRef]
- Papalia, L.; Goldoni, M.; Spaggiari, M.C.; Roscelli, F.; Corradi, M.; Mutti, A. Sleep disorders, risk of accidents and traffic accidents in a group of drivers of public transport. G. Ital. Med. Lav. Ergon. 2012, 34, 353–356. [Google Scholar]
- Konlan, K.D.; Doat, A.R.; Mohammed, I.; Amoah, R.M.; Saah, J.A.; Konlan, K.D.; Abdulai, J.A. Prevalence and Pattern of Road Traffic Accidents among Commercial Motorcyclists in the Central Tongu District, Ghana. Sci. World J. 2020, 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Poku, S.; Bandoh, D.; Kenu, E.; Kploanyi, E.; Addo- Lartey, A. Factors contributing to road crashes among commercial vehicle drivers in the Kintampo North Municipality, Ghana in 2017. Ghana Med. J. 2020, 54, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Gates, J.; Dubois, S.; Mullen, N.; Weaver, B.; Bédard, M. The influence of stimulants on truck driver crash responsibility in fatal crashes. Forensic Sci. Int. 2013, 228, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Wadsworth, E.J.K.; Moss, S.C.; Simpson, S.A.; Smith, A.P. A community based investigation of the association between cannabis use, injuries and accidents. J. Psychopharmacol. Oxf. Engl. 2006, 20, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Reguly, P.; Dubois, S.; Bédard, M. Examining the impact of opioid analgesics on crash responsibility in truck drivers involved in fatal crashes. Forensic Sci. Int. 2014, 234, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Khoshakhlagh, A.H.; Yazdanirad, S.; Laal, F.; Sarsangi, V. The relationship between illnesses and medical drug consumption with the occurrence of traffic accidents among truck and bus drivers in Tehran, Iran. Chin. J. Traumatol. Zhonghua Chuang Shang Za Zhi 2019, 22, 142–147. [Google Scholar] [CrossRef]
- Qi, Y.; Srinivasan, R.; Teng, H.; Baker, R. Analysis of the frequency and severity of rear-end crashes in work zones. Traffic Inj. Prev. 2013, 14, 61–72. [Google Scholar] [CrossRef]
- Liu, P.; Fan, W. Analyzing injury severity of rear-end crashes involving large trucks using a mixed logit model: A case study in North Carolina. J. Transp. Saf. Secur. 2020. [Google Scholar] [CrossRef]
- Monárrez-Espino, J.; Möller, J.; Berg, H.-Y.; Kalani, M.; Laflamme, L. Analgesics and road traffic crashes in senior drivers: An epidemiological review and explorative meta-analysis on opioids. Accid. Anal. Prev. 2013, 57, 157–164. [Google Scholar] [CrossRef]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef]
| Alcohol, Recreational Drugs, Medicines | Work | Road Traffic Crashes |
|---|---|---|
| alcohol | bus | accident |
| amphetamine | business driver | blameworthiness |
| analgesic | commercial driver | collision |
| antidepressant | commuting | crash |
| antihistamine | company car | crashes |
| anxiolytic | delivery worker | culpability |
| BAC | emergency vehicle | death |
| barbiturate | grey fleet | fatalities |
| benzodiazepine | heavy commercial vehicle | fatality |
| cannabinoid | itinere | incident |
| cannabis | job | injuries |
| cocaine | light commercial vehicle | injury |
| drink | lorry | near miss |
| drink-drive | occupational driver | road risk |
| drink-driving | private car | |
| drinking and driving | professional driver | |
| driving under the influence | public transport vehicle | |
| driving while intoxicated | taxi | |
| drug | trailer | |
| drunk | transport | |
| drunk driving | transportation | |
| drunk-driving | truck | |
| DUI | work | |
| DUID | workplace | |
| ethanol | work-place | |
| heroin | work-related | |
| hypnotic | ||
| intoxicated | ||
| medication | ||
| narcotic | ||
| opiate | ||
| opioid | ||
| polypharmacy | ||
| psychoactive | ||
| psychostimulant | ||
| psychotropic | ||
| sedative | ||
| stimulant | ||
