Factors which Influence Risk Taking and the Evolution of Social-Identity in Stroke Narratives: A Thematic Synthesis
Abstract
1. Introduction
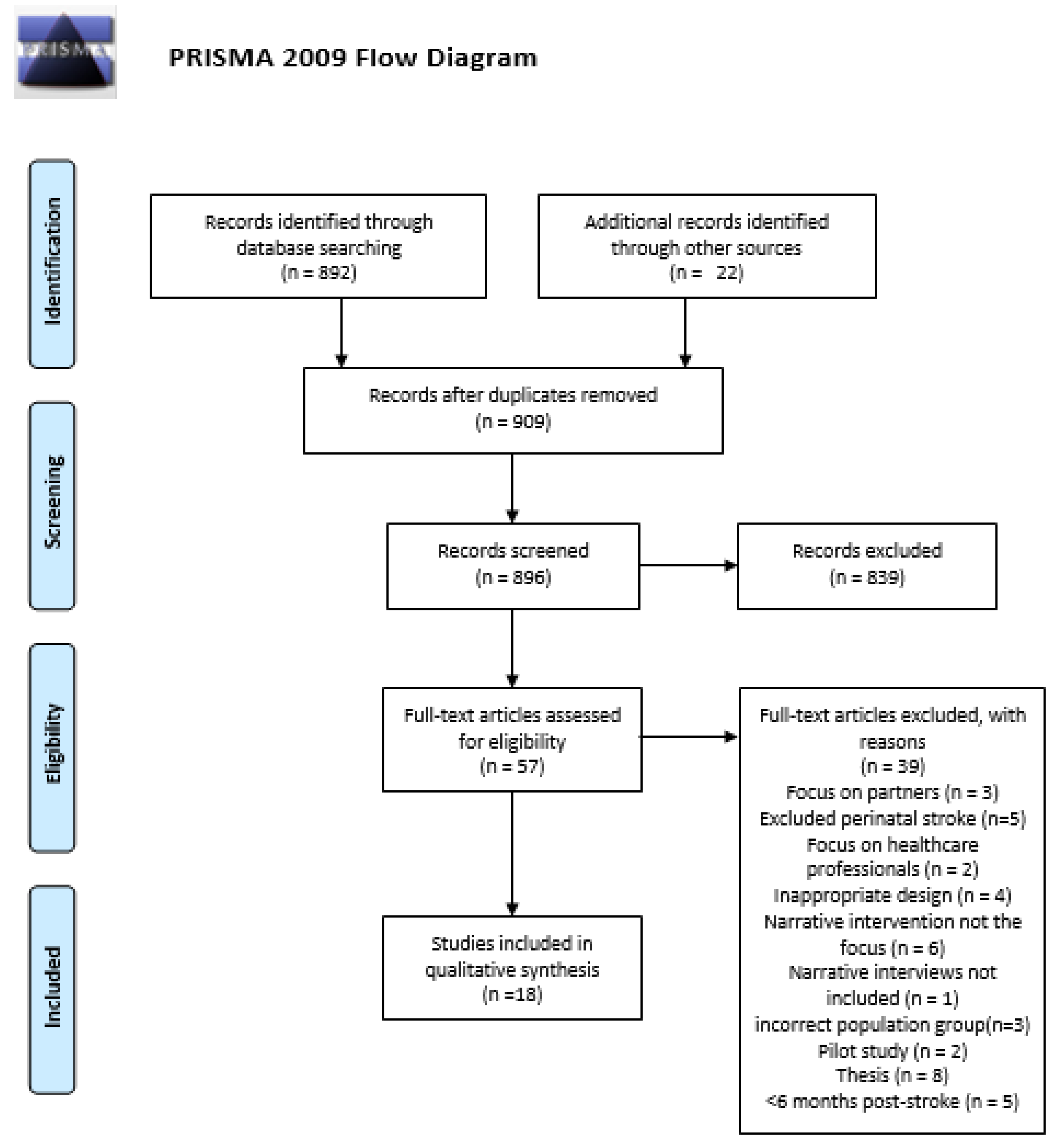
2. Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.2.1. P
2.2.2. I
2.2.3. C
2.2.4. O
2.2.5. S
2.3. Other Criteria
2.4. The Search Process
2.5. Study Selection
2.6. Data Collection
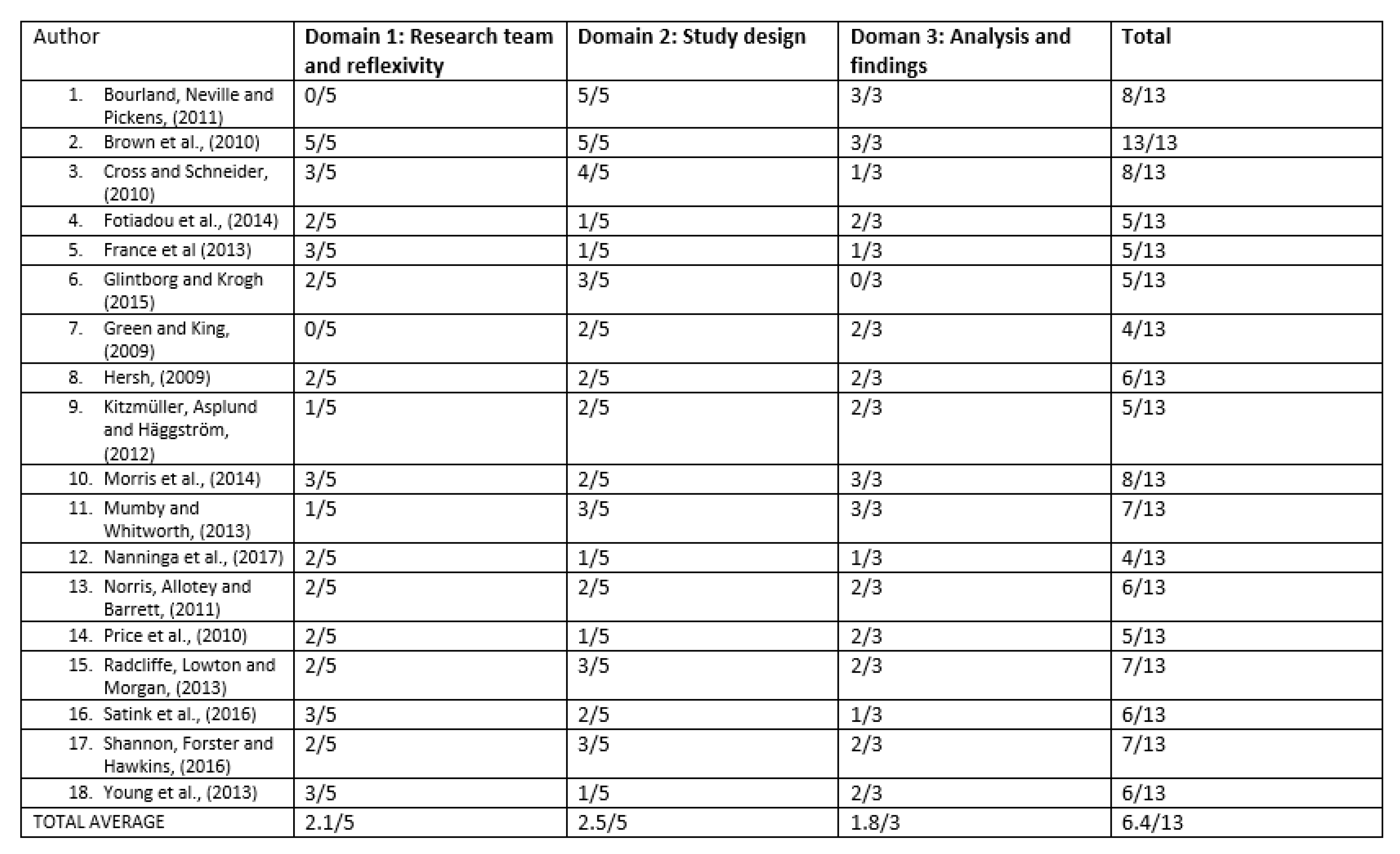
2.7. Study Quality Assessment
2.8. Synthesis
2.9. Trustworthiness
3. Results
3.1. Demographics
3.2. Quality Appraisal
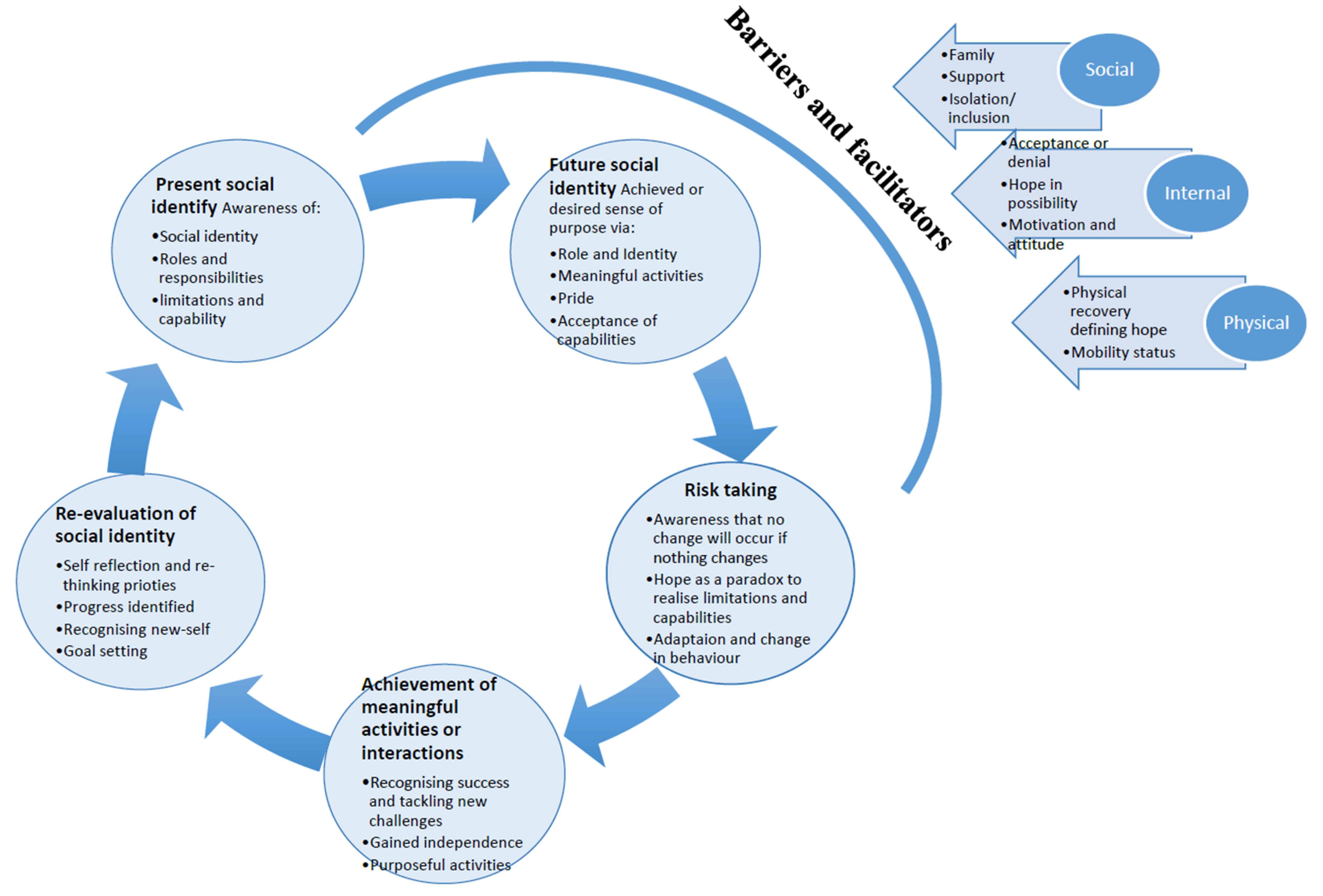
3.3. Synthesis
3.3.1. Stage 1 Present Social Identity:
3.3.2. Stage 2: Future Social Identity
3.3.3. Stage 3: Risk Taking
3.3.4. Stage 4: Achievement of Meaningful Activities or Interactions
3.3.5. Stage 5: Re-evaluation of Social Identity
3.3.6. Factors that can Influence Social Identity Evolution
