Abstract
Background: Sepsis diagnosis can be incorrectly associated with the presence of hypotension during an infection, so the detection and management of non-hypotensive sepsis can be delayed. We aimed to evaluate how the presence or absence of hypotension, on admission at the emergency department, affects the initial management and outcomes of patients with community-onset severe sepsis. Methods: Demographic, clinical, laboratory, process of care, and outcome variables were recorded for all patients, at the emergency department of our university hospital, who presented with community-onset severe sepsis, between 1 March and 31 August in three consecutive years. Patient management consisted of standardized bundled care with five measures: Detection, blood cultures and empirical antibiotics, oxygen supplementation and fluid resuscitation (if needed), clinical monitoring, and noradrenalin administration (if needed). We compared all variables between patients who had hypotension (mean arterial pressure <65 mmHg), on admission to the emergency department, and those who did not. Results: We identified 153 episodes (84 (54.5%) men; mean age 73.6 ± 1.2; mean Sequential Organ Failure Assessment (SOFA) score 4.9 ± 2.7, and 41.2% hospital mortality). Hypotension was present on admission to the emergency department in 57 patients (37.2%). Hemodynamic treatment was applied earlier in patients who presented hypotension initially. Antibiotics were administered 48 min later in non-hypotensive sepsis (p = 0.08). A higher proportion of patients without initial hypotension required admission to the intensive care unit (ICU) (43.1% for patients initially hypotensive vs. 56.9% in those initially non-hypotensive, p < 0.05). Initial hypotension was not associated with mortality. A delay in door-to-antibiotic administration time was associated with mortality [OR 1.150, 95%CI: 1.043–1.268). Conclusions: Initial management of patients with community-onset severe sepsis differed according to their clinical presentation. Initial hypotension was associated with early hemodynamic management and less ICU requirement. A non-significant delay was observed in the administration of antibiotics to initially non-hypotensive patients. The time of door-to-antibiotic administration was related to mortality.
1. Introduction
The incidence of sepsis [1] in developed countries is over 200 cases/100,000 inhabitants per year [2,3,4], and about 50 cases of community-onset sepsis/100,000 inhabitants/year require admission to intensive care units (ICU) [5]. The outcomes and the use of healthcare resources for community-onset sepsis are influenced both by factors that cannot be modified (e.g., infection site, causal microorganism, and patient characteristics) and by other, time-dependent, factors that can be modified, mainly early appropriate infection control and hemodynamic resuscitation [6]. Delayed or inappropriate resuscitation or infection-control measures are strongly associated with increased morbidity and mortality [7,8]. The heterogeneous clinical presentation of community-onset sepsis can make it difficult to detect, thus delaying the application of therapeutic measures and increasing mortality. We analyzed how the clinical presentation affects the management of patients with community-onset sepsis in our emergency department. Our main objective was to determine the effect of the absence of initial hypotension on emergency department management, and accordingly the impact on clinical evolution.
2. Materials and Methods
This observational study collected data from all patients, at the emergency department of our university hospital, that fulfilled the sepsis-II criteria for severe sepsis [1], between 1 March and 31 August in three consecutive years (2008, 2009, and 2010). The study took place in a university hospital, with 320 acute beds and 14 ICU beds, that provides care for a population of 250,000 inhabitants. The management of patients was according to Surviving Sepsis Campaign recommendations [9]. A resuscitation chain for sepsis was developed by investigators [10] and was used to spread general recommendations for sepsis management (Figure 1).
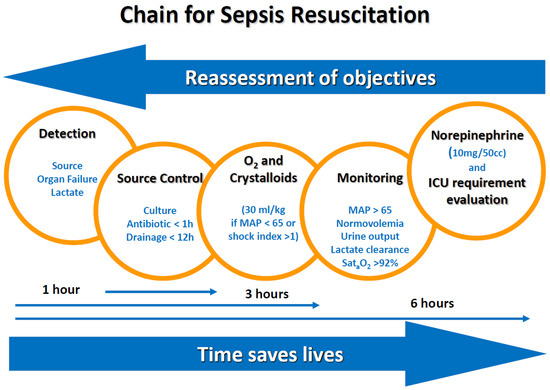
Figure 1.
Chain for sepsis resuscitation that resumes the clinical algorithm for initial management of septic patients. ICU—intensive care unit; MAP—Mean Arterial Pressure.