| substance | ||
| tranquilizer |
| Parameters | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Participants | Healthy humans; Working population | Young people (<18 years) or older people (>65 years); Students, unemployed, or retired people; Subjects with chronic diseases. |
| Interventions | Use/abuse of alcohol during and/or near the use of vehicles on the road related to work; Use/abuse of psychotropic drugs during and/or near the use of vehicles on the road related to work; Use/abuse of drugs during and/or near the use of vehicles on the road related to work; | Use of very specific vehicles (e.g., trains, off-road vehicles, tractors, quads, etc.). |
| Comparisons | Any comparison; Stratification of the population according to age, gender, marital status, vehicle, years of experience, distance travelled, workload, night shifts, level of education, commuting. | Driving simulation studies. |
| Outcomes | Prevalence and characterization of alcohol/psychotropic drugs/drugs related traffic accidents during or close to working hours. | Injuries at work not related to alcohol/psychotropic drugs/drugs; Alcohol/psychotropic drugs/drugs related accidents that occurred outside or outside of working hours; Accidents related to alcohol/psychotropic drugs/drugs that did not occur on the road; Alcohol/psychotropic drugs/drugs related health problems; Use of alcohol/ psychotropic drugs/drugs AFTER an accident at work; Violence, homicide, suicide, or overdose in the workplace related to alcohol/psychotropic drugs/drugs use. |
| Study Design | Original studies: longitudinal, cross-sectional, randomized controlled, pre-post. | Case reports, narrative reviews, systematic reviews and meta-analyses; Lack of rigorous description of experimental methodology; |
| Study | Country (Region) | Time Period | Data Source | Study Design | Substance(s) Investigated | Consumption Assessment | Sample(s) Features | Positivity Rates (N) | Synthesis of Main Findings |
|---|---|---|---|---|---|---|---|---|---|
| Asefa et al., 2015 | Ethiopia (Mekelle) | 2014 | Recruitment from a representative population of taxi drivers | Cross-Sectional | Alcohol | Subjective (semi-structured questionnaire) | N = 712 taxi drivers | / | Self-reported history of alcohol use was an independent predictor of W-R RTC |
| Bacchieri et al., 2010 | Brazil (Pelotas) | 2006 | Recruitment from a representative population of cycling commuters | Cross-Sectional | Alcohol | Subjective (semi-structured survey) | N = 1133 cycling commuters | / | Riding right after alcohol consumption was a risk factor only if considered together with other extremely imprudent behaviors |
| Bamberger and Cohen, 2015 | Israel | 2015 | Recruitment of a random sample of employees from 8 transportation enterprises | Cross-Sectional | Alcohol | Subjective (AUDIT) | N = 227 commercial drivers (truck or bus) | / | Severity of alcohol misuse and number of accidents reported in the past year were significantly related |
| Boufous and Williamson, 2006 | Australia (New South Wales) | 1998–2002 | Traffic Accident Database System (TADS), Workers’ Compensation Scheme Statistics (WCSS) | Cross-Sectional | Alcohol | Objective (illegal alcohol level) | N = 13,124 drivers injured/dead from W-R RTC | 1.36 % (N = 179) | Over a 5-year period, an illegal alcohol level was found in a minority of workers driving on duty or during commuting |
| Chu, 2014 | Taiwan | 2005–2011 | Taiwan’s National Police Accident Reports | Cross-Sectional | Alcohol | Objective (BrAC) | N = 1286 freeway high-deck buses involved in RTC | 7.07 % (N = 91) | 70% (N = 64) of 91 drivers reported as drunk were involved in fatal or injurious RTC |
