Psychopathology Changes in Alzheimer’s Disease
Abstract
1. Introduction
Aim of the Study
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Socio-Demographic Questionnaire (e.g., Age, Schooling)
2.2.2. Mini Mental State Examination (MMSE)
2.2.3. The Personality Diagnostic Questionnaire (PDQ–4+)
2.3. Procedure
2.3.1. AD Group and AD Group Informants
2.3.2. Control Group and Control Group Informants
2.4. Data Analysis
3. Results
3.1. Current and Premorbid Psychopathology Studies
3.2. Psychopathology Changes Study
4. Discussion
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Terracciano, A.; Bilgel, M.; Aschwanden, D.; Luchetti, M.; Stephan, Y.; Moghekar, A.R.; Wong, D.F.; Ferrucci, L.; Sutin, A.R.; Resnick, S.M. Personality associations with amyloid and tau: Results from the baltimore longitudinal study of aging and meta-analysis. Biol. Psychiatry 2022, 15, 359–369. [Google Scholar] [CrossRef] [PubMed]
- Gahr, M.; Connemann, B.; Schonfeldt-Lecuona, C. Behavioural problems and personality change related to cerebral amyloid angiopathy. Psychiatr. Prax. 2012, 39, 410–413. [Google Scholar] [PubMed]
- Pocnet, C.; Rossier, J.; Antonietti, J.; von Gunten, A. Personality features and cognitive level in patients at an early stage of Alzheimer´s disease. Pers. Individ. Differ. 2013, 54, 174–179. [Google Scholar] [CrossRef]
- Tautvydaitė, D.; Antonietti, J.P.; Henry, H.; von Gunten, A.; Popp, J. Relations between personality changes and cerebrospinal fluid biomarkers of Alzheimer’s disease pathology. Psychiatry Res. 2017, 90, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Caselli, R.J. Midlife personality and risk of Alzheimer disease and distress: A 38-year follow-up. Neurology 2015, 85, 298. [Google Scholar] [CrossRef] [PubMed]
- Cipriani, G.; Borin, G.; Del Debbio, A.; Di Fiorino, M. Personality and dementia. J. Nerv. Ment. Dis. 2015, 203, 210–214. [Google Scholar] [CrossRef]
- Duberstein, P.R.; Chapman, B.P.; Tindle, H.A.; Sink, K.M.; Bamonti, P.; Robbins, J.; Jerant, A.F.; Franks, P. Personality and risk for Alzheimer’s disease in adults 72 years of age and older: A 6-year follow-up. Psychol. Aging 2010, 26, 351–362. [Google Scholar] [CrossRef]
- Duchek, J.M.; Balota, D.A.; Storandt, M.; Larsen, R. The power of personality in discriminating between healthy aging and early-stage Alzheimer’s disease. J. Gerontol. B Psychol. Sci. Soc. Sci. 2007, 62, 353–361. [Google Scholar] [CrossRef]
- Henriques-Calado, J.; Duarte-Silva, M.E.; Sousa Ferreira, A. Depressive vulnerability in women with Alzheimer’s disease: Relationship with personality traits and abnormal personality dimensions. J. Affect. Disord. 2018, 241, 182–191. [Google Scholar] [CrossRef]
- Henriques-Calado, J.; Duarte-Silva, M.E.; Sousa Ferreira, A. Anaclitic personality dimension in women with Alzheimer’s disease: Comparison with control groups. Pers. Individ. Differ. 2017, 109, 166–171. [Google Scholar] [CrossRef]
- Henriques-Calado, J.; Duarte-Silva, M.E.; Sousa Ferreira, A. Personality traits in women with Alzheimer’s disease: Comparisons with control groups with the NEO-FFI. Pers. Individ. Differ. 2016, 101, 341–347. [Google Scholar] [CrossRef]
- Osborne, H.; Simpson, J.; Stokes, G. The relationship between pre-morbid personality and challenging behaviour in people with dementia: A systematic review. Aging Ment. Health 2010, 14, 503–515. [Google Scholar] [CrossRef] [PubMed]
