It Takes a Village: Multidisciplinary Approach to Screening and Prevention of Pediatric Sleep Issues
Abstract
:1. Introduction
2. Pediatric Sleep Across Disciplines
2.1. Primary Care Providers
2.2. Behavioral Health Providers and Psychiatrists
2.3. Childcare Providers and School Personnel
2.4. Dentists and Otolaryngologists
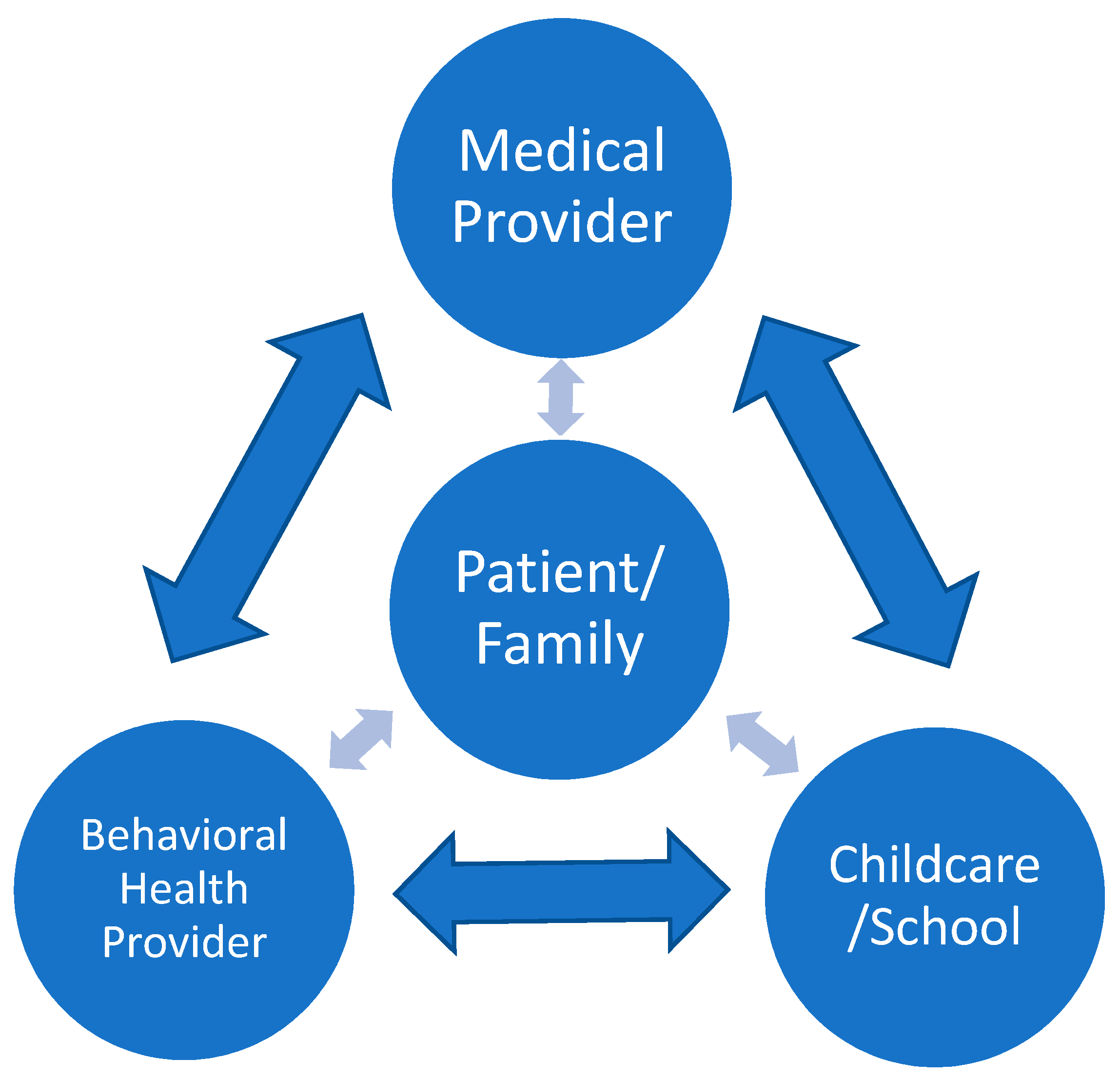
3. Multidisciplinary Sleep Model
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Baum, K.T.; Desai, A.; Field, J.; Miller, L.E.; Rausch, J.; Beebe, D.W. Sleep restriction worsens mood and emotional regulation in adolescents. J. Child Psychol. Psychiatry 2014, 55, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Beebe, D.W. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr. Clin. N. Am. 2011, 58, 649–665. [Google Scholar] [CrossRef] [PubMed]
- Beebe, D.W.; Simon, S.; Summer, S.; Hemmer, S.; Strotman, D.; Dolan, L.M. Dietary intake following experimentally restricted sleep in adolescents. Sleep 2013, 36, 827–834. [Google Scholar] [CrossRef] [PubMed]
- Garetz, S.L.; Mitchell, R.B.; Partker, P.D.; Moore, R.H.; Rosen, C.L.; Giordani, B.; Redline, S. Quality of life and obstructive sleep apnea symptoms after pediatric adenotonsillectomy. Pediatrics 2015, 135, e477–e486. [Google Scholar] [CrossRef] [PubMed]
- Sleep and Sleep Disorder Statistics; American Sleep Association: Lititz, PA, USA, 2018; Available online: www.sleepassociation.org/about-sleep/sleep-statistics (accessed on 28 August 2018).
