Understanding Somatic Symptoms Associated with South Korean Adolescent Suicidal Ideation, Depression, and Social Anxiety
Abstract
:1. Introduction
Current Study
2. Method
2.1. Sample
2.2. Measures
2.3. Plan for Analyses
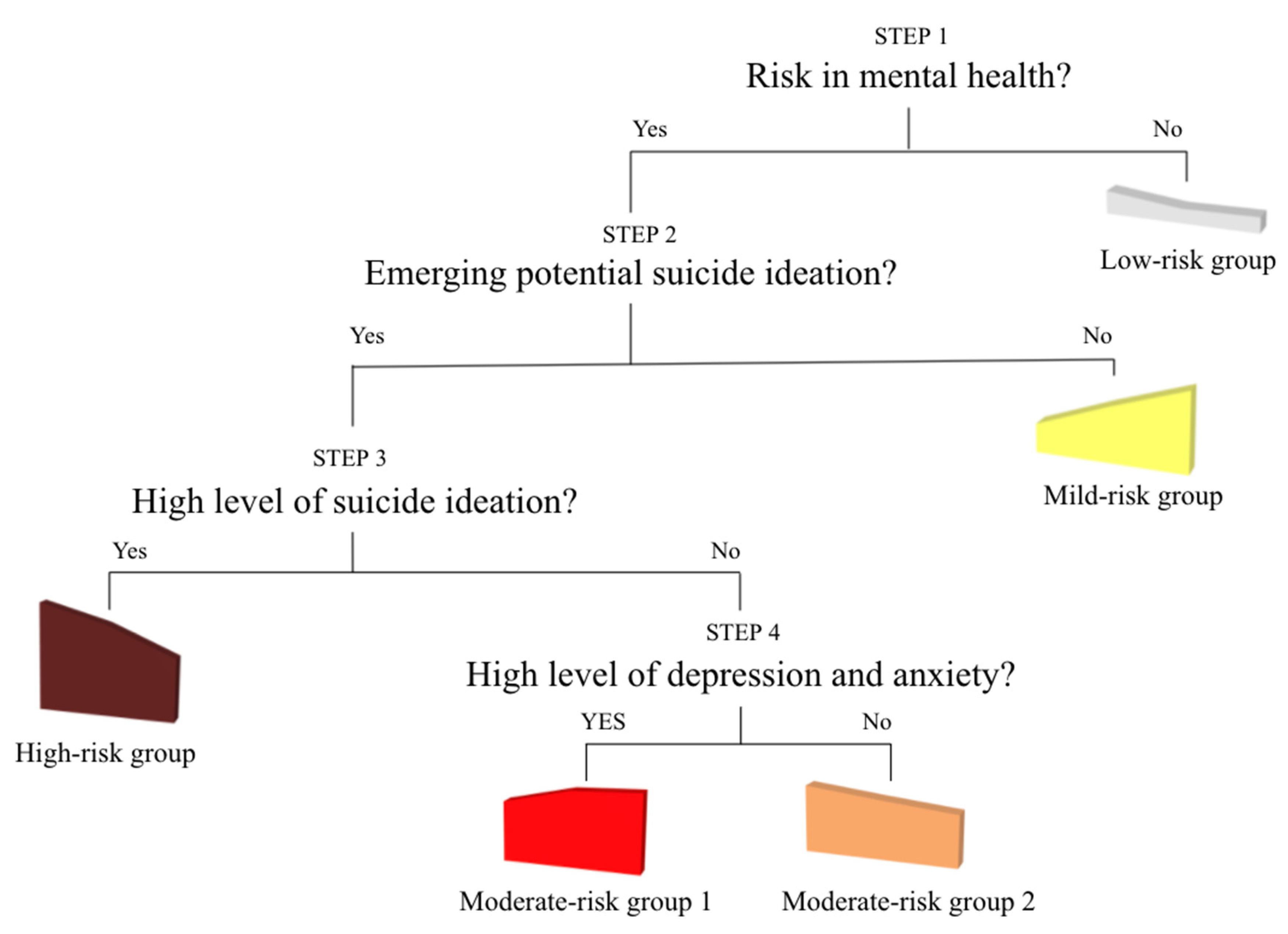
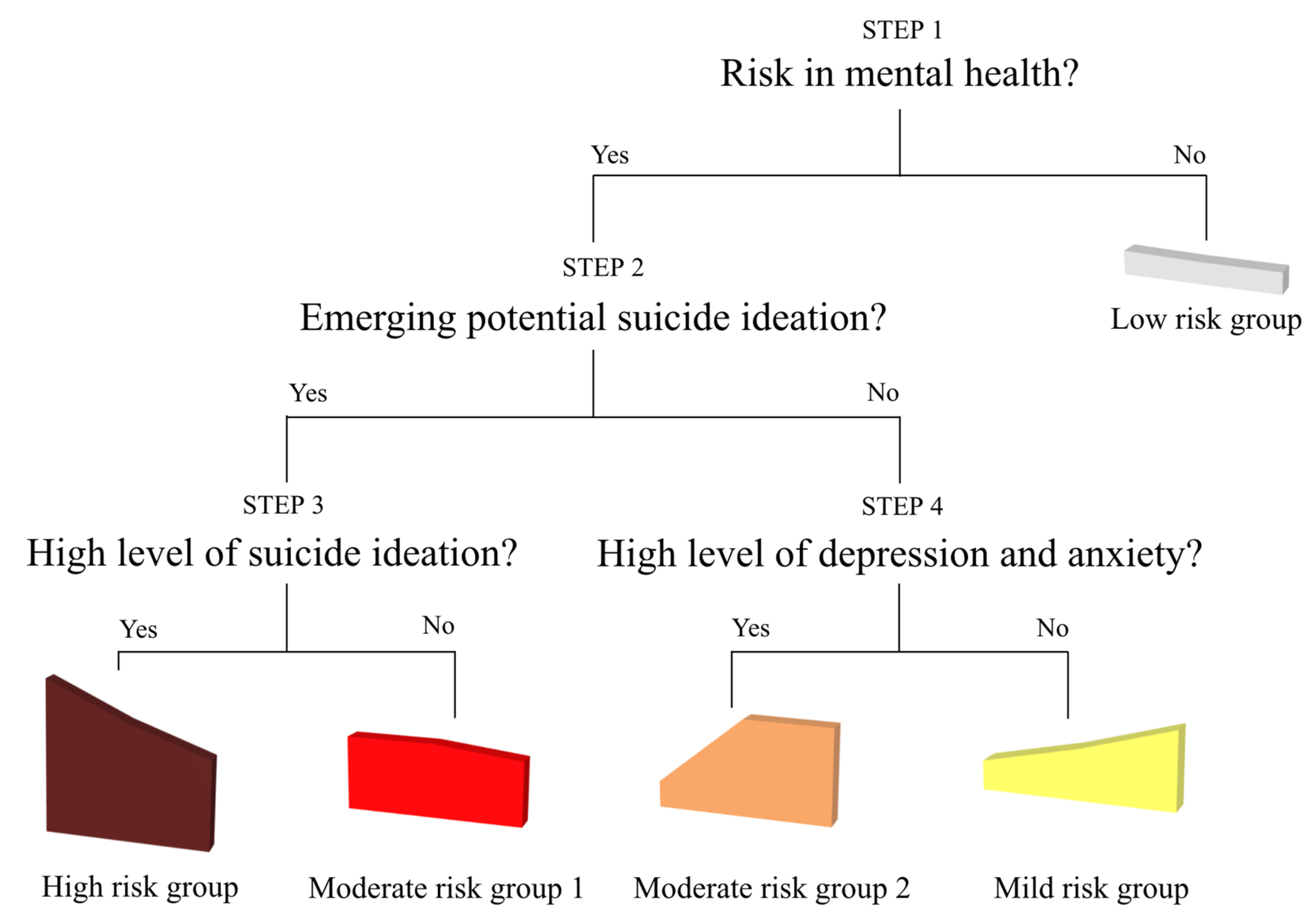
2.3.1. Primary Analysis Using Latent Profile Analysis
2.3.2. Post-Hoc Analysis Using Logistic Regression
3. Results
3.1. Prevalence Rates among Korean Youth
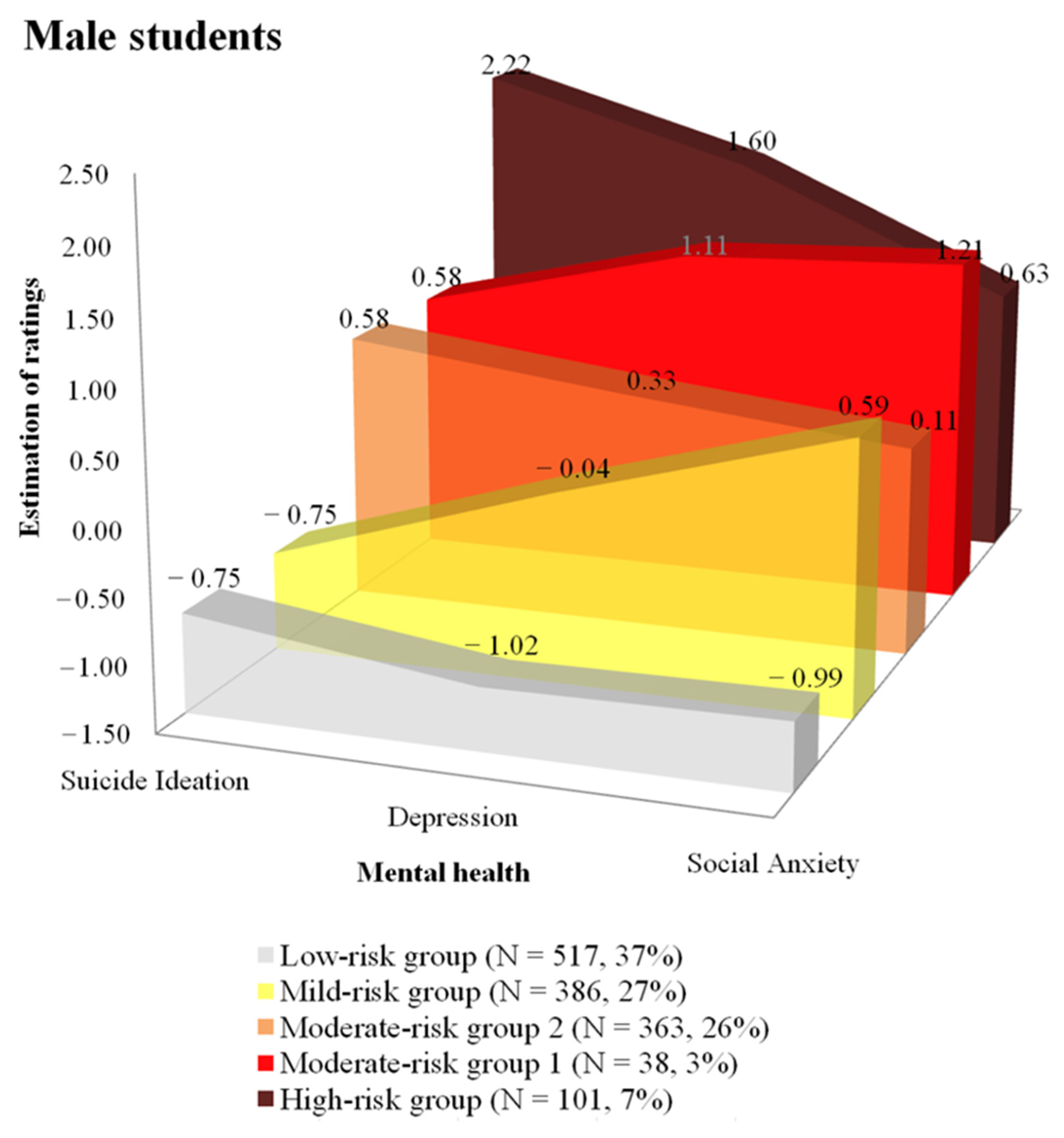
3.2. Latent Mental Health Profiles among Korean Youth
3.3. Somatic Symptoms Associated with Mental Health Profiles
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Westefeld, J.S. 2010 Presidential Address A Tale of Two Gavels. Couns. Psychol. 2010, 39, 171–182. [Google Scholar] [CrossRef]
- Westefeld, J.S. Suicide Prevention: An Issue of Social Justice. J. Prev. Health Promot. 2020, 1, 58–79. [Google Scholar] [CrossRef]
- World Health Organization. GHO | World Health Statistics Data Visualizations Dashboard | Suicide. 2018. Available online: https://apps.who.int/gho/data/node.sdg.3-4-viz-2?lang=en (accessed on 19 November 2020).
- Hedegaard, H.; Curtin, S.C.; Warner, M. Increase in Suicide Mortality in the United States, 1999–2018. NCHS Data Brief 2020, 362, 1–8. [Google Scholar]
- WHO Preventing Suicide: A Global Imperative; WHO: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/131056/9789241564779_eng.pdf;jsessionid=926027CB27C8539BDABF8C2991F7FBFC?sequence=1 (accessed on 19 November 2020).
