People’s Experience of Shared Decision Making in Musculoskeletal Physiotherapy: A Systematic Review and Thematic Synthesis
Abstract
:1. Introduction
2. Materials and Methods
- A systematic search and data extraction;
- An appraisal of qualitative literature;
- A synthesis of qualitative data.
2.1. Literature Search
- S: individuals who have experienced MSK physiotherapy. Studies relating to other specialities within physiotherapy were excluded.
- PI: studies must have included at least 1 paragraph of explicit reference to SDM. Articles were accepted if this was contained within broader phenomena such as person-centred care or satisfaction. Articles were accepted as referencing SDM when the following could be identified, as discussed in the principles of SDM above: (a) a relationship between physiotherapist and person accessing physiotherapy, (b) a collaborative approach to discussions about rehabilitation options and (c) a discussion of the person’s preferences for rehabilitation.
- D: a broad range of qualitative types were included, whilst quantitative research, conference proceedings and pilot studies were excluded.
- E: exploration of people’s experiences of SDM in MSK physiotherapy. Studies must report first-hand experiences of people, as opposed to perceptions of healthcare professionals. If an article included both perspectives, clear distinction between clinicians’ and people’s views was required.
- R: all qualitative research types were included in the search. As SDM is a complex intervention likely affected by multiple factors [12], the intention to fully understand context is integral, and quantitative research limited to numerical data may misrepresent findings [22]. Moreover, as the aim of this review is to understand the patient’s perspective, retaining narratives presented through qualitative research is fundamental, resulting in the exclusion of quantitative methodologies.
- Other: date of publication was not limited, as a scoping literature search demonstrated no known systematic reviews published previously. Language was limited to English as the primary language understood by the review team.
2.2. Study Selection and Data Extraction
2.3. Critical Appraisal
2.4. Analysis and Synthesis
3. Results
3.1. Study Characteristics
3.2. Critical Appraisal
3.3. Synthesis
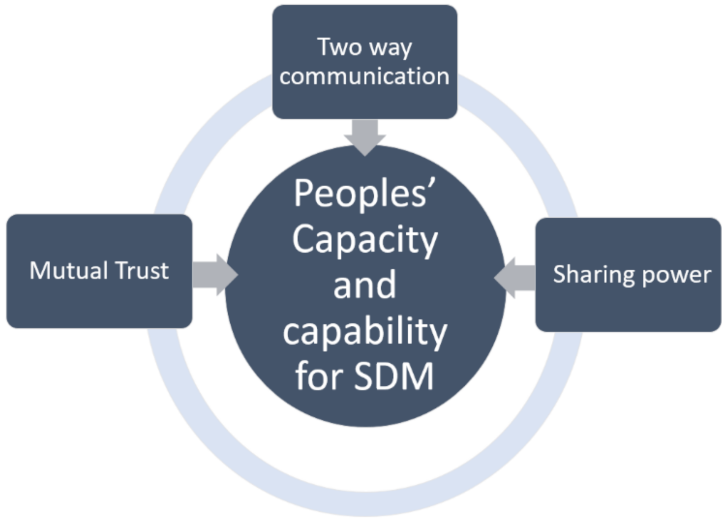
3.4. Theme 1: Trust
3.4.1. The Development of Trust
3.4.2. The Positive Impact of Trust
3.4.3. The Negative Impact of Trust
3.5. Theme 2: Communication
Two-Way Communication Is Essential for Collaboration
3.6. Theme 3: Decision Preferences
3.6.1. Preferences for Involvement in Decision-Making
3.6.2. Factors Which Influence Involvement
3.7. Theme 4: Decision Ability
3.7.1. People Are Not Involved in Decision-Making
3.7.2. The Power Struggle
4. Discussion
4.1. Trust
4.2. Communication
4.3. Decision Preferences
4.4. Decision Ability
4.5. Limitations
4.6. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Légaré, F.; Adekpedjou, R.; Stacey, D.; Turcotte, S.; Kryworuchko, J.; Graham, I.D.; Lyddiatt, A.; Politi, M.C.; Thomson, R.; Elwyn, G.; et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst. Rev. 2018, 7. [Google Scholar] [CrossRef] [PubMed]
- Légaré, F.; Stacey, D.; Pouliot, S.; Gauvin, F.P.; Desroches, S.; Kryworuchko, J.; Dunn, S.; Elwyn, G.; Frosch, D.; Gagnon, M.P.; et al. Interprofessionalism and shared decision-making in primary care: A stepwise approach towards a new model. J. Int. Care 2011, 25, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Towle, A.; Greenhalgh, T.; Gambrill, J.; Godolphin, W. Framework for teaching and learning informed shared decision making. Competencies for informed shared decision making. Proposals based on too many assumptions. BMJ 1999, 319, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Elwyn, G.; Edwards, A.; Kinnersley, P. Shared decision-making in primary care: The neglected second half of the consultation. Br. J. Gen. Pract. 1999, 49, 477–482. [Google Scholar] [PubMed]
- Towle, A.; Bainbridge, L.; Godolphin, W.; Katz, A.; Kline, C.; Lown, B.; Madularu, I.; Solomon, P.; Thistlethwaite, J. Active patient involvement in the education of health professionals. Med. Educ. 2010, 44, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Härter, M.; van der Weijden, T.; Elwyn, G. Policy and practice developments in the implementation of shared decision making: An international perspective. Z. Evidenz Fortbild. Qual. Gesundh. 2011, 105, 229–233. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Shared Decision Making Collaborative. A Consensus Statement. 2016. Available online: https://www.nice.org.uk/Media/Default/About/what-we-do/SDM-consensus-statement.pdf (accessed on 2 April 2020).