| Karakus et al., 2015 | Turkey (Izmir) | 2010–2011 | Izmir Forensic Medicine Group Presidency database | Retrospective Cross-Sectional | Alcohol | Objective (BAC) | N = 33 drivers involved in non-fatal W-R RTC | 3.03 % (N = 1) | Comparing two different BAC limit, the highest significantly increased risk of non-fatal accident; the lowest did not |
| Sam et al., 2018 | Ghana | 2011–2015 | National Accident Database | Cross-Sectional | Alcohol | Objective | N = 33,694 bus and minibus involved in RTC | 1.87% (N = 630) | Drivers who tested positive for alcohol were more likely to have a more severe RTC |
| Smailović et al., 2019 | Serbia | 2016 | National Traffic Accident Database | Cross-Sectional | Alcohol | Objective (BAC) | N = 3335 truck drivers involved in RTC N = 825 bus drivers involved in RTC | 32.6% (N = 1087) 42.67% (N = 352) | Among commercial drivers involved in W-R RTC, positivity to alcohol was found in about 1/3 |
| Thiese et al., 2015 | USA | 2015 | Recruitment of a random sample of truck drivers | Cross-Sectional | Alcohol | Subjective (computerized questionnaire) | N = 797 truck drivers | / | Alcohol use significantly increased the risk of W-R RTC among truck drivers |
| Thygerson et al., 2011 | USA (Utah) | 1999–2005 | Police crash reports and hospital inpatient and emergency department records | Cross-Sectional | Alcohol | Objective | N = 2330 workers who accessed the emergency department because of RTCN = 235 workers who were hospitalized because of RTC | 1% (N = 31) 3% (N = 7) | W-R RTC were associated with a higher severity of prognosis and with a higher fatality rate |
| Chen et al., 2020 | USA (Los Angeles) | 2010–2018 | US Statwide Integrated Traffic Records System (SWITRS) | Cumulative link mixed model | Alcohol | Objective | N = 21,258 truck drivers | 7.26% (N = 1544) | Among various risky driving behaviors, alcohol consumption independently and significantly increases severity of W-R RTC |
| Konlan et al., 2020 | Ghana (Adidome) | 2018 | Recruitment from a sample of commercial motorcyclists | Descriptive cross-sectional | Alcohol | Subjective (questionnaire) | N = 114 commercial motorcyclists | / | A history of alcohol use was associated with a higher prevalence of W-R RTC |
| French and Gumus, 2021 | USA and Puerto Rico | 2004–2012 | Fatality Analysis Reporting System (FARS) database | Longitudinal | Alcohol | Objective (BAC) | N = 1800 traffic fatalities | 2.1% (N = 38) | Alcohol was one of the factors increasing the number of fatalities due to W-R RTC during prosperous times |
| Mitchell et al., 2014 | Australia (New South Wales) | 2001–2011 | Admitted Patient Data Collection (APDC) | Retrospective analysis | Alcohol | Objective (BAC) | N = 3888 car drivers and motorcyclists involved in RTC | 1.77% (N = 69) | Risky behaviors (alcohol assumption) were more common in non-W-R journeys than W-R journeys |
| Poku et al., 2020 | Ghana (Kintampo North Municipality) | 2017 | Recruitment from a sample of commercial vehicle drivers from Driver and Vehicle Licensing Authority (DVLA) | Cross-Sectional | Alcohol | Subjective (semi-structured questionnaire) | N = 126 commercial drivers involved in at least one RTC | / | Alcohol use significantly increased the risk of W-R RTC among commercial drivers |
| Brodie et al., 2009 | Australia (Victoria) | 1999–2007 | Victorian State Coroner’s Office | Cross-Sectional | Alcohol, drugs (stimulants and cannabis) | Objective (BAC, toxicological screen) | N = 61 truck drivers killed in an RTC | Alcohol: 1.64 % (N = 1) Drugs: 16.3 % (N = 10) | Among heavy vehicle (≥ 4.5 tons) drivers, fatalities associated with consumption of drugs outnumbered those associated with consumption of alcohol |
