Dynamics of Physiological, Biochemical and Psychological Markers during Single Session of Virtual Reality-Based Respiratory Biofeedback Relaxation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Procedure
2.3. Measures
2.3.1. Perceived Stress and Anxiety
2.3.2. Mood Status, Fatigue, and Strain
2.3.3. Salivary Cortisol and Cortisone Levels
2.3.4. Heart Rate, Respiratory Rate, and Heart Rate Variability Measurement
2.3.5. Galvanic Skin Response
2.4. Statistical Analysis
3. Results
3.1. Perceived Stress and Anxiety Levels in the Study Sample
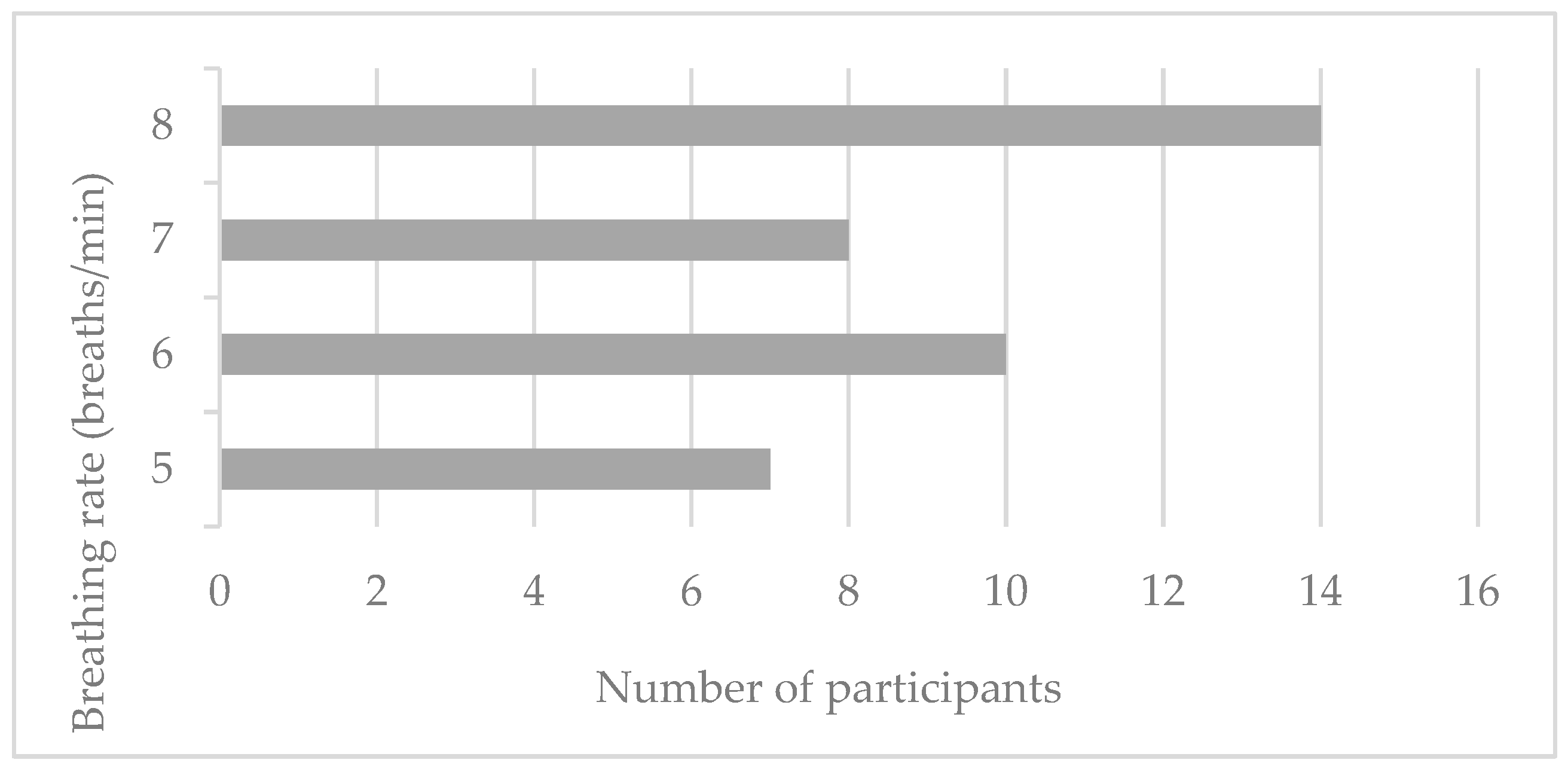
3.2. Determination of the Most Suitable Breathing Rate for Each Individual
3.3. Influence of Relaxation Session on Psychological, Physiological, and Biochemical Stress Indicators
3.4. Dynamics of Physiological Stress Measures during Relaxation Session
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. The Instructions Provided to the Subjects Prior the Relaxation Session
References
- Tan, S.; Yip, A. Hans Selye (1907–1982): Founder of the stress theory. Singap. Med. J. 2018, 59, 170–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guilliams, T.; Edwards, L. Chronic Stress and the HPA Axis: Clinical Assessment and Therapeutic Consideration. Standard 2010, 9, 1–12. [Google Scholar]
- Keller, A.; Litzelman, K.; Wisk, L.E.; Maddox, T.; Cheng, E.R.; Creswell, P.D.; Witt, W.P. Does the perception that stress affects health matter? The association with health and mortality. Health Psychol. 2012, 31, 677–684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McEwen, B.; Sapolsky, R. Stress and Your Health. J. Clin. Endocrinol. Metab. 2006, 91, E2. [Google Scholar] [CrossRef] [Green Version]
- Varvogli, L.; Darviri, C. Stress Management Techniques: Evidence-based procedures that reduce stress and promote health. Health Sci. J. 2011, 5, 74–89. [Google Scholar]
- Frank, D.L.; Khorshid, L.; Kiffer, J.F.; Moravec, C.S.; McKee, M.G. Biofeedback in medicine: Who, when, how and why? Ment. Health Fam. Med. 2010, 7, 85–91. [Google Scholar]
- Schwartz, M.S. A New Improved Universally Accepted Official Definition of Biofeedback: Where Did It Come From? Why? Who Did It? Who Is It for? What’s Next? Biofeedback 2010, 38, 88–90. [Google Scholar] [CrossRef]
- Nestoriuc, Y.; Martin, A.; Rief, W.; Andrasik, F. Biofeedback Treatment for Headache Disorders: A Comprehensive Efficacy Review. Appl. Psychophysiol. Biofeedback 2008, 33, 125–140. [Google Scholar] [CrossRef]
- McGrady, A. The effects of biofeedback in diabetes and essential hypertension. Cleve Clin. J. Med. 2010, 77, S68–S71. [Google Scholar] [CrossRef] [Green Version]
