Process Evaluation of a Personality Targeted Intervention for Addictive Eating in Australian Adults
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Intervention
2.4. Training of Intervention Providers
2.5. Measures
2.5.1. Intervention Delivery
2.5.2. Program Acceptability—Participants
2.5.3. Program Acceptability—Intervention Providers
2.6. Statistical Analysis
3. Results
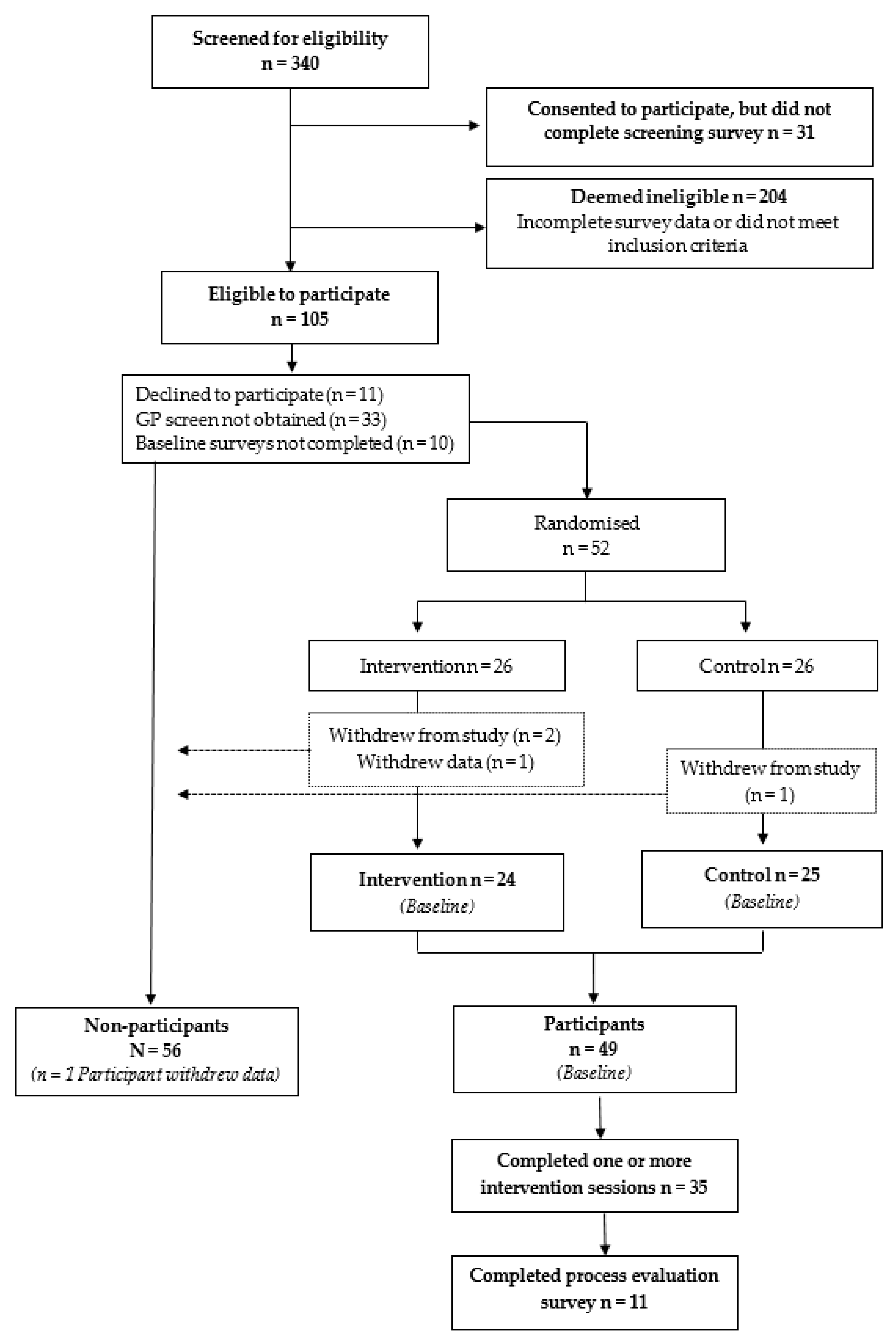
3.1. Participants
3.2. Intervention Delivery
3.3. Program Acceptability—Participants
3.4. Program Acceptability—Intervention Providers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Meule, A. Back by Popular Demand: A Narrative Review on the History of Food Addiction Research. Yale J. Biol. Med. 2015, 88, 295–302. [Google Scholar] [PubMed]
- Bąk-Sosnowska, M. Differential criteria for binge eating disorder and food addiction in the context of causes and treatment of obesity. Psychiatr. Pol. 2017, 51, 247–259. [Google Scholar] [CrossRef] [PubMed]
- Vella, S.C.; Pai, N.B. A narrative review of potential treatment strategies for food addiction. Eat. Weight. Disord. 2017, 1, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Ivezaj, V.; Wiedemann, A.A.; Grilo, C.M. Food addiction and bariatric surgery: A systematic review of the literature. Obes. Rev. 2017, 18, 1386–1397. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.L.; Skinner, J.; McKenna, R.; Rollo, M. Food Addiction, Binge Eating Disorder, and Obesity: Is There a Relationship? Behav. Sci. 2017, 7, 54. [Google Scholar] [CrossRef] [PubMed]
- Gordon, E.L.; Ariel-Donges, A.H.; Bauman, V.; Merlo, L.J. What Is the Evidence for ℌFood Addiction?ℍ A Systematic Review. Nutrients 2018, 10, 477. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Development of the Yale Food Addiction Scale Version 2.0. Psychol. Addict. Behav. 2016, 30, 113–121. [Google Scholar] [CrossRef]
- Lee, N.M.; Hall, W.D.; Lucke, J.; Forlini, C.; Carter, A. Food addiction and its impact on weight-based stigma and the treatment of obese individuals in the U.S. and Australia. Nutrients 2014, 6, 5312–5326. [Google Scholar] [CrossRef]
