Breast Cancer Progression and Its Theranostic Management via Folate-Directed Targeting of Glycoprotein Receptor
Abstract
1. Introduction
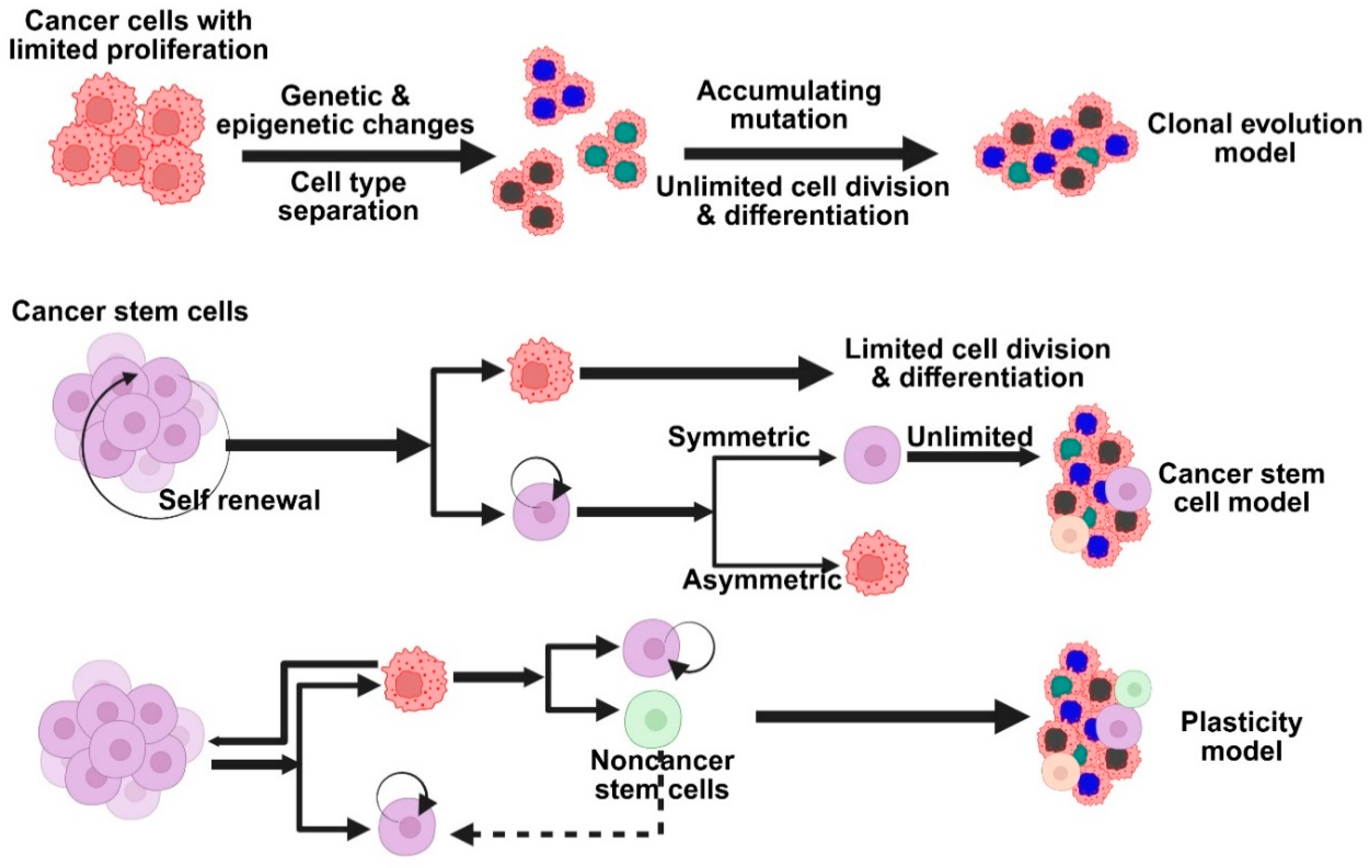
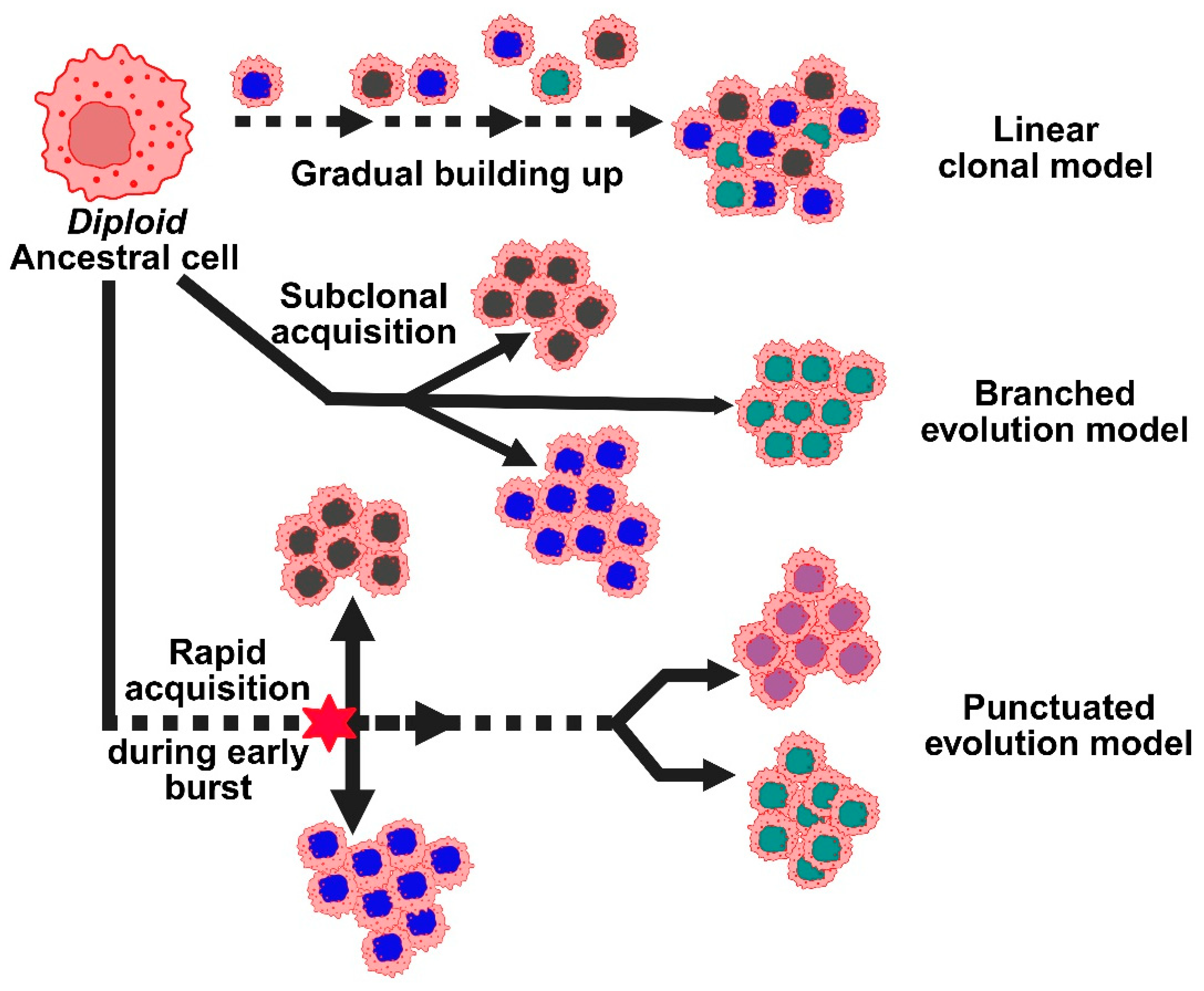
2. Progression of Breast Cancer
2.1. Pathophysiology of Breast Cancer
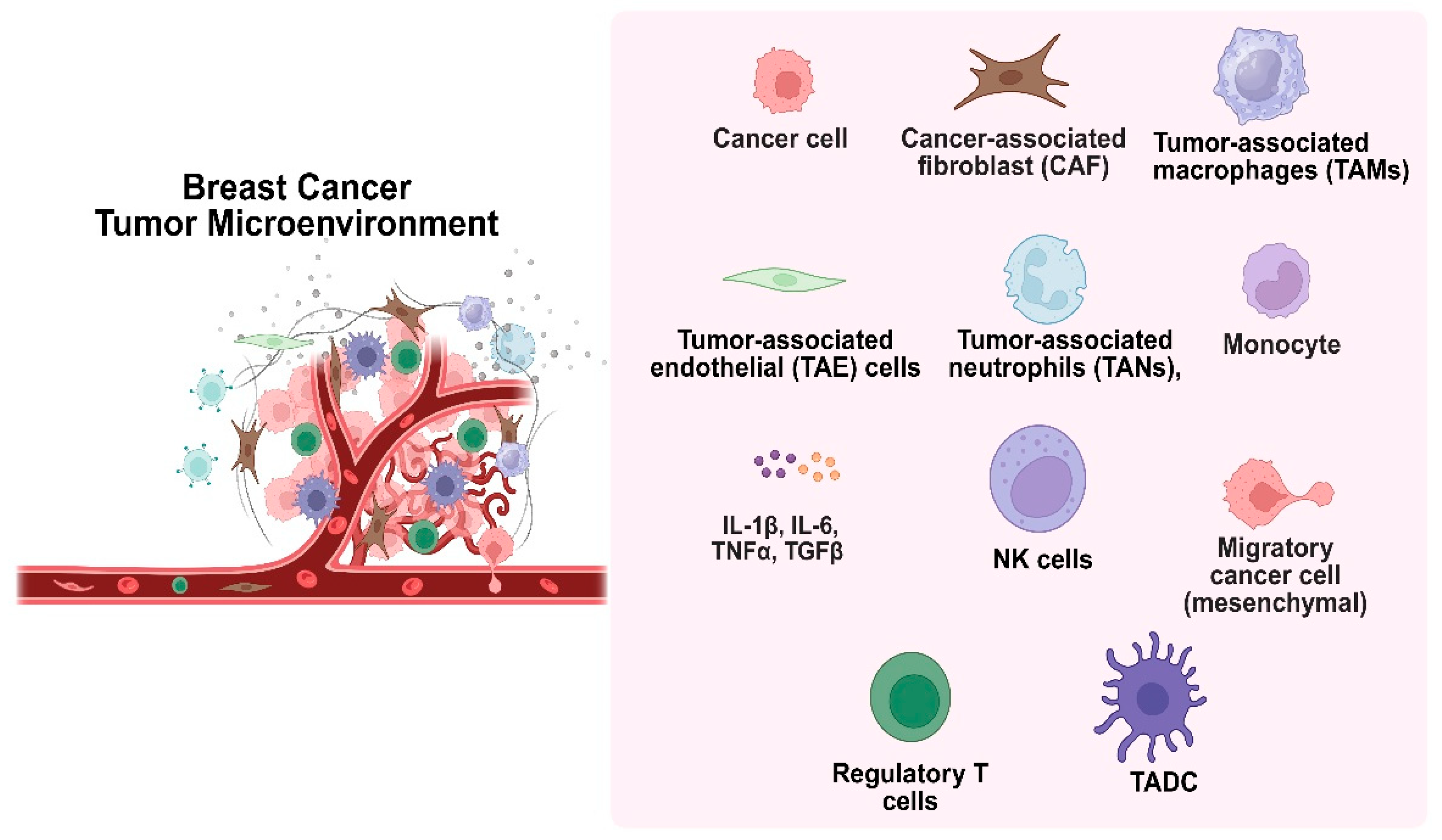
2.2. Tumor Microenvironment
3. Conventional Therapy for Breast Cancer
| Drugs | Mode of Action | Limitations | Ref. |
|---|---|---|---|
| Cyclophosphamide (prodrug) | Active components Acrolein and Phosphoramide mustard (DNA alkylating agent) damage DNA by crosslinking. | Stimulate the immune system | [37] |
| Methotrexate (antimetabolite) | Stops tetrahydrofolate (THF) synthesis, inhibiting dihydrofolate reductase. Therefore, it stops DNA replication and protein synthesis. | Poor aqueous solubility & hepatotoxicity | [38] |
| Thiotepa (antineoplastic) | Alkylating (Guanine) agent involved in depurination and crosslinking DNA | Skin toxicity & myelosuppression | [39] |
| 5-fluorouracil (5-FU) (antimetabolite/analog of uracil) | Interfere with thymidylate synthase & misincorporate metabolites in DNA & RNA. | Myelosuppression & mucositis | [40] |
| Capecitabine (prodrug/neoadjuvant) | Converted to 5-FU at the tumor site. | Gastrointestinal adverse event | [41] |
| Vinorelbine (vinca-alkaloid) | Inhibits tubulin polymerization & binds to mitotic microtubules, blocks mitosis at the G2-M phase | Granulocytopenia, thrombocytopenia, neurotoxicity | [42] |
| Doxorubicin (anthracycline) | Intercalates to DNA, inhibits topoisomerase II, generates ROS, damages DNA | Lower blood cell count, cardiotoxicity, healthy tissue ulceration | [43] |
| Docetaxel (antineoplastic) | Disorganize microtubular network, antimitotic | Febrile neutropenia, enterocolitis, bronchospasm | [44] |
| Paclitaxel (taxane) | Microtubule depolymerization, mitotic arrest | Myelosuppression, peripheral neuropathy | [45] |
| Lapatinib | Target the tyrosine-kinase domain of human epidermal growth factor receptor-2 (HER2), subdue phosphorylation, MAPK signaling, and Akt/mTOR pathways. | Skin lesions, hepatic toxicity | [46] |
| Trastuzumab (monoclonal antibody or mAb) | Binds with high affinity to HER2, induces cytostatic effects related to G1 arrest, reduces cell proliferation, and controls the effects of various pro-angiogenic and anti-angiogenic factors | Cardiotoxicity | [47] |
| Margetuximab (2nd Gen, Fc-engineered mAb) | Binds to Fab epitopes of HER2, shows Fc-independent antiproliferation, and increased binding affinity to CD16A. | Hematologic toxicity | [48] |
| Atezolizumab (FcγR-optimized mAb) | Interferes with binding of PD-L1 to PD-1 receptor, immunosuppressive signal reduction, and enhances T-cell-driven immunity. | Cardiovascular toxicity | [49] |
| Abemaciclib (LY2835219) | Selectively inhibit CDK4/cyclin D1 complex with IC50 2 nM/L & CDK6/cyclin D1 with IC50 10 nM/L | Neutropenia, fatigue, and diarrhea. | [50] |
| Alpelisib (BYL719) | PI3K inhibitor, specifically PI3Kα (catalytic p110α subunit) | Hyperglycemia, diarrhea, blurred vision, bladder pain, and frequent urination | [51] |