- Taghizadeh, N.; Eslaminejad, A.; Raoufy, M.R. Protective effect of heart rate variability biofeedback on stress-induced lung function impairment in asthma. Respir. Physiol. Neurobiol. 2019, 262, 49–56. [Google Scholar] [CrossRef]
- Reiner, R. Integrating a Portable Biofeedback Device into Clinical Practice for Patients with Anxiety Disorders: Results of a Pilot Study. Appl. Psychophysiol. Biofeedback 2008, 33, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Schoenberg, P.L.; David, A.S. Biofeedback for psychiatric disorders: A systematic review. Appl. Psychophysiol. Biofeedback 2014, 39, 109–135. [Google Scholar] [CrossRef] [PubMed]
- Kudo, N.; Shinohara, H.; Kodama, H. Heart Rate Variability Biofeedback Intervention for Reduction of Psychological Stress During the Early Postpartum Period. Appl. Psychophysiol. Biofeedback 2014, 39, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Funk, M.; Hu, J.; Wang, Q.; Feijs, L. Biofeedback for Everyday Stress Management: A Systematic Review. Front. ICT 2018, 5, 1–23. [Google Scholar] [CrossRef] [Green Version]
- Zhu, Q.; Kong, X.; Xie, Y. The influence of biofeedback on respiratory training effect. In Proceedings of the 2012 International Conference on Systems and Informatics (ICSAI2012), Yantai, China, 19–20 May 2012. [Google Scholar] [CrossRef]
- Beauchaine, T.P. Respiratory sinus arrhythmia: A transdiagnostic biomarker of emotion dysregulation and psychopathology. Curr. Opin. Psychol. 2015, 3, 43–47. [Google Scholar] [CrossRef] [Green Version]
- Lehrer, P.M.; Vaschillo, E.; Vaschillo, B.; Lu, S.-E.; Eckberg, D.L.; Edelberg, R.; Shih, W.J.; Lin, Y.; Kuusela, T.A.; Tahvanainen, K.U.O.; et al. Heart Rate Variability Biofeedback Increases Baroreflex Gain and Peak Expiratory Flow. Psychosom. Med. 2003, 65, 796–805. [Google Scholar] [CrossRef] [Green Version]
- Patron, E.; Benvenuti, S.M.; Favretto, G.; Valfrè, C.; Bonfà, C.; Gasparotto, R.; Palomba, D. Biofeedback Assisted Control of Respiratory Sinus Arrhythmia as a Biobehavioral Intervention for Depressive Symptoms in Patients After Cardiac Surgery: A Preliminary Study. Appl. Psychophysiol. Biofeedback 2012, 38, 1–9. [Google Scholar] [CrossRef]
- Munafo, M.; Patron, E.; Palomba, D. Improving managers’ psychophysical well-being: Effectiveness of respiratory sinus arrhythmia biofeedback. Appl. Psychophysiol. Biofeedback 2016, 41, 129–139. [Google Scholar] [CrossRef]
- Deschodt-Arsac, V.; Lalanne, R.; Spiluttini, B.; Bertin, C.; Arsac, L.M. Effects of heart rate variability biofeedback training in athletes exposed to stress of university examinations. PLoS ONE 2018, 13, e0201388. [Google Scholar] [CrossRef] [Green Version]
- Gromala, D.; Tong, X.; Choo, A.; Karamnejad, M.; Shaw, C.D. The Virtual Meditative Walk. In Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems—CHI ’15, Seoul, Republic of Korea, 18–23 April 2015. [Google Scholar] [CrossRef]