- Pursey, K.M.; Stanwell, P.; Gearhardt, A.N.; Collins, C.E.; Burrows, T.L. The prevalence of food addiction as assessed by the Yale Food Addiction Scale: A systematic review. Nutrients 2014, 6, 4552–4590. [Google Scholar] [CrossRef]
- Penzenstadler, L.; Soares, C.; Karila, L.; Khazaal, Y. Systematic Review of Food Addiction as Measured With the Yale Food Addiction Scale: Implications for the Food Addiction Construct. Curr. Neuropharmacol. 2018, 16, 1–13. [Google Scholar] [CrossRef]
- Pedram, P.; Wadden, D.; Amini, P.; Gulliver, W.; Randell, E.; Cahill, F.; Vasdev, S.; Goodridge, A.; Carter, J.C.; Zhai, G.; et al. Food Addiction: Its Prevalence and Significant Association with Obesity in the General Population. PLoS ONE 2013, 8, e74832. [Google Scholar] [CrossRef] [PubMed]
- McKenna, R.A.; Rollo, M.E.; Skinner, J.A.; Burrows, T.L. Food Addiction Support: Website Content Analysis. JMIR Cardio 2018, 2, e10. [Google Scholar] [CrossRef] [PubMed]
- Cassin, S.E.; Sijercic, I.; Montemarano, V. Psychosocial Interventions for Food Addiction: A Systematic Review. Curr. Addict. Rep. 2020, 7, 9–19. [Google Scholar] [CrossRef]
- Sackett, D.L.; Straus, S.E.; Richardson, W.S.; Rosenberg, W.; Haynes, R.B. Evidence-Based Medicine: How to Practice and Teach EBM, 2nd ed.; Churchill Livingstone: London, UK, 2000. [Google Scholar]
- Fletcher, P.C.; Kenny, P.J. Food addiction: A valid concept? Neuropsychopharmacology 2018, 43, 2506–2513. [Google Scholar] [CrossRef] [PubMed]
- Davis, C. From passive overeating to “food addiction”: A spectrum of compulsion and severity. ISRN Obes. 2013, 2013, 435027. [Google Scholar] [CrossRef] [PubMed]
- Hides, L.; Kavanagh, D.J.; Daglish, M.; Cotton, S.; Connor, J.P.; Barendregt, J.J.; Young, R.M.; Sanders, D.; White, A.; Mergard, L. The Quik Fix study: A randomised controlled trial of brief interventions for young people with alcohol-related injuries and illnesses accessing emergency department and crisis support care. BMC Emerg. Med. 2014, 14, 19. [Google Scholar] [CrossRef]
- Borrelli, B. The Assessment, Monitoring, and Enhancement of Treatment Fidelity In Public Health Clinical Trials. J. Public Health Dent. 2011, 71, S52–S63. [Google Scholar] [CrossRef]