The hospital’s clinical research ethics committee approved the study (serial number: 48/17) and waived the requirement for informed consent due to its observational nature. Patient information was appropriately encrypted before inclusion in the study database.
2.1. Patient Selection
We included all patients aged >18 years who presented, at the emergency department of our university hospital, with an acute community-onset infection, and who developed acute organ dysfunction or lactate concentrations above 2 mmol/L. We excluded patients undergoing palliative care, those with orders to withhold the life-support measures that were included in the initial resuscitation process (noradrenaline or mechanical ventilation), those who were diagnosed with severe sepsis and/or started resuscitation in another center, and those diagnosed with severe sepsis after transfer to hospital wards.
We defined infection as a clinical process characterized by an inflammatory response to the presence of microorganisms; or the invasion of normally sterile host tissue by microorganisms in the absence of other causes for an inflammatory response. Systemic inflammatory response syndrome (SIRS) was defined if two or more of the following conditions were present: Temperature >38 °C, heart rate >90 beats per minute; respiratory rate >20 breaths per minute, and/or white blood cell count >12,000 or <4000. Sepsis was defined as an infection with the presence of two or more criteria of SIRS. Severe sepsis was defined as sepsis associated with organ dysfunction. Sepsis-induced hypotension was defined as mean arterial blood pressure <65mmHg, whereas septic shock was defined as maintained sepsis-induced hypotension despite adequate fluid resuscitation, which needs inotropic or vasopressor agents to restore perfusion abnormalities. To define organ failure, we used SOFA score criteria, requiring a score of ≥2 for at least one organ’s failure evaluation, being: Cardiovascular, respiratory, central nervous system, coagulation, liver or renal failure [11].
2.2. Data Collection
For patients presenting with severe sepsis in the emergency department, we recorded their demographics (age, sex, and comorbidity assessed with an age-adjusted Charlson Index) [12], clinical variables related to the presentation of sepsis (heart rate, blood pressure, respiratory rate, arterial oxygen saturation, and mental status), laboratory test results, focus of infection, and SOFA score [13]. We recorded the following process of care variables: Time from administrative admission to the obtainment of blood samples for cultures (door-to-culture time), to the administration of empirical antibiotics (door-to-antibiotic time), to the administration of 2 L of crystalloids (door-to-fluid resuscitation time), and to the administration of noradrenalin (door-to-noradrenalin time). We recorded the following outcome variables: Lactate levels 6 h after admission, the need for ICU admission, and hospital mortality. We compared variables between patients initially presenting with hypotension (mean arterial pressure (MAP) <65 mmHg) and those initially presenting without hypotension. Initial clinical variables were recorded during the first hour after administrative admission. The SOFA score was evaluated after 6h of admission. The time-to-procedure measurements were determined from the time of administrative admission to the time of the procedure.
2.3. Statistical Analysis
We used Student’s t-tests to compare continuous variables with normal distribution, Mann–Whitney U tests to compare continuous variables without normal distribution, and chi-square tests to compare categorical variables. We used simple logistic regression to calculate odds ratios and 95% confidence intervals. Statistical significance was set at p < 0.05. We used the forward stepwise method for the multivariate analysis.
3. Results
During the 18 months comprising the study period, a total of 3856 patients were admitted to the hospital after presenting, at the emergency department, with acute community-onset infections; 321 (8.3% of the total) had acute organ dysfunction and/or elevated lactate concentrations, and 153 (4.0% of the total) of these were eligible for all resuscitation measures (Figure 2).
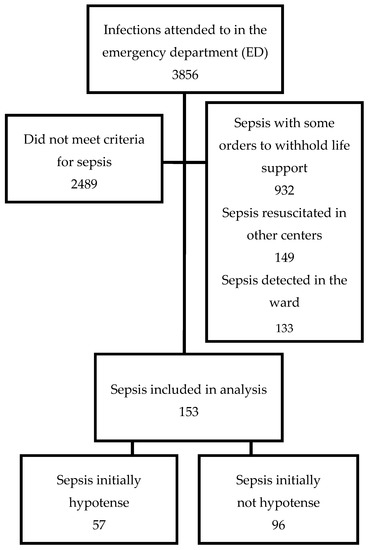
Figure 2.
Enrollment flow chart.