- Meltzer, L.J.; Johnson, C.; Crosetter, J.; Ramos, M.; Mindell, J.A. Prevalence of diagnoses sleep disorders in pediatric primary care practices. Pediatrics 2010, 125, 1410–1418. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.A.; Mendelsohn, J.; Obermeyer, W.H.; Amromin, J.; Benca, R. Sleep and behavior problems in school-aged children. Pediatrics 2001, 107, 1–9. [Google Scholar] [CrossRef]
- Hagan, J.F.; Shaw, J.S.; Duncan, P.M. (Eds.) Guidelines for health supervision of infants, children, and adolescents. In Bright Futures, 4th ed.; American Psychological Association: Worcester, MA, USA, 2017. [Google Scholar]
- Mindell, J.A.; Owens, J.A. A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems, 3rd ed.; Lippincott Williams & Williams: Philadelphia, PA, USA, 2015; ISBN 978-1451193008. [Google Scholar]
- Honaker, S.M.; Saunders, T. The Sleep Checkup: Sleep screening, guidance, and management in pediatric primary care. Clin. Pract. Pediatr. Psychol. 2018, 6, 201–210. [Google Scholar] [CrossRef]
- Dahl, R.E. Biological, developmental, and neurobehavioral factors relevant to adolescent driving risks. Am. J. Prev. Med. 2008, 35, S278–S284. [Google Scholar] [CrossRef] [PubMed]
- Taras, H.; Potts-Datema, W. Sleep and student performance at school. J. School Health 2005, 75, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.E.; Miller, A.L.; Bonuck, K.; Lumeng, J.C.; Chervin, R.D. Evaluation of a sleep education program for low-income preschool children and their families. Sleep 2014, 37, 1117–1125. [Google Scholar] [CrossRef] [PubMed]
- Quach, J.; Hisock, H.; Ukoumunne, O.C.; Wake, M. A brief sleep intervention improves outcomes in the school entry year: A randomized control trial. Pediatrics 2011, 128, 692–701. [Google Scholar] [CrossRef] [PubMed]
- Moseley, L.; Gradisar, M. Evaluation of school-based intervention for adolescent sleep problems. Sleep 2009, 32, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Cain, N.; Gradisar, M.; Moseley, L. A motivational school-based intervention for adolescent sleep problems. Sleep Med. 2011, 12, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Danner, F.; Philips, B. Adolescent sleep, school start times, and teen motor vehicle crashes. J. Clin. Sleep Med. 2008, 4, 533–535. [Google Scholar] [PubMed]
- Owens, J.A.; Belon, K.; Moss, P. Impact of delaying school start time an adolescent sleep, mood, and behavior. Arch. Pediatr. Adolesc. Med. 2010, 164, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Arguelles, L.; Jiang, F.; Chen, W.; Jin, X.; Yan, C.; Tian, Y.; Hong, X.; Qian, C.; Zhang, J.; et al. Sleep, school performance, and a school-based intervention among school-aged children: A sleep series study in China. PLoS ONE 2013, 8, e67928. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics. Policy statement: School start times and adolescents. Pediatrics 2014, 642–649. [CrossRef]
- American Academy of Pediatric Dentistry. Policy on Obstructive Sleep Apnea. Oral Health Policies 2016, 39, 96–98. [Google Scholar]
- Ask Your Doctor about Regular Dental Visits. Am. Acad. Pediatr. Dent. 2011. Available online: www.aapd.org (accessed on 30 July 2018).