| Holizki et al., 2015 | Canada (British Columbia) | 2003–2007 | Workers’ Compensation Board of British Columbia | Cross-Sectional | Alcohol, drugs | Objective (toxicological screen) | N = 71 workers’ compensation claims for traumatic fatalities | Alcohol: 5.6 % (N = 4) Drugs: 18.3 % (N = 13) Alcohol and Drugs: 8.45% (N = 6) | Injurious and fatal crashes were more frequently associated with drugs than with alcohol or with a combination of the two Fatality rates were higher for small businesses (9.7) than for larger businesses (2.7) |
| Lambrechts et al., 2019 | Belgium | 2015–2016 | Recruitment from a sample of the Belgian working population | Cross-Sectional | Alcohol, drugs | Subjective (AUDIT-C) | N = 4197 workers who used alcohol and 403 who used drugs, in the last year | / | Workers were found to consume alcohol more frequently than drugs; however, ratios were overturned when considering the prevalence of RTC |
| Rudisill et al., 2019 | USA (West Virginia) | 2000–2017 | Fatality Analysis Reporting System (FARS) database | Cross-Sectional | Alcohol, drugs | Objective (BAC, toxicological screen) | N = 209 workers fatally injured in RTC | Alcohol: 3.82 % (N = 8) Drugs: 13.39% (N = 28) | The odds of being involved in a work-related fatal collision were predicted by alcohol Alcohol and drugs are less used during work-related journeys, but this reduction is halved for drugs |
| Yuan, 2021 | USA and Puerto Rico | 2012–2016 | Fatality Analysis Reporting System (FARS) database | Partial Proportional Odds | Alcohol, drugs | Objective (BAC, toxicological screen) | N = 15,506 truck drivers | Alcohol: 2.4% (N = 372) Drugs: 1.2% (N = 186) | Among truck drivers with high risk of driving violations and high historical crash records, alcohol and drugs were significantly associated with the RTC severity |
| Li et al., 2020 | USA (Texas) | 2011–2015 | Texas Crash Records Information System (CRIS) | Mixed Logit Model | Alcohol, drugs | Objective | N = 85,184 large truck involved in RTC | Alcohol: 1.29% (N = 1103) Drugs: 0.6% (N = 305) | Consumption of alcohol was more frequent than that of drugs, but ratio between serious and non-serious RTC was higher for drugs (1:3) than alcohol (1:4). |
| Liu and Fan, 2020 | USA (North Carolina) | 2005–2013 | Highway Safety Information System (HSIS) | Mixed Logit Model | Alcohol, drugs | Objective | N = 7976 rear-end RTC involving large trucks | Alcohol and/or drugs: 0.45% (N = 36) | Driving under the influence of alcohol or drugs significantly increases the injury severity of RTC |
| Papalia et al., 2012 | Italy | 2011- 2012 | Recruitment from a sample of employees of an urban and suburban transport company | Cross-Sectional | Alcohol, medicines (antihistamines and benzodiazepines) | Subjective (questionnaire) | N = 253 workers of an urban/extra-urban transport company | / | Use of antihistamines and benzodiazepines was found to significantly correlate with the risk of RTC |
| Bourdeau et al., 2021 | France | 2005–2015 | Police reports (PRs)Bulletins d’Analyse des Accidents Corporels (BAAC)Système National d’Informations Inter Régimes de l’Assurance Maladie | Logistic Regression model | Alcohol, medicines (10 classes) | Objective (medicines prescriptions) | N = 21,490 workers involved in an injurious RTC during a W-R mission N = 43,012 commuters involved in an injurious RTC | 15% (N = 3213) 17.9% (N = 7689) | Among the ten classes of medicines investigated, the higher risk of W-R RTC was associated with the assumption of: antiepileptics, psycholeptics or psychoanaleptics for the commuters; antiepileptics, other nervous system drugs or psychoanaleptics for the drivers on a work-related mission. |
| McNeilly et al., 2010 | Australia (Victoria) | 2001–2006 | National Coroner’sInformation System database | Retrospective, observational, cross-sectional | Alcohol, drugs, and medicines | Objective (BAC, toxicological screen) | N = 64 worker and commuter deaths with positive toxicological screening | Alcohol: 14% (N = 9) Drugs: 21.33 % (N = 16) Medicines: 43.75% (N = 28) | Medicines are the substances more frequently associated with fatal W-R RTC |
