Abstract
It is speculated that lifestyle interventions known to improve diabetic metabolic state may exert their effects via adipokines. The aim of this systematic review and meta-analysis was to evaluate the chronic effects of physical exercise on adiponectin and leptin levels in adult prediabetic and diabetic individuals. PubMed, Embase, Scopus, The Cochrane Library, clinicaltrials.gov, and WHO Clinical Trials Registry were searched for randomized controlled trials. Pooled effects of interventions were assessed as mean difference (MD) with random effects model. Sensitivity analysis was conducted to test data robustness and subgroup analysis for study heterogeneity. Twenty-two trials with 2996 individuals were included in the meta-analysis. Physical exercise increased levels of adiponectin (MD: 0.42 µg/mL; 95% confidence interval (CI), 0.23, 0.60, p < 0.00001, n = 19 trials) and reduced leptin levels (MD: −1.89 ng/mL; 95% CI, −2.64, −1.14, p < 0.00001, n = 14 trials). These results were robust and remained significant after sensitivity analysis. Study heterogeneity was generally high. As for physical exercise modalities, aerobic exercise, but not other modalities, increased adiponectin and reduced leptin levels. In conclusion, physical exercise and, specifically, aerobic exercise, leads to higher adiponectin and lower leptin levels in prediabetic and diabetic adults. However, cautious interpretation of current findings is warranted.
1. Introduction
Diabetes mellitus represents a major global public burden. The number of diseased individuals has quadrupled between 1980 and 2014, rising from 108 million to 422 million [1]. Recent data demonstrate that about 150 million people worldwide suffer from diabetes, a number which is expected to double by 2025 [2]. Diabetic individuals are at a high risk of developing a range of complications, including heart disease, retinopathy, nephropathy, neuropathy, and diabetic foot complications [2]. An estimated 1.8 million deaths in 2012 were due to diabetes worldwide, whilst an additional 2.2 million deaths were associated with complications arising from higher-than-optimal blood glucose [1]. It is projected that, in 2030, diabetes mellitus will be the seventh leading cause of death globally [3]. Overweight and obesity and physical inactivity are major risk factors for developing the disease, as 9 out of 10 diabetic individuals in the United States are overweight or obese, and 4 out of 10 are physically inactive [4]. The pathological dysregulations that eventually lead to diabetes are preceded by prediabetes in most individuals [5]. This early phase represents a major opportunity for preventive interventions. The seminal Diabetes Prevention Program (DPP) showed that a lifestyle intervention including a physical activity component could significantly reduce the incidence of diabetes in high risk individuals, and the effects were even greater than with pharmacotherapy based on metformin [6]. In general, engaging in regular physical activity can reduce the risk of developing diabetes by 30–50% [7]. Even moderate intensity of physical activity, such as brisk walking, seems to offer protective benefits [8]. However, most individuals who are at risk or are already diagnosed with diabetes are not physically active on a regular basis [9]. Regular physical activity is also associated with improved glucose control in individuals already diagnosed with the disease. Physical exercise can reduce glycated haemoglobin HbA(1c) significantly, even in the absence of body weight changes [10], while higher intensity exercise is suggested to offer additional benefits on glycemic control and cardiorespiratory fitness [11]. Different training modalities are employed as strategies for managing abnormal glucose metabolism, including aerobic exercise, resistance exercise, and combined exercise. Both training modalities are important. For instance, aerobic exercise can prevent or change the course of peripheral diabetic neuropathy [12] and improve the cardiac autonomic nervous system function [13]. Resistance exercise was found to alter body composition in favor of lean muscle vs. adipose tissue which results in increased peripheral insulin sensitivity, among a plethora of other mechanisms [14]. In a randomized controlled trial, a combination of aerobic and resistance exercise was better in improving glycemic control than each modality alone [15]. Similar findings were found in a recent meta-analysis, where combined exercise was not only superior for glycemic control, but also in improving blood lipids in patients with diabetes [16]. However, another meta-analysis found that engaging in some form of physical activity is more important than choosing the type itself [17], which is important, given the rates of physically inactive diabetic and prediabetic individuals [18].
The physiological benefits of regular physical activity, as well as guidelines and recommendations on the type and amount, are provided in different guidelines for prevention and treatment of diabetes [18,19,20].
Adipose tissue is not considered an inert energy storage system any more. Since the discovery of leptin in 1994 [21], adipose tissue is regarded as a highly active endocrine system secreting a plethora of signaling molecules collectively known as adipokines [22]. Physical exercise has been found to affect adipose tissue, especially visceral adipose tissue, even in the absence of weight loss, and the effects are suggested to be even greater than with dietary restriction [23]. Leptin regulates a wide range of physiological mechanisms important for obesity and metabolic disorders, including energy balance, neuroendocrine function, and metabolic pathways. Leptin levels are primarily associated with the amount of fat tissue and energy balance. Leptin exerts is effects by binding to its receptor (ObR) in the hypothalamus, activating several signal transduction pathways, such as Janus kinase/signal transducer and activator of transcription-3 (JAK-STAT3), which is involved in the regulation of energy homeostasis, and phosphatidylinositol 3-kinase (PI3K), involved in the regulation of food intake and glucose homeostasis. Ultimately, leptin induces decreased food intake and increased energy expenditure, i.e., it has weight-reducing effects. However, in the state of leptin resistance, which is often found in type 2 diabetes, leptin cannot exert its effects, making these individuals resistant to the weight-reducing effects, even in the presence of hyperleptinemia [24]. Adiponectin is a hormone with anti-inflammatory and cardioprotective functions. Under normal conditions, it is secreted exclusively from adipose tissue. It is found abundantly in the plasma, accounting for 0.01% of plasma proteins in humans. Adiponectin exerts its effects by binding the receptors AdipoR1 and AdipoR2. The anti-inflammatory and cardioprotective properties are mostly due to inhibiting the expression of adhesion molecules, thereby reducing the adherence of monocytes to endothelial cells. In addition, adiponectin reduces plaque formation and increases plaque stability and nitric oxide (NO) production. In the liver, adiponectin reduces glucose output by inhibiting the expression of enzymes for gluconeogenesis. Its expression is paradoxically reduced in obesity, insulin resistance, and type 2 diabetes [25]. Both adipokines are clinically very relevant in prediabetes and diabetes, with the general perception that they exert contrary effects—leptin upregulates proinflammatory pathways which are associated with type 2 diabetes and cardiovascular disease, while adiponectin downregulates them [26]. Physical exercise has been found to affect adiponectin and leptin levels in a favorable manner [27,28], and the effect may be potentiated with dietary co-intervention [29].
The aim of this systematic review and meta-analysis was to synthesize data on the effects of physical exercise, including different exercise modalities, on adiponectin and leptin levels in prediabetic and diabetic individuals.
2. Materials and Methods
2.1. Literature Search
The following databases were searched until 1 March 2018 for randomized controlled trials: PubMed, Embase, Scopus, The Cochrane Library, clinicaltrials.gov, and WHO Clinical Trials Registry. Key words applied in the literature search were exercise, physical activity, training, adipokines, leptin, adiponectin, prediabetes, and diabetes. The reference sections of retrieved trials were also hand searched in order to identify further potentially relevant trials. Systematic reviews and meta-analysis which were identified were also hand-searched for additional trials. The search strategy for PubMed is provided in the Supplementary Material (Figure SX). Our systematic review is registered in PROSPERO (CRD42018098633).