- Pocnet, C.; Rossier, J.; Antonietti, J.; von Gunten, A. Personality changes in patients with beginning Alzheimer disease. Can. J. Psychiatry 2011, 56, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Pocnet, C.; Rossier, J.; Antonietti, J.; von Gunten, A. Personality traits and behavioral and psychological symptoms in patients at an early stage of Alzheimer´s disease. Int. J. Geriatr. Psychiatry 2012, 28, 276–283. [Google Scholar] [CrossRef]
- Terracciano, A.; Iacono, D.; O’Brien, R.J.; Troncoso, J.C.; An, Y.; Sutin, A.; Ferrucci, L.; Zonderman, A.B.; Resnick, S.M. Personality and resilience to Alzheimer’s disease neuropathology: A prospective autopsy study. Neurobiol. Aging 2013, 34, 1045–1050. [Google Scholar] [CrossRef] [PubMed]
- Terracciano, A.; Sutin, A.R.; An, Y.; O’Brien, R.J.; Ferrucci, L.; Zonderman, A.B.; Resnick, S.M. Personality and risk of Alzheimer’s disease: New data and meta-analysis. Alzheimers Dement. 2014, 10, 179–186. [Google Scholar] [CrossRef]
- Von Gunten, A.; Pocnet, C.; Rossier, J. The impact of personality characteristics on the clinical expression in neurodegenerative disorders: A review. Brain Res. Bull. 2009, 80, 179–191. [Google Scholar] [CrossRef]
- Wahlin, R.T.B.; Byrne, G.J. Personality changes in Alzheimer’s disease: A systematic review. Int. J. Geriatr. Psychiatry 2011, 26, 1019–1029. [Google Scholar] [CrossRef]
- Balsis, S.; Carpenter, B.D.; Storandt, M. Personality change precedes clinical diagnosis of dementia of the Alzheimer type. J. Gerontol. B Psychol. Sci. Soc. Sci. 2005, 60, 98–101. [Google Scholar] [CrossRef]
- Gilbert, T.; Herbst, M. Alzheimer’s disease: Charting the crossroads between neurology and psychology. J. Neurol. Neurosurg. Psychiatry 2014, 85, 133–134. [Google Scholar] [CrossRef]
- Auguste, N.; Federico, D.; Dorey, J.M.; Sagne, A.; Thomas-Antérion, C.; Rouch, I.; Laurent, B.; Gonthier, R.; Girtanner, C. Particularités sémiologiques des synptômes comportamentaux et psycholoqiques de la démence en fonction de la personalité antérieure, de lénvironnement familial et de la sévérité de la démence. Role of personality, familial environment, and severity of the disease on the behavioral and psychological symptoms of dementia. Geriatr. Psychol. Neuropsychiatr. Vieil. 2006, 4, 227–235. [Google Scholar]
- Clement, J.P.; Darthout, N.; Nubukpo, P. Événements de vie, personnalité et démence. Life events, personality and dementia. Geriatr. Psychol. Neuropsychiatr. Vieil. 2003, 1, 129–138. [Google Scholar]
- Devenand, D.P. Comorbid psychiatric disorders in late life. Biol. Psychiatry 2002, 52, 236–242. [Google Scholar] [CrossRef]
- Holwerda, T.J.; Deeg, D.J.H.; Beekman, A.T.; Tilburg, T.G.; Stek, J.; Schoevers, R.A. Feelings of loneliness, but not social isolation, predict dementia onset: Results from the Amsterdam study of the elderly (AMSTEL). J. Neurol. Neurosurg. Psychiatry 2012, 85, 135–142. [Google Scholar] [CrossRef]
- Kunik, M.E.; Martinez, M.; Snow, A.L.; Beck, C.K.; Cody, M.; Rapp, C.G.; Molinari, V.A.; Orengo, C.A.; Hamilton, J.D. Determinants of behavioral symptoms in dementia patients. Clin. Gerontol. 2003, 26, 83–89. [Google Scholar] [CrossRef]
- Mordekar, A.; Spence, S.A. Personality disorder in older people: How common is it and what can be done? Adv. Psychiatr. Treat. 2008, 14, 71–77. [Google Scholar] [CrossRef][Green Version]