| Qi et al., 2013 | USA (New York State) | 1994–2001 | New York StateStatewide Work Zone Safety Inspection Program database | Cross-Sectional | Alcohol, drugs, and medicines | Objective | N = 2481 rear-end RTC | Alcohol, drugs, and medicines: 1.45% (N = 36) | Consumption of substances was associated with higher severity of W-R RTC |
| Gates et al., 2013 | USA (Puerto Rico and D.C.) | 1993–2008 | Fatality Analysis Reporting System (FARS) database | Cross-sectional | Drugs (stimulant use) | Objective (toxicological screen) | N = 10,190 truck drivers involved in fatal RTC and tested for stimulant use | 3.7 % (N = 372) | The use of stimulant was found to increase the risk of performing an unsafe driving action in a fatal crash (AOR = 1.78; 95%CI = 1.41–2.26) |
| Wadsworth et al., 2006 | U.K. (Wales) | 2001 | Recruitment of a random sample from the electoral registers of Cardiff and Merthyr Tydfil | Cross-Sectional | Drugs (Cannabis) | Subjective (postal questionnaire survey) | N = 2801 W-R RTC | / | Cannabis use tripled the risk of injury |
| Khoshakhlagh et al., 2019 | Iran (Teheran) | 2011–2016 | Recruitment from a random sample of Iranian truck and bus drivers (selected during annual healthy job visit) | Cross-Sectional | Medicines | Subjective (Specially designed questionnaire) | N = 323 truck and bus drivers | / | The consumption of two medicines significantly increased the incidence of RTC: Gemfibrozil (used to reduce cholesterol) and Glibenclamide (used to treat type 2 diabetes) |
| Reguly et al., 2014 | USA (Puerto Rico and D.C.) | 1993–2008 | Fatality Analysis Reporting System (FARS) database | Case-control cross-sectional | Medicines (opioids analgesics) | Objective (toxicological screen) | N = 10,190 truck drivers tested for drugs | 1.03 % (N= 105) | Male truck drivers using opioid analgesics had greater odds of committing unsafe driver actions |
| Substances | Weighted Average 95%CI | Range (Minimum-Maximum) |
|---|---|---|
| Alcohol | 3.02% (2.21–4.04%) | 1.29–42.67% |
| Drugs | 0.84% (0.30–1.84%) | 0.6–21.33% |
| Medicines | 14.8% (10.74–19.8%) | 1.03–43.75% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frumento, S.; Bufano, P.; Zaccaro, A.; Poma, A.M.; Persechino, B.; Gemignani, A.; Laurino, M.; Menicucci, D. A Systematic Review on the Role of Substance Consumption in Work-Related Road Traffic Crashes Reveals the Importance of Biopsychosocial Factors in Prevention. Behav. Sci. 2022, 12, 23. https://doi.org/10.3390/bs12020023
Frumento S, Bufano P, Zaccaro A, Poma AM, Persechino B, Gemignani A, Laurino M, Menicucci D. A Systematic Review on the Role of Substance Consumption in Work-Related Road Traffic Crashes Reveals the Importance of Biopsychosocial Factors in Prevention. Behavioral Sciences. 2022; 12(2):23. https://doi.org/10.3390/bs12020023
Chicago/Turabian StyleFrumento, Sergio, Pasquale Bufano, Andrea Zaccaro, Anello Marcello Poma, Benedetta Persechino, Angelo Gemignani, Marco Laurino, and Danilo Menicucci. 2022. "A Systematic Review on the Role of Substance Consumption in Work-Related Road Traffic Crashes Reveals the Importance of Biopsychosocial Factors in Prevention" Behavioral Sciences 12, no. 2: 23. https://doi.org/10.3390/bs12020023
APA StyleFrumento, S., Bufano, P., Zaccaro, A., Poma, A. M., Persechino, B., Gemignani, A., Laurino, M., & Menicucci, D. (2022). A Systematic Review on the Role of Substance Consumption in Work-Related Road Traffic Crashes Reveals the Importance of Biopsychosocial Factors in Prevention. Behavioral Sciences, 12(2), 23. https://doi.org/10.3390/bs12020023