| Palbociclib | Inhibit CDK4 & CDK6 along with serine-threonine kinase. | Neutropenia, anemia, fatigue | [52] |
| Tucatinib | Involves HER2 targeting and inhibiting tyrosine kinase | Fatigue, diarrhea, and an increase in the level of ALT & AST | [53] |
| Pertuzumab (Humanized mAb) | Binds to the dimerized domain of HER2 and inhibits heterodimerization | Neutropenia, diarrhea | [54] |
| Tamoxifen (nonsteroidal antiestrogen) | Selective ER modulator, useful in ER-positive breast cancer | Vaginal dryness, Hot flashes | [55] |
3.1. Nanomedicine in Breast Cancer
3.2. Potential Nanocarriers in Breast Cancer Therapy
3.3. Passive Diffusion
3.4. Active Targeting
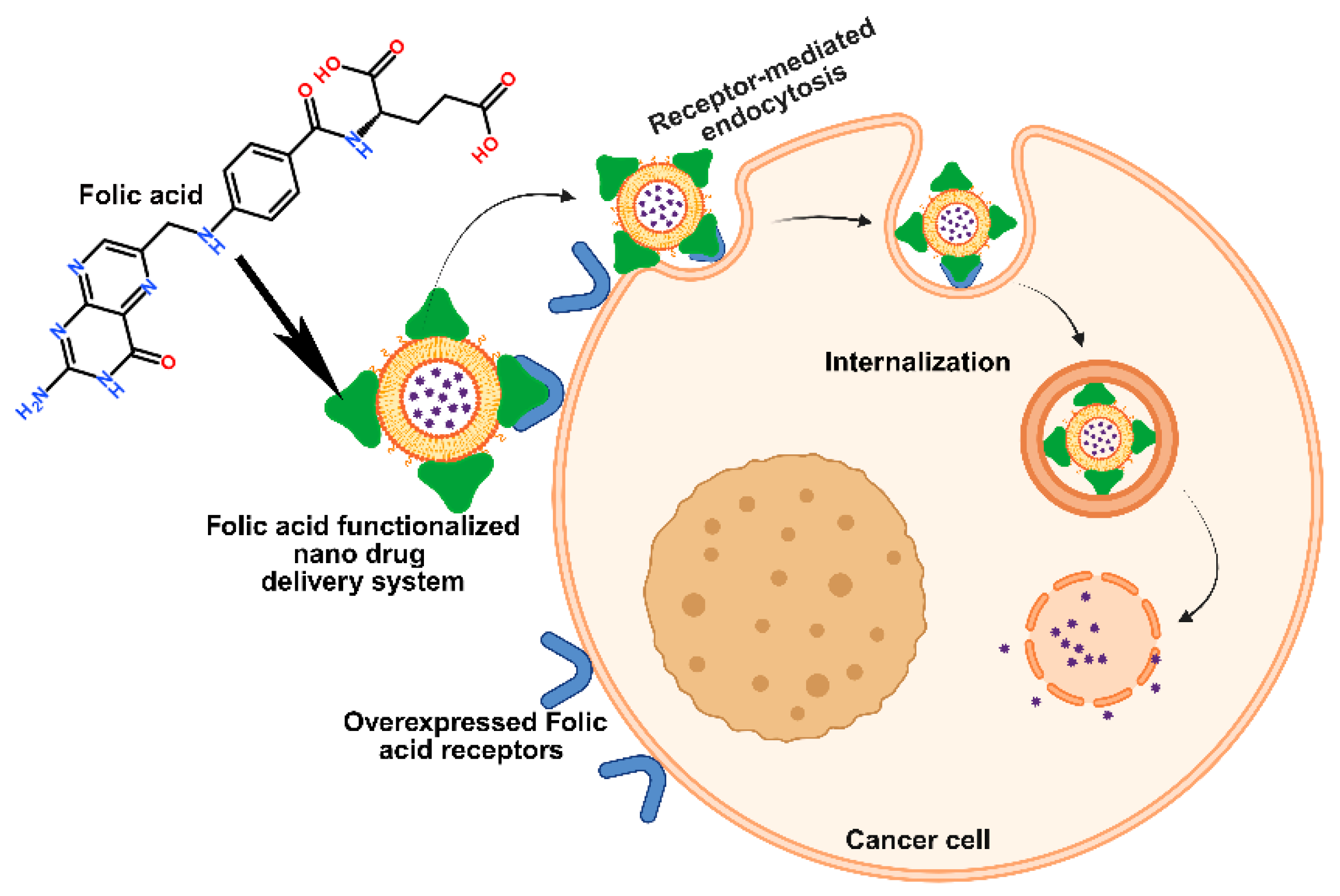
4. Folic Acid-Driven Targeting
4.1. Methods of FA Linking on Nanocarriers
4.2. Folate-Mediated Breast Cancer Cell Targeting
4.3. Folic Acid-Conjugated Nanostructures for Therapeutic Benefit
4.4. Folate-Targeted Nanoparticles for Diagnostic Applications
4.5. Folate Receptor-Targeted Immune Therapy
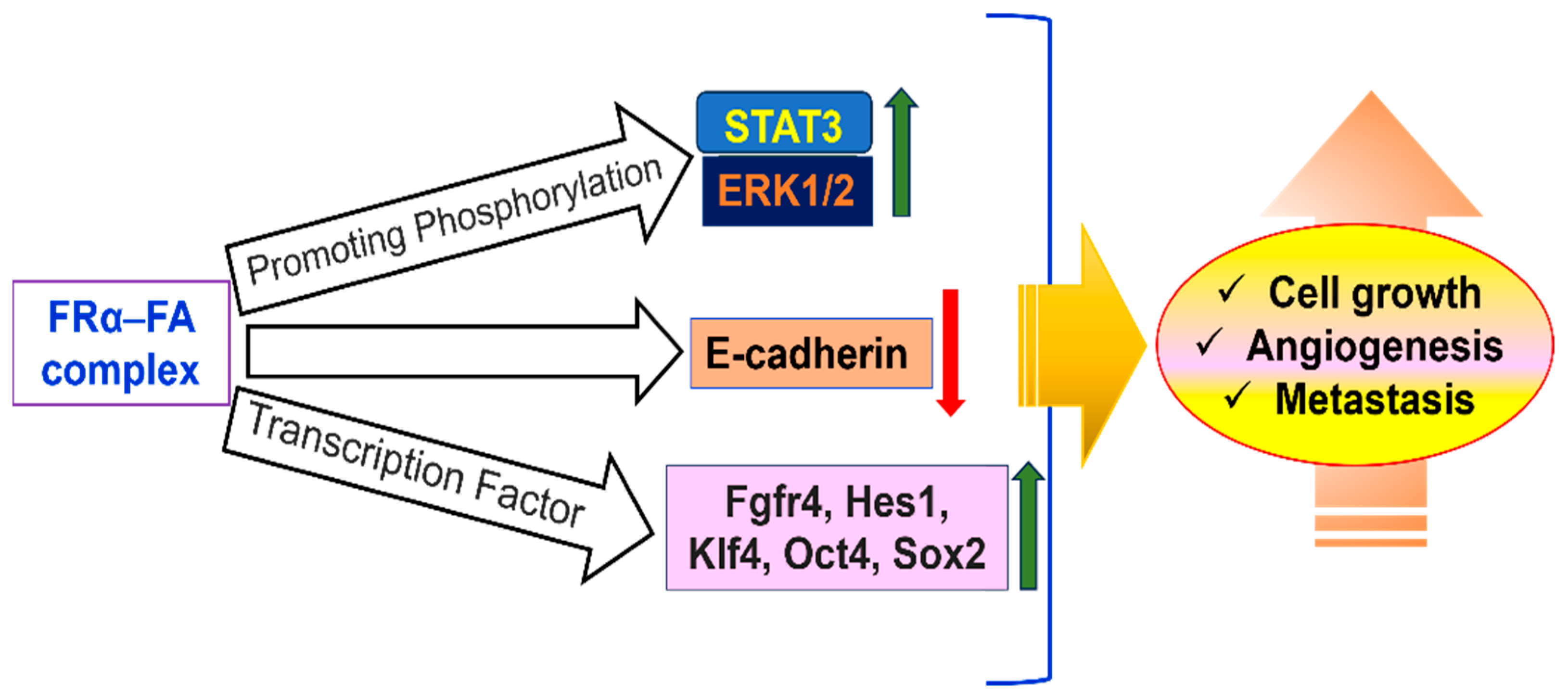
4.6. Folate-Mediated Signaling Pathways
4.7. Folate-Targeted Radioimmunotherapy
4.8. Challenges to Patient Safety
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef]
- Xiong, X.; Zheng, L.-W.; Ding, Y.; Chen, Y.-F.; Cai, Y.-W.; Wang, L.-P.; Huang, L.; Liu, C.-C.; Shao, Z.-M.; Yu, K.-D. Breast cancer: Pathogenesis and treatments. Signal Transduct. Target. Ther. 2025, 10, 49. [Google Scholar] [CrossRef] [PubMed]
- Orshiso, T.A.; Zereffa, E.A.; Murthy, H.C.A.; Demissie, T.B.; Pardeshi, O.; Avhad, L.S.; Ghotekar, S. Biosynthesis of Artemisia abyssinica Leaf Extract-Mediated Bimetallic ZnO–CuO Nanoparticles: Antioxidant, Anticancer, and Molecular Docking Studies. ACS Omega 2023, 8, 41039–41053. [Google Scholar] [CrossRef]
- Raman, L.S.; Shanmuganathan, A.; Chandrashekar, S.; Kaliyaperumal, P.; Perumal, E.; Mudiganti, R.K.R.; Nachammai, K.T.; Kulanthaivel, L.; Subbaraj, G.K.; Chandrasekaran, K.; et al. Antioxidant, Anti-Inflammatory, and Anticarcinogenic Efficacy of an Ayurvedic Formulation: Amritotharanam Kashyam. Adv. Pharmacol. Pharm. Sci. 2023, 2023, 3387261. [Google Scholar] [CrossRef]
- Kulothungan, V.; Ramamoorthy, T.; Sathishkumar, K.; Mohan, R.; Tomy, N.; Miller, G.J.; Mathur, P. Burden of female breast cancer in India: Estimates of YLDs, YLLs, and DALYs at national and subnational levels based on the national cancer registry programme. Breast Cancer Res. Treat. 2024, 205, 323–332. [Google Scholar] [CrossRef]
- Vemula, S.; Dhakshanamoorthy, K. Epidemiology of Cancer Incidence Estimates and Statistics 2000–2025: Analysis from National Cancer Registry Programme in India. Indian J. Med. Paediatr. Oncol. 2025, 46, 278–287. [Google Scholar] [CrossRef]
- Fitzmaurice, C.; Abate, D.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdel-Rahman, O.; Abdelalim, A.; Abdoli, A.; Abdollahpour, I.; Abdulle, A.S.M.; et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2019, 5, 1749–1768. [Google Scholar] [CrossRef]
