Validation of an ICD-9-CM-Based Monitoring Tool for Regional Trauma Systems: The PaTraME Study in Pavia Province, Italy
Abstract
1. Introduction
2. Materials and Methods
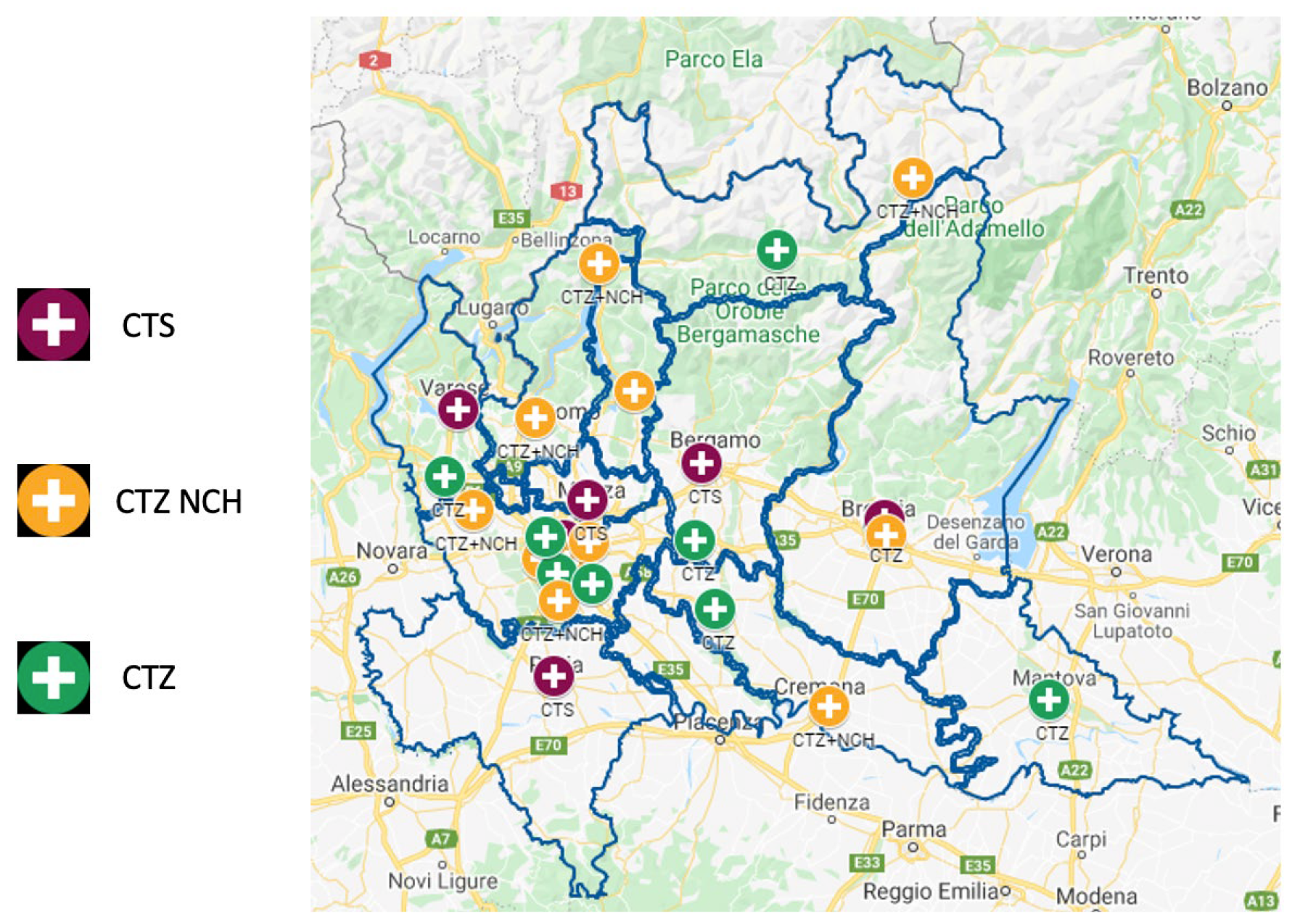
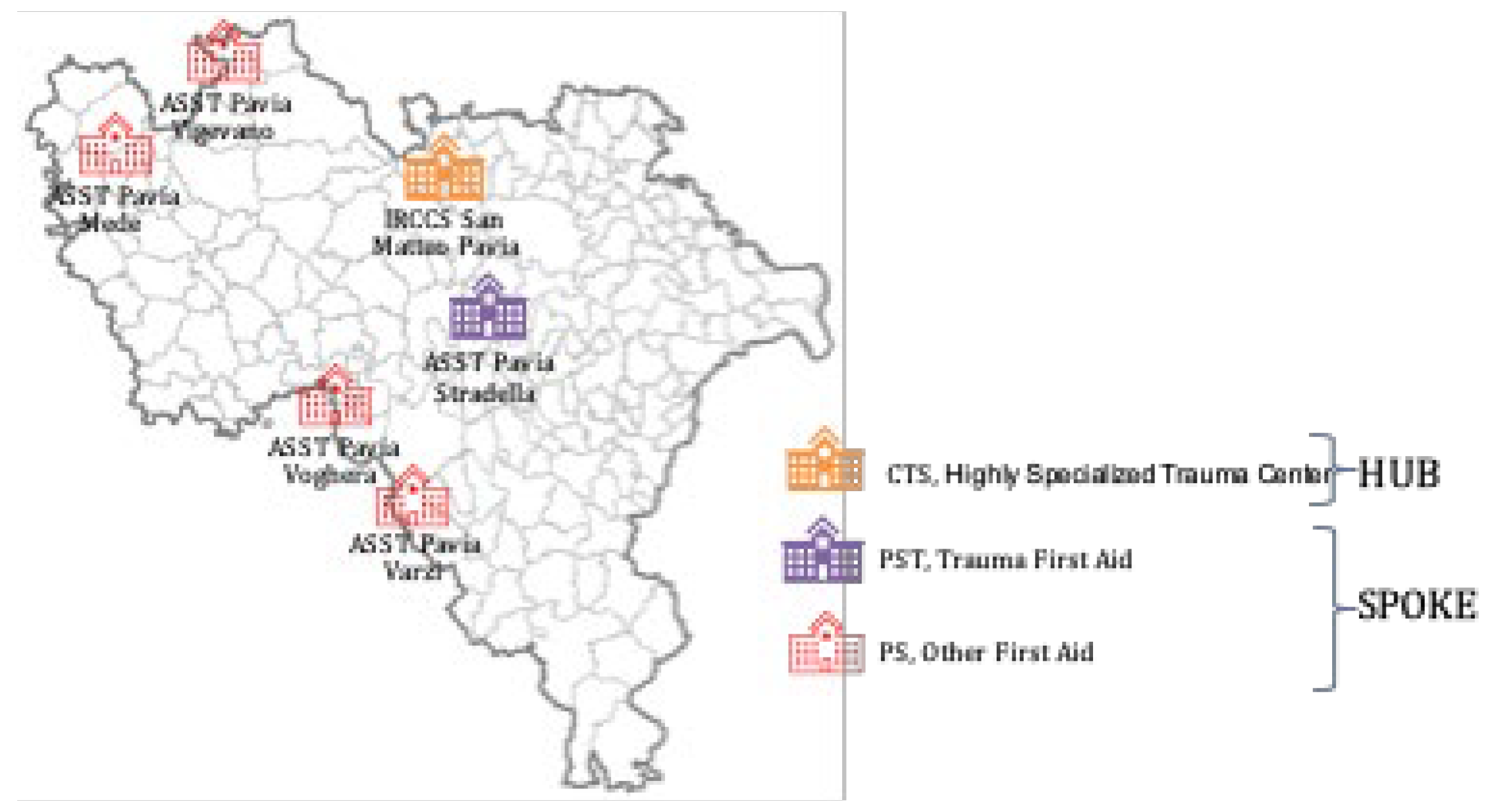
2.1. Study Design and Setting
2.2. Aim
2.3. Data Sources
- SDO (Hospital Discharge Records): all hospital episodes with any ICD-9-CM code in the trauma ranges (800.xx–904.xx, 920.xx–939.xx, 950.xx–959.xx).
- Emergency Room flow (PS flow): ED visits linked to subsequent SDOs, including arrival mode (118 ambulance, self-presenting, helicopter), triage code, and primary complaint.
- Mortality registry: date and cause of death up to 180 days post-admission.
2.4. Variables Collected
- Demographics: anonymous patient ID, sex, date of birth, and residence.
- Admission details: date/time of ED arrival and hospital admission, hospital ID, ward of entry and discharge, and mode of transport.
- Clinical codes: all ICD-9-CM diagnoses (up to five), procedures (up to five), and DRG.
- Transfers: intra-hospital transfers and secondary transfers to hub (date/time).
- Outcomes: in-hospital death and vital status at 30 days and 180 days post-admission.
2.5. Severity Scoring
- XISS: an indirect Injury Severity Score analogous to AIS-derived ISS.
- TMPM-POD: the Trauma Mortality Probability Model.