- OECD. Suicide Rates (Indicator). 2021. Available online: https://data.oecd.org/healthstat/suicide-rates.htm (accessed on 8 January 2021).
- Chen, Y.-Y.; Wu, K.C.-C.; Yousuf, S.; Yip, P.S.F. Suicide in Asia: Opportunities and Challenges. Epidemiol. Rev. 2011, 34, 129–144. [Google Scholar] [CrossRef]
- Statistics of Korea. 2017 Statistics Reports in Cause of Death. Available online: http://kostat.go.kr/portal/korea/kor_nw/1/6/2/index.board?bmode=read&bSeq=&aSeq=370710&pageNo=1&rowNum=10&navCount=10&currPg=&searchInfo=&sTarget=title&sTxt= (accessed on 8 January 2021).
- Park, S. Gender-Specific Factors of Suicide Ideation Among Adolescents in the Republic of Korea: A Nationally Representative Population-Based Study. Arch. Psychiatr. Nurs. 2013, 27, 253–259. [Google Scholar] [CrossRef]
- Jung, S.; Lee, D.; Park, S.; Lee, K.; Kweon, Y.-S.; Lee, E.-J.; Yoon, K.H.; Cho, H.; Jung, H.; Kim, A.R.; et al. Gender differences in Korean adolescents who died by suicide based on teacher reports. Child Adolesc. Psychiatry Ment. Health 2019, 13, 12. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Hong, S.-C. Prevalence of major depressive disorder in the general population of South Korea. J. Psychiatr. Res. 2006, 40, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, T.; Brown, T.L. Mental illness stigma and ethnocultural beliefs, values, and norms: An integrative review. Clin. Psychol. Rev. 2011, 31, 934–948. [Google Scholar] [CrossRef]
- Choi, E.; Chentsova-Dutton, Y.; Parrott, W.G. The Effectiveness of Somatization in Communicating Distress in Korean and American Cultural Contexts. Front. Psychol. 2016, 7, 383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeon, H.J.; Walker, R.S.; Inamori, A.; Hong, J.P.; Cho, M.J.; Baer, L.; Clain, A.; Fava, M.; Mischoulon, D. Differences in depressive symptoms between Korean and American outpatients with major depressive disorder. Int. Clin. Psychopharmacol. 2014, 29, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S. Risk factors for suicide attempts among Korean adolescents. Child Psychiatry Hum. Dev. 2008, 39, 221–235. [Google Scholar] [CrossRef]
- Korea Psychological Autopsy Center. Psychological Autopsy Interview Report 2015–2018; Korea Psychological Autopsy Center: Seoul, Korea, 2018.
- Hetland, J.; Torsheim, T.; Aarø, L.E. Subjective health complaints in adolescence: Dimensional structure and variation across gender and age. Scand. J. Public Health 2002, 30, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Beck, J.E. A Developmental Perspective on Functional Somatic Symptoms. J. Pediatr. Psychol. 2007, 33, 547–562. [Google Scholar] [CrossRef] [Green Version]
- Lauber, C.; Rössler, W. Stigma towards people with mental illness in developing countries in Asia. Int. Rev. Psychiatry 2007, 19, 157–178. [Google Scholar] [CrossRef]
- Lee, S.; Chiu, M.Y.; Tsang, A.; Chui, H.; Kleinman, A. Stigmatizing experience and structural discrimination associated with the treatment of schizophrenia in Hong Kong. Soc. Sci. Med. 2006, 62, 1685–1696. [Google Scholar] [CrossRef]
- Alvidrez, J.; Snowden, L.R.; Kaiser, D.M. The Experience of Stigma among Black Mental Health Consumers. J. Health Care Poor Underserved 2008, 19, 874–893. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, P. How stigma interferes with mental health care. Am. Psychol. 2004, 59, 614–625. [Google Scholar] [CrossRef] [Green Version]