- Prabakaran, L.; Sathyaraj, W.V.; Yesudhason, B.V.; Subbaraj, G.K.; Atchudan, R. Green Synthesis of Multifunctional Silver Nanoparticles Using Plectranthus amboinicus for Sensitive Detection of Triethylamine, with Potential In Vitro Antibacterial and Anticancer Activities. Chemosensors 2023, 11, 373. [Google Scholar] [CrossRef]
- Zhang, B.; Li, J.; Yu, W. Integration of CRISPR/dCas9-Based methylation editing with guide positioning sequencing identifies dynamic changes of mrDEGs in breast cancer progression. Cell. Mol. Life Sci. 2025, 82, 46. [Google Scholar] [CrossRef]
- Swietach, P.; Boedtkjer, E.; Pedersen, S.F. How protons pave the way to aggressive cancers. Nat. Rev. Cancer 2023, 23, 825–841. [Google Scholar] [CrossRef]
- Capik, O.; Karatas, O.F. Pathways and outputs orchestrated in tumor microenvironment cells by hypoxia-induced tumor-derived exosomes in pan-cancer. Cell. Oncol. 2025, 48, 539–557. [Google Scholar] [CrossRef] [PubMed]
- Thirumalai, A.; Girigoswami, K.; Pallavi, P.; Harini, K.; Gowtham, P.; Girigoswami, A. Cancer therapy with iRGD as a tumor-penetrating peptide. Bull. Cancer 2023, 110, 1288–1300. [Google Scholar] [CrossRef] [PubMed]
- Thirumalai, A.; Girigoswami, K.; Harini, K.; Kiran, V.; Durgadevi, P.; Girigoswami, A. Natural Polymer Derivative-based pH responsive Nanoformulations Entrapped Diketo-tautomers of 5-fluorouracil for Enhanced Cancer Therapy. ADMET DMPK 2025, 13, 2554. [Google Scholar] [CrossRef]
- Chatterjee, S.; Harini, K.; Girigoswami, A.; Nag, M.; Lahiri, D.; Girigoswami, K. Nanodecoys: A Quintessential Candidate to Augment Theranostic Applications for a Plethora of Diseases. Pharmaceutics 2022, 15, 73. [Google Scholar] [CrossRef]
- Mercy, D.J.; Harini, K.; Madhumitha, S.; Anitha, C.; Iswariya, J.; Girigoswami, K.; Girigoswami, A. pH-responsive polymeric nanostructures for cancer theranostics. J. Met. Mater. Miner. 2023, 33, 1–15. [Google Scholar] [CrossRef]
- Zwicke, G.L.; Ali Mansoori, G.; Jeffery, C.J. Utilizing the folate receptor for active targeting of cancer nanotherapeutics. Nano Rev. 2012, 3, 18496. [Google Scholar] [CrossRef]
- Park, M.; Kim, D.; Ko, S.; Kim, A.; Mo, K.; Yoon, H. Breast cancer metastasis: Mechanisms and therapeutic implications. Int. J. Mol. Sci. 2022, 23, 6806. [Google Scholar] [CrossRef]
- Nolan, E.; Lindeman, G.J.; Visvader, J.E. Deciphering breast cancer: From biology to the clinic. Cell 2023, 186, 1708–1728. [Google Scholar] [CrossRef]
- Grimm, L.J.; Rahbar, H.; Abdelmalak, M.; Hall, A.H.; Ryser, M.D. Ductal carcinoma in situ: State-of-the-art review. Radiology 2022, 302, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Zagami, P.; Carey, L.A. Triple negative breast cancer: Pitfalls and progress. npj Breast Cancer 2022, 8, 95. [Google Scholar] [CrossRef]
- Moelans, C.B.; de Weger, R.A.; Van der Wall, E.; van Diest, P.J. Current technologies for HER2 testing in breast cancer. Crit. Rev. Oncol./Hematol. 2011, 80, 380–392. [Google Scholar] [CrossRef]
- Bagaria, S.P.; Ray, P.S.; Sim, M.-S.; Ye, X.; Shamonki, J.M.; Cui, X.; Giuliano, A.E. Personalizing breast cancer staging by the inclusion of ER, PR, and HER2. JAMA Surg. 2014, 149, 125–129. [Google Scholar] [CrossRef]