- Murphy, S.L.; Gutman, S.A. Intervention fidelity: A necessary aspect of intervention effectiveness studies. Am. J. Occup. Ther. 2012, 66, 387–388. [Google Scholar] [CrossRef]
- Resnick, B.; Inguito, P.; Orwig, D.; Yahiro, J.Y.; Hawkes, W.; Werner, M.; Zimmerman, S.; Magaziner, J. Treatment Fidelity in Behavior Change Research: A Case Example. Nurs. Res. 2005, 54, 139–143. [Google Scholar] [CrossRef]
- Burrows, T.; Collins, R.; Rollo, M.; Leary, M.; Hides, L.; Davis, C. The feasibility of a personality targeted intervention for addictive overeating: FoodFix. Appetite 2020. Currently under review. [Google Scholar] [CrossRef]
- Chai, L.K.; Collins, C.E.; May, C.; Brown, L.J.; Burrows, T.L. Fidelity and acceptability of a family-focused technology-based telehealth intervention for child weight management. J. Telemed. Telecare 2019. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.; Hides, L.; Brown, R.; Dayas, C.V.; Kay-Lambkin, F. Differences in Dietary Preferences, Personality and Mental Health in Australian Adults with and without Food Addiction. Nutrients 2017, 9, 285. [Google Scholar] [CrossRef] [PubMed]
- Schulte, E.M.; Gearhardt, A.N. Development of the Modified Yale Food Addiction Scale Version 2.0. Eur. Eat. Disord. Rev. 2017, 25, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Cotter, E.W.; Kelly, N.R. Binge Eating Scale (BES). In Encyclopedia of Feeding and Eating Disorders; Wade, T., Ed.; Springer Singapore: Singapore, 2016; pp. 1–5. [Google Scholar]
- Woicik, P.A.; Stewart, S.H.; Pihl, R.O.; Conrod, P.J. The substance use risk profile scale: A scale measuring traits linked to reinforcement-specific substance use profiles. Addict. Behav. 2009, 34, 1042–1055. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations of thought and action: A Social Cognitive Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Mattoo, S.K.; Prasad, S.; Ghosh, A. Brief intervention in substance use disorders. Indian J. Psychiatry 2018, 60, S466–S472. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Socio-Economic Indexes for Areas. Available online: https://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa (accessed on 3 February 2020).