4. Discussion
4.1. Clinical Implications
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Level of Hope associated with difficulty | Circle a number reflecting the statements on the left |
| I am completely certain and have no doubt that I will be able to overcome this difficulty | +4 |
| I am certain that I will be able to overcome this difficulty | +3 |
| I believe it is likely that I will overcome this difficulty | +2 |
| I believe it is possible to overcome this difficulty | +1 |
| I accept that it might not be possible to overcome this difficulty | 0 |
| I feel uncertain and don’t know if this difficulty can be overcome | −1 |
| I feel that it is likely that I wont overcome this difficulty | −2 |
| I have little hope or ability to overcome this difficulty | −3 |
| I see neither hope or ability to overcome this difficulty | −4 |
| Ability to adapt to the difficulty | Circle a number reflecting the statements on the left |
| I am able to positively embrace and use this difficulty for benefit | +4 |
| I am able to fully accept and embrace this difficulty | +3 |
| I am able to fully accept this difficulty | +2 |
| I acknowledge this difficulty but can’t fully accept it | +1 |
| I am able to acknowledge this difficulty | 0 |
| I struggle with acknowledging this difficulty | −1 |
| I find it difficult to accept this difficulty | −2 |
| I find it very difficult to accept this difficulty | −3 |
| I reject and cannot accept this difficulty | −4 |
References
- Stroke Association. A New Era for Stroke. 2016. Available online: https://www.stroke.org.uk/get-involved/campaigning/new-era-for-stroke (accessed on 29 May 2019).