- Bombonati, A.; Sgroi, D.C. The molecular pathology of breast cancer progression. J. Pathol. 2011, 223, 308–318. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Karnoub, A.E. Endocrine regulation of cancer stem cell compartments in breast tumors. Mol. Cell. Endocrinol. 2021, 535, 111374. [Google Scholar] [CrossRef]
- Lim, E.; Vaillant, F.; Wu, D.; Forrest, N.C.; Pal, B.; Hart, A.H.; Asselin-Labat, M.-L.; Gyorki, D.E.; Ward, T.; Partanen, A.; et al. Aberrant luminal progenitors as the candidate target population for basal tumor development in BRCA1 mutation carriers. Nat. Med. 2009, 15, 907–913. [Google Scholar] [CrossRef] [PubMed]
- van Neerven, S.M.; Tieken, M.; Vermeulen, L.; Bijlsma, M.F. Bidirectional interconversion of stem and non-stem cancer cell populations: A reassessment of theoretical models for tumor heterogeneity. Mol. Cell. Oncol. 2016, 3, e1098791. [Google Scholar] [CrossRef]
- Lüönd, F.; Tiede, S.; Christofori, G. Breast cancer as an example of tumour heterogeneity and tumour cell plasticity during malignant progression. Br. J. Cancer 2021, 125, 164–175. [Google Scholar] [CrossRef]
- Shahrouzi, P.; Forouz, F.; Mathelier, A.; Kristensen, V.N.; Duijf, P.H. Copy number alterations: A catastrophic orchestration of the breast cancer genome. Trends Mol. Med. 2024, 30, 750–764. [Google Scholar] [CrossRef]
- Pös, O.; Radvanszky, J.; Buglyó, G.; Pös, Z.; Rusnakova, D.; Nagy, B.; Szemes, T. DNA copy number variation: Main characteristics, evolutionary significance, and pathological aspects. Biomed. J. 2021, 44, 548. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Im, S.-A.; Park, K.; Wen, J.; Lee, K.-H.; Choi, Y.-L.; Lee, W.-C.; Min, A.; Bonato, V.; Park, S.; et al. Longitudinal multi-omics study of palbociclib resistance in HR-positive/HER2-negative metastatic breast cancer. Genome Med. 2023, 15, 55. [Google Scholar] [CrossRef] [PubMed]
- Watson, E.V.; Lee, J.J.-K.; Gulhan, D.C.; Melloni, G.E.M.; Venev, S.V.; Magesh, R.Y.; Frederick, A.; Chiba, K.; Wooten, E.C.; Naxerova, K.; et al. Chromosome evolution screens recapitulate tissue-specific tumor aneuploidy patterns. Nat. Genet. 2024, 56, 900–912. [Google Scholar] [CrossRef]
- Hajizadeh, F.; Aghebati Maleki, L.; Alexander, M.; Mikhailova, M.V.; Masjedi, A.; Ahmadpour, M.; Hashemi, V.; Jadidi-Niaragh, F. Tumor-associated neutrophils as new players in immunosuppressive process of the tumor microenvironment in breast cancer. Life Sci. 2021, 264, 118699. [Google Scholar] [CrossRef] [PubMed]
- Janssen, J.B.E.; Medema, J.P.; Gootjes, E.C.; Tauriello, D.V.F.; Verheul, H.M.W. Mutant RAS and the tumor microenvironment as dual therapeutic targets for advanced colorectal cancer. Cancer Treat. Rev. 2022, 109, 102433. [Google Scholar] [CrossRef]
- Yu, J.; Mu, Q.; Fung, M.; Xu, X.; Zhu, L.; Ho, R.J.Y. Challenges and opportunities in metastatic breast cancer treatments: Nano-drug combinations delivered preferentially to metastatic cells may enhance therapeutic response. Pharmacol. Ther. 2022, 236, 108108. [Google Scholar] [CrossRef] [PubMed]