- Iacovino, J.M.; Gredysa, D.M.; Altman, M.; Wilfley, D.E. Psychological treatments for binge eating disorder. Curr. Psychiatry Rep. 2012, 14, 432–446. [Google Scholar] [CrossRef] [PubMed]
- Linardon, J.; Hindle, A.; Brennan, L. Dropout from cognitive-behavioral therapy for eating disorders: A meta-analysis of randomized, controlled trials. Int. Eat. Disord. 2018, 51. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, D.M.; Borsari, B.; Levine, M.J.; Li, S.; Lamberson, K.A.; Matta, L.A. A Systematic Review of the mHealth Interventions to Prevent Alcohol and Substance Abuse. J. Health Commun. 2017, 22, 413–432. [Google Scholar] [CrossRef] [PubMed]
- Giroux, I.; Goulet, A.; Mercier, J.; Jacques, C.; Bouchard, S. Online and Mobile Interventions for Problem Gambling, Alcohol, and Drugs: A Systematic Review. Front. Psychol. 2017, 8. [Google Scholar] [CrossRef]
- Durland, L.; Interian, A.; Pretzer-Aboff, I.; Dobkin, R.D. effect of telehealth-to-home interventions on quality of life for individuals with depressive and anxiety disorders. Smart Homecare Technol. TeleHealth 2014, 2, 105–119. [Google Scholar]
- Edalati, H.; Conrod, P.J. A Review of Personality-Targeted Interventions for Prevention of Substance Misuse and Related Harm in Community Samples of Adolescents. Front. Psychiatry 2019, 9, 770. [Google Scholar] [CrossRef] [PubMed]
- Conrod, P.J. Personality-Targeted Interventions for Substance Use and Misuse. Curr. Addict. Rep. 2016, 3, 426–436. [Google Scholar] [CrossRef] [PubMed]
- Rose, G.; Smith, L. Mental health recovery, goal setting and working alliance in an Australian community-managed organisation. Health Psychol. Open 2018, 5, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ashton, L.M.; Sharkey, T.; Whatnall, M.C.; Haslam, R.L.; Bezzina, A.; Aguiar, E.J.; Collins, C.E.; Hutchesson, M.J. Which behaviour change techniques within interventions to prevent weight gain and/or initiate weight loss improve adiposity outcomes in young adults? A systematic review and meta-analysis of randomized controlled trials. Obes. Rev. 2020, 21, e13009. [Google Scholar] [CrossRef] [PubMed]
- Ruddock, H.K.; Christiansen, P.; Halford, J.C.G.; Hardman, C.A. The development and validation of the Addiction-like Eating Behaviour Scale. Int. J. Obes. (Lond.) 2017, 41, 1710–1717. [Google Scholar] [CrossRef] [PubMed]
- Hebebrand, J.; Albayrak, Ö.; Adan, R.; Antel, J.; Dieguez, C.; de Jong, J.; Leng, G.; Menzies, J.; Mercer, J.G.; Murphy, M.; et al. “Eating addiction”, rather than “food addiction”, better captures addictive-like eating behavior. Neurosci. Biobehav. Rev. 2014, 47, 295–306. [Google Scholar] [CrossRef]
- Lacroix, E.; Oliveira, E.; Saldanha de Castro, J.; Cabral, J.R.; Tavares, H.; von Ranson, K.M. “There is no way to avoid the first bite”: A qualitative investigation of addictive-like eating in treatment-seeking Brazilian women and men. Appetite 2019, 137, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Paterson, C.; Lacroix, E.; von Ranson, K.M. Conceptualizing addictive-like eating: A qualitative analysis. Appetite 2019, 141, 104326. [Google Scholar] [CrossRef]
- Ruddock, H.K.; Dickson, J.M.; Field, M.; Hardman, C.A. Eating to live or living to eat? Exploring the causal attributions of self-perceived food addiction. Appetite 2015, 95, 262–268. [Google Scholar] [CrossRef]
| Intervention Session | ||
|---|---|---|
| Session Two | Intervention (n = 22) | Control (n = 17) |
| Scheduled days since baseline | 14 | 14 |
| Median (IQR) days since baseline | 16 (14–18) a | 16 (14–21) a |