2.6. Statistical Analysis
3. Results
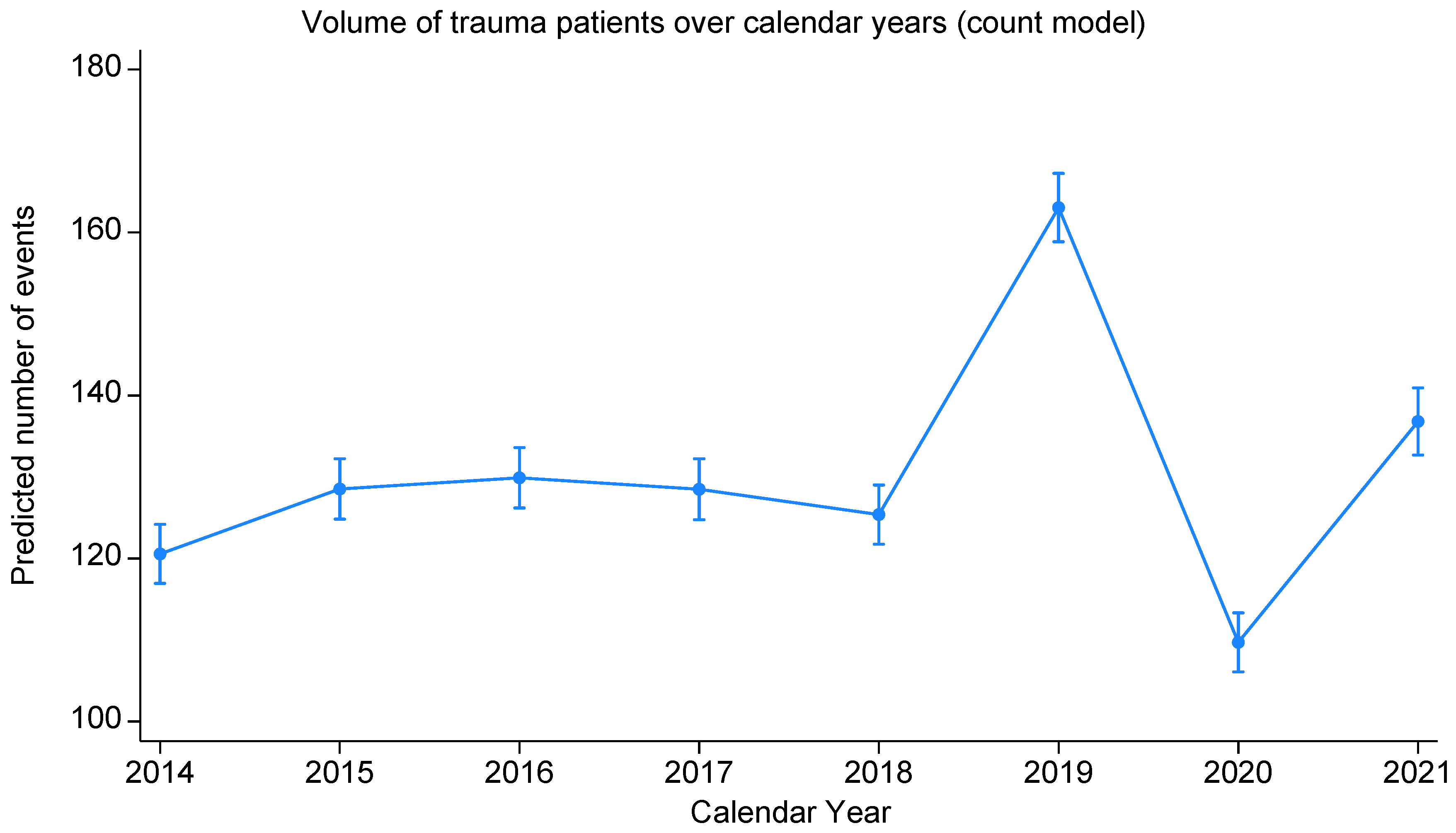
3.1. Epidemiology and Case Volumes
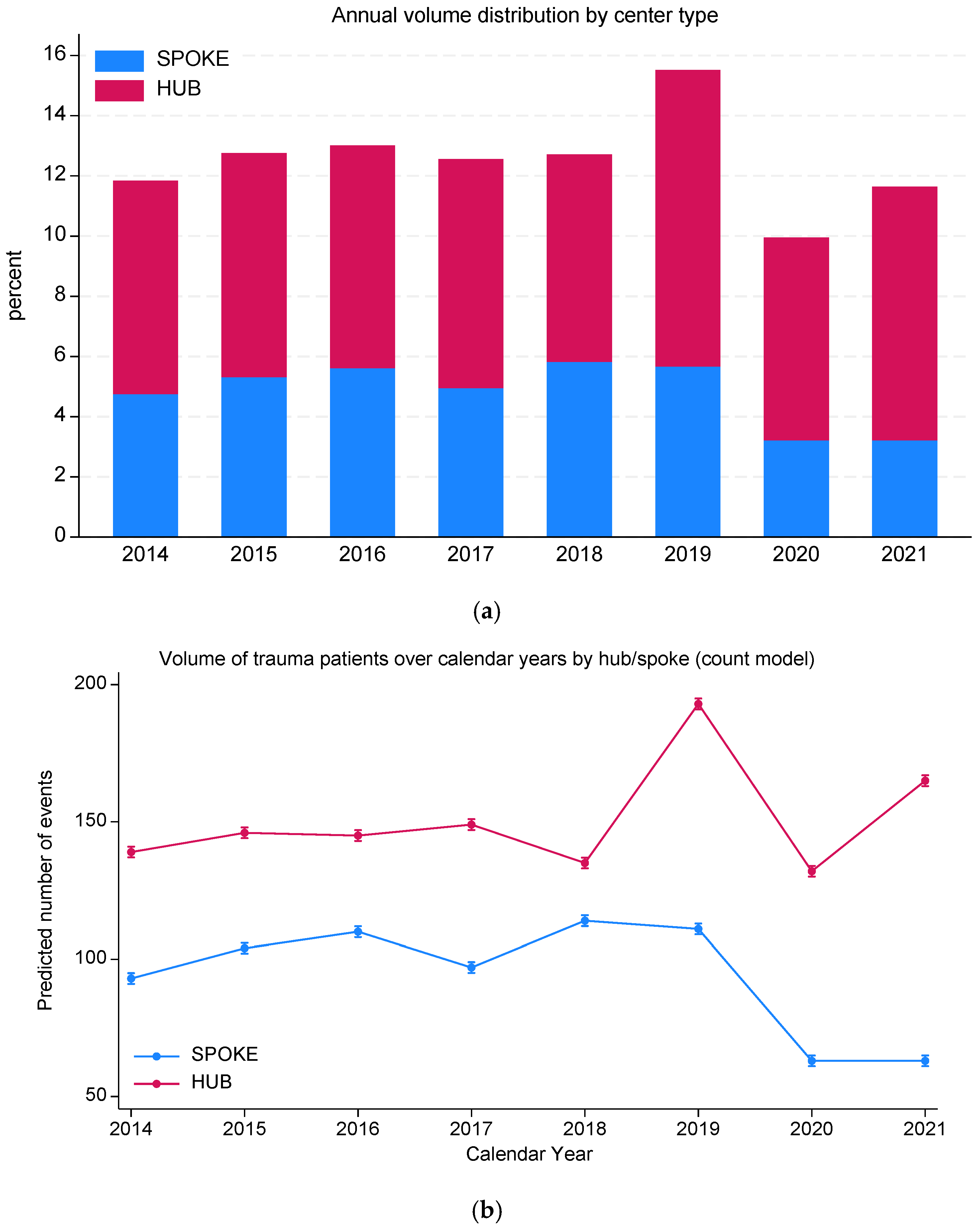
3.2. Centralization Trends and System Quality
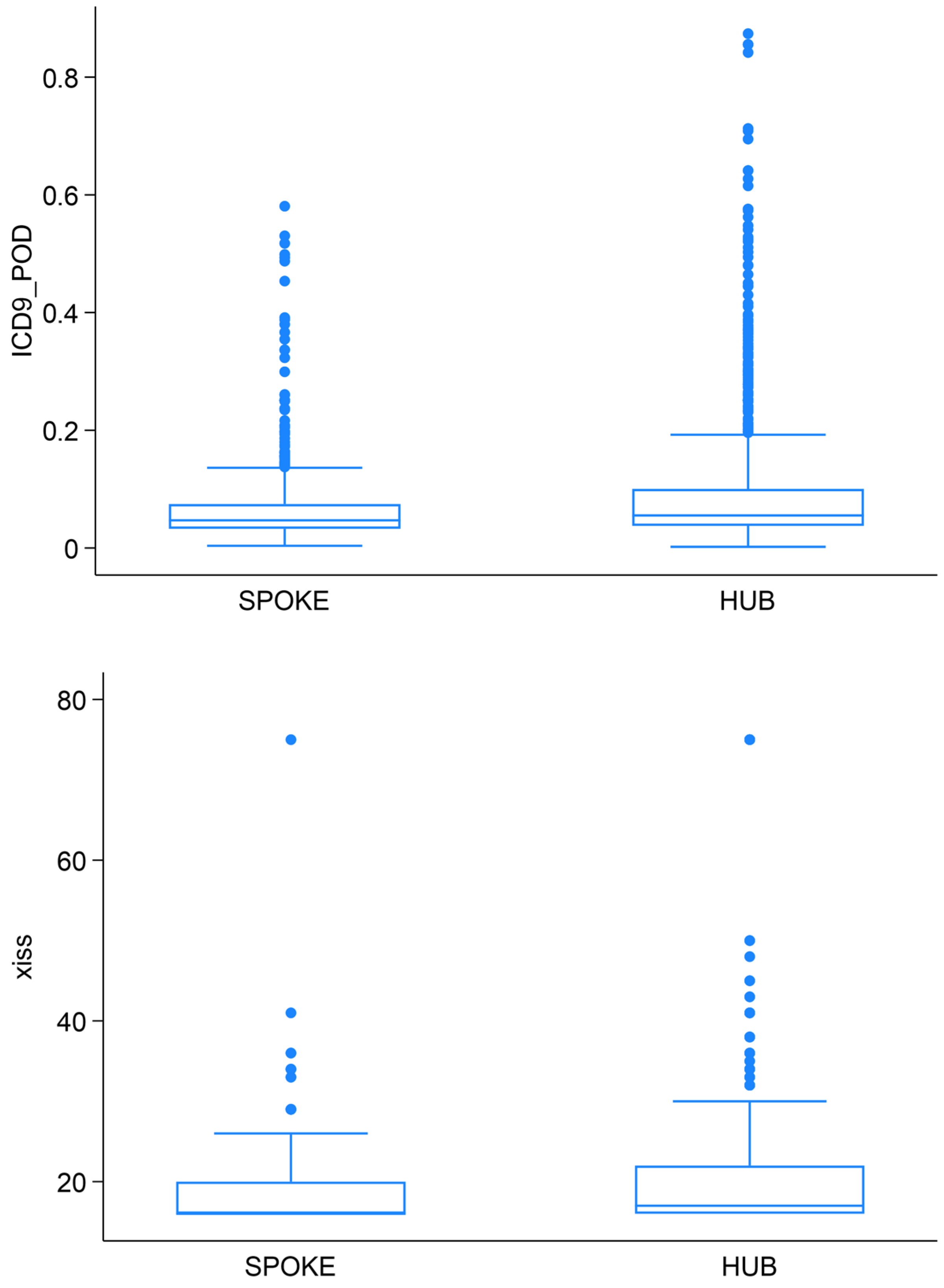
3.3. Severity-Score Distributions
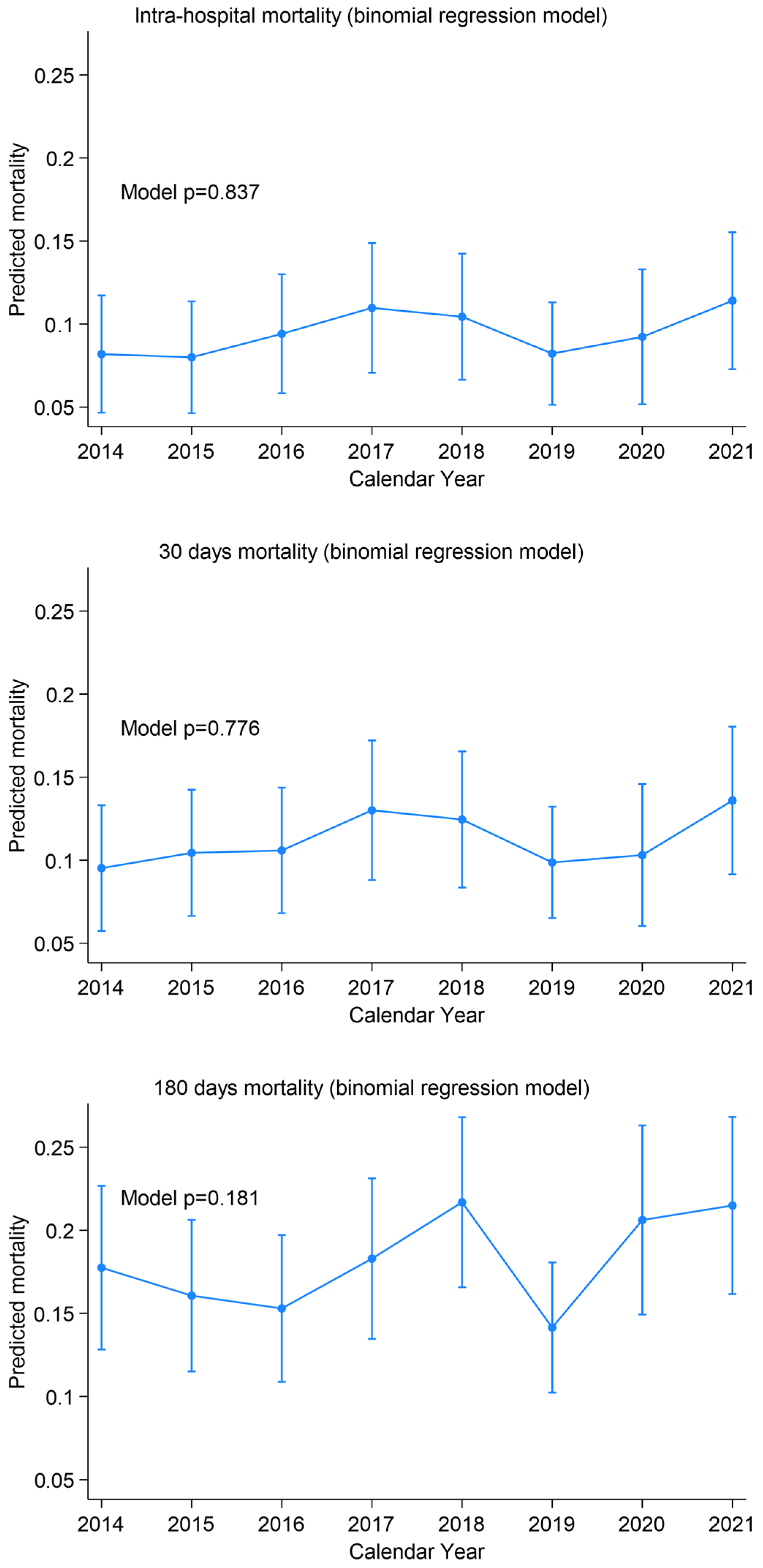
3.4. Mortality Overview
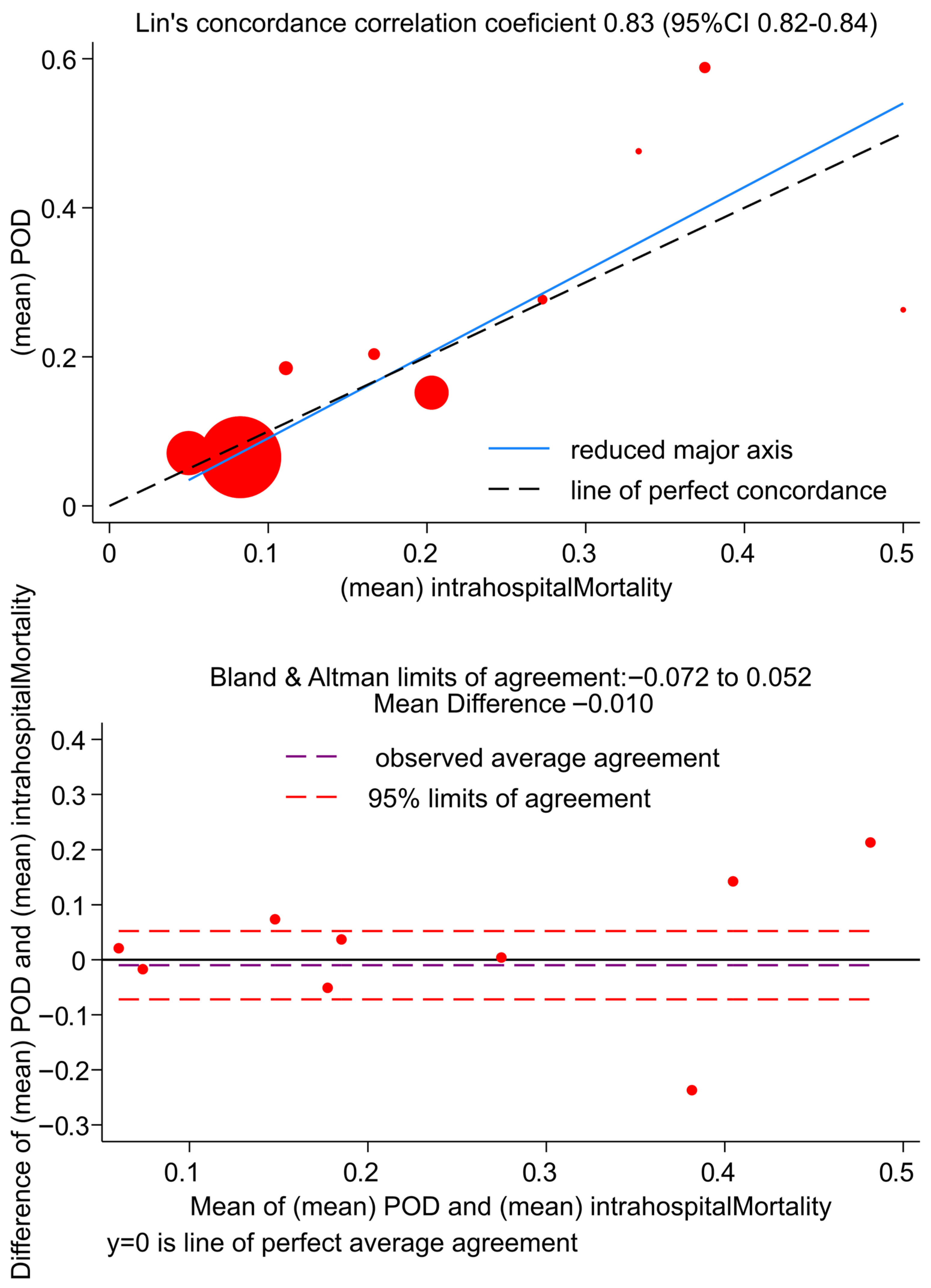
3.5. Correlation Between TMPM-POD and In-Hospital Mortality
4. Discussion
- Case volume varied significantly between 2014 and 2021, with a steady increase until 2019, a marked drop during the