- Feigin, V.L.; Forouzanfar, M.H.; Krishnamurthi, R.; A Mensah, G.; Connor, M.; A Bennett, D.; E Moran, A.; Sacco, R.L.; Anderson, L.; Truelsen, T.; et al. Global and regional burden of stroke during 1990–2010: Findings from the Global Burden of Disease Study 2010. Lancet 2014, 383, 245–254. [Google Scholar] [CrossRef]
- Mallick, A.A.; O’Callaghan, F.J. The epidemiology of childhood stroke. Eur. J. Paediatr. Neurol. 2010, 14, 197–205. [Google Scholar] [CrossRef]
- Department of Health. Quality and outcomes framework (QOF) achievement data 2015/2016. 2016. Available online: https://www.health-ni.gov.uk/publications/quality-and-outcomes-framework-qof-achievement-data-201516 (accessed on 29 May 2019).
- De Wit, L.; Theuns, P.; Dejaeger, E.; Devos, S.; Gantenbein, A.R.; Kerckhofs, E.; Schuback, B.; Schupp, W.; Putman, K. Long-term impact of stroke on patients’ health-related quality of life. Disabil. Rehabil. 2016, 39, 1435–1440. [Google Scholar] [CrossRef]
- Tajfel, H. Social categorization. English manuscript of ‘Le categorisation sociale’. In Introduction a la Psychologie Sociale; Moscovici, S., Ed.; Larousse Université: Paris, France, 1972; Volume 1, pp. 272–302. [Google Scholar]
- Hackett, M.L.; Glozier, N.; Jan, S.; Lindley, R. Returning to Paid Employment after Stroke: The Psychosocial Outcomes In StrokE (POISE) Cohort Study. PLoS ONE 2012, 7, e41795. [Google Scholar] [CrossRef] [PubMed]
- Mumby, K.; Whitworth, A. Adjustment processes in chronic aphasia after stroke: Exploring multiple perspectives in the context of a community-based intervention. Aphasiology 2013, 27, 462–489. [Google Scholar] [CrossRef]
- Rudd, A.G.; Bowen, A.; Young, G.R.; A James, M. The latest national clinical guideline for stroke. Clin. Med. 2017, 17, 154–155. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.; Whitfield, K. Social identity and stroke: ‘they don’t make me feel like, there’s something wrong with me’. Scand. J. Caring Sci. 2012, 27, 820–830. [Google Scholar] [CrossRef] [PubMed]
- Northcott, S.; Moss, B.; Harrison, K.; Hilari, K. A systematic review of the impact of stroke on social support and social networks: Associated factors and patterns of change. Clin. Rehabil. 2015, 30, 811–831. [Google Scholar] [CrossRef]
- Woodman, P.; Riazi, A.; Pereira, C.; Jones, F. Social participation post stroke: A meta-ethnographic review of the experiences and views of community-dwelling stroke survivors. Disabil. Rehabil. 2013, 36, 2031–2043. [Google Scholar] [CrossRef]
- Hole, E.; Stubbs, B.; Roskell, C.; Soundy, A. The Patient’s Experience of the Psychosocial Process That Influences Identity following Stroke Rehabilitation: A Metaethnography. Sci. World J. 2014, 2014. [Google Scholar] [CrossRef]
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res. Methodol. 2008, 8, 45. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Moher, D. Evaluations of the uptake and impact of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Statement and extensions: A scoping review. Syst. Rev. 2017, 6, 263. [Google Scholar] [CrossRef] [PubMed]
- Maruatona, T.L. Foundations of qualitative research: Interpretive and critical approaches by W. Jerry Willis. New Horiz. Adult Educ. Hum. Resour. Dev. 2013, 25, 83–85. [Google Scholar] [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Heal. Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef]
- Mahendran, N.; Kuys, S.S.; Brauer, S.G. Accelerometer and Global Positioning System Measurement of Recovery of Community Ambulation Across the First 6 Months After Stroke: An Exploratory Prospective Study. Arch. Phys. Med. Rehabil. 2016, 97, 1465–1472. [Google Scholar] [CrossRef]