- Nicholas, H.; Moran, P.; Foy, C.; Brown, R.G.; Lovestone, S.; Bryant, S.; Boothby, H. Are abnormal premorbid personality traits associated with Alzheimer’s disease? Int. J. Geriatr. Psychiatry 2010, 25, 345–351. [Google Scholar] [CrossRef]
- Oltmanns, T.F.; Balsis, S. Personality disorders in later life: Questions about the measurement, course, and impact of disorders. Annu. Rev. Clin. Psychol. 2011, 7, 321–349. [Google Scholar] [CrossRef]
- Sadavoy, J. Psychodynamic perspectives on Alzheimer´s disease and related dementias. Am. J. Alzheimer’s Care Relat. Disord. Res. 1991, 6, 12–20. [Google Scholar]
- Segal, D.L.; Coolidge, F.L.; Rosowsky, E. Personality Disorders and Older Adults: Diagnosis, Assessment, and Treatment; Wiley: Hoboken, NJ, USA, 2006. [Google Scholar]
- Dowson, J.H. Assessment of DSM-II-R personality disorders by self-report questionnaire: The role of informants and a screening test for co-morbid personality disorders (STCPD). Br. J. Psychiatry 1992, 161, 344–352. [Google Scholar] [CrossRef]
- Lykou, E.; Rankin, K.P.; Chatziantoniou, L.; Boulas, C.; Papatriantafyllou, O.; Tsaousis, I.; Neuhaus, J.; Karageorgiou, C.; Miller, B.L.; Papatriantafyllou, J.D. Big 5 personality changes in Greek bvFTD, AD, and MCI patients. Alzheimer Dis. Assoc. Disord. 2013, 27, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Rankin, K.P.; Kramer, J.H.; Mychack, P.; Miller, B.L. Double dissociation of social functioning in frontotemporal dementia. Neurology 2003, 60, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Torrente, F.; Pose, M.; Gleichgerrcht, E.; Torralva, T.; López, P.; Cetkovich-Bakmas, M.; Manes, F. Personality changes in dementia: Are they disease specific and universal? Alzheimer Dis. Assoc. Disord. 2014, 28, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Yoneda, T.; Rush, J.; Berg, A.I.; Johansson, B.; Piccinin, A.M. Trajectories of personality traits preceding dementia diagnosis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2017, 72, 922–931. [Google Scholar] [CrossRef] [PubMed]
- Yoneda, T.; Rush, J.; Graham, E.K.; Berg, A.I.; Comijs, H.; Katz, M.; Lipton, R.B.; Johansson, B.; Mroczek, D.K.; Piccinin, A.M. Increases in neuroticism may be an early indicator of dementia: A coordinated analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 14, 251–262. [Google Scholar] [CrossRef]
- Hyler, S.E. The Personality Diagnostic Questionnaire; New York State Psychiatric Institute: New York, NY, USA, 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Mihura, J.L.; Meyer, G.J.; Bel-Bahar, T.; Gunderson, J. Correspondence among observer ratings of Rorschach, Big Five Model, and DSM-IV personality disorder constructs. J. Pers. Assess 2003, 81, 20–39. [Google Scholar] [CrossRef]
- Zimmerman, M.; Coryell, W.H. Diagnosing personality disorders in the community: A comparison of self-report and interview measures. Arch. Gen. Psychiatry 1990, 47, 527–531. [Google Scholar] [CrossRef]
- Bagby, R.M.; Farvolden, P. The Personality Diagnostic Questionnaire-4+ (PDQ-4+). In Comprehensive Handbook of Psychological Assessment: Personality Assessment; John Wiley: New York, NY, USA, 2004; pp. 122–133. [Google Scholar]
- Alzheimer Europe. The Ethics of Dementia Research. 2011. Available online: http://www.alzheimer-europe.org/OEN/Ethics/Ethical-issues-in-practice/Ethics-of-dementia-research (accessed on 1 September 2022).