2.2. Study Selection
Studies were included if they were (i) randomized controlled trials involving adults (minimum 18 years of age) with prediabetes (insulin resistance, impaired glucose tolerance, impaired fasting glucose) or type 2 diabetes; (ii) used physical exercise in supervised form, including different exercise modalities (aerobic, resistance, and concurrent exercise) or provided exercise advice to enrolled individuals; (iii) an intervention time of minimum 4 weeks; iv) evaluated adiponectin and/or leptin as outcomes; and (v) reported change in means or baseline and postintervention means with standard deviations for the intervention and control group, or values from which these could be calculated.
Studies were excluded if they (i) lacked a control group; (ii) included individuals with type 1 diabetes; (iii) involved a confounding co-intervention other than diet, e.g., a drug cotreatment; (iii) lacked sufficient information on the outcomes of interest; (iv) were conference abstracts, reviews, case reports, commentaries; and (v) were duplicate publications.
2.3. Risk of Bias Assessment
The Cochrane risk of bias tool [30] was used to evaluate the risk of bias of included trials (low, unclear, high) for the following study characteristics: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias.
2.4. Data Extraction and Analysis
The following data, that were abstracted from every trial, included first author’s last name, publication year, modality of physical exercise, sample size, sex distribution, baseline characteristics (age, body mass index (BMI)), medical condition, number of training sessions per week, intervention duration, dietary co-intervention, and outcome parameters. If several time points were reported for an outcome, then data from the longest follow-up time period was taken. If the trials included multiple different physical exercise interventions, then data were extracted from every intervention arm.
Where reported, changes in group means and corresponding standard deviations (SDs) for levels of adiponectin and leptin were extracted for the intervention and control groups. Otherwise, changes were calculated as the difference between the post-intervention and baseline mean; in this case, SD was calculated for each group, assuming that r = 0.5 [31], as:
If medians or interquartile ranges were reported instead of means, then mean values and SDs were calculated as proposed by Hozo et al. [32].
The statistical analysis was done with Review Manager 5.3 of the Cochrane Collaboration Group [33]. The analysis was done by using the inverse-variance random effects model [34]. Effect size of the intervention was calculated as the pooled estimates of the weighted mean differences (WMD) between the intervention and control groups.
Study heterogeneity was measured by Higgins I2 statistic [35], where a value higher than 50% was considered to represent considerable heterogeneity.
Subgroup analyses were conducted according to preset criteria: (i) intervention duration, where we applied 12 weeks as cut-off [36]; (ii) dietary co-intervention, as it can modulate the effect of exercise [29]; and (iii) number of training sessions per week, based on recent recommendations of the American Diabetes Association [37].
Sensitivity analysis through the leave-one-out method was employed to verify the robustness of data by removing one trial at a time from the meta-analysis, and recalculating the effects with the remaining trials. In addition, sensitivity analysis was also done by leaving out studies which involved prediabetics, and by excluding trials with two or more defined areas of high risk of bias.
Publication bias was inspected through the funnel plot method, where the differences in mean changes are plotted against their standard errors, in order to determine the precision of the studies.
3. Results
3.1. Characteristics of Included Trials
Once all selection criteria were applied, a total of 22 studies with 2996 individuals were included in the analysis [38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. Figure S1 provides an overview of the search strategy.
A total of 19 studies reported adiponectin levels as outcome, while 14 studies reported leptin levels (Table 1). Most studies employed a structured physical exercise program, the majority of which was aerobic exercise. Three studies [39,58,59] provided exercise advice. Multiple different exercise modalities were used in three studies [39,40,51]; therefore, multiple effect sizes were extracted from these studies. Most trials included both sexes; whilst five [38,41,42,45,53] enrolled men only and one [51] women only. The participants were heterogeneous in terms of age (overall range: 36–66 years). Mean BMI of all groups was higher than 25 kg/m2 or 30 kg/m2, hence, the participants included were overweight and obese. The absolute majority of trials enrolled individuals with type 2 diabetes, while three [52,53,59] included prediabetic individuals. The number of training sessions per week was in the range of 2–6. The length of intervention duration, in weeks, ranged between six and 104. Five out of 22 studies [44,48,54,58,59] provided dietary treatment as part of the intervention. Figure S2 provides an overview of the risk of bias.

Table 1.
Study characteristics. Values expressed are mean ± standard deviation (SD), unless indicated otherwise.
3.2. Influence of Exercise on Adiponectin and Leptin Levels
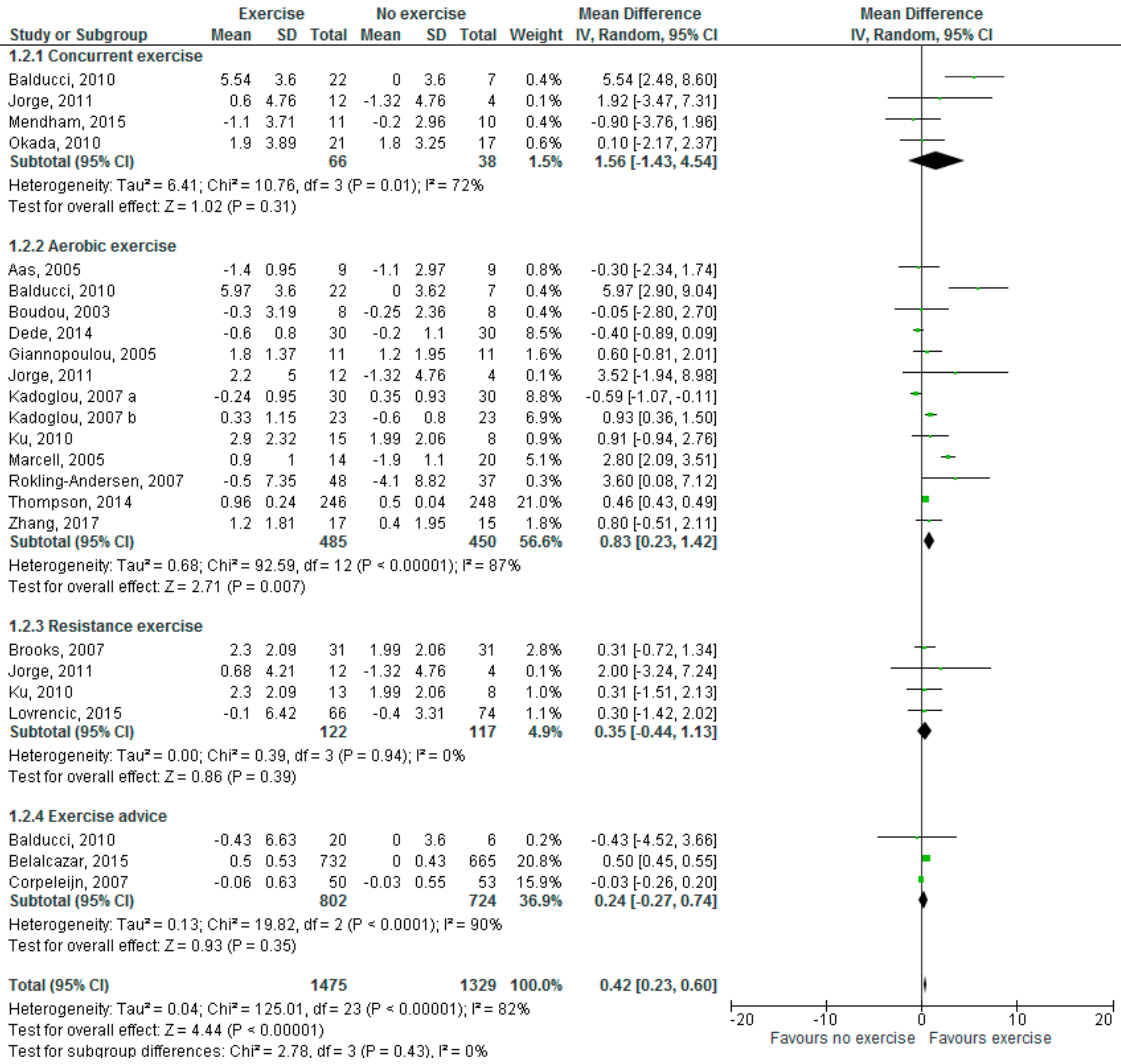
The present meta-analysis shows that physical exercise significantly increases adiponectin levels (Figure 1) in prediabetic and diabetic individuals (mean difference (MD): 0.42 µg/mL; 95% CI 0.23, 0.60, p < 0.00001), but significant study heterogeneity was found (I2 = 82%).