- Mulley, A.G.; Trimble, C.; Elwyn, G. Stop the silent misdiagnosis: Patients’ preferences matter. BMJ 2012, 345, e6572. [Google Scholar] [CrossRef] [Green Version]
- Wennberg, J.E. Practice variation: Implications for our health care system. Manag. Care 2004, 13, 3. [Google Scholar]
- Stacey, D.; Légaré, F.; Lewis, K.; Barry, M.J.; Bennett, C.L.; Eden, K.B.; Holmes-Rovner, M.; Llewellyn-Thomas, H.; Lyddiatt, A.; Thomson, R.; et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst. Rev. 2017, 4, CD001431. [Google Scholar] [CrossRef] [Green Version]
- Brody, D.S. The patient’s role in clinical decision-making. Ann. Intern. Med. 1980, 93, 718–722. [Google Scholar] [CrossRef]
- Härter, M.; Moumjid, N.; Cornuz, J.; Elwyn, G.; van der Weijden, T. Shared decision making in 2017: International accomplishments in policy, research and implementation. Z. Evidenz Fortbild. Qual. Gesundh. 2017, 123, 1–5. [Google Scholar] [CrossRef]
- Josefsson, K.A.; Andersson, A.C. The co-constructive processes in physiotherapy. Cog. Med. 2017, 4, 1290308. [Google Scholar] [CrossRef]
- Dierckx, K.; Deveugele, M.; Roosen, P.; Devisch, I. Implementation of shared decision making physical therapy: Observed level of involvement and patient preference. Phys. Ther. 2013, 93, 1321–1330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sam, S.; Sharma, R.; Corp, N.; Igwesi-Chidobe, C.; Babatunde, O.O. Shared decision making in musculoskeletal pain consultations in low-and middle-income countries: A systematic review. Int. Health 2020, 12, 455–471. [Google Scholar] [CrossRef]
- Joseph-Williams, N.; Lloyd, A.; Edwards, A.; Stobbart, L.; Tomson, D.; Macphail, S.; Dodd, C.; Brain, K.; Elwyn, G.; Thomson, R. Implementing shared decision making in the NHS: Lessons from the MAGIC programme. BMJ 2017, 357, j1744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kidd, M.O.; Bond, C.H.; Bell, M.L. Patients’ perspectives of patient-centredness as important in musculoskeletal physiotherapy interactions: A qualitative study. Physiotherapy 2011, 97, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Stenner, R.; Palmer, S.; Hammond, R. What matters most to people in musculoskeletal physiotherapy consultations? A qualitative study. Musc. Sci. Pract. 2018, 35, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Stenner, R.; Swinkels, A.; Mitchell, T.; Palmer, S. Exercise prescription for non-specific chronic low back pain (NSCLBP): A qualitative study of patients’ experiences of involvement in decision making. Physiotherapy 2016, 102, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.; May, S. A qualitative study into Egyptian patients’ satisfaction with physiotherapy management of low back pain. Physiother. Res. Int. 2017, 22, e1647. [Google Scholar] [CrossRef] [Green Version]
- Hausheer, A.C.; Suter, L.C.; Kool, J. Shared decision-making in physical therapy: A cross-sectional observational study. Eur. J. Physiother. 2020, 23, 368–376. [Google Scholar] [CrossRef]
- Sutton, A.; Clowes, M.; Preston, L.; Booth, A. Meeting the review family: Exploring review types and associated information retrieval requirements. Health Inf. Libr. J. 2019, 36, 202–222. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008, 8, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maxwell, J.A. A Realist Approach for Qualitative Research; Sage: London, UK, 2012. [Google Scholar]
- Duncan, E.A.; Nicol, M.M. Subtle realism and occupational therapy: An alternative approach to knowledge generation and evaluation. Br. J. Occup. Ther. 2004, 67, 453–456. [Google Scholar] [CrossRef]
- Tong, A.; Flemming, K.; McInnes, E.; Oliver, S.; Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med. Res. Methodol. 2012, 12, 181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pawson, R.; Greenhalgh, T.; Harvey, G.; Walshe, K. Realist review-a new method of systematic review designed for complex policy interventions. J. Health Serv. Res. Policy 2005, 10, 21–34. [Google Scholar] [CrossRef]