- Sohail, M.; Sun, Z.; Li, Y.; Gu, X.; Xu, H. Research progress in strategies to improve the efficacy and safety of doxorubicin for cancer chemotherapy. Expert Rev. Anticancer Ther. 2021, 21, 1385–1398. [Google Scholar] [CrossRef] [PubMed]
- Girigoswami, K.; Pallavi, P.; Girigoswami, A. Intricate subcellular journey of nanoparticles to the enigmatic domains of endoplasmic reticulum. Drug Deliv. 2023, 30, 2284684. [Google Scholar] [CrossRef]
- Lai, Y.-G.; Liao, H.-T.; Chen, Y.-H.; Huang, S.-W.; Liou, Y.-H.; Wu, Z.-Q.; Liao, N.-S. cGAS and STING in Host Myeloid Cells Are Essential for Effective Cyclophosphamide Treatment of Advanced Breast Cancer. Cancers 2025, 17, 1130. [Google Scholar] [CrossRef]
- Abdullah, S.; Altwaijry, N.; Alnakhli, M.; ALenezi, G.; Al-Masud, A.A.; Henidi, H.; Jamous, Y.F. Novel methotrexate long-acting system using ambroxol coating and hydroxypropyl methylcellulose encapsulation for preferential and enhanced lung cancer efficiency. PLoS ONE 2025, 20, e0314941. [Google Scholar] [CrossRef]
- Torabifard, H.; Fattahi, A. Mechanisms and kinetics of thiotepa and tepa hydrolysis: DFT study. J. Mol. Model. 2012, 18, 3563–3576. [Google Scholar] [CrossRef]
- Zhong, C.; Wang, S.; Jiang, W.-J.; Li, Z.; Wang, X.; Fan, S.; Huang, J.; Wu, H.-J.; Sheng, R.; Fei, T. Chemoresistance mechanisms to 5-Fluorouracil and reversal strategies in lung and breast cancer. Sci. Rep. 2025, 15, 6074. [Google Scholar] [CrossRef]
- Masuda, N.; Lee, S.-J.; Ohtani, S.; Im, Y.-H.; Lee, E.-S.; Yokota, I.; Kuroi, K.; Im, S.-A.; Park, B.-W.; Kim, S.-B. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N. Engl. J. Med. 2017, 376, 2147–2159. [Google Scholar] [CrossRef]
- Aapro, M.; Finek, J. Oral vinorelbine in metastatic breast cancer: A review of current clinical trial results. Cancer Treat. Rev. 2012, 38, 120–126. [Google Scholar] [CrossRef]
- Bisht, A.; Avinash, D.; Sahu, K.K.; Patel, P.; Das Gupta, G.; Kurmi, B.D. A comprehensive review on doxorubicin: Mechanisms, toxicity, clinical trials, combination therapies and nanoformulations in breast cancer. Drug Deliv. Transl. Res. 2025, 15, 102–133. [Google Scholar] [CrossRef]
- Stoicescu, E.A.; Burcea, M.; Iancu, R.C.; Zivari, M.; Popa Cherecheanu, A.; Bujor, I.A.; Rastoaca, C.; Iancu, G. Docetaxel for breast cancer treatment-side effects on ocular surface, a systematic review. Processes 2021, 9, 1086. [Google Scholar] [CrossRef]
- Urbaniak, A.; Piña-Oviedo, S.; Yuan, Y.; Huczyński, A.; Chambers, T.C. Limitations of an ex vivo breast cancer model for studying the mechanism of action of the anticancer drug paclitaxel. Eur. J. Pharmacol. 2021, 891, 173780. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Valencia, J.; García-Villarreal, R.; Rodríguez-Jiménez, M.; Hernández-Avalos, A.D.; Rivero, I.A.; Vique-Sánchez, J.L.; Chimal-Vega, B.; Pulido-Capiz, A.; García-González, V. Lapatinib-Resistant HER2+ Breast Cancer Cells Are Associated with Dysregulation of MAPK and p70S6K/PDCD4 Pathways and Calcium Management, Influence of Cryptotanshinone. Int. J. Mol. Sci. 2025, 26, 3763. [Google Scholar] [CrossRef] [PubMed]
- Fiszman, G.L.; Jasnis, M.A. Molecular mechanisms of trastuzumab resistance in HER2 overexpressing breast cancer. Int. J. Breast Cancer 2011, 2011, 352182. [Google Scholar] [CrossRef]