- Ng, C.H. The Stigma of Mental Illness in Asian Cultures. Aust. N. Z. J. Psychiatry 1997, 31, 382–390. [Google Scholar] [CrossRef]
- Cheng, H.-L.; Wang, C.; McDermott, R.C.; Kridel, M.; Rislin, J.L. Self-Stigma, Mental Health Literacy, and Attitudes Toward Seeking Psychological Help. J. Couns. Dev. 2018, 96, 64–74. [Google Scholar] [CrossRef]
- Sue, D.W. Asian-American mental health and help-seeking behavior: Comment on Solberg et al. (1994), Tata and Leong (1994), and Lin (1994). J. Couns. Psychol. 1994, 41, 292–295. [Google Scholar] [CrossRef]
- Sanchez, F.; Gaw, A. Mental health care of Filipino Americans. Psychiatr. Serv. 2007, 58, 810–815. [Google Scholar] [CrossRef] [PubMed]
- Yun, M.H.; Shim, E.-J. The relationship among dichotomous thinking, dysfunctional perfectionism and suicide Ideation in adolescents: The mediating role of hopelessness depression symptom. Korean J. Sch. Psychol. 2014, 11, 621–638. [Google Scholar]
- Lee, H.; An, S. Analysis of the stigma factor of suicide prevention news. Korean J. Journal. Commun. Stud. 2013, 57, 27–47. [Google Scholar]
- Park, B.B.; Im, J.S.; Ratcliff, K.S. Rising Youth Suicide and the Changing Cultural Context in South Korea. Crisis 2014, 35, 102–109. [Google Scholar] [CrossRef]
- Kim, G.E.; Jo, M.-W.; Shin, Y.-W. Increased prevalence of depression in South Korea from 2002 to 2013. Sci. Rep. 2020, 10, 1–9. [Google Scholar] [CrossRef]
- Kwon, J.-W.; Chun, H.; Cho, S.-I. A closer look at the increase in suicide rates in South Korea from 1986–2005. BMC Public Health 2009, 9, 72. [Google Scholar] [CrossRef] [Green Version]
- Kahng, S.K.; Kim, H. A Developmental Overview of Mental Health System in Korea. Soc. Work. Public Health 2010, 25, 158–175. [Google Scholar] [CrossRef]
- Heo, Y.-C.; Kahng, S.K.; Kim, S. Mental health system at the community level in Korea: Development, recent reforms and challenges. Int. J. Ment. Health Syst. 2019, 13, 1–5. [Google Scholar] [CrossRef]
- WHO-AIMS Report on Mental Health System in Republic of Korea; WHO and Ministry of Health and Welfare: Gwacheon City, Korea, 2007.
- Ministry of Health and Welfare. National Suicide Prevention Action Plan [Policy Report]. Sejong. 2018. Available online: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=44&CONT_SEQ=343649 (accessed on 19 November 2020).
- Park, S.-C.; Na, K.-S.; Kwon, S.-J.; Kim, M.; Kim, H.-J.; Baik, M.; Seol, J.; An, E.J.; Lee, S.M.; Lee, E.-J.; et al. “Suicide CARE” (Standardized Suicide Prevention Program for Gatekeeper Intervention in Korea): An Update. Psychiatry Investig. 2020, 17, 911–924. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare of Korea. The 2016 Survey of Mental Disorders in Korea [Research Report]; Ministry of Health and Welfare of Korea: Sejong, Korea, 2017. Available online: http://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=032901&CONT_SEQ=339138&page=1 (accessed on 8 January 2021).
- Kim, Y.; Chang, H. Effect of physical health conditions on suicidal ideation in Korean adolescents. Korean J. Health Educ. Promot. 2016, 33, 27–37. [Google Scholar] [CrossRef] [Green Version]
- Wong, Y.J.; Maffini, C.S.; Shin, M. The Racial-Cultural Framework. Couns. Psychol. 2013, 42, 13–54. [Google Scholar] [CrossRef]