Of the 153 patients included in the study, 84 (54.5%) were men, the mean age was 73.6 ± 1.2 years, and the mean age-adjusted Charlson score was 6.2 ± 2.9. The most common focus of infection was urinary (29.9%), followed by pulmonary (26%), abdominal (24%), and then unknown (13.6%). The mean SOFA score in the first six hours was 4.9 ± 2.7. Blood pressure, heart rate, and temperature were assessed in 100%, saturated O2 in 97.4%, and respiratory rate in 93%of patients. Mental status was considered normal if agitation, confusion, and coma were not reported (32%). Initial lactate concentrations were measured in 55 patients; the mean concentration was 5.2 ± 3.2 mmol/L. Hospital mortality was 41.2% (Table 1).

Table 1.
Comparison, between the survivors and non-survivors, among patients who presented with severe community-acquired sepsis at the emergency department.
On arrival at the emergency department, 57 (37.2%) patients presented with initial hypotension. Hypotensive patients had higher initial lactate concentrations. Patients were managed differently according to whether they initially presented with hypotension or not (Table 2). Hypotensive patients received intervention measures earlier than those who were non-hypotensive; door-to-culture time, door-to-antibiotic time, door-to-fluid resuscitation time, and door-to-noradrenalin time were shorter in hypotensive patients.

Table 2.
Main epidemiological and clinical variables depending on the presence or absence of hypotension. Differences in response time (in hours), from the time of admission to the emergency department, for patients with initial hypotension versus those without.
Although the group of patients who were hypotensive at admission had higher initial lactate concentrations, lactate concentrations measured six hours after admission did not differ between the two groups. Fewer patients in the group with initial hypotension, compared to the group without initial hypotension, required admission to the ICU (43% vs. 56.9%, respectively, p < 0.01). No significant differences in hospital mortality were observed between the two groups (35.7% in the group with initial hypotension vs. 44.3% in the group without initial hypotension, p = 0.297) (Figure 3).
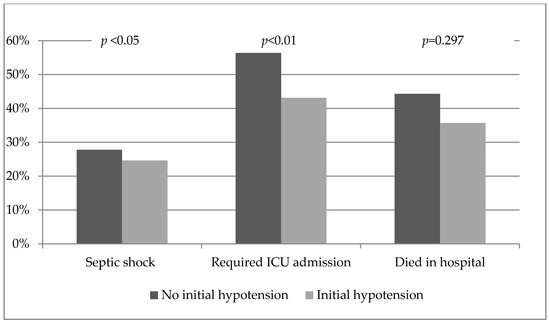
Figure 3.
Differences in clinical evolution and outcomes between patients, with community-onset severe sepsis, that initially presented with hypotension and those that initially presented without hypotension.
In the bivariate analysis, the initial presence of hypotension was not associated with mortality or the need for ICU admission. Initial symptoms associated with mortality were tachypnea, greater hypoxia, greater acidosis, higher lactate concentrations, and higher baseline blood glucose. Table 1 reports the differences between patients who survived the hospital stay and those who died in the hospital.
The management of a patient during their stay in the emergency department had an effect on whether they required admission to the ICU and whether they survived the hospital stay, which correlated significantly with delayed administration of therapeutic measures. Patients who survived had shorter door-to-culture time, door-to-antibiotic time, door-to-fluid resuscitation time, and door-to-noradrenalin time than those who died in the hospital (Table 2).
The multivariate analysis found that among the variables recorded in the emergency department, only age (OR 1.049; 95% CI: 1.020–1.079) and door-to-antibiotic time (OR 1.150; 95% CI: 1.043–1.268) were significantly associated with mortality. Retrospectively, a power analysis was performed. Accepting an alpha risk of 0.05 in a two-sided test, with 97 subjects in the no hypotension group and 57 in the hypotension group, the statistical power was 18% to recognize as statistically significant the observed differences in the mortality rates between groups.
4. Discussion
We found that the time from admission to the administration of empirical antibiotics was delayed in patients with community-onset severe sepsis who were not hypotensive at the time of admission to the emergency department. In the multivariate analysis, time-to-antibiotic administration was the only modifiable factor associated with mortality.
The main measures to prevent death in patients with severe community-acquired sepsis are controlling the focus of infection and restoring tissue perfusion. However, these apparently simple measures are difficult to implement. Only 19% of septic patients, from a worldwide multicenter study, received the complete management bundle within three hours of triage, which correlated with a lower hospital mortality rate when compared with septic patients that did not receive complete management within three hours of triage, (19.7% vs. 30.5%, respectively; p < 0.0001) [14]. These results show the need for strategies to improve the management of patients with sepsis [15,16,17].