- Soundy, A.; Roskell, C.; Elder, T.; Collett, J.; Dawes, H. The Psychological Processes of Adaptation and Hope in Patients with Multiple Sclerosis: A Thematic Synthesis. Open J. Ther. Rehabil. 2016, 4, 22–47. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Heal. Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Campbell, R.; Pound, P.; Morgan, M.; Daker-White, G.; Britten, N.; Pill, R.; Yardley, L.; Pope, C.; Donovan, J. Evaluating meta-ethnography: Systematic analysis and synthesis of qualitative research. Heal. Technol. Assess. 2011, 15. [Google Scholar] [CrossRef]
- Thorne, S.; Jensen, L.; Kearney, M.H.; Noblit, G.; Sandelowski, M. Qualitative meta-synthesis: Reflections on methodolgoical orientation and ideological agenda. Qual. Heal. Res. 2004, 14, 1342–1365. [Google Scholar] [CrossRef]
- Tong, A.; Flemming, K.; McInnes, E.; Oliver, S.; Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res. Methodol. 2012, 12, 181. [Google Scholar] [CrossRef]
- Bourland, E.L.R.; Neville, M.A.; Pickens, N.D. Loss, Gain, and the Reframing of Perspectives in Long-Term Stroke Survivors: A Dynamic Experience of Quality of Life. Top. Stroke Rehabil. 2011, 18, 437–449. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.; Worrall, L.; Davidson, B.; Howe, T.; Hudson, K. Snapshots of success: An insider perspective on living successfully with aphasia. Aphasiology 2010, 24, 1267–1295. [Google Scholar] [CrossRef]
- Cross, A.; Schneider, M. A preliminary qualitative analysis of the impact of hope on stroke recovery in women. Top. Stroke Rehabil. 2010, 17, 484–495. [Google Scholar] [CrossRef] [PubMed]
- Fotiadou, D.; Northcott, S.; Chatzidaki, A.; Hilari, K. Aphasia blog talk: How does stroke and aphasia affect a person’s social relationships? Aphasiology 2014, 28, 1281–1300. [Google Scholar] [CrossRef]
- France, E.; Hunt, K.; Dow, C.; Wyke, S. Do men’s and women’s accounts of surviving a stroke conform to Frank’s narrative genres? Qual. Heal. Res. 2013, 23, 1649–1659. [Google Scholar] [CrossRef]
- Glintborg, C.; Krogh, L. The psychological challenges of identity reconstruction following an acquired brain injury. Narrat. Works 2015, 5, 50–70. [Google Scholar]
- Green, T.L.; King, K.M. Experiences of male patients and wife-caregivers in the first year post-discharge following minor stroke: A descriptive qualitative study. Int. J. Nurs. Stud. 2009, 46, 1194–1200. [Google Scholar] [CrossRef]
- Hersh, D. How do people with aphasia view their discharge from therapy? Aphasiology 2009, 23, 331–350. [Google Scholar] [CrossRef]
- Kitzmüller, G.; Asplund, K.; Häggström, T. The Long-Term Experience of Family Life After Stroke. J. Neurosci. Nurs. 2012, 44, E1–E13. [Google Scholar] [CrossRef]
- Morris, J.H.; Oliver, T.; Kroll, T.; Joice, S.; Williams, B. From physical and functional to continuity with pre-stroke self and participation in valued activities: A qualitative exploration of stroke survivors’, carers’ and physiotherapists’ perceptions of physical activity after stroke. Disabil. Rehabil. 2014, 37, 64–77. [Google Scholar] [CrossRef]
- Nanninga, C.S.; Meijering, L.; Postema, K.; Schönherr, M.C.; Lettinga, A.T. Unpacking community mobility: A preliminary study into the embodied experiences of stroke survivors. Disabil. Rehabil. 2017, 40, 2015–2024. [Google Scholar] [CrossRef] [PubMed]
- Norris, M.; Allotey, P.; Barrett, G. ‘It burdens me’: The impact of stroke in central Aceh, Indonesia. Sociol. Heal. Illn. 2011, 34, 826–840. [Google Scholar] [CrossRef] [PubMed]