- Van Rooij, M.; Lobel, A.; Harris, O.; Smit, N.; Granic, I. DEEP: A Biofeedback Virtual Reality Game for Children At-risk for Anxiety. In Proceedings of the 2016 CHI Conference Extended Abstracts on Human Factors in Computing Systems—CHI EA ’16, San Jose, CA, USA, 7–12 May 2016. [Google Scholar] [CrossRef] [Green Version]
- Blum, J.; Rockstroh, C.; Göritz, A.S. Development and pilot test of a virtual reality respiratory biofeedback approach. Appl. Psychophysiol. Biofeedback 2020, 45, 153–163. [Google Scholar] [CrossRef]
- Rockstroh, C.; Blum, J.; Göritz, A.S. Virtual reality in the application of heart rate variability biofeedback. Int. J. Hum. Comput. Stud. 2019, 130, 209–220. [Google Scholar] [CrossRef]
- Lehrer, P.; Vaschillo, B.; Zucker, T.; Graves, J.; Katsamanis, M.; Aviles, M.; Wamboldt, F. Protocol for Heart Rate Variability Biofeedback Training. Biofeedback 2013, 41, 98–109. [Google Scholar] [CrossRef] [Green Version]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.; Jacobs, G. State-Trait Anxiety Inventory for Adults Manual; Mind Garden: Redwood City, CA, USA, 1983. [Google Scholar]
- Mazgelytė, E.; Chomentauskas, G.; Dereškevičiūtė, E.; Rekienė, V.; Jakaitienė, A.; Petrėnas, T.; Songailienė, J.; Utkus, A.; Kučinskienė, A.Z.; Karčiauskaitė, D. Association of salivary steroid hormones and their ratios with time-domain heart rate variability indices in healthy individuals. J. Med. Biochem. 2021, 40, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Bartels, R.; Neumamm, L.; Peçanha, T.; Carvalho, A.R.S. SinusCor: An advanced tool for heart rate variability analysis. BioMed. Eng. Online 2017, 16, 110. [Google Scholar] [CrossRef] [PubMed]
- Berntson, G.G.; Bigger, T., Jr.; Eckberg, D.L.; Grossman, P.; Kaufmann, P.G.; Malik, M.; Nagaraja, H.N.; Porges, S.W.; Saul, P.J.; Stone, P.H.; et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology 1997, 34, 623–648. [Google Scholar] [CrossRef]
- Shaffer, F.; Meehan, Z.M. A practical guide to resonance frequency assessment for heart rate variability biofeedback. Front. Neurosci. 2020, 14, 570400. [Google Scholar] [CrossRef]
- Zaccaro, A.; Piarulli, A.; Laurino, M.; Garbella, E.; Menicucci, D.; Neri, B.; Gemignani, A. How breath-control can change your life: A systematic review on psycho-physiological correlates of slow breathing. Front. Hum. Neurosci. 2018, 12, 353. [Google Scholar] [CrossRef] [Green Version]
- Lin, I.M.; Wang, S.Y.; Fan, S.Y.; Peper, E.; Chen, S.P.; Huang, C.Y. A single session of heart rate variability biofeedback produced greater increases in heart rate variability than autogenic training. Appl. Psychophysiol. Biofeedback 2020, 45, 343–350. [Google Scholar] [CrossRef]