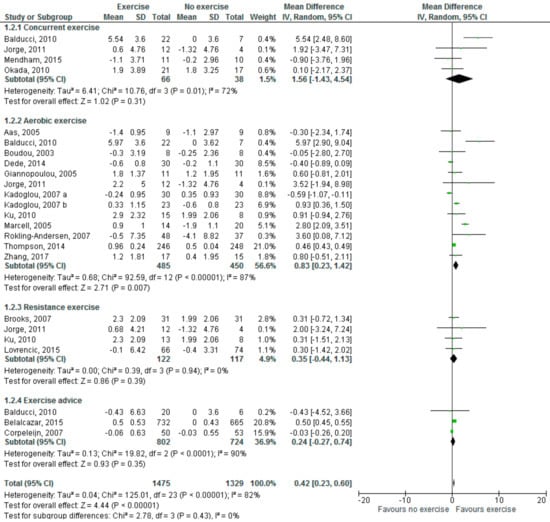
Figure 1.
Effects of physical exercise, including different modalities, on adiponectin levels (µg/mL). Forest plot shows pooled mean differences with 95% confidence intervals (CI) for 24 effect sizes pooled from 19 trials (two separate effect sizes were pooled for different exercise modalities from Jorge [40] and Ku [51], and three from Balducci [39]). The green colored square represents the point estimate of the effect of the intervention for each trial. The horizontal line joins the upper and lower limits of the 95% CI of the effects. The square area represents the relative weight of the trial in the meta-analysis. The black colored diamond at the bottom represents the pooled mean difference with 95% CI for all study groups.
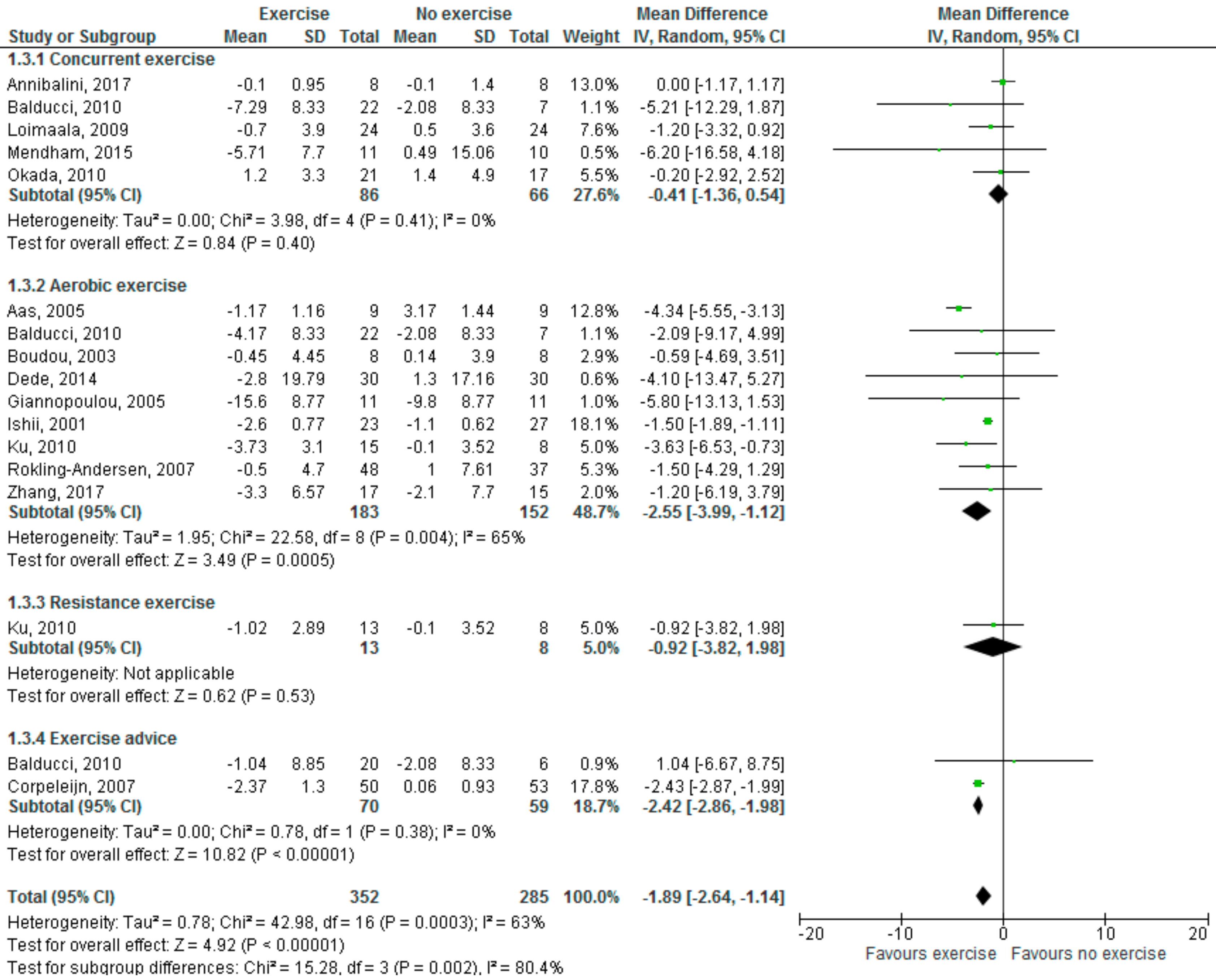
As shown in Figure 2, physical exercise significantly reduced leptin levels (MD: −1.89 ng/mL; 95% CI, −2.64, −1.14, p < 0.00001); here, as well, high heterogeneity was found (I2 = 63%).
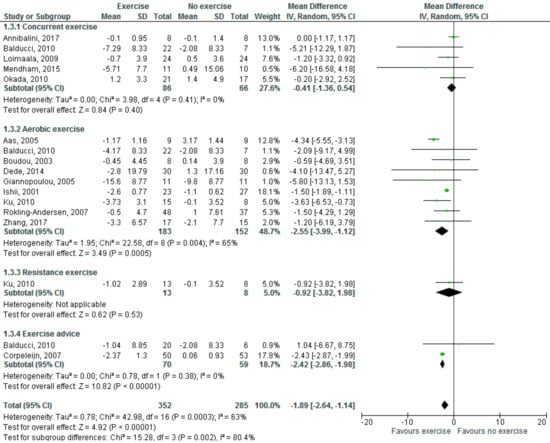
Figure 2.