- Kim, K.; Kim, J.; Won, H. Korean Manual of Symptom Checklist-90-Revision; Chungang Aptitude Publishing: Seoul, Korea, 1984. [Google Scholar]
- Kim, S.; Kim, K. Development of Behavior Problem Scale for Children and Adolescence. J. Korean Home Manag. Assoc. 1998, 16, 155–166. [Google Scholar] [CrossRef]
- Cho, B.; Lim, K. Development and validation of emotional or behavioral problems scale. Korean J. Couns. Psychother. 2003, 15, 729–746. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2012. [Google Scholar]
- Vrieze, S.I. Model selection and psychological theory: A discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Psychol. Methods 2012, 17, 228–243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramaswamy, V.; DeSarbo, W.S.; Reibstein, D.J.; Robinson, W.T. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Market. Sci. 1993, 12, 103–124. [Google Scholar] [CrossRef]
- Feldman, B.J.; Masyn, K.E.; Conger, R.D. New approaches to studying problem behaviors: A comparison of methods for modeling longitudinal, categorical adolescent drinking data. Dev. Psychol. 2009, 45, 652–676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, H.S.; Schepp, K.G.; Jang, E.H.; Koo, H.Y. Predictors of Suicidal Ideation Among High School Students by Gender in South Korea. J. Sch. Health 2006, 76, 181–188. [Google Scholar] [CrossRef]
- Merikangas, K.R.; He, J.-P.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 980–989. [Google Scholar] [CrossRef] [Green Version]
- Bernert, R.A.; Kim, J.S.; Iwata, N.G.; Perlis, M.L. Sleep Disturbances as an Evidence-Based Suicide Risk Factor. Curr. Psychiatry Rep. 2015, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Nrugham, L.; Larsson, B.; Sund, A.M. Specific depressive symptoms and disorders as associates and predictors of suicidal acts across adolescence. J. Affect. Disord. 2008, 111, 83–93. [Google Scholar] [CrossRef]
- Wong, M.M.; Brower, K.J. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J. Psychiatr. Res. 2012, 46, 953–959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, S.-G.; Lee, Y.J.; Kim, S.J.; Lim, W.; Lee, H.-J.; Park, Y.-M.; Cho, I.H.; Cho, S.-J.; Hong, J.P. Weekend catch-up sleep is independently associated with suicide attempts and self-injury in Korean adolescents. Compr. Psychiatry 2014, 55, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Cho, S.-J.; Cho, I.H.; Kim, S.J. Insufficient Sleep and Suicidality in Adolescents. Sleep 2012, 35, 455–460. [Google Scholar] [CrossRef]
- Park, H. Effect of Sleep Duration on Suicidal Ideation in Korean Adolescents. J. Korean Soc. Sch. Health 2015, 28, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Kitagawa, Y.; Ando, S.; Yamasaki, S.; Foo, J.C.; Okazaki, Y.; Shimodera, S.; Nishida, A.; Togo, F.; Sasaki, T. Appetite loss as a potential predictor of suicidal ideation and self-harm in adolescents: A school-based study. Appetite 2017, 111, 7–11. [Google Scholar] [CrossRef]
- Jeon, H.J.; Woo, J.-M.; Kim, H.-J.; Fava, M.; Mischoulon, D.; Cho, S.J.; Chang, S.M.; Park, D.-H.; Kim, J.W.; Yoo, I.; et al. Gender Differences in Somatic Symptoms and Current Suicidal Risk in Outpatients with Major Depressive Disorder. Psychiatry Investig. 2016, 13, 609–615. [Google Scholar] [CrossRef] [Green Version]
- Spitzer, R.L.; Williams, J.B.; Kroenke, K.; Linzer, M.; Degruy, F.V.; Hahn, S.R.; Brody, D.; Johnson, J.G. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994, 272, 1749–1756. [Google Scholar] [CrossRef]