Door-to-antibiotic time is considered one of the key elements in the management of community-onset severe sepsis [6,18,19,20,21,22,23]. Although it seems reasonable that patients who are hemodynamically unstable would undergo fluid resuscitation earlier than those who are not, it was surprising that the application of the infection-control measures in our study was also affected by patients’ hemodynamic presentation. The door-to-antibiotic time was shorter in patients with hypotension than in those without (3.6 ± 3.9 h vs.4.4 ± 4.2 h, respectively, p < 0.05), and this factor was independently associated with mortality. Other authors have documented how delays in identifying patients with severe sepsis are associated with delays in the administration of empirical antibiotics. In patients that presented, at the emergency department, with severe community-acquired pneumonia delays in pulseoximetry monitoring were associated with delays in door-to-antibiotic times, and consequently with worse survival rates [23].
In our study series, 37% of the patients with community-onset severe sepsis were hypotensive at triage, but only 25% required noradrenalin in the first six hours. Among our patients, initial presentation of hypotension was not a good indicator of mortality, probably because it was associated with earlier application of therapeutic measures. Thus, six hours after admission, lactate concentrations were similar among patients who initially presented hypotension and those who did not. The prognostic value of lactate concentrations measured six hours after admission in patients with severe sepsis, regardless of their blood pressure, has been widely reported [24].
Recently hypotension has been proposed as a major and easy clinical criterion to identify septic patients. Some authors are concerned about the possibility that it may delay the identification of septic patients in the early phase that could be called “pre-sepsis”. Moreover, several authors have found no differences in mortality between patients with hypotensive shock and those with cryptic shock (lactate >4mmol/L and tachycardia without hypotension) [25,26]. Thus, as our results suggest, it is important to detect sepsis or shock, regardless of the presence of hypotension [27,28,29,30]. In septic patients without comorbidities, tachycardia can raise blood pressure to normal levels through increased cardiac output, especially in children and younger adults in whom hypotension is a terminal phenomenon. To help in the detection of cryptic shock, the shock index can be useful, which is defined as the heart rate divided by the systolic blood pressure [31,32,33], or cutaneous refilling. Another useful measure is the use of sensors to detect somatic hypoxia-hypoperfusion (e.g., near-infrared spectrometry) in patients with normal blood pressure [34,35].
In our bivariate analyses, initial hypotension was not associated with mortality, but other factors were, for example, mortality was higher in patients who initially had hypoxia, tachypnea, or metabolic abnormalities (high lactate, hyperglycemia, and metabolic acidosis). These findings support the new definition of septic shock [36], which emphasizes the metabolic nature of shock beyond the purely macrohemodynamic characterization in earlier definitions. Systematic assessment of organ systems (respiratory system, circulatory system, central nervous system, etc.) has proven useful in detecting patients with life-threatening conditions. The qSOFA score has been proposed as an instrument to screen patients for sepsis [37]. Ot her, nonspecific mortality risk assessment scales include hypotension among other easily obtainable variables such as heart rate, respiratory rate, and oxygen saturation, and these can be easily applied in the emergency department. The modified early warning scale (MEWS) has been proven to be the most effective at identifying patients whose condition is likely to deteriorate [38], also specifically in septic patients [39].
The number of septic patients that were attended to at the emergency department, 1367 cases in 18 months, suggested an incidence of 365 cases/100,000 inhabitants; however, most of them had significant comorbidities and were finally excluded from the process of care analysis. The incidence of sepsis in this study was slightly higher than suggested by epidemiological local studies, based on ICD-9 or ICD-10 diagnosis codification system at hospital discharge [40]. Studies based on administrative codification can be useful to monitor trends of incidence or mortality, but they seem to underestimate real incidence, and therefore should be used with caution to provide an absolute value of incidence [41]. Although our study was not designed to analyze the incidence of sepsis, our results support this controversial topic.
The major limitations of our study were that it was carried out in a single center and included few patients, so caution is warranted when extrapolating our results. We observed a slight difference in antibiotic administration between both groups; however, it was not statistically significant because our study is clearly underpowered. A multicentric study, based on the monitoring of key process indicators has been presented to the Catalan Society of Intensive Care Medicine in order to be developed in the future. By not including patients whose resuscitation measures had started at other centers and patients with limits on life support (i.e., vasoactive drugs and/or mechanical ventilation), the size of our sample was restricted. Furthermore, because our aim was to analyze the effect of the presentation of vital signs at the emergency department on the outcomes in patients with community-onset severe sepsis, we calculated times to the application of therapeutic measures from nursing triage, rather than from the detection of sepsis (as specified in quality indicators).This therefore, made it difficult to compare our results with those of other studies.