- Alasmari, M.M. A review of margetuximab-based therapies in patients with HER2-positive metastatic breast cancer. Cancers 2022, 15, 38. [Google Scholar] [CrossRef]
- Inman, B.A.; Longo, T.A.; Ramalingam, S.; Harrison, M.R. Atezolizumab: A PD-L1–blocking antibody for bladder cancer. Clin. Cancer Res. 2017, 23, 1886–1890. [Google Scholar] [CrossRef]
- Corona, S.P.; Generali, D. Abemaciclib: A CDK4/6 inhibitor for the treatment of HR+/HER2− advanced breast cancer. Drug Des. Dev. Ther. 2018, 12, 321–330. [Google Scholar] [CrossRef]
- André, F.; Ciruelos, E.; Rubovszky, G.; Campone, M.; Loibl, S.; Rugo, H.S.; Iwata, H.; Conte, P.; Mayer, I.A.; Kaufman, B. Alpelisib for PIK3CA-mutated, hormone receptor–positive advanced breast cancer. N. Engl. J. Med. 2019, 380, 1929–1940. [Google Scholar] [CrossRef]
- Serra, F.; Lapidari, P.; Quaquarini, E.; Tagliaferri, B.; Sottotetti, F.; Palumbo, R. Palbociclib in metastatic breast cancer: Current evidence and real-life data. Drugs Context 2019, 8, 212579. [Google Scholar] [CrossRef]
- Chaurasia, M.; Singh, R.; Sur, S.; Flora, S. A review of FDA approved drugs and their formulations for the treatment of breast cancer. Front. Pharmacol. 2023, 14, 1184472. [Google Scholar] [CrossRef] [PubMed]
- Von Minckwitz, G.; Procter, M.; De Azambuja, E.; Zardavas, D.; Benyunes, M.; Viale, G.; Suter, T.; Arahmani, A.; Rouchet, N.; Clark, E. Adjuvant pertuzumab and trastuzumab in early HER2-positive breast cancer. N. Engl. J. Med. 2017, 377, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Srivastava, A.; Pateriya, A.; Tomar, M.S.; Mishra, A.K.; Shrivastava, A. Metabolic reprograming confers tamoxifen resistance in breast cancer. Chem.-Biol. Interact. 2021, 347, 109602. [Google Scholar] [CrossRef]
- Nag, S.; Mitra, O.; Tripathi, G.; Adur, I.; Mohanto, S.; Nama, M.; Samanta, S.; Gowda, B.H.J.; Subramaniyan, V.; Sundararajan, V.; et al. Nanomaterials-assisted photothermal therapy for breast cancer: State-of-the-art advances and future perspectives. Photodiagn. Photodyn. Ther. 2024, 45, 103959. [Google Scholar] [CrossRef]
- Chandrakala, V.; Aruna, V.; Angajala, G. Review on metal nanoparticles as nanocarriers: Current challenges and perspectives in drug delivery systems. Emergent Mater. 2022, 5, 1593–1615. [Google Scholar] [CrossRef]
- Iqbal, S.; Zaman, M.; Waqar, M.A.; Sarwar, H.S.; Jamshaid, M. Vesicular approach of cubosomes, its components, preparation techniques, evaluation and their appraisal for targeting cancer cells. J. Liposome Res. 2024, 34, 368–384. [Google Scholar] [CrossRef]
- Mughees, M.; Kumar, K.; Wajid, S. Exosome vesicle as a nano-therapeutic carrier for breast cancer. J. Drug Target. 2021, 29, 121–130. [Google Scholar] [CrossRef]
- Saadh, M.J.; Saeed, T.N.; Alfarttoosi, K.H.; Sanghvi, G.; Roopashree, R.; Thakur, V.; Lakshmi, L.; Aminov, Z.; Taher, W.M.; Alwan, M.; et al. Plasmonic Nanoparticles: Enhancing Early Breast Cancer Detection Through Biosensors. Plasmonics 2025, 20, 8067–8084. [Google Scholar] [CrossRef]