Effects of physical exercise, including different modalities, on leptin levels (ng/mL). Forest plot shows pooled mean differences with 95% confidence intervals (CI) for 17 pooled effect sizes from 14 trials (two separate effect sizes were pooled for different exercise modalities from Ku [51] and three from Balducci [39]). The green colored square represents the point estimate of the effect of the intervention for each trial. The horizontal line joins the upper and lower limits of the 95% CI of the effects. The square area represents the relative weight of the trial in the meta-analysis. The black colored diamond at the bottom represents the pooled mean difference with 95% CI for all study groups.
With regards to effects of different exercise modalities, aerobic exercise significantly increased adiponectin levels (MD: 0.83 µg/mL; 95% CI, 0.23, 1.42, p = 0.007, I2 = 89%), but neither concurrent/resistance exercise nor exercise advice significantly affected adiponectin levels. With regards to leptin levels, both aerobic exercise (MD: −2.55; 95% CI, −3.99, −1.12, p = 0.0005, I2 = 65%) and exercise advice (MD: −2.42; 95% CI, −2.86, −1.98, p < 0.00001, I2 = 0%) led to a significant reduction in serum levels.
3.3. Sensitivity Analysis
As described above, each study was removed once from the meta-analysis, and the effects recalculated with the remaining studies. No major changes in the effect size were found, suggesting a robustness of data in the primary analysis. For adiponectin, the minimal effect size was found once Marcell [52] was removed from the meta-analysis (MD: 0.30; 95% CI, 0.14, 0.46, p = 0.0003, I2 = 74%), while removing Thompson [54] from the analysis generated the largest effect size (MD: 0.64; 95% CI, 0.24, 1.04, p = 0.002, I2 = 82%).
Once Aas [44] and Kadoglu [50] were removed from the analysis, there was an increase in effect size, but the effects remained statistically significant (MD: 0.65 µg/mL; 95% CI, 0.21, 1.09, p = 0.004, I2 = 84%).
Removing studies which involved prediabetic subjects [52,53,59] from the analysis did not change the overall effect size of physical exercise on adiponectin levels (MD: 0.37 µg/mL; 95% CI, 0.21, 0.53, p < 0.00001, I2 = 68%). However, removing Corpeleijn [59] from the analysis doubled the effect size of exercise advice, reduced study heterogeneity to 0%, and the effect was statistically significant (MD: 0.50 µg/mL; 95% CI, 0.45, 0.55, p < 0.00001, I2 = 0%). For leptin, removing Aas [44] decreased the effect size the most, but also reduced heterogeneity below 50% (MD: −1.55; 95% CI, −2.20, −0.91, p < 0.00001, I2 = 44%). Once Annibalini [38] was left out from the analysis, the largest effect size was seen for leptin (MD: −2.19; 95% CI, −2.92, −1.46, p < 0.00001, I2 = 53%). Removing the two studies with high risk of bias [44,48] from the analysis reduced study heterogeneity both for the overall effect of physical exercise (MD: −1.54; 95% CI, −2.45, −0.63, p = 0.0009, I2 = 38%), and in the aerobic exercise subgroup (MD: −2.28; 95% CI, −3.86, −0.69, p = 0.005, I2 = 0%). Limiting the analysis to type 2 diabetics only did not change the overall effects of physical exercise (MD: −1.81; 95% CI, −2.84, −0.79, p = 0.0005, I2 = 59%), but the results in the exercise advice subgroup became non-significant after removing Corpeleijn [59] (MD: −1.04; 95% CI, −6.67, 8.75, p = 0.79).
3.4. Subgroup Analysis
Subgroup analyses were conducted for intervention duration, dietary co-intervention, and the number of training sessions per week (Table 2). For the number of training sessions per week, Okada [43] and Giannopoulou [47] were excluded from the analysis as they did not specify the exact number of training sessions per week; all exercise advice studies were excluded, as well.

Table 2.
Results of subgroup analysis.
A statistically significant increase in adiponectin levels was found across all subgroups, but study heterogeneity remained high. Interestingly, for intervention duration, studies which lasted ≥12 weeks produced an approximately 5-fold higher increase in adiponectin levels than studies with longer duration (MD: 0.12 vs. 0.49 µg/mL). Interventions that did not include a dietary co-intervention produced a double higher increase in adiponectin levels (MD: 0.99 vs. 0.40 µg/mL). Limiting the number of training sessions to three times per week or less led to approximately 2-fold higher adiponectin levels increase than a higher number of training sessions (MD: 1.70 vs. 0.76). However, statistically significant differences were found only between the subgroups for intervention duration (p = 0.0009).
As for leptin levels, a significant reduction was found across all subgroups as well. Intervention duration >12 weeks led to a higher reduction than shorter duration (MD: −2.69 vs. −1.50 ng/mL). Dietary co-intervention tripled the reduction effect on leptin levels (MD: −2.60 vs. −0.87 ng/mL). Exercising three or less times per week reduced leptin more than a higher frequency (MD: −2.27 vs. −1.72 ng/mL). Interestingly, in subgroups with ≤12 weeks treatment duration, no dietary co-intervention, and >3 training sessions per week, there was very low study heterogeneity. Based on the test for subgroup differences, statistically significant differences were found for the intervention duration and dietary co-intervention subgroup analyses.
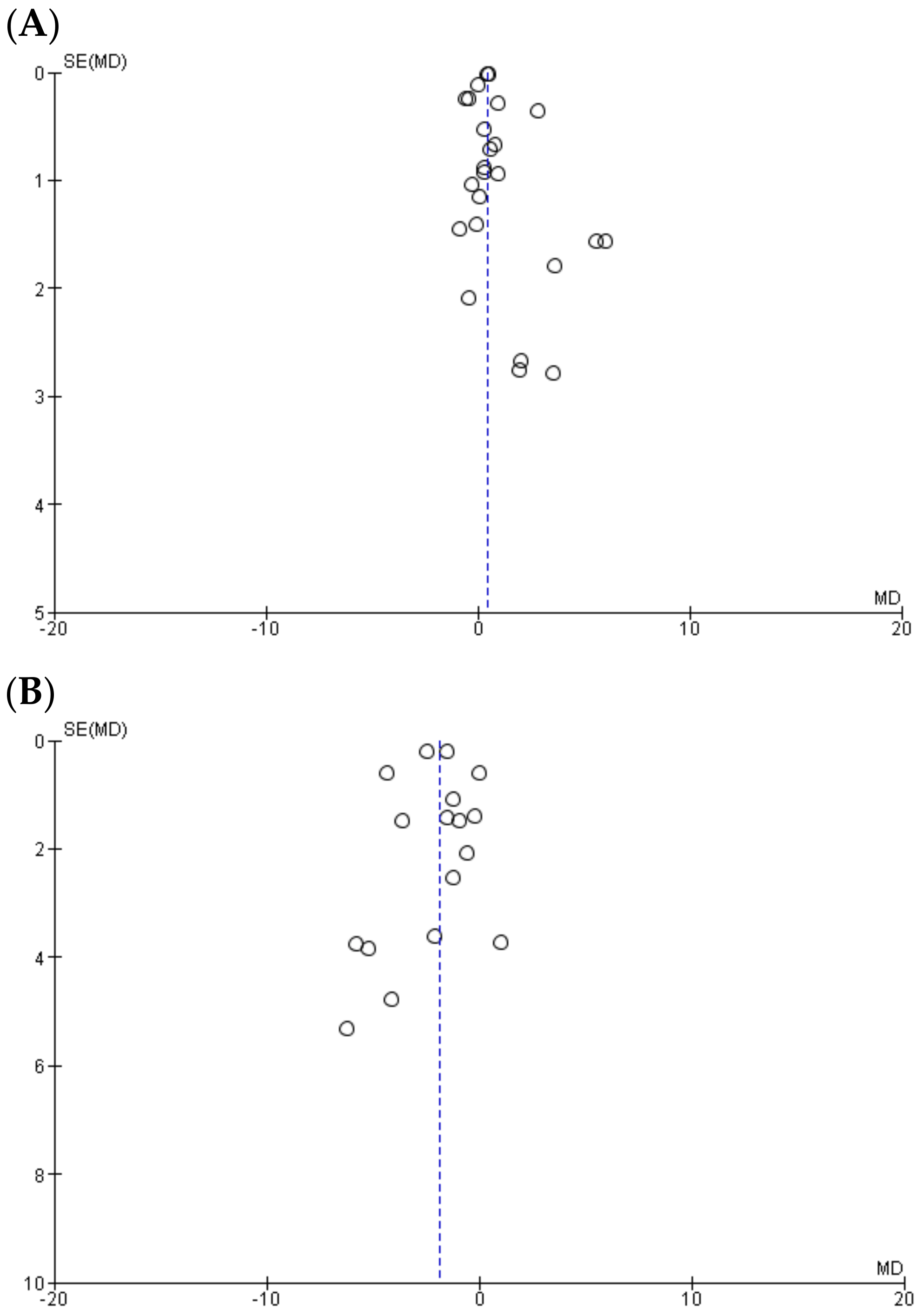
3.5. Publication Bias
Visually inspecting the funnel plots both for adiponectin (Figure 3A) and leptin (Figure 3B) revealed a moderate asymmetry, such that it cannot be excluded that a publication bias, such as not publishing indecisive data, could have affected the results of the present meta-analysis.