5. Conclusions
In conclusion, time from administrative admission to antibiotic administration was related to mortality in our study, so it could be used as a key process indicator of sepsis management in the emergency department. The presentation of hypotension on admission indicated more severe sepsis in patients, but as these patients were; accordingly, treated earlier than patients that did not initially present with hypotension, they consequently had fewer admissions to ICU. Our results underline the controversy about hypotension and sepsis detection. Relying excessively on the presentation of hypotension can lead to delays in hemodynamic management and the administration of antibiotics in septic patients with normal blood pressure, and thus affect prognosis. New studies are needed to confirm this hypothesis.
Author Contributions
Conceptualization, J.C.Y. and L.B.; Methodology, J.C.Y., J.A.C., and L.B.; Formal Analysis, E.P.; Investigation, L.B., M.S., R.M., and G.M.; Writing—Original Draft Preparation, J.C.Y., L.B., J.A.C., and A.R.; Writing—Review & Editing, all authors; Supervision, J.C.Y.
Funding
A grant from the www.sepsischallenge.cat cycle race (a non-profit organization that organize sporting events to support sepsis research) supported this work.
Conflicts of Interest
Authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; and in the decision to publish the results.
References
- Levy, M.M.; Fink, M.P.; Marshall, J.C.; Abraham, E.; Angus, D.; Cook, D.; Cohen, J.; Opal, S.M.; Vincent, J.L.; Ramsay, G.; et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit. Care Med. 2003, 31, 1250–1256. [Google Scholar] [CrossRef] [PubMed]
- Yébenes, J.C.; Ruiz-Rodriguez, J.C.; Ferrer, R.; Clèries, M.; Bosch, A.; Lorencio, C.; Rodriguez, A.; Nuvials, X.; Martin-Loeches, I.; Artigas, A.; et al. Epidemiology of sepsis in Catalonia: Analysis of incidence and outcomes in a European setting. Ann. Intensive Care 2017, 7, 19. [Google Scholar] [CrossRef] [PubMed]
- Rubens, M.; Saxena, A.; Ramamoorthy, V.; Das, S.; Khera, R.; Hong, J.; Armaignac, D.; Veledar, E.; Nasir, K.; Gidel, L. Increasing Sepsis Rates in the United States: Results From National Inpatient Sample, 2005 to 2014. J. Intensive Care Med. 2018, 2, 885066618794136. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, D.P.; Laursen, C.B.; Jensen, T.G.; Hallas, J.; Pedersen, C.; Lassen, A.T. Incidence rate of community-acquired sepsis among hospitalized acute medical patients-a population-based survey. Crit. Care Med. 2015, 43, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Almirall, J.; Güell, E.; Capdevila, J.A.; Campins, L.; Palomera, E.; Martinez, R.; Miró, G.; de la Torre, M.C.; Solsona, M.; Yébenes, J.C. Epidemiology of community-acquired severe sepsis. A population-based study. Med. Clin. 2016, 147, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Seymour, C.W.; Gesten, F.; Prescott, H.C.; Friedrich, M.E.; Iwashyna, T.J.; Phillips, G.S.; Lemeshow, S.; Osborn, T.; Terry, K.M.; Levy, M.M. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis. N. Engl. J. Med. 2017, 376, 2235–2244. [Google Scholar] [CrossRef] [PubMed]
- De Miguel-Yanes, J.M.; Andueza-Lillo, J.A.; Gonzalez-Ramallo, V.J.; Pastor, L.; Munoz, J. Failure to implement evidence-based clinical guidelines for sepsis at the ED. Am. J. Emerg. Med. 2006, 24, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Vallés, J.; Rello, J.; Ochagavía, A.; Garnacho, J.; Alcalá, M.A. Community-acquired bloodstream infection in critically ill adult patients: Impact of shock and inappropriate antibiotic therapy on survival. Chest 2003, 123, 1615–1624. [Google Scholar] [CrossRef] [PubMed]
- Dellinger, R.P.; Levy, M.M.; Carlet, J.M.; Bion, J.; Parker, M.M.; Jaeschke, R.; Reinhart, K.; Angus, D.C.; Brun-Buisson, C.; et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit. Care Med. 2008, 36, 296–327. [Google Scholar] [CrossRef] [PubMed]
- Yébenes, J.C. Chain for the resuscitation of septic patients. PsterSSpsiaGreu2016CSdMCC.