- Salvador-Oliván, J.A.; Marco-Cuenca, G.; Arquero-Avilés, R. Errors in search strategies used in systematic reviews and their effects on information retrieval. J. Med. Libr. Assoc. 2019, 107, 210. [Google Scholar] [CrossRef] [Green Version]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS peer review of electronic search strategies: 2015 guideline statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef] [Green Version]
- Schoeb, V.; Bürge, E. Perceptions of patients and physiotherapists on patient participation: A narrative synthesis of qualitative studies. Physiother. Res. Int. 2012, 17, 80–91. [Google Scholar] [CrossRef]
- Joseph-Williams, N.; Elwyn, G.; Edwards, A. Knowledge is not power for patients: A systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ. Couns. 2014, 94, 291–309. [Google Scholar] [CrossRef]
- Cooke, A.; Smith, D.; Booth, A. Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qual. Health Res. 2012, 22, 1435–1443. [Google Scholar] [CrossRef] [PubMed]
- Eakin, J.M.; Mykhalovskiy, E. Reframing the evaluation of qualitative health research: Reflections on a review of appraisal guidelines in the health sciences. J. Eval. Clin. Pract. 2003, 9, 187–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thorne, S.; Jensen, L.; Kearney, M.H.; Noblit, G.; Sandelowski, M. Qualitative metasynthesis: Reflections on methodological orientation and ideological agenda. Qual. Health Res. 2004, 14, 1342–1365. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Payton, O.D.; Nelson, C.E.; Hobbs, M.S. Physical therapy patients’ perceptions of their relationships with health care professionals. Physiother. Theory Pract. 1998, 14, 211–221. [Google Scholar] [CrossRef]
- Cooper, K.; Smith, B.H.; Hancock, E. Patient-centredness in physiotherapy from the perspective of the chronic low back pain patient. Physiotherapy 2008, 94, 244–252. [Google Scholar] [CrossRef]
- Potter, M.; Gordon, S.; Hamer, P. The physiotherapy experience in private practice: The patients’ perspective. Aus. J. Physiother. 2003, 49, 195–202. [Google Scholar] [CrossRef] [Green Version]
- Wikman, A.; Fältholm, Y. Patient empowerment in rehabilitation: “Somebody told me to get rehabilitated”. Adv. Physiother. 2006, 8, 23–32. [Google Scholar] [CrossRef]
- Lindahl, M.; Teljigović, S.; Heegaard Jensen, L.; Hvalsoe, B.; Juneja, H. Importance of a patient-centred approach in ensuring quality of post-fracture rehabilitation for working aged people: A qualitative study of therapists’ and patients’ perspectives. Work 2016, 55, 831–839. [Google Scholar] [CrossRef] [PubMed]
- Bernhardsson, S.; Larsson, M.E.; Johansson, K.; Öberg, B. “In the physio we trust”: A qualitative study on patients’ preferences for physiotherapy. Physiother. Theory Pract. 2017, 33, 535–549. [Google Scholar] [CrossRef] [PubMed]
- Bernhardsson, S.; Samsson, K.S.; Johansson, K.; Öberg, B.; Larsson, M.E. A preference for dialogue: Exploring the influence of patient preferences on clinical decision making and treatment in primary care physiotherapy. Eur. J. Physiother. 2019, 21, 21–107. [Google Scholar] [CrossRef]
- Doyle, L.H. Synthesis through meta-ethnography: Paradoxes, enhancements, and possibilities. Qual. Res. 2003, 3, 321–344. [Google Scholar] [CrossRef]
- Caress, A.L.; Luker, K.; Woodcock, A.; Beaver, K. A qualitative exploration of treatment decision-making role preference in adult asthma patients. Health Expect. 2002, 5, 223–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bastiaens, H.; Van Royen, P.; Pavlic, D.R.; Raposo, V.; Baker, R. Older people’s preferences for involvement in their own care: A qualitative study in primary health care in 11 European countries. Patient Educ. Couns. 2007, 68, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Aasen, E.M.; Kvangarsnes, M.; Heggen, K. Perceptions of patient participation amongst elderly patients with end-stage renal disease in a dialysis unit. Scand. J. Caring Sci. 2012, 26, 61–69. [Google Scholar] [CrossRef] [Green Version]
- Frosch, D.L.; May, S.G.; Rendle, K.A.; Tietbohl, C.; Elwyn, G. Authoritarian physicians and patients’ fear of being labeled ‘difficult’among key obstacles to shared decision making. Health Aff. 2012, 31, 1030–1038. [Google Scholar] [CrossRef] [Green Version]