- Jo, S.A.; Park, M.H.; Jo, I.; Ryu, S.-H.; Han, C. Usefulness of Beck Depression Inventory (BDI) in the Korean elderly population. Int. J. Geriatr. Psychiatry 2007, 22, 218–223. [Google Scholar] [CrossRef]
- Ozawa-de Silva, C. Too lonely to die alone: Internet suicide pacts and existential suffering in Japan. Cult. Med. Psychiatry 2008, 32, 516–551. [Google Scholar] [CrossRef]
- Takeshima, T.; Yamauchi, T.; Inagaki, M.; Kodaka, M.; Matsumoto, T.; Kawano, K.; Katsumata, Y.; Fujimori, M.; Hisanaga, A.; Takahashi, Y. Suicide prevention strategies in Japan: A 15-year review (1998–2013). J. Public Health Policy 2014, 36, 52–66. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021, 5, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Matsubayashi, T.; Ueda, M.; Yoshikawa, K. School and seasonality in youth suicide: Evidence from Japan. J. Epidemiol. Community Health 2016, 70, 1122–1127. [Google Scholar] [CrossRef]
- Hansen, B.; Lang, M. Back to school blues: Seasonality of youth suicide and the academic calendar. Econ. Educ. Rev. 2011, 30, 850–861. [Google Scholar] [CrossRef]
- Ahmad, F.; Jhajj, A.K.; E Stewart, D.; Burghardt, M.; Bierman, A.S. Single item measures of self-rated mental health: A scoping review. BMC Health Serv. Res. 2014, 14, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Bergkvist, L. Appropriate use of single-item measures is here to stay. Mark. Lett. 2015, 26, 245–255. [Google Scholar] [CrossRef]
- Millner, A.J.; Lee, M.D.; Nock, M.K. Single-Item Measurement of Suicidal Behaviors: Validity and Consequences of Misclassification. PLoS ONE 2015, 10, e0141606. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Gender | Profiles | AIC | BIC | SSABIC | Entropy | Adj. LRT |
|---|---|---|---|---|---|---|
| Male | 2 | 10,331.98 | 10,384.46 | 10,352.69 | 0.95 | - |
| 3 | 7768.593 | 7842.062 | 7797.589 | 0.99 | 0.049 | |
| 4 | 7313.878 | 7408.338 | 7351.159 | 0.91 | 0.000 | |
| 5 | 7263.248 | 7378.700 | 7308.814 | 0.90 | 0.001 | |
| 6 | 7200.809 | 7337.252 | 7254.660 | 0.87 | 0.167 | |
| Female | 2 | 9517.120 | 9567.895 | 9536.131 | 0.75 | - |
| 3 | 8077.246 | 8148.331 | 8103.862 | 0.99 | 0.015 | |
| 4 | 7904.613 | 7996.008 | 7938.833 | 0.91 | 0.000 | |
| 5 | 7882.058 | 7993.763 | 7923.883 | 0.87 | 0.007 | |
| 6 | 7862.872 | 7994.887 | 7912.302 | 0.84 | 0.075 |
| Step 1 | Step 2 | Step 3 | Step 4 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | S.E. | OR | 95% CI | B | S.E. | OR | 95% CI | B | S.E. | OR | 95% CI | B | S.E. | OR | 95% CI | ||
| Male | Constant | 1.22 *** | 0.09 | 3.37 | 0.07 | 0.07 | 1.07 | −1.80 *** | 0.16 | 0.17 | −4.19 *** | 0.44 | 0.02 | ||||
| Sleep | 0.25 ** | 0.09 | 1.28 | [1.06, 1.54] | 0.18 * | 0.09 | 1.19 | [1.00, 1.42] | 0.11 | 0.14 | 1.12 | [0.86, 1.47] | 0.63 ** | 0.24 | 1.87 | [1.17, 2.98] | |
| Headache | 0.08 | 0.10 | 1.08 | [0.90, 1.31] | 0.11 | 0.1 | 1.12 | [0.92, 1.37] | 0.27 | 0.17 | 1.31 | [0.94, 1.84] | 0.92 ** | 0.29 | 2.5 | [1.41, 4.45] | |
| Nausea | 0.19 | 0.11 | 1.20 | [0.97, 1.49] | 0.18 | 0.10 | 1.2 | [0.98, 1.47] | 0.07 | 0.16 | 1.07 | [0.78, 1.47] | −0.16 | 0.3 | 0.85 | [0.48, 1.53] | |
| Stomach Ache | 0.21 * | 0.10 | 1.23 | [1.01, 1.50] | 0.23 * | 0.09 | 1.26 | [1.05, 1.51] | 0.19 | 0.15 | 1.20 | [0.90,1.60] | 0.24 | 0.26 | 1.27 | [0.76, 2.13] | |