COVID-19 pandemic in 2020, and a partial rebound in 2021; these fluctuations highlight the need for continuous monitoring and network readiness.
- Severity distributions (XISS and TMPM-POD) were higher in patients admitted to the hub versus spoke centers, confirming the tool’s ability to reflect case complexity.
- Centralization to the hub improved significantly, reflecting enhanced prehospital triage, Emergency Medical Services (EMS) training, and adherence to regional protocols. The regional trauma-network structure and EMS centralization framework remained formally stable throughout the study period, as defined by Lombardy Regional Decree n. 8531 (01/10/2012), including hospital designation (CTS/PST) within the provincial network. Hence, the observed improvement in centralization over time likely reflects system maturation and organizational learning (e.g., increased experience, strengthened coordination, and continuous training), rather than a change in formal protocols. Nevertheless, we acknowledge that external factors not captured in administrative data—such as demographic changes and local organizational refinements—may have influenced centralization patterns and should be considered when informing policy decisions.
- Mortality (in-hospital, 30-day, and 180-day) showed no significant trends, confirming that increased centralization and stable patient volumes did not compromise overall outcomes, but rather maintained high-quality care.
- Zero-cost scalability: Every hospital collects SDO for reimbursement; no dedicated registry infrastructure or manual coding is required beyond applying the free TMPM module in Stata. This makes the approach readily adoptable by regions or countries using ICD coding.