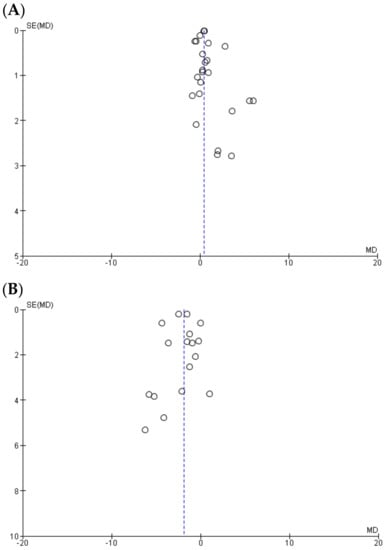
Figure 3.
Funnel plot showing study precision against the mean difference effect estimate with 95% confidence interval for (A) adiponectin and (B) leptin. SE—standard error, MD—mean difference.
4. Discussion
Our meta-analysis shows that physical exercise and, specifically, aerobic exercise, increased adiponectin and reduced leptin levels in prediabetic and diabetic individuals.
As global diabetes rates continue to increase and the underlying conditions, such as obesity and prediabetes, are on the rise, it is of utmost importance to identify strategies for their successful management. Although numerous pharmacotherapy options are available for type 2 diabetes, lifestyle interventions always form an integral part of a diabetes management plan. A preponderance of evidence demonstrates the benefits of physical exercise for a whole set of criteria relevant for prediabetes and diabetes, including better immediate glucose clearance from the blood and long-term improvements of blood sugar and HbA(1c) levels, favorable body composition changes, increased aerobic capacity, better cardiovascular outcomes, and overall reduced morbidity and mortality [1,7,10,11,16].
Adipokines might represent a possible explanation when it comes to the mechanisms mediating the beneficial effects of physical exercise on impaired glucose metabolism.
Hypoadiponectinemia has been associated with impaired glucose regulation, inflammation, obesity, atherosclerosis, and type 2 diabetes [60]. Increasing adiponectin levels has been associated with a lower risk for developing diabetes across populations in a dose–response relationship [61]. In diabetic individuals, enhancing adiponectin levels has emerged as a promising strategy due to its beneficial clinical effects, including anti-inflammatory [62], insulin-mimicking, and insulin-sensitizing [62] properties. Physical exercise exerts increasing effects on adiponectin comparable to the one of some anti-diabetic drugs [63]. Our meta-analysis shows that physical exercise, in general, and aerobic exercise, significantly increase adiponectin levels in prediabetic and diabetic adults. These results are in line with previous meta-analysis done in overweight and obese individuals [64] and, also, with systematic reviews [36]. Another meta-analysis from 2014 [65] did not find significant changes in adiponectin levels in response to physical exercise in diabetic individuals; however, this meta-analysis included much less studies than ours, it did not include prediabetic individuals and, also, considered interventions which included drug co-treatment. The robustness of the data was demonstrated in the sensitivity analysis, where it was demonstrated that the results were not dependent on any single study included. Interestingly, exercise advice also led to a significant increase in adiponectin levels once the analysis was constrained to diabetic individuals only. However, high inter-study heterogeneity was generally found. In the subgroup analysis, intervention duration was the only characteristic with significant differences between the subgroups and might, therefore, explain, in part, the heterogeneity. Notably, high study heterogeneity for adiponectin levels was found in previous meta-analysis as well [65].
Leptin is an “adipostat” regulating body fat mass, whose concentration changes with changing fat stores under physiological conditions, with the ultimate goal of maintaining stable body energy stores [66]. However, in type 2 diabetes, leptin levels are generally higher independently of body fat mass [67]. This hyperleptinemia is regarded as a marker of leptin resistance, a condition where tissues do not respond normally to leptin [68]. Leptin resistance in diabetes further aggravates the disarrangements in glucose metabolism [69] and is a significant factor in the development of diastolic function and heart failure [70]. Reducing leptin levels, inflammation, and oxidative stress, are suggested to improve overall leptin sensitivity [71]. Physical exercise is known to reduce oxidative stress and inflammation [72]. In our meta-analysis, we show that physical exercise, especially aerobic exercise, significantly reduces leptin levels. The data were robust, as no significant changes of effect size were found in the sensitivity analysis. However, after leaving out studies with a high risk of bias, study heterogeneity was reduced to below 50%. Exercise advice also led to a significant reduction in leptin levels, but the effect disappeared once the analysis was constrained to only type 2 diabetic individuals, which might imply that exercise advice is able to reduce leptin levels primarily in prediabetic individuals. In general, our results are in accordance with previous work, which also reported significant leptin reduction following physical exercise interventions [64,65]. The subgroup analysis showed that intervention duration and presence of dietary co-intervention are variables with statistically significant differences between subgroups. Leptin levels are highly sensitive to energy balance, such that negative energy balance through caloric deficit leads to a reduction in circulating leptin [73]. It is, therefore, plausible that the addition of dietary co-intervention potentiates the reducing effects of exercise on leptin through creating a larger negative energy balance, and the effects are greater with the duration of the negative energy state.
Interestingly, the present meta-analysis revealed that aerobic exercise, but not other exercise modalities, lead to significant increase in adiponectin levels and a reduction in leptin levels. This was also found in previous meta-analyses [64,65], and might be explained through greater negative energy balance induced by aerobic exercise as compared to other exercise modalities [74], but also an overall greater effect of aerobic exercise on body weight and fat mass [75].