- World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research. 1993. Available online: https://apps.who.int/iris/handle/10665/37108 (accessed on 1 September 2022).
- McKhann, G.; Drachman, D.; Folstein, M.; Katzman, R.; Price, D.; Stadlan, E.M. Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group under the auspices of the Department of Health and Human Services Task Forces on Alzheimer’s disease. Neurology 1984, 34, 939–944. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: New York, NY, USA, 1998. [Google Scholar]
| AD Group Informants (n = 40) | AD Group (n = 44) | |||||
|---|---|---|---|---|---|---|
| Variable | M (SD) | M (SD) | F | p | η2p | π |
| PDQ-4+ Total | 38.50 (15.16) | 44.57 (17.41) | 2.87 | 0.09 | 0.03 | 0.39 |
| AD Group Informants (n = 40) | AD Group (n = 44) | ||||
|---|---|---|---|---|---|
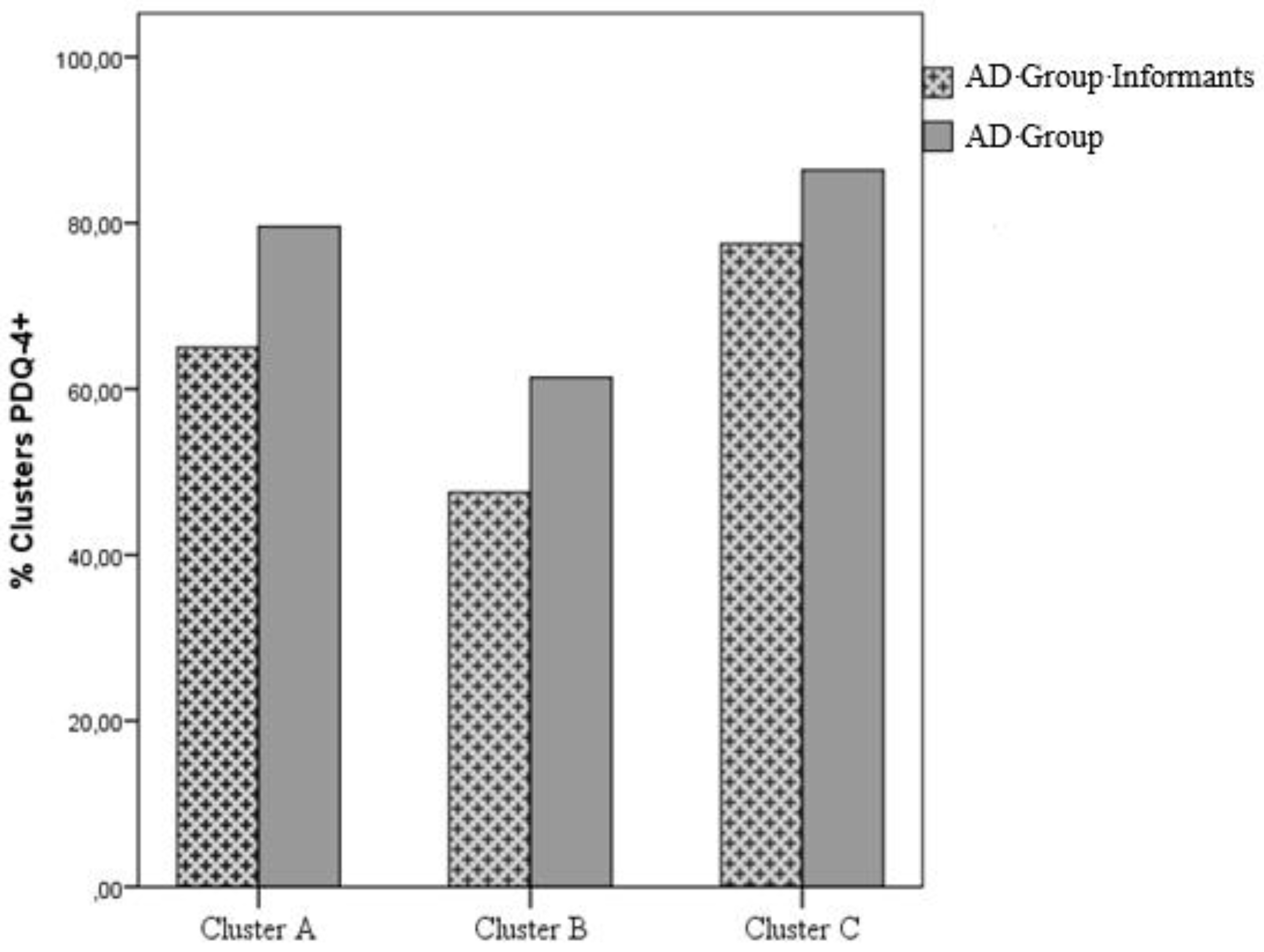
| Clusters | % (n Observed) | % (n Observed) | U | Z | p |
| Cluster A | 65.00 (26) | 79.55 (35) | 594.50 | −2.64 | 0.008 |