- Van Diest, I.; Verstappen, K.; Aubert, A.E.; Widjaja, D.; Vansteenwegen, D.; Vlemincx, E. Inhalation/exhalation ratio modulates the effect of slow breathing on heart rate variability and relaxation. Appl. Psychophysiol. Biofeedback 2014, 39, 171–180. [Google Scholar] [CrossRef] [Green Version]
- Tinga, A.M.; Nyklíček, I.; Jansen, M.P.; de Back, T.T.; Louwerse, M.M. Respiratory Biofeedback Does Not Facilitate Lowering Arousal in Meditation Through Virtual Reality. Appl. Psychophysiol. Biofeedback 2018, 44, 51–59. [Google Scholar] [CrossRef]
- Lemaire, J.B.; Wallace, J.E.; Lewin, A.M.; de Grood, J.; Schaefer, J.P. The effect of a biofeedback-based stress management tool on physician stress: A randomized controlled clinical trial. Open Med. 2011, 5, 154–163. [Google Scholar]
| Variable | Mean ± SD or N (%) |
|---|---|
| Gender | |
| Women | 28 (71.79) |
| Men | 11 (28.21) |
| Age (years) | 37.28 ± 6.98 |
| BMI (kg/m2) | 22.64 ± 2.97 |
| Smoking status | |
| Non-smoker | 33 (84.62) |
| Moderate smoker | 5 (12.82) |
| Heavy smoker | 1 (2.56) |
| Exposure to environmental tobacco smoke | |
| No | 38 (97.44) |
| Yes | 1 (2.56) |
| Alcohol consumption | |
| No | 3 (7.69) |
| Yes (sometimes) | 36 (92.31) |
| Physical activity at work | |
| Inactive | 31 (79.49) |
| Active | 8 (20.51) |
| Leisure time physical activity | |
| Inactive | 6 (15.38) |
| Active | 33 (84.62) |
| Variable | Pre-Session (Mean ± SD) | Post-Session (Mean ± SD) | p-Value | Effect Size (Cohen‘s d) |
|---|---|---|---|---|
| Strain | 3.85 ± 1.06 | 4.38 ± 0.88 | 0.001 | 0.556 (moderate) |
| Fatigue | 3.41 ± 1.14 | 4.13 ± 0.95 | <0.001 | 0.668 (moderate) |
| Mood | 3.64 ± 1.01 | 4.00 ± 1.08 | 0.037 | 0.346 (small) |
| Variable | Pre-Session (Median (IQR)) | Post-Session (Median (IQR)) | p-Value | Effect Size (Cohen’s d or r) |
|---|---|---|---|---|
| Cortisol (ng/mL) | 2.24 (2.29) | 1.85 (1.24) | 0.002 | r = 0.469 (moderate) |
| Cortisone (ng/mL) | 11.79 (6.51) | 11.68 (6.86) | 0.166 | r = 0.233 (small) |
| Cortisol + cortisone (ng/mL) | 13.88 (9.62) | 13.58 (7.97) | 0.051 | r = 0.291 (small) |
| Cortisol/cortisone | 0.19 ±0.05 | 0.16 ±0.05 | 0.008 | d = 0.460 (small) |
| Variable | Pre-Session (Mean ± SD or Median (IQR)) | Post-Session (Mean ± SD or Median (IQR)) | p-Value | Effect Size (Cohen’s d or r) |
|---|---|---|---|---|
| HR (bpm) | 70.9 ± 6.75 | 69.35 ± 5.68 | 0.002 | d = 0.507 (moderate) |
| RR (bpm) | 7.5 (1.5) | 7 (2) | 0.017 | r = 0.430 (moderate) |
| pNN50 (%) | 23.63 ± 13.69 | 22.93 ± 13.95 | 0.604 | d = 0.0838 (negligible) |
| RMSSD (ms) | 42.97 ± 13.02 | 43.95 ± 15.46 | 0.984 | d = 0.0321(negligible) |
| GSR | 251.76 ± 123.99 | 320.38 ± 163.39 | <0.001 | d = 0.795 (moderate) |