- Major, M.P.; El-Hakim, H.; Witmans, M.; Major, P.W.; Flores-Mir, C. Adenoid hypertrophy in pediatric sleep disordered breathing and craniofacial growth: The emerging role of dentistry. J. Dent. Sleep Med. 2014, 1, 83–87. [Google Scholar] [CrossRef]
- Brown, K. Pediatric consideration in sedation for patients with obstructive sleep apnea syndrome. Semin. Anesth. Perioper. Med. Pain 2007, 26, 94–102. [Google Scholar] [CrossRef]
- Chiang, H.K.; Cronly, J.K.; Best, A.M.; Brickhouse, T.H.; Leszczyszyn, D.J. Development of a simplified pediatric obstructive sleep apnea (OSA) screening tool. J. Dental Sleep Med. 2015, 2, 163–173. [Google Scholar] [CrossRef]
- Herrera, M.; Valencia, I.; Grant, M.; Metroka, D.; Chialastri, A.; Kothare, S.V. Bruxism in children: Effect on sleep architecture and daytime cognitive performance and behavior. Sleep 2006, 29, 1143–1148. [Google Scholar] [CrossRef] [PubMed]
- Lous, J.; Burton, M.J.; Felding, J.U.; Ovesen, T.; Rovers, M.M.; Williamson, I. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst. Rev. 2005, 1, 1–46. [Google Scholar] [CrossRef]
- Paradise, J.L.; Feldman, H.M.; Campbell, T.F.; Dollaghan, C.A.; Colborn, D.K.; Bernard, B.S.; Rockette, H.E.; Janosky, J.E.; Pitcairn, D.L.; Sabo, D.L.; et al. Effect of early or delayed insertion of tympanostomy tubes for persistent otitis media on developmental outcomes at the age of three years. N. Engl. J. Med. 2001, 344, 1179–1187. [Google Scholar] [CrossRef] [PubMed]
- Brietzke, S.; Gallagher, D. The effectiveness of tonsillectomy and adenoidectomy in the treatment of pediatric obstructive sleep apnea/hypopnea syndrome: A meta-analysis. Otolaryngol. Head Neck Surg. 2006, 136, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.J.; Pitson, D.J.; Stradling, J.R. Snoring, sleep disturbance, and behaviour in 4–5-year olds. Arch. Dis. Child. 1993, 68, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Redline, S.; Tishle, P.V.; Schluchter, M.; Aylor, J.; Clark, K.; Graham, G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am. J. Respir. Crit. Care Med. 1999, 159, 1527–1532. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, L.J.; Moore, M.; Mindell, J.A. The need for interdisciplinary pediatric sleep clinics. Behav. Sleep Med. 2008, 6, 266–282. [Google Scholar] [CrossRef] [PubMed]
| Sleep Anticipatory Guidance: Infants | |
|---|---|
| Primary Care Provider | 1 to 6 Months - Encourage parents to get plenty of sleep and sleep when infant is sleeping - Help baby wake for feedings by light patting, changing the diaper, or undressing - Continue to offer feeds during the night every 3 h - Put infant to sleep on his/her back; choose a crib with slats 2 ⅜ inches apart; do not use loose, soft bedding - Put baby to sleep drowsy but awake - Pay attention to infant’s cues for sleep - Develop a schedule for naps and nighttime sleep - Infant should sleep in crib in caregiver’s room - Do not but baby in crib with a bottle - Create daily routine for naps and bedtime for baby - Choose mesh playpen with weave less than ¼ inches 7 to 12 Months - Discuss changing sleep pattern - Discuss limit setting and positive discipline - Nighttime feeds not necessary |
| Behavioral Health Provider | 1 to 6 Months - Provide coping skill recommendations to caregivers to help with transition of having a newborn at home and impact on parental sleep and stress level - Help family set a consistent schedule and routine for sleep - Provide psychoeducation on sleep-onset associations - Discuss routine for feeds - Provide psychoeducation on daytime disruptive behavior management (i.e., differential attention) 7 to 12 Months - Help family gradually reduce nighttime feeds - Further discuss limit-setting techniques and positive discipline |
| Childcare/School | 1 to 6 Months - Maintain regular sleep and feeding schedules - Maintain safety recommendations - Put baby to sleep drowsy but awake - Implement consistent routine for sleep - Provide feedback to caregivers on daytime sleep habits - Support independent sleep onset and reduce feedings during naps 7 to 12 Months - Provide family with feedback on helpful behavioral strategies and positive discipline techniques used at daycare - Monitor sleepiness outside of daily sleep schedule - Monitor developmental performance (i.e., cognitive, oral, and motor development) |
| Dentist/Otolaryngologist | - First visit with a dentist by the time of eruption of first tooth or first birthday - Screen for breathing concerns, oral and craniofacial abnormalities, and obstructions |
| Sleep Anticipatory Guidance: Toddlers (1 to 3 Years) | |
| Primary Care Provider | - Continue one nap per day - Follow nightly bedtime routine - Encourage quiet time such as reading, singing, and a favorite toy before bed - Maintain consistent bedtime routines and sleep times - Discuss night awakenings: parents should reassure briefly, give a preferred object (blanket or stuffed animal), and put back to bed - Do not put TV, computer, or digital device in bedroom - No bottle in bed - Use methods other than TV or digital media when tired to improve calming behavior |