| Number (%) of participants with good adherence to session scheduling | 17 (77) | 14 (82) |
| Number (%) of participants rescheduling b | 2 (9) | 2 (12) |
| Session Three | Intervention (n = 20) | Control (n = 15) |
| Scheduled days since baseline | 42 | 42 |
| Median (IQR) days since baseline | 51 (44–68) a | 55 (48–69) a |
| Number (%) of participants with good adherence to session scheduling | 10 (50) | 5 (33) |
| Number (%) of participants rescheduling b | 2 (10) | 4 (27) |
| n (%) | |||||
|---|---|---|---|---|---|
| Process Evaluation Items | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
| Pre-treatment questionnaire | |||||
| The questionnaires easy to understand | 4 (36) | 6 (55) | 1 (9) | 0 (0) | 0 (0) |
| The questionnaires easy to complete | 4 (36) | 4 (36) | 2 (18) | 1 (9) | 0 (0) |
| Intervention delivery and timing | |||||
| Over the phone was easier than in person | 7 (64) | 3 (27) | 1 (9) | 0 (0) | 0 (0) |
| The number of sessions was sufficient | 1 (9) | 4 (36) | 5 (45) | 1 (9) | 0 (0) |
| The session durations were appropriate | 4 (36) | 6 (55) | 1 (9) | 0 (0) | 0 (0) |
| The availability of times for sessions was suitable (n = 9) | 5 (56) | 2 (22) | 2 (22) | 0 (0) | 0 (0) |
| Compared with in person, I felt comfortable interacting over the phone | 4 (36) | 5 (45) | 2 (18) | 0 (0) | 0 (0) |
| Intervention content | |||||
| The information provided was useful and helpful | 4 (36) | 6 (55) | 1 (9) | 0 (0) | 0 (0) |
| The information provided helped me change my behaviours | 2 (18) | 5 (45) | 3 (27) | 1 (9) | 0 (0) |
| The sessions motivated me to eat better and make changes | 3 (27) | 5 (45) | 2 (18) | 1 (9) | 0 (0) |
| The sessions helped me achieve my goals | 2 (18) | 1 (9) | 7 (64) | 1 (9) | 0 (0) |
| The goals were personalised to my needs | 4 (36) | 6 (55) | 1 (9) | 0 (0) | 0 (0) |
| The strategies suggested by the dietitian addressed the barriers preventing me from changing my eating behaviours | 3 (27) | 4 (36) | 3 (27) | 1 (9) | 0 (0) |
| The information provided was easy to understand | 7 (64) | 4 (36) | 0 (0) | 0 (0) | 0 (0) |
| I found the summaries I received after the sessions useful | 4 (36) | 6 (55) | 1 (9) | 0 (0) | 0 (0) |
| Intervention providers | |||||
| The dietitian was very knowledgeable | 1 (9) | 8 (73) | 1 (9) | 0 (0) | 1 (9) |
| The dietitian had good communication skills | 1 (9) | 8 (73) | 1 (9) | 0 (0) | 1 (9) |
| I felt comfortable asking the dietitian questions | 1 (9) | 8 (73) | 1 (9) | 0 (0) | 1 (9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.; Chai, L.K.; Collins, R.; Leary, M.; Whatnall, M.; Burrows, T. Process Evaluation of a Personality Targeted Intervention for Addictive Eating in Australian Adults. Behav. Sci. 2020, 10, 186. https://doi.org/10.3390/bs10120186
Yang Y, Chai LK, Collins R, Leary M, Whatnall M, Burrows T. Process Evaluation of a Personality Targeted Intervention for Addictive Eating in Australian Adults. Behavioral Sciences. 2020; 10(12):186. https://doi.org/10.3390/bs10120186
Chicago/Turabian StyleYang, Yive, Li Kheng Chai, Rebecca Collins, Mark Leary, Megan Whatnall, and Tracy Burrows. 2020. "Process Evaluation of a Personality Targeted Intervention for Addictive Eating in Australian Adults" Behavioral Sciences 10, no. 12: 186. https://doi.org/10.3390/bs10120186
APA StyleYang, Y., Chai, L. K., Collins, R., Leary, M., Whatnall, M., & Burrows, T. (2020). Process Evaluation of a Personality Targeted Intervention for Addictive Eating in Australian Adults. Behavioral Sciences, 10(12), 186. https://doi.org/10.3390/bs10120186