However, the present study has several limitations. The risk of bias could not be assessed across many of the preset criteria. In addition, high study heterogeneity was found, and could not be fully explained in the subgroup analyses. Furthermore, the population set analyzed was heterogeneous in terms of age distribution, BMI, and clinical condition. Also, the design of physical exercise interventions differed, e.g., in terms of session duration and intensity. For aerobic exercise, we could not make a differentiation between potentially different effects of interval vs. continuous exercise. Some studies also had very small study groups, which tends to produce more extreme effects. Publication bias could also not be excluded.
In conclusion, the present systematic review and meta-analysis shows that exercise represents a viable strategy to increase adiponectin and reduce leptin levels in prediabetic and diabetic individuals. However, a cautious interpretation is warranted.
Supplementary Materials
The following are available online at http://www.mdpi.com/2076-3271/6/4/97/s1, Figure S1: Flow diagram of study selection, Figure S2: Risk of bias assessment. Search strategy for PubMed: (“training” OR “exercise” OR “physical activity”) and (“diabetes” OR “prediabetes” OR “insulin resistance” OR “impaired glucose tolerance” OR “impaired fasting glucose” OR “leptin” OR “adiponectin” OR “adipokines”) and (“randomized controlled trial” OR “randomized” OR “clinical trials as topic” OR “placebo” OR “randomly” OR “trial”) not (“animals” NOT “humans”).
Author Contributions
Systematic literature search, T.B. Data extraction and statistical analysis, T.B. and C.F. Validation, G.F. Original draft preparation, T.B. and C.F. Writing—Review & Editing, G.F. Final draft, T.B.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Global Report on Diabetes. 2016. Available online: http://apps.who.int/iris/bitstream/10665/204871/1/9789241565257_eng.pdf (accessed on 3 April 2018).
- World Health Organization. Diabetes Fact Sheet. Available online: http://www.who.int/mediacentre/factsheets/fs138/en (accessed on 3 April 2018).
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS ONE 2006, 3, e442. [Google Scholar] [CrossRef] [PubMed]
- US National Center for Chronic Disease Prevention and Health Promotion. National Diabetes Statistics Report 2017: Estimates of Diabetes and its Burden in the United States. Available online: http://www.diabetes.org/assets/pdfs/basics/cdc-statistics-report-2017.pdf (accessed on 4 April 2018).
- Tabák, A.G.; Herder, C.; Rathmann, W.; Brunner, E.J.; Kivimäki, M. Prediabetes: A high-risk state for diabetes development. Lancet 2012, 379, 2279–2790. [Google Scholar] [CrossRef]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef] [PubMed]
- UK Academy of Medical Royal Colleges. Exercise—The Miracle Cure. 2015. Available online: http://www.aomrc.org.uk/wp-content/uploads/2016/05/Exercise_the_Miracle_Cure_0215.pdf (accessed on 5 April 2018).
- Jeon, C.Y.; Lokken, R.P.; Hu, F.B.; van Dam, R.M. Physical activity of moderate intensity and risk of type 2 diabetes, a systematic review. Diabetes Care 2007, 30, 744–752. [Google Scholar] [CrossRef] [PubMed]
- Morrato, E.H.; Hill, J.O.; Wyatt, H.R.; Ghushchyan, V.; Sullivan, P.W. Physical activity in U.S. adults with diabetes and at risk for developing diabetes, 2003. Diabetes Care 2007, 30, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Boulé, N.G.; Haddad, E.; Kenny, G.P.; Wells, G.A.; Sigal, R.J. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: A meta-analysis of controlled clinical trials. JAMA 2001, 286, 1218–1227. [Google Scholar] [CrossRef] [PubMed]
- Boulé, N.G.; Kenny, G.P.; Haddad, E.; Wells, G.A.; Sigal, R.J. Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in type 2 diabetes mellitus. Diabetologia 2003, 46, 1071–1081. [Google Scholar] [CrossRef] [PubMed]
- Balducci, S.; Iacobellis, G.; Parisi, L.; Di Biase, N.; Calandriello, E.; Leonetti, F.; Fallucca, F. Exercise training can modify the natural history of diabetic peripheral neuropathy. J. Diabetes Complications 2006, 20, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Pagkalos, M.; Koutlianos, N.; Kouidi, E.; Pagkalos, E.; Mandroukas, K.; Deligiannis, A. Heart rate variability modifications following exercise training in type 2 diabetic patients with definite cardiac autonomic neuropathy. Br. J. Sports Med. 2008, 42, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Eves, N.D.; Plotnikoff, R.C. Resistance training and type 2 diabetes. Considerations for implementation at the population level. Diabetes Care 2006, 29, 1933–1941. [Google Scholar] [CrossRef] [PubMed]
- Church, T.S.; Blair, S.N.; Cocreham, S.; Johannsen, N.; Johnson, W.; Kramer, K.; Mikus, C.R.; Myers, V.; Nauta, M.; Rodarte, R.Q.; et al. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: A randomized controlled trial. JAMA 2010, 304, 2253–2262. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Missbach, B.; Dias, S.; König, J.; Hoffmann, G. Impact of different training modalities on glycaemic control and blood lipids in patients with type 2 diabetes: A systematic review and network meta-analysis. Diabetologia 2014, 57, 1789–1797. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Scott, C.A.; Mao, C.; Tang, J.; Farmer, A.J. Resistance exercise versus aerobic exercise for type 2 diabetes: A systematic review and meta-analysis. Sports Med. 2014, 44, 487–49. [Google Scholar] [CrossRef] [PubMed]
- Paulweber, B.; Valensi, P.; Lindström, J.; Lalic, N.M.; Greaves, C.J.; McKee, M.; Kissimova-Skarbek, K.; Liatis, S.; Cosson, E.; Szendroedi, J.; et al. A European evidence-based guideline for the prevention of type 2 diabetes. Horm. Metab. Res. 2010, 42 (Suppl. 1), S3–S36. [Google Scholar] [CrossRef] [PubMed]
- The American Diabetes Association. Standards of Medical Care in Diabetes—2016. Available online: http://care.diabetesjournals.org/content/suppl/2015/12/21/39.Supplement_1.DC2/2016-Standards-of-Care.pdf (accessed on 18 April 2018).