| Appetite | 0.28 ** | 0.09 | 1.32 | [1.11, 1.56] | 0.06 | 0.09 | 1.06 | [0.89, 1.28] | 0.25 | 0.16 | 1.28 | [0.93, 1.75] | 0.44 | 0.3 | 1.55 | [0.87, 2.78] | |
| Tiredness | 0.37 *** | 0.08 | 1.45 | [1.23, 1.71] | −0.07 | 0.09 | 0.93 | [0.77, 1.12] | 0.07 | 0.17 | 1.08 | [0.77, 1.50] | 0.98 ** | 0.32 | 2.68 | [1.44, 4.97] | |
| Breathing | 0.43 *** | 0.11 | 1.53 | [1.25, 1.89] | 0.22 * | 0.09 | 1.25 | [1.04, 1.49] | 0.02 | 0.15 | 1.02 | [0.77, 1.35] | 0.07 | 0.25 | 1.07 | [0.66, 1.73] | |
| Fever | 0.86 *** | 0.13 | 2.37 | [1.85, 3.02] | 0.05 | 0.10 | 1.05 | [0.87, 1.27] | −0.04 | 0.16 | 0.96 | [0.69, 1.32] | 0.28 | 0.27 | 1.32 | [0.78, 2.22] | |
| Step 1 | Step 2 | Step 3 | Step 4 | ||||||||||||||
| B | S.E. | OR | 95% CI | B | S.E. | OR | 95%CI | B | S.E. | OR | 95%CI | B | S.E. | OR | 95%CI | ||
| Female | Constant | 1.23 | 0.09 | 3.42 | 0.62 | 0.08 | 1.86 | −1.21 | 0.12 | 0.30 | −2.35 | 0.25 | 0.1 | ||||
| Sleep | 0.36 ** | 0.10 | 1.43 | [1.17, 1.75] | 0.28 ** | 0.09 | 1.33 | [1.11, 1.59] | 0.23 * | 0.10 | 1.26 | [1.04, 1.54] | 0.00 | 0.22 | 1 | [0.65, 1.52] | |
| Headache | −0.08 | 0.11 | 0.92 | [0.75, 1.14] | 0.16 | 0.11 | 1.17 | [0.94, 1.45] | 0.16 | 0.13 | 1.18 | [0.91, 1.52] | −0.05 | 0.26 | 0.95 | [0.57, 1.58] | |
| Nausea | 0.37 ** | 0.12 | 1.44 | [1.14, 1.82] | −0.08 | 0.11 | 0.92 | [0.75, 1.14] | 0.03 | 0.12 | 1.03 | [0.81, 1.32] | 0.24 | 0.25 | 1.27 | [0.77, 2.09] | |
| Stomach Ache | 0.25 ** | 0.11 | 1.28 | [1.04, 1.58] | 0.05 | 0.09 | 1.05 | [0.87, 1.26] | −0.02 | 0.10 | 0.98 | [0.80, 1.20] | 0.55 ** | 0.19 | 1.74 | [1.19, 2.54] | |
| Appetite | 0.30 ** | 0.09 | 1.35 | [1.12, 1.61] | 0.09 | 0.09 | 1.1 | [0.92, 1.31] | −0.11 | 0.11 | 0.89 | [0.72, 1.11] | 0.05 | 0.23 | 1.06 | [0.67, 1.66] | |
| Tiredness | 0.3 ** | 0.09 | 1.35 | [1.14, 1.60] | 0.05 | 0.09 | 1.05 | [0.87, 1.27] | 0.30 * | 0.12 | 1.34 | [1.06, 1.70] | 0.36 | 0.26 | 1.43 | [0.86, 2.39] | |
| Breathing | 0.38 ** | 0.12 | 1.46 | [1.16, 1.83] | 0.26 ** | 0.10 | 1.29 | [1.07, 1.56] | 0.09 | 0.11 | 1.10 | [0.89, 1.35] | 0.25 | 0.20 | 1.28 | [0.87, 1.90] | |
| Fever | 0.22 | 0.12 | 1.24 | [0.99, 1.56] | 0.11 | 0.10 | 1.11 | [0.91, 1.37] | 0.23 | 0.12 | 1.26 | [0.99, 1.59] | −0.03 | 0.23 | 0.97 | [0.61, 1.54] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Donnelly, H.K.; Richardson, D.; Solberg, S.V. Understanding Somatic Symptoms Associated with South Korean Adolescent Suicidal Ideation, Depression, and Social Anxiety. Behav. Sci. 2021, 11, 151. https://doi.org/10.3390/bs11110151
Donnelly HK, Richardson D, Solberg SV. Understanding Somatic Symptoms Associated with South Korean Adolescent Suicidal Ideation, Depression, and Social Anxiety. Behavioral Sciences. 2021; 11(11):151. https://doi.org/10.3390/bs11110151
Chicago/Turabian StyleDonnelly, Hayoung Kim, Danielle Richardson, and Scott V. Solberg. 2021. "Understanding Somatic Symptoms Associated with South Korean Adolescent Suicidal Ideation, Depression, and Social Anxiety" Behavioral Sciences 11, no. 11: 151. https://doi.org/10.3390/bs11110151
APA StyleDonnelly, H. K., Richardson, D., & Solberg, S. V. (2021). Understanding Somatic Symptoms Associated with South Korean Adolescent Suicidal Ideation, Depression, and Social Anxiety. Behavioral Sciences, 11(11), 151. https://doi.org/10.3390/bs11110151