- Patitsa, M.; Karathanou, K.; Kanaki, Z.; Tzioga, L.; Pippa, N.; Demetzos, C.; Verganelakis, D.A.; Cournia, Z.; Klinakis, A. Magnetic nanoparticles coated with polyarabic acid demonstrate enhanced drug delivery and imaging properties for cancer theranostic applications. Sci. Rep. 2017, 7, 775. [Google Scholar] [CrossRef]
- Mousavi-Kiasary, S.M.S.; Senabreh, A.; Zandi, A.; Pena, R.; Cruz, F.; Adibi, A.; Hooshmand, N. Synergistic Cancer Therapies Enhanced by Nanoparticles: Advancing Nanomedicine Through Multimodal Strategies. Pharmaceutics 2025, 17, 682. [Google Scholar] [CrossRef]
- Ebrahimi, N.; Manavi, M.S.; Nazari, A.; Momayezi, A.; Faghihkhorasani, F.; Rasool Riyadh Abdulwahid, A.-H.; Rezaei-Tazangi, F.; Kavei, M.; Rezaei, R.; Mobarak, H.; et al. Nano-scale delivery systems for siRNA delivery in cancer therapy: New era of gene therapy empowered by nanotechnology. Environ. Res. 2023, 239, 117263. [Google Scholar] [CrossRef]
- Damiana, T.S.T.; Dalm, S.U. Combination Therapy, a Promising Approach to Enhance the Efficacy of Radionuclide and Targeted Radionuclide Therapy of Prostate and Breast Cancer. Pharmaceutics 2021, 13, 674. [Google Scholar] [CrossRef]
- Li, M.; Li, S.; Li, Y.; Li, X.; Yang, G.; Li, M.; Xie, Y.; Su, W.; Wu, J.; Jia, L.; et al. Cationic liposomes co-deliver chemotherapeutics and siRNA for the treatment of breast cancer. Eur. J. Med. Chem. 2022, 233, 114198. [Google Scholar] [CrossRef]
- Yıldırım, M.; Acet, Ö.; Yetkin, D.; Acet, B.Ö.; Karakoc, V.; Odabası, M. Anti-cancer activity of naringenin loaded smart polymeric nanoparticles in breast cancer. J. Drug Deliv. Sci. Technol. 2022, 74, 103552. [Google Scholar] [CrossRef]
- Liu, Y.; Guo, K.; Ding, M.; Zhang, B.; Xiao, N.; Tang, Z.; Wang, Z.; Zhang, C.; Shubhra, Q.T.H. Engineered Magnetic Polymer Nanoparticles Can Ameliorate Breast Cancer Treatment Inducing Pyroptosis–Starvation along with Chemotherapy. ACS Appl. Mater. Interfaces 2022, 14, 42541–42557. [Google Scholar] [CrossRef]
- Khoshnood, A.; Iranpour, S.; Khaksari, S.; Mousavi Shaegh, S.A.; Abnous, K.; Taghdisi, S.M. Liposome/AZIF-8 Janus nanoplatforms: Promising nanocarriers for improving chemotherapeutic outcomes in breast cancer treatment. Int. J. Pharm. 2025, 678, 125702. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Lu, B.; Meng, S.; Xinlei, Y.; Ying, X.; Yu, W.; Yue, G.; Xingyou, L.; Leijie, Y.; Xing, Z.; et al. ROS-Responsive Biomimetic Nanocomplexes of Liposomes and Macrophage-Derived Exosomes for Combination Breast Cancer Therapy. Int. J. Nanomed. 2025, 20, 5161–5180. [Google Scholar] [CrossRef] [PubMed]
- Feith, M.; Das Sajib, S.; Myrann, A.G.; Høgset, A.; Garrido, P.; Martinez, A.; Knutsen, E.; Sandvig, K.; Skotland, T.; Mælandsmo, G.M.; et al. Induction of Cell Death by Combined Treatment with Photosensitizer-Chitosan Nanoparticles and the Ferroptosis Inducer RSL3 in Breast Cancer Cell Lines. Adv. NanoBiomed Res. 2025, 5, 2400208. [Google Scholar] [CrossRef]
- Wu, Z.; Tang, Y.; Liu, Y.; Chen, Z.; Feng, Y.; Hu, H.; Liu, H.; Chen, G.; Lu, Y.; Hu, Y.; et al. Co-delivery of fucoxanthin and Twist siRNA using hydroxyethyl starch-cholesterol self-assembled polymer nanoparticles for triple-negative breast cancer synergistic therapy. J. Adv. Res. 2025, 70, 463–479. [Google Scholar] [CrossRef]