- Sigal, R.J.; Kenny, G.P.; Wasserman, D.H.; Castaneda-Sceppa, C.; White, R.D. Physical activity/exercise and type 2 diabetes. A consensus statement from the American Diabetes Association. Diabetes Care 2006, 29, 1433–1438. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Proenca, R.; Maffei, M.; Barone, M.; Leopold, L.; Friedman, J.M. Positional cloning of the mouse obese gene and its human homologue. Nature 1994, 372, 425–432. [Google Scholar] [CrossRef] [PubMed]
- McGown, C.; Birerdinc, A.; Younossi, Z.M. Adipose tissue as an endocrine organ. Clin. Liver Dis. 2014, 18, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Verheggen, R.J.; Maessen, M.F.; Green, D.J.; Hermus, A.R.; Hopman, M.T.; Thijssen, D.H. A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: Distinct effects on body weight and visceral adipose tissue. Obes. Rev. 2016, 17, 664–690. [Google Scholar] [CrossRef] [PubMed]
- Kelesidis, T.; Kelesidis, I.; Chou, S.; Mantzoros, C.S. Narrative review: The role of leptin in human physiology: Emerging clinical applications. Ann. Intern. Med 2010, 152, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Matsuzawa, Y. Adiponectin: Identification, physiology and clinical relevance in metabolic and vascular disease. Atheroscler. Suppl. 2005, 6, 7–14. [Google Scholar] [CrossRef] [PubMed]
- López-Jaramillo, P.; Gómez-Arbeláez, D.; López-López, J.; López-López, C.; Martínez-Ortega, J.; Gómez-Rodríguez, A.; Triana-Cubillos, S. The role of leptin/adiponectin ratio in metabolic syndrome and diabetes. Horm. Mol. Biol. Clin. Investig. 2014, 18, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Hu, M.; Yan, Y.; Zhang, H. The effect of exercise on adiponectin and leptin levels in overweight or obese subjects: A meta-analysis of randomized controlled trials. Sport Sci. Health 2017, 13, 303–314. [Google Scholar] [CrossRef]
- Sturgeon, K.; Digiovanni, L.; Good, J.; Salvatore, D.; Fenderson, D.; Domchek, S.; Stopfer, J.; Galantino, M.L.; Bryan, C.; Hwang, W, T.; Schmitz, K. Exercise-induced dose-response alterations in adiponectin and leptin levels are dependent on body fat changes in women at risk for breast cancer. Cancer Epidemiol. Biomarkers Prev. 2016, 25, 1195–1200. [Google Scholar] [CrossRef] [PubMed]
- Abbenhardt, C.; McTiernan, A.; Alfano, C.M.; Wener, M.H.; Campbell, K.L.; Duggan, C.; Foster-Schubert, K.E.; Kong, A.; Toriola, A.T.; Potter, J.D.; et al. Effects of individual and combined dietary weight loss and exercise interventions in postmenopausal women on adiponectin and leptin levels. J. Intern. Med. 2013, 274, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Greean, S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1. Available online: http://handbook.cochrane.org (accessed on 19 April 2018).
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Cochrane Community: Review Manager 5.3. Available online: http://tech.cochrane.org/revman/download (accessed on 18 April 2018).
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Bouassida, A.; Chamari, K.; Zaouali, M.; Feki, Y.; Zbidi, A.; Tabka, Z. Review on leptin and adiponectin responses and adaptations to acute and chronic exercise. Br. J. Sports Med. 2010, 44, 620–630. [Google Scholar] [CrossRef] [PubMed]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical activity/exercise and diabetes: A position statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef] [PubMed]
- Annibalini, G.; Lucertini, F.; Agostini, D.; Vallorani, L.; Gioacchini, A.; Barbieri, E.; Guescini, M.; Casadei, L.; Passalia, A.; Del Sal, M.; et al. Concurrent aerobic and resistance training has anti-inflammatory effects and increases both plasma and leukocyte levels of IGF-1 in late middle aged type 2 diabetic. Oxid. Med. Cell. Longev. 2017, 2017, 3937842. [Google Scholar] [CrossRef] [PubMed]
- Balducci, S.; Zanuso, S.; Nicolucci, A.; Fernando, F.; Cavallo, S.; Cardelli, P.; Fallucca, S.; Alessi, E.; Letizia, C.; Jimenez, A.; et al. Anti-inflammatory effect of exercise training in subjects with type 2 diabetes and the metabolic syndrome is dependent on exercise modalities and independent of weight loss. Nutr. Metab. Cardiovasc. Dis. 2010, 20, 608–617. [Google Scholar] [CrossRef] [PubMed]
- Jorge, M.L.; de Oliveira, V.N.; Resende, N.M.; Paraiso, L.F.; Calixto, A.; Debs Diniz, A.L.; Resende, E.S.; Ropelle, E.R.; Carvalheira, J.B.; Espindola, F.S.; et al. The effects of aerobic, resistance, and combined exercise on metabolic control, inflammatory markers, adipocytokines, and muscle insulin signaling in patients with type 2 diabetes mellitus. Metabolism 2011, 60, 1244–1252. [Google Scholar] [CrossRef] [PubMed]
- Loimaala, A.; Groundstroem, K.; Rinne, M.; Nennonen, A.; Huhtala, H.; Parkkari, J.; Vuori, I. Effect of long-term endurance and strength training on metabolic control and arterial elasticity in patients with type 2 diabetes mellitus. Am. J. Cardiol. 2009, 103, 972–977. [Google Scholar] [CrossRef] [PubMed]
- Mendham, A.E.; Duffield, R.; Marino, F.; Coutts, A.J. A 12-week sports-based exercise programme for inactive Indigenous Australian men improved clinical risk factors associated with type 2 diabetes mellitus. J. Sci. Med. Sport 2015, 18, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Okada, S.; Hiuge, A.; Makino, H.; Nagumo, A.; Takaki, H.; Konishi, H.; Goto, Y.; Yoshimasa, Y.; Miyamoto, Y. Effect of exercise intervention on endothelial function and incidence of cardiovascular disease in patients with type 2 diabetes. J. Atheroscler. Thromb. 2010, 17, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Aas, A.M.; Seljeflot, I.; Torjesen, P.A.; Diep, L.M.; Thorsby, P.M.; Birkeland, K.I. Blood glucose lowering by means of lifestyle intervention has different effects on adipokines as compared with insulin treatment in subjects with type 2 diabetes. Diabetologia 2006, 49, 872–880. [Google Scholar] [CrossRef] [PubMed]
- Boudou, P.; Sobngwi, E.; Mauvais-Jarvis, F.; Vexiau, P.; Gautier, J.F. Absence of exercise-induced variations in adiponectin levels despite decreased abdominal adiposity and improved insulin sensitivity in type 2 diabetic men. Eur. J. Endocrinol. 2003, 149, 421–444. [Google Scholar] [CrossRef] [PubMed]
- Dede, N.D.; Ipekci, S.H.; Kebapcilar, L.; Arslan, M.; Kurban, S.; Yildiz, M.; Gönen, M.S. Influence of exercise on leptin, adiponectin and quality of life in type 2 diabetics. Turkish J. Endocrin. Metable. 2015, 19, 7–13. [Google Scholar] [CrossRef]
- Giannopoulou, I.; Fernhall, B.; Carhart, R.; Weinstock, R.S.; Baynard, T.; Figueroa, A.; Kanaley, J.A. Effects of diet and/or exercise on the adipocytokine and inflammatory cytokine levels of postmenopausal women with type 2 diabetes. Metabolism 2005, 54, 866–875. [Google Scholar] [CrossRef] [PubMed]
- Ishii, T.; Yamakita, T.; Yamagami, K.; Yamamoto, T.; Miyamoto, M.; Kawasaki, K.; Hosoi, M.; Yoshioka, K.; Sato, T.; Tanaka, S.; et al. Effect of exercise training on serum leptin levels in type 2 diabetic patients. Metabolism 2001, 50, 1136–1140. [Google Scholar] [CrossRef] [PubMed]