| Cluster B | 47.50 (19) | 61.36 (27) | 802.00 | −0.74 | 0.46 |
| Cluster C | 77.50 (31) | 88.06 (39) | 700.00 | −1.68 | 0.09 |
| AD Group Informants (n = 40) | AD Group (n = 44) | ||||
|---|---|---|---|---|---|
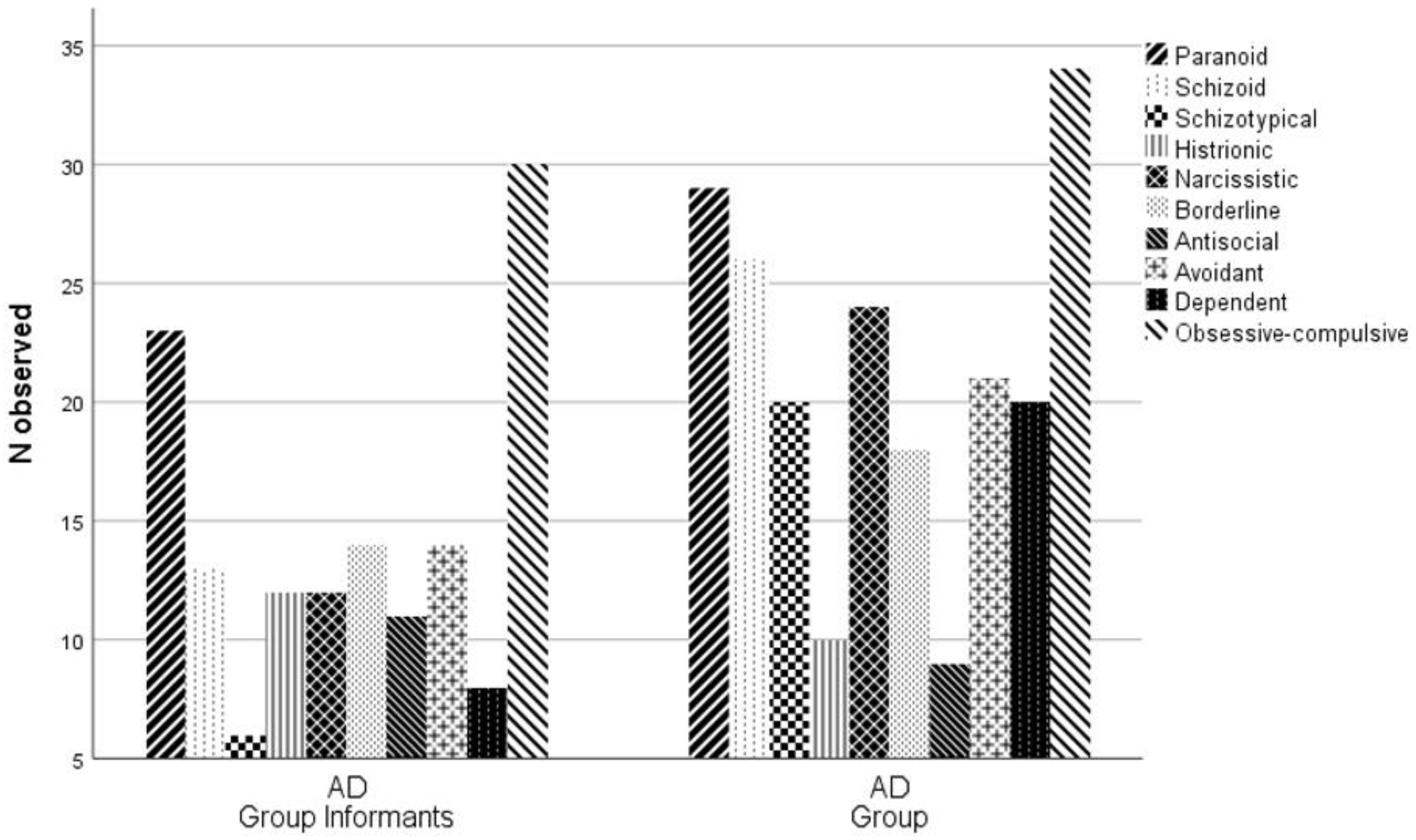
| PDQ-4+ Scales | % (n Observed) | % (n Observed) | χ2 | df | p |
| Paranoid | 57.50 (23) | 65.90 (29) | 0.32 | 1 | 0.57 |
| Schizoid | 32.50 (13) | 59.10 (26) | 4.94 | 1 | 0.03 |
| Schizotypical | 15.00 (6) | 45.50 (20) | 7.72 | 1 | 0.005 |
| Histrionic | 30.00 (12) | 22.70 (10) | 0.26 | 1 | 0.61 |
| Narcissistic | 30.00 (12) | 54.50 (24) | 4.20 | 1 | 0.04 |
| Borderline | 35.00 (14) | 40.90 (18) | 0.11 | 1 | 0.74 |
| Antisocial | 27.50 (11) | 20.50 (9) | 0.25 | 1 | 0.62 |
| Avoidant | 35.00 (14) | 47.70 (21) | 2.88 | 1 | 0.24 |
| Dependent | 20.00 (8) | 45.50 (20) | 5.02 | 1 | 0.03 |
| Obsessive-Compulsive | 75.00 (30) | 77.30 (34) | 0.001 | 1 | 1.00 |
| PCADGroup (n = 40) | PCCGroup (n = 42) | |||||
|---|---|---|---|---|---|---|