- Real-time monitoring and benchmarking: Health authorities can generate regular reports on case volumes, severity distributions, centralization, and mortality without incremental costs. Such reports enable identification of undertriage “hot spots,” seasonal surges, or gaps in EMS coverage.
- Policy and planning: Mapping centralization against EMS response times, spoke distribution, and hospital capacity, planners can optimize resource allocation (e.g., positioning of air-ambulance bases or adding training in peripheral EDs) to further improve hub access.
- Severity stratification: Clear differences in XISS and TMPM-POD between hub and spoke patients validate the discriminative power of the tool, highlighting spoke hospitals consistently receiving higher-severity cases than is safe for their resources.
- Identification of improvement margins: Although hub-admission has increased, 38.5% of major-trauma cases still presented to spoke centers—an undertriage rate that could be reduced. Moreover, spoke patients’ mean XISS, while lower than hub cases, remains relatively high for facilities with limited trauma resources, suggesting need for targeted training or restructuring.
- Extensibility to other outcomes: The same dataset can be analyzed for other quality indicators—such as splenectomy rates in blunt abdominal trauma, length of stay or distribution of interventions (e.g., angioembolization or surgical airway). Incorporating such metrics could build a comprehensive trauma performance dashboard.
- National and international benchmarking: Standardizing on XISS/TMPM-POD across all Italian provinces (or regions using ICD-9/10-CM) would enable direct comparisons of system performance, promoting best-practice sharing and quality improvement initiatives.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ICD-9-CM | International Classification of Disease—9th revision—Clinical Modification |
| SDO | Scheda Dimissione Ospedaliera (Hospital Discharge Records) |
| GAT | Technical Study Group |
| CTS | Highly Specialized Trauma Center |
| CTZ | Zone Trauma Centre |
| PST | Trauma First Aid |
| SIAT | Integrated System for Trauma Patient Care |
| TMPM | Trauma Mortality Probability Model |
| POD | Probability of Death |
| PaTraME | Pavia Trauma Management Epidemiology |
| XISS | Extended Injury Severity Score |
| ED | Emergency Department |
| IRR | Incidence Rate Ratio |
| CI | Confidence Interval |
References
- World Health Organization. Preventing Injuries and Violence: An Overview; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Chiara, O.; Gordini, G.; Nardi, G.; Sanson, G. Trauma Care: La Cura Definitiva del Trauma Maggiore; Elsevier Health Sciences: Milan, Italy, 2012. [Google Scholar]
- Glance, L.G.; Osler, T.M.; Mukamel, D.B.; Meredith, W.; Wagner, J.; Dick, A.W. TMPM–ICD9: A trauma mortality prediction model based on ICD-9-CM codes. Ann. Surg. 2009, 249, 1032–1039. [Google Scholar] [CrossRef] [PubMed]
- Fugazzola, P.; Agnoletti, V.; Bertoni, S.; Martino, C.; Tomasoni, M.; Coccolini, F.; Gamberini, E.; Russo, E.; Ansaloni, L. The value of trauma patients’ centralization: An analysis of a regional Italian trauma system performance with TMPM-ICD-9. Intern. Emerg. Med. 2021, 16, 1951–1958. [Google Scholar] [CrossRef] [PubMed]
- Gagné, M.; Moore, L.; Beaudoin, C.; Batomen Kuimi, B.L.; Sirois, M.J. Performance of International Classification of Diseases–based injury severity measures used to predict in-hospital mortality: A systematic review and meta-analysis. J. Trauma Acute Care Surg. 2016, 80, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Cook, A.; Weddle, J.; Baker, S.; Hosmer, D.; Glance, L.; Friedman, L.; Osler, T. A comparison of the injury severity score and the trauma mortality prediction model. J. Trauma Acute Care Surg. 2014, 76, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Regione Lombardia. D.d.g. 1 ottobre 2012, n. 8531: Determinazioni in merito all’organizzazione di un sistema integrato per l’assistenza al trauma maggiore. Bollettino Ufficiale della Regione Lombardia (BURL) 2012, Anno XLII, N. 248, Serie Ordinaria n. 40 (05 October 2012). 2012, pp. 61–73. Available online: https://www.comune.suzzara.mn.it/servizi/gestionedocumentale/visualizzadocumento.aspx?ID=25971 (accessed on 19 December 2025).
- Greene, N.H.; Kernic, M.A.; Vavilala, M.S.; Rivara, F.P. Validation of ICDPIC software injury severity scores using a large regional trauma registry. Inj. Prev. 2015, 21, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.E.; Osler, T.M.; Hahn, D.R. ICDPIC: Stata Module to Provide Methods for Translating International Classification of Diseases (Ninth Revision) Diagnosis Codes into Standard Injury Categories and/or Scores. Statistical Software Components. 2010. Available online: https://ideas.repec.org/c/boc/bocode/s457028.html (accessed on 13 October 2025).