- Kadoglou, N.P.; Iliadis, F.; Angelopoulou, N.; Perrea, D.; Ampatzidis, G.; Liapis, C.D.; Alevizos, M. The anti-inflammatory effects of exercise training in patients with type 2 diabetes mellitus. Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Kadoglou, N.P.; Iliadis, F.; Liapis, C.D.; Perrea, D.; Angelopoulou, N.; Alevizos, M. Beneficial effects of combined treatment with rosiglitazone and exercise on cardiovascular risk factors in patients with type 2 diabetes. Diabetes Care 2007, 30, 2242–2244. [Google Scholar] [CrossRef] [PubMed]
- Ku, Y.H.; Han, K.A.; Ahn, H.; Kwon, H.; Koo, B.K.; Kim, H.C.; Min, K.W. Resistance exercise did not alter intramuscular adipose tissue but reduced retinol-binding protein-4 concentration in individuals with type 2 diabetes mellitus. J. Int. Med. Res. 2010, 38, 782–791. [Google Scholar] [CrossRef] [PubMed]
- Marcell, T.J.; McAuley, K.A.; Traustadóttir, T.; Reaven, P.D. Exercise training is not associated with improved levels of C-reactive protein or adiponectin. Metabolism 2005, 54, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Rokling-Andersen, M.H.; Reseland, J.E.; Veierød, M.B.; Anderssen, S.A.; Jacobs, D.R.; Urdal, P.; Jansson, J.O.; Drevon, C.A. Effects of long-term exercise and diet intervention on plasma adipokine concentrations. Am. J. Clin. Nutr. 2007, 86, 1293–1301. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.; Walhin, J.P.; Batterham, A.M.; Stokes, K.; Cooper, A.R.; Andrews, R.C. Effect of diet or diet plus physical activity versus usual care on inflammatory markers in patients with newly diagnosed type 2 diabetes: The Early ACTivity In Diabetes (ACTID) randomized, controlled trial. J. Am. Heart Assoc. 2014, 3, e000828. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.Y.; Liu, T.; Teng, Y.Q.; Yao, X.Y.; Zhao, T.T.; Lin, L.Y.; Jin, Q.S.; Jin, Y.J. Effect of a 12-week aerobic exercise training on serum fetuin-A and adipocytokine levels in type 2 diabetes. Exp. Clin. Endocrinol. Diabetes 2017. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Brook, N.; Layne, J.E.; Gordon, P.L.; Roubenoff, R.; Nelson, M.E.; Castaneda-Sceppa, C. Strength training improves muscle quality and insulin sensitivity in Hispanic older adults with type 2 diabetes. Int. J. Med. Sci. 2006, 4, 19–27. [Google Scholar] [CrossRef]
- Vučić Lovrenčić, M.; Pibernik-Okanović, M.; Šekerija, M.; Prašek, M.; Ajduković, D.; Kos, J.; Hermanns, N. Improvement in depressive symptoms is associated with reduced oxidative damage and inflammatory response in type 2 diabetic patients with subsyndromal depression: The results of a randomized controlled trial comparing psychoeducation, physical exercise, and enhanced treatment as usual. Int. J. Endocrin. 2015, 2015, 210406. [Google Scholar] [CrossRef]
- Belalcazar, L.M.; Lang, W.; Haffner, S.M.; Schwenke, D.C.; Kriska, A.; Balasubramanyam, A.; Hoogeveen, R.C.; Pi-Sunyer, F.X.; Tracy, R.P.; Ballantyne, C.M. Improving adiponectin levels in individuals with diabetes and obesity: Insights from look AHEAD. Diabetes Care 2015, 38, 1544–1560. [Google Scholar] [CrossRef] [PubMed]
- Corpeleijn, C.; Feskens, E.J.M.; Jansen, E.; Mensink, M.; Saris, W.; Blaak, E.E. Lifestyle intervention and adipokine levels in subjects at high Risk for type 2 diabetes. The study on lifestyle intervention and impaired glucose tolerance Maastricht (SLIM). Diabetes Care 2007, 30, 3125–3127. [Google Scholar] [CrossRef] [PubMed]
- Kishida, K.; Funahashi, T.; Shimomura, I. Molecular mechanisms of diabetes and atherosclerosis: Role of adiponectin. Endocr. Metab. Immune Disord. Drug Targets 2012, 12, 118–131. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Shin, H.J.; Ding, E.L.; van Dam, R.M. Adiponectin levels and risk of type 2 diabetes: A systematic review and meta-analysis. JAMA 2009, 302, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Sweeney, G. Mechanisms regulating energy metabolism by adiponectin in obesity and diabetes. Biochem. Soc. Trans. 2006, 34, 798–801. [Google Scholar] [CrossRef] [PubMed]
- Achari, A.E.; Jain, S.K. Adiponectin, a therapeutic target for obesity, diabetes, and endothelial dysfunction. Int. J. Mol. Sci. 2017, 18, 1321. [Google Scholar] [CrossRef] [PubMed]
- Yu, N.; Ruan, Y.; Gao, X.; Sun, J. Systematic review and meta-analysis of randomized, controlled trials on the effect of exercise on serum leptin and adiponectin in overweight and obese individuals. Horm. Metab. Res. 2017, 49, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Hayashino, Y.; Jackson, J.L.; Hirata, T.; Fukumori, N.; Nakamura, F.; Fukuhara, S.; Tsujii, S.; Ishii, H. Effects of exercise on C-reactive protein, inflammatory cytokine and adipokine in patients with type 2 diabetes: A meta-analysis of randomized controlled trials. Metabolism 2014, 63, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Baile, C.A.; Della-Fera, M.A.; Martin, R.J. Regulation of metabolism and body fat mass by leptin. Ann. Rev. Nutr. 2000, 20, 105–127. [Google Scholar] [CrossRef] [PubMed]
- Fischer, S.; Hanefeld, M.; Haffner, S.M.; Fusch, C.; Schwanebeck, U.; Kohler, C.; Fucker, K.; Julius, U. Insulin-resistant patients with type 2 diabetes mellitus have higher serum leptin levels independently of body fat mass. Acta Diabetol. 2002, 39, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.S.; Qasim, A.; Reilly, M.P. Leptin resistance: A possible interface of inflammation and metabolism in obesity-related cardiovascular disease. J. Am. Coll. Cardiol. 2008, 52, 1201–1110. [Google Scholar] [CrossRef] [PubMed]
- Meek, T.H.; Morton, G.J. Leptin, diabetes, and the brain. Indian J. Endocrinol. Metab. 2012, 16, 534–542. [Google Scholar] [CrossRef]
- Zhuravlyova, L.; Sokolnikova, N. The relationship between hyperleptinemia and diastolic dysfunction in patients with diabetes mellitus type 2. Arch. Cardiovasc. Dis. Suppl. 2016, 8, 23–40. [Google Scholar] [CrossRef]
- Zhou, Y.; Rui, L. Leptin signaling and leptin resistance. Front. Med. 2013, 7, 207–222. [Google Scholar] [CrossRef] [PubMed]
- Sallam, N.; Laher, I. Exercise modulates oxidative stress and inflammation in aging and cardiovascular diseases. Oxid. Med. Cell. Longev. 2016, 2016, 7239639. [Google Scholar] [CrossRef] [PubMed]
- Steinera, A.A.; Romanovsky, A.A. Leptin: At the crossroads of energy balance and systemic inflammation. Prog. Lipid. Res. 2007, 46, 89–107. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.A.; Dolmage, T.E.; Robles, P.G.; Brooks, D.; Goldberg, R.S. The effects of exercise modality and intensity on energy expenditure and cardiorespiratory response in adults with obesity and treated obstructive sleep apnoea. Chron. Respir. Dis. 2017, 14, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Willis, L.H.; Slentz, C.A.; Bateman, L.A.; Shields, T.; Piner, L.W.; Bales, C.W.; Houmard, J.A.; Kraus, W. Effects of aerobic and/or resistance training on body mass and fat mass in overweight or obese adults. J. Appl. Physiol. 2012, 113, 1831–1837. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).