| ≠ PDQ-4+ Dimensions Current–Pre-Morbid | M (SD) | M (SD) | F | p | η2p | π |
| PDQ-4+ Total | 6.52 (21.68) | −2.90 (18.31) | 4.54 | 0.04 | 0.05 | 0.56 |
| Cluster A | 0.78 (1.35) | −0.43 (1.47) | 14.91 | 0.001 | 0.16 | 0.97 |
| Cluster B a | 0.28 (1.78) | −0.19 (0.99) | 2.13 | 0.15 | 0.03 | 0.31 |
| Cluster C | 0.38 (1.41) | −0.26 (1.11) | 5.22 | 0.03 | 0.06 | 0.62 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Henriques-Calado, J. Psychopathology Changes in Alzheimer’s Disease. Behav. Sci. 2022, 12, 418. https://doi.org/10.3390/bs12110418
Henriques-Calado J. Psychopathology Changes in Alzheimer’s Disease. Behavioral Sciences. 2022; 12(11):418. https://doi.org/10.3390/bs12110418
Chicago/Turabian StyleHenriques-Calado, Joana. 2022. "Psychopathology Changes in Alzheimer’s Disease" Behavioral Sciences 12, no. 11: 418. https://doi.org/10.3390/bs12110418
APA StyleHenriques-Calado, J. (2022). Psychopathology Changes in Alzheimer’s Disease. Behavioral Sciences, 12(11), 418. https://doi.org/10.3390/bs12110418