| Behavioral Health Provider | - Discuss nap schedule so as to not disrupt nighttime sleep - Discuss use of transitional object for sleep and how to decrease maladaptive sleep onset associations - Discuss limit setting around electronics and digital media for sleep |
| Childcare/School | - Maintain consistent naptime earlier in the afternoon to avoid impact on nighttime sleep - Use transitional object at naptime - Continue to monitor developmental gains and recommend early intervention services or developmental assessment as indicated - Assess for sleep concerns if developmental delays appear evident |
| Dentist/Otolaryngologist | - Encourage regular dental visits (i.e., every 6 months) - Dentist discusses incorporating nightly oral hygiene habits into bedtime routine - Dentist screens for consumption of sugary and caffeinated drinks and provide education on impact of dental health and sleep - Screen for tonsillar hypertrophy, oral and craniofacial abnormalities, and nighttime breathing concerns and mouth breathing; may use pediatric-adapted screening tools such as STOP-BANG [25] - Dentist assesses for and provide psychoeducation about bruxism - Dentist discusses use of positional therapy to reduce snoring or bruxism - Otolaryngologist screens for obstructive sleep apnea (OSA) |
| Sleep Anticipatory Guidance: School-Aged Children | |
| Primary Care Provider | - Create and maintain a calm bedtime routine - Limit TV to no more than 1 h a day, no TV in bedroom - Monitor school performance and consider impact of poor sleep on tardiness, daytime behavior - Consider implementing a family media plan to balance needs of physical activity, sleep, school, and quiet time without media (www.healthychildren.org/mediauseplan) - Maintain consistent sleep routine (even on weekends) to obtain adequate sleep - Do not operate machinery, especially motor vehicles, when drowsy - Discuss maintaining a sleep routine in light of other activities, work, school, exercise, extracurricular activities, free time - Provide psychoeducation around proper use of melatonin if used |
| Behavioral Health Provider | - Help family establish a consistent bedtime routine that is not too long (e.g., bath, brush teeth, PJs, story, lights out) - Encourage daytime exercise and limit electronics use; eliminate TV and other screens at least 1 h before bed - Introduce Cognitive Behavioral Therapy (CBT) strategies for older children to help calm bedtime fears, anxiety, and mood concerns - Help family implement behavioral strategies for bedtime refusal, night awakenings, and parasomnias - Discuss daily schedule to maintain balance between school, friends, homework, and work - Discuss setting limits around driving a vehicle if sleep deprived |
| School | - Monitor drowsiness in school, report episodes of sleep during school day to caregivers - Monitor academic and behavioral performance; assess sleep difficulties when evaluating concerns - Introduce psychoeducation on sleep during class time and to parents during parent-teacher meetings and back-to-school night - Monitor tardiness, school attendance, and changes in mood or anxiety levels - Encourage regular exercise (e.g., PE classes) - Consider changing school start times - Provide psychoeducation on the impact of poor sleep on driving behavior and safety - Manage school schedules so extracurricular activities do not occur too early in the morning or too late at night |
| Dentist/Otolaryngologist | - Dentist assesses for tooth wear and screen for bruxism if wear is evident - Otolaryngologist screens for and monitors tonsillar hypertrophy and sleep-disordered breathing concerns; screens for OSA before sedating a child for oral surgery - Otolaryngologist discusses impact of obesity on breathing-related sleep disorders - Otolaryngologist discusses impact of decongestants and corticosteroids on sleep - Otolaryngologist screens for nocturnal enuresis in patients who snore - Discuss nonsurgical appliances to help correct oral abnormalities that may impact sleep-disordered breathing |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sevecke, J.R.; Meadows, T.J. It Takes a Village: Multidisciplinary Approach to Screening and Prevention of Pediatric Sleep Issues. Med. Sci. 2018, 6, 77. https://doi.org/10.3390/medsci6030077
Sevecke JR, Meadows TJ. It Takes a Village: Multidisciplinary Approach to Screening and Prevention of Pediatric Sleep Issues. Medical Sciences. 2018; 6(3):77. https://doi.org/10.3390/medsci6030077
Chicago/Turabian StyleSevecke, Jessica R., and Tawnya J. Meadows. 2018. "It Takes a Village: Multidisciplinary Approach to Screening and Prevention of Pediatric Sleep Issues" Medical Sciences 6, no. 3: 77. https://doi.org/10.3390/medsci6030077
APA StyleSevecke, J. R., & Meadows, T. J. (2018). It Takes a Village: Multidisciplinary Approach to Screening and Prevention of Pediatric Sleep Issues. Medical Sciences, 6(3), 77. https://doi.org/10.3390/medsci6030077