| Variable | Percent Change (Mean ± SD or Median (IQR)) | p-Value | Effect Size (Cohen’s d) |
|---|---|---|---|
| Cortisol (%) | −24.00 ± 24.85 | <0.001 | 0.966 (large) |
| Cortisone (%) | −10.11 ± 24.44 | 0.018 | 0.413 (small) |
| Cortisol + cortisone (%) | −11.70 ± 24.10 | 0.006 | 0.486 (small) |
| Cortisol/cortisone (%) | −12.06 ± 25.54 | 0.008 | 0.472 (small) |
| HR (%) | −2.23 ± 4.30 | 0.002 | 0.519 (moderate) |
| Respiratory rate (%) | −3.59 ± 6.36 | 0.002 | 0.564 (moderate) |
| pNN50 (%) | −2.52 ± 30.35 | 0.637 | 0.0830 (negligible) |
| RMSSD (%) | −0.25 ± 14.82 | 0.920 | 0.0166 (negligible) |
| GSR (%) | 22.96 ± 27.31 | <0.001 | 0.841 (large) |
| Variable | Estimate | SE | p-Value |
|---|---|---|---|
| Heart rate (bpm) | |||
| Intercept | 70.99 | 1.03 | |
| Time | −0.14 | 0.03 | <0.001 |
| Respiratory rate (bpm) | |||
| Intercept | 6.75 | 0.23 | |
| Time | 0.02 | 0.01 | 0.108 |
| Heart rate variability: RMSSD (ms) | |||
| Intercept | 43.59 | 2.23 | |
| Time | 7.61×10−4 | 0.08 | 0.992 |
| Heart rate variability: pNN50 (%) | |||
| Intercept | 23.99 | 2.04 | |
| Time | −0.14 | 0.08 | 0.071 |
| GSR | |||
| Intercept | 257.46 | 23.62 | |
| Time | 5.89 | 0.48 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mazgelytė, E.; Zagorskaja, J.; Dereškevičiūtė, E.; Petrėnas, T.; Kaminskas, A.; Songailienė, J.; Utkus, A.; Chomentauskas, G.; Karčiauskaitė, D. Dynamics of Physiological, Biochemical and Psychological Markers during Single Session of Virtual Reality-Based Respiratory Biofeedback Relaxation. Behav. Sci. 2022, 12, 482. https://doi.org/10.3390/bs12120482
Mazgelytė E, Zagorskaja J, Dereškevičiūtė E, Petrėnas T, Kaminskas A, Songailienė J, Utkus A, Chomentauskas G, Karčiauskaitė D. Dynamics of Physiological, Biochemical and Psychological Markers during Single Session of Virtual Reality-Based Respiratory Biofeedback Relaxation. Behavioral Sciences. 2022; 12(12):482. https://doi.org/10.3390/bs12120482
Chicago/Turabian StyleMazgelytė, Eglė, Julija Zagorskaja, Edita Dereškevičiūtė, Tomas Petrėnas, Andrius Kaminskas, Jurgita Songailienė, Algirdas Utkus, Gintaras Chomentauskas, and Dovilė Karčiauskaitė. 2022. "Dynamics of Physiological, Biochemical and Psychological Markers during Single Session of Virtual Reality-Based Respiratory Biofeedback Relaxation" Behavioral Sciences 12, no. 12: 482. https://doi.org/10.3390/bs12120482
APA StyleMazgelytė, E., Zagorskaja, J., Dereškevičiūtė, E., Petrėnas, T., Kaminskas, A., Songailienė, J., Utkus, A., Chomentauskas, G., & Karčiauskaitė, D. (2022). Dynamics of Physiological, Biochemical and Psychological Markers during Single Session of Virtual Reality-Based Respiratory Biofeedback Relaxation. Behavioral Sciences, 12(12), 482. https://doi.org/10.3390/bs12120482