- Price, P.; Kinghorn, J.; Patrick, R.; Cardell, B. “Still there is beauty”: One man’s resilient adaptation to stroke. Scand. J. Occup. Ther. 2010, 19, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Radcliffe, E.; Morgan, M.; Lowton, K. Co-construction of chronic illness narratives by older stroke survivors and their spouses. Sociol. Heal. Illn. 2013, 35, 993–1007. [Google Scholar] [CrossRef] [PubMed]
- Satink, T.; Josephsson, S.; Zajec, J.; Cup, E.H.C.; De Swart, B.J.M.; Der Sanden, M.W.G.N.-V. Negotiating role management through everyday activities: Narratives in action of two stroke survivors and their spouses. Disabil. Rehabil. 2016, 38, 2354–2364. [Google Scholar] [CrossRef] [PubMed]
- Shannon, R.L.; Forster, A.; Hawkins, R.J. A qualitative exploration of self-reported unmet need one year after stroke. Disabil. Rehabil. 2016, 38, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Young, C.; Mills, R.; Gibbons, C.; Thornton, E. Poststroke Fatigue: The Patient Perspective. Top. Stroke Rehabil. 2013, 20, 478–484. [Google Scholar] [CrossRef]
- Corsten, S.; Schimpf, E.J.; Konradi, J.; Keilmann, A.; Hardering, F. The participants’ perspective: How biographic-narrative intervention influences identity negotiation and quality of life in aphasia. Int. J. Lang. Commun. Disord. 2015, 50, 788–800. [Google Scholar] [CrossRef]
- Törnbom, K.; Lundälv, J.; Sunnerhagen, K.S. Long-term participation 7-8 years after stroke: Experiences of people in working-age. PLoS ONE 2019, 14, e0213447. [Google Scholar]
- Gibbs, G.; Flick, U. Analyzing Qualitative Data; Sage Publishing Ltd.: London, UK, 2018. [Google Scholar]
- Soundy, A.; Smith, B.; Dawes, H.; Pall, H.; Gimbrere, K.; Ramsay, J. Patient’s expression of hope and illness narratives in three neurological conditions: A meta-ethnography. Heal. Psychol. Rev. 2013, 7, 177–201. [Google Scholar] [CrossRef]
- Sulistová, R.; Stasková, V.; Kaas, J.; Kimmer, D.; Treslova, M.; Olišarová, V.; Filausová, D. Participation of adult patients in healthcare. Neuroendocrinol. Lett. 2016, 37, 21–31. [Google Scholar]
- Wilson, T.; Holt, T.; Greenhalgh, T. Complexity science: Complexity and clinical care. BMJ 2001, 323, 685–688. [Google Scholar] [CrossRef]
- Soundy, A.; Reid, K. The Psychosocial Impact and Value of Participating in a Storytelling Intervention for Patients Diagnosed with Cancer: An Integrative Review. Open J. Ther. Rehabil. 2019, 7, 35–77. [Google Scholar] [CrossRef]
- Soundy, A.; Rosenbaum, S.; Elder, T.; Kyte, D.; Stubbs, B.; Hemmings, L.; Roskell, C.; Collett, J.; Dawes, H. The Hope and Adaptation Scale (HAS): Establishing Face and Content Validity. Open J. Ther. Rehabil. 2016, 4, 76–86. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Higgs, R.; Soundy, A. Factors which Influence Risk Taking and the Evolution of Social-Identity in Stroke Narratives: A Thematic Synthesis. Behav. Sci. 2020, 10, 46. https://doi.org/10.3390/bs10020046
Higgs R, Soundy A. Factors which Influence Risk Taking and the Evolution of Social-Identity in Stroke Narratives: A Thematic Synthesis. Behavioral Sciences. 2020; 10(2):46. https://doi.org/10.3390/bs10020046
Chicago/Turabian StyleHiggs, Richard, and Andrew Soundy. 2020. "Factors which Influence Risk Taking and the Evolution of Social-Identity in Stroke Narratives: A Thematic Synthesis" Behavioral Sciences 10, no. 2: 46. https://doi.org/10.3390/bs10020046
APA StyleHiggs, R., & Soundy, A. (2020). Factors which Influence Risk Taking and the Evolution of Social-Identity in Stroke Narratives: A Thematic Synthesis. Behavioral Sciences, 10(2), 46. https://doi.org/10.3390/bs10020046