- Chen, H.; Qu, H.; Pan, Y.; Cheng, W.; Xue, X. Manganese-coordinated nanoparticle with high drug-loading capacity and synergistic photo-/immuno-therapy for cancer treatments. Biomaterials 2025, 312, 122745. [Google Scholar] [CrossRef]
- Yan, W.; Wang, S.; Zhu, L.; Yu, X.; Li, J. Targeted editing of CCL5 with CRISPR-Cas9 nanoparticles enhances breast cancer immunotherapy. Apoptosis 2025, 30, 912–935. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Yang, X.; Qu, Z.; Ding, P.; Kong, X.; Wang, X.; Liu, Q.; Zhang, X.; Lu, Y.; Wang, J.; et al. DNA tetrahedral nanoparticles: Co-delivery of siOTUD6B/DOX against triple-negative breast cancer. J. Control. Release 2025, 377, 197–211. [Google Scholar] [CrossRef] [PubMed]
- Are, V.; Das, S.; P S, S.; Biswas, S. Combination therapy of Lapatinib/Letrozole-based protein-vitamin nanoparticles to enhance the therapeutic effectiveness in drug-resistant breast cancer. Colloids Surf. B Biointerfaces 2025, 247, 114399. [Google Scholar] [CrossRef]
- Lunawat, A.K.; Mukherjee, D.; Shivgotra, R.; Raikwar, S.; Awasthi, A.; Singh, A.; Singh, S.; Chandel, S.; Jain, S.K.; Thakur, S. Carboplatin Co-loaded 5-Fluorouracil Nanoparticles Conjugated with Trastuzumab for Targeted Therapy in HER2+ Heterogeneity Breast Cancer. AAPS PharmSciTech 2025, 26, 114. [Google Scholar] [CrossRef] [PubMed]
- Arya, D.K.; Prashant, P.; Anit, K.; Kumarappan, C.; Al, F.A.; Giriraj, P.; Saurabh, S.; Rajinikanth, P.S. Dual-ligand functionalized liposomes with iRGD/trastuzumab co-loaded with gefitinib and lycorine for enhanced metastatic breast cancer therapy. J. Liposome Res. 2025, 35, 173–187. [Google Scholar] [CrossRef]
- Tavakoli, M.; Maghsoudian, S.; Rezaei-Aderiani, A.; Hajiramezanali, M.; Fatahi, Y.; Amani, M.; Sharifikolouei, E.; Ghahremani, M.H.; Raoufi, M.; Motasadizadeh, H.; et al. Synergistic effects of paclitaxel and platelet-superparamagnetic iron oxide nanoparticles for targeted chemo-hyperthermia therapy against breast cancer. Colloids Surf. B Biointerfaces 2025, 251, 114584. [Google Scholar] [CrossRef]
- Ferreira, V.R.; Ventura, A.; Cândido, M.; Ferreira-Strixino, J.; Raniero, L. Curcumin-coated iron oxide nanoparticles for photodynamic therapy of breast cancer. Photochem. Photobiol. Sci. 2025, 24, 181–190. [Google Scholar] [CrossRef]
- Medina-Moreno, A.; El-Hammadi, M.M.; Martínez-Soler, G.I.; Ramos, J.G.; García-García, G.; Arias, J.L. Magnetic and pH-responsive magnetite/chitosan (core/shell) nanoparticles for dual-targeted methotrexate delivery in cancer therapy. Drug Deliv. Transl. Res. 2025, 15, 1646–1659. [Google Scholar] [CrossRef]
- Danhier, F.; Feron, O.; Préat, V. To exploit the tumor microenvironment: Passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J. Control. Release 2010, 148, 135–146. [Google Scholar] [CrossRef]
- Liu, C.; Li, M.; Sun, J.; Li, P.; Bai, Y.; Zhang, J.; Qian, Y.; Shi, M.; He, J.; Huo, H.; et al. Cation-π Interaction-Mediated Tumour Drug Delivery for