- Marshall, J.C.; Cook, D.J.; Christou, N.V.; Bernard, G.R.; Sprung, C.L.; Sibbald, W.J. Multiple organ dysfunction score: A reliable descriptor of a complex clinical outcome. Crit. Care Med. 1995, 23, 1638–1652. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.; Phillips, G.; Beale, R.; Cecconi, M.; Chiche, J.D.; De Backer, D.; Divatia, J.; Du, B.; Evans, L.; Ferrer, R.; et al. The Surviving Sepsis Campaign bundles and outcome: Results from the International Multicentre Prevalence Study on Sepsis (the IMPreSS study). Intensive Care Med. 2015, 41, 1620–1628. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, R.; Artigas, A.; Levy, M.M.; Blanco, J.; González-Díaz, G.; Garnacho-Montero, J.; Ibáñez, J.; Palencia, E.; Quintana, M.; de la Torre-Prados, M.V.; et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA 2008, 299, 2294–2303. [Google Scholar] [CrossRef] [PubMed]
- Coba, V.; Whitmill, M.; Mooney, R.; Horst, H.M.; Brandt, M.M.; Digiovine, B.; Mlynarek, M.; McLellan, B.; Boleski, G.; Yang, J.; et al. Resuscitation bundle compliance in severe sepsis and septic shock: Improves survival, is better late than never. J. Intensive Care Med. 2011, 26, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.B.; Corbett, S.W.; Steele, R.; Banta, J.; Clark, R.T.; Hayes, S.R.; Edwards, J.; Cho, T.W.; Wittlake, W.A. Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality. Crit. Care Med. 2007, 35, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Roberts, D.; Wood, K.E.; Light, B.; Parrillo, J.E.; Sharma, S.; Suppes, R.; Feinstein, D.; Zanotti, S.; Taiberg, L.; et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit. Care Med. 2006, 34, 1589–1596. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, R.; Martin-Loeches, I.; Phillips, G.; Osborn, T.M.; Townsend, S.; Dellinger, R.P.; Artigas, A.; Schorr, C.; Levy, M.M. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: Results from a guideline-based performance improvement program. Crit. Care Med. 2014, 42, 1749–1755. [Google Scholar] [CrossRef] [PubMed]
- Joo, Y.M.; Chae, M.K.; Hwang, S.Y.; Jin, S.C.; Lee, T.R.; Cha, W.C.; Jo, I.J.; Sim, M.S.; Song, K.; Jeong, Y.K.; et al. Impact of timely antibiotic administration on outcomes in patients with severe sepsis and septic shock in the emergency department. Clin. Exp. Emerg. Med. 2014, 1, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Puskarich, M.A.; Trzeciak, S.; Shapiro, N.I.; Arnold, R.C.; Horton, J.M.; Studnek, J.R.; Kline, J.A.; Jones, A.E. Emergency Medicine Shock Research Network (EMSHOCKNET). Association between timing of antibiotic administration and mortality from septic shock in patients treated with a quantitative resuscitation protocol. Crit. Care Med. 2011, 39, 2066–2071. [Google Scholar] [CrossRef] [PubMed]
- Lu, N.F.; Zheng, R.Q.; Lin, H.; Shao, J.; Yu, J.Q.; Yang, D.G. Improved sepsis bundles in the treatment of septic shock: A prospective clinical study. Am. J. Emerg. Med. 2015, 33, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Blot, S.I.; Rodriguez, A.; Solé-Violán, J.; Blanquer, J.; Almirall, J.; Rello, J. Community-Acquired Pneumonia Intensive Care Units (CAPUCI) Study Investigators. Effects of delayed oxygenation assessment on time to antibiotic delivery and mortality in patients with severe sepsis community-acquired pneumonia. Crit. Care Med. 2007, 35, 2509–2514. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.B.; Loomba, M.; Yang, J.J.; Jacobsen, G.; Shah, K.; Otero, R.M.; Suarez, A.; Parekh, H.; Jaehne, A.; Rivers, E.P. Early lactate clearance is associated with biomarkers of inflammation, coagulation, apoptosis, organ dysfunction and mortality in severe sepsis and septic shock. J. Inflamm. (Lond.) 2010, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- Ranzani, O.T.; Monteiro, M.B.; Ferreira, E.M.; Santos, S.R.; Machado, F.R.; Noritomi, D.T. Reclassifying the spectrum of septic patients using lactate: Severe sepsis, cryptic shock, vasoplegic shock and dysoxic shock. Rev. Bras. Ter. Intensiva 2013, 25, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Sterling, S.A.; Puskarich, M.A.; Shapiro, N.I.; Trzeciak, S.; Kline, J.A.; Summers, R.L.; Jones, A.E. Emergency Medicine Shock Research Network (EMSHOCKNET). Characteristics and outcomes of patients with vasoplegic versus tissue dysoxic septic shock. Shock 2013, 40, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Bermejo-Martin, J.F.; Martín-Fernandez, M.; Almansa, R. Pre-sepsis: A necessary concept to complete the SEPSIS-3 picture? J. Crit. Care 2017, 44, 148. [Google Scholar] [CrossRef] [PubMed]
- Yébenes, J.C. Early detection of sepsis: To adapt or to die. Med. Clin. 2017, 149, 209–210. [Google Scholar] [CrossRef] [PubMed]
- Giamarellos-Bourboulis, E.J.; Tsaganos, T.; Tsangaris, I.; Lada, M.; Routsi, C.; Sinapidis, D.; Koupetori, M.; Bristianou, M.; Adamis, G.; Mandragos, K.; et al. Validation of the new Sepsis-3 definitions: Proposal for improvement in early risk identification. Clin. Microbiol. Infect. 2017, 23, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Bermejo-Martin, J.F.; Almansa, R.; Yebenes, J.C. New Organ Failure as an Alternative Endpoint to Develop Diagnostic Criteria for Sepsis. Chest 2018, 153, 1278. [Google Scholar] [CrossRef] [PubMed]
- Allgöwer, M.; Buri, C. Schockindex. Deutsche Med. Wodenschrift 1967, 46, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Birkhahn, R.H.; Gaeta, T.J.; Terry, D.; Bove, J.J.; Tloczkowski, J. Shock Index in diagnosing early acute hypovolemia. Am. J. Emerg. Med. 2005, 23, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Berger, T.; Green, J.; Horeczko, T.; Hagar, Y.; Garg, N.; Suarez, A.; Panacek, E.; Shapiro, N. Shock Index and Early Recognition of Sepsis in the Emergency Department: Pilot Study. West. J. Emerg. Med. 2013, 14, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, N.I.; Arnold, R.; Sherwin, R.; O’Connor, J.; Najarro, G.; Singh, S.; Lundy, D.; Nelson, T.; Trzeciak, S.W.; Jones, A.E. The association of near-infrared spectroscopy-derived tissue oxygenation measurements with sepsis syndromes, organ dysfunction and mortality in emergency department patients with sepsis. Crit. Care 2011, 15, R223. [Google Scholar] [CrossRef] [PubMed]
- Claverias, L.; Marí, M.; Marín-Corral, J.; Magret, M.; Trefler, S.; Bodí, M.; García-España, A.; Yébenes, J.C.; Pascual, S.; Gea, J.; et al. The prognostic value of muscle regional oxygen saturation index in severe community-acquired pneumonia: A prospective observational study. J. Intensive Care 2016, 4, 7. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Deutschman, C.; Seymour, C.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 762–774. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.B.; Prytherch, D.R.; Meredith, P.; Schmidt, P.E.; Featherstone, P.I. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013, 84, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Churpek, M.M.; Snyder, A.; Han, X.; Sokol, S.; Pettit, N.; Howell, M.D.; Edelson, D.P. Quick Sepsis-related Organ Failure Assessment, Systemic Inflammatory Response Syndrome, and Early Warning Scores for Detecting Clinical Deterioration in Infected Patients outside the Intensive Care Unit. Am. J. Respir. Crit. Care Med. 2017, 195, 906–911. [Google Scholar] [CrossRef] [PubMed]
- Heldens, M.; Schout, M.; Hammond, N.E.; Bass, F.; Delaney, A.; Finfer, S.R. Sepsis incidence and mortality are underestimated in Australian intensive care unit administrative data. Med. J. 2018, 6, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, E.K.; Rubenstein, A.R.; Radin, G.T.; Wiener, R.S.; Walkey, A.J. Two decades of mortality trends among patients with severe sepsis: A comparative meta-analysis. Crit. Care Med. 2014, 42, 625–631. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).