- Say, R.; Murtagh, M.; Thomson, R. Patients’ preference for involvement in medical decision making: A narrative review. Patient Educ. Couns. 2006, 60, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Kelsey, J.; Abelson-Mitchell, N.; Skirton, H. Perceptions of young people about decision making in the acute healthcare environment. Nurse Child. Young People 2007, 19, 14–18. [Google Scholar] [CrossRef]
- Patel, S.; Ngunjiri, A.; Sandhu, H.; Griffiths, F.; Thistlewaite, J.; Brown, S.; Friede, T.; Lord, J.; Tysall, C.; Woolvine, M.; et al. Design and development of a decision support package for low back pain. Arthritis Care Res. 2014, 66, 925–933. [Google Scholar] [CrossRef]
- Makoul, G.; Arntson, P.; Schofield, T. Health promotion in primary care: Physician-patient communication and decision making about prescription medications. Soc. Sci. Med. 1995, 41, 1241–1254. [Google Scholar] [CrossRef]
- Joseph-Williams, N.; Williams, D.; Wood, F.; Lloyd, A.; Brain, K.; Thomas, N.; Prichard, A.; Goodland, A.; McGarrigle, H.; Sweetland, H.; et al. A descriptive model of shared decision making derived from routine implementation in clinical practice (‘Implement-SDM’): Qualitative study. Patient Educ. Couns. 2019, 102, 1774–1785. [Google Scholar] [CrossRef]
- Pinto, R.Z.; Ferreira, M.L.; Oliveira, V.C.; Franco, M.R.; Adams, R.; Maher, C.G.; Ferreira, P.H. Patient-centred communication is associated with positive therapeutic alliance: A systematic review. J. Physiother. 2012, 58, 77–87. [Google Scholar] [CrossRef] [Green Version]
- Flynn, K.E.; Smith, M.A.; Vanness, D. A typology of preferences for participation in healthcare decision making. Soc. Sci. Med. 2006, 63, 1158–1169. [Google Scholar] [CrossRef] [Green Version]
- Chewning, B.; Bylund, C.L.; Shah, B.; Arora, N.K.; Gueguen, J.A.; Makoul, G. Patient preferences for shared decisions: A systematic review. Patient Educ. Couns. 2012, 86, 9–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doherty, C.; Doherty, W. Patients’ preferences for involvement in clinical decision-making within secondary care and the factors that influence their preferences. J. Nurs. Manag. 2005, 13, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.G. The meaning of patient involvement and participation in health care consultations: A taxonomy. Soc. Sci. Med. 2007, 64, 1297–1310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hargraves, I.; Montori, V.M. Decision aids, empowerment, and shared decision making. BMJ 2014, 357, g5811. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Pound, P.; Campbell, R. Exploring the feasibility of theory synthesis: A worked example in the field of health related risk-taking. Soc. Sci. Med. 2015, 124, 57–65. [Google Scholar] [CrossRef] [Green Version]
- Turner, J.H. Developing cumulative and practical knowledge through metatheorizing. Sociol. Perspect. 1991, 34, 249–268. [Google Scholar] [CrossRef]
- Hellmann, G. In conclusion: Dialogue and synthesis in individual scholarship and collective inquiry. Int. Stud. Rev. 2003, 5, 147–153. [Google Scholar] [CrossRef]
- Mays, N.; Pope, C. Assessing quality in qualitative research. BMJ 2000, 320, 50–52. [Google Scholar] [CrossRef] [PubMed]
- Berger, R. Now I see it, now I don’t: Researcher’s position and reflexivity in qualitative research. Qual. Res. 2015, 2, 219–234. [Google Scholar] [CrossRef]
- Elwyn, G.; Frosch, D.; Thomson, R.; Joseph-Williams, N.; Lloyd, A.; Kinnersley, P.; Cording, E.; Tomson, D.; Dodd, C.; Rollnick, S.; et al. Shared decision making: A model for clinical practice. J. Gen. Int. Med. 2012, 27, 1361–1367. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grenfell, J.; Soundy, A. People’s Experience of Shared Decision Making in Musculoskeletal Physiotherapy: A Systematic Review and Thematic Synthesis. Behav. Sci. 2022, 12, 12. https://doi.org/10.3390/bs12010012
Grenfell J, Soundy A. People’s Experience of Shared Decision Making in Musculoskeletal Physiotherapy: A Systematic Review and Thematic Synthesis. Behavioral Sciences. 2022; 12(1):12. https://doi.org/10.3390/bs12010012
Chicago/Turabian StyleGrenfell, Jessica, and Andrew Soundy. 2022. "People’s Experience of Shared Decision Making in Musculoskeletal Physiotherapy: A Systematic Review and Thematic Synthesis" Behavioral Sciences 12, no. 1: 12. https://doi.org/10.3390/bs12010012