- Vallmuur, K.; Cameron, C.M.; Watson, A.; Warren, J. Comparing the accuracy of ICD-based severity estimates to trauma registry-based injury severity estimates for predicting mortality outcomes. Injury 2021, 52, 1732–1739. [Google Scholar] [CrossRef] [PubMed]
- Fleischman, R.J.; Mann, N.C.; Dai, M.; Holmes, J.F.; Wang, N.E.; Haukoos, J.; Hsia, R.Y.; Rea, T.; Newgard, C.D. Validating the use of ICD-9 code mapping to generate injury severity scores. J. Trauma Nurs. 2017, 24, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.L.; Wang, M.C. Accuracy of ICD-9-CM coding of cervical spine fractures: Implications for research using administrative databases. Ann. Adv. Automot. Med. 2008, 52, 101–108. [Google Scholar] [PubMed]
- Bazarian, J.J.; Veazie, P.; Mookerjee, S.; Lerner, E.B. Accuracy of mild traumatic brain injury case ascertainment using ICD-9 codes. Acad. Emerg. Med. 2006, 13, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Agenzia Nazionale per i Servizi Sanitari Regionali. Quarta Indagine Nazionale Sullo Stato di Attuazione Delle Reti Tempo-Dipendenti; Rapporto su Dati 2023; Agenzia Nazionale per i Servizi Sanitari Regionali: Rome, Italy, 2025. [Google Scholar]
| Characteristics | Median (IQR) N (%) N = 1959 |
|---|---|
| Age (years) | 77.0 (59–85) * |
| Gender (male) | 1043 (55.7) * |
| XISS | 17.0 (16–20) |
| TMPM-POD | 0.05 (0.04–0.09) |
| Variable | N (%) | IRR (95%CI) vs. Previous | p-Value * | Interaction of Year and Centre p-Value | Spoke N (%) | p-Value | Hub N (%) | p-Value * |
|---|---|---|---|---|---|---|---|---|
| YEAR | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| 2014 | 232 (12) | 1 | 93 (12) | 139 (11) | ||||
| 2015 | 250 (13) | 1.07 (1.05–1.10) | 0.073 | 104 (14) | 146 (12) | |||
| 2016 | 255 (13) | 1.02 (0.99–1.04) | 0.811 | 110 (15) | 145 (12) | |||
| 2017 | 246 (12) | 0.97 (0.95–1.00) | 0.022 | 97 (13) | 149 (12) | |||
| 2018 | 249 (13) | 1.00 (0.98–1.03) | 1.000 | 114 (15) | 135 (11) | |||
| 2019 | 304 (15) | 1.25 (1.23–1.28) | <0.001 | 111 (15) | 193 (16) | |||
| 2020 | 195 (10) | 0.66 (0.64–0.68) | <0.001 | 63 (8) | 132 (11) | |||
| 2021 | 228 (12) | 1.22 (1.19–1.26) | <0.001 | 63 (8) | 165 (14) | |||
| Centre Type | <0.001 | - | - | - | - | |||
| Spoke | 755 (39) | 1 | ||||||
| Hub | 1204 (61) | 1.56 (1.54–1.57) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Fugazzola, P.; Gentile, L.; Chiarolanza, F.; Perotti, P.; Alessiani, M.; Capra Marzani, F.; Cobianchi, L.; Frassini, S.; Grassi, F.A.; Klersy, C.; et al. Validation of an ICD-9-CM-Based Monitoring Tool for Regional Trauma Systems: The PaTraME Study in Pavia Province, Italy. Med. Sci. 2026, 14, 13. https://doi.org/10.3390/medsci14010013
Fugazzola P, Gentile L, Chiarolanza F, Perotti P, Alessiani M, Capra Marzani F, Cobianchi L, Frassini S, Grassi FA, Klersy C, et al. Validation of an ICD-9-CM-Based Monitoring Tool for Regional Trauma Systems: The PaTraME Study in Pavia Province, Italy. Medical Sciences. 2026; 14(1):13. https://doi.org/10.3390/medsci14010013
Chicago/Turabian StyleFugazzola, Paola, Leandro Gentile, Francesco Chiarolanza, Pietro Perotti, Mario Alessiani, Federico Capra Marzani, Lorenzo Cobianchi, Simone Frassini, Federico Alberto Grassi, Catherine Klersy, and et al. 2026. "Validation of an ICD-9-CM-Based Monitoring Tool for Regional Trauma Systems: The PaTraME Study in Pavia Province, Italy" Medical Sciences 14, no. 1: 13. https://doi.org/10.3390/medsci14010013
APA StyleFugazzola, P., Gentile, L., Chiarolanza, F., Perotti, P., Alessiani, M., Capra Marzani, F., Cobianchi, L., Frassini, S., Grassi, F. A., Klersy, C., Muzzi, A., Palo, A., Perlini, S., Raimondi, M., Ansaloni, L., & on behalf of the PaTraME Study Group. (2026). Validation of an ICD-9-CM-Based Monitoring Tool for Regional Trauma Systems: The PaTraME Study in Pavia Province, Italy. Medical Sciences, 14(1), 13. https://doi.org/10.3390/medsci14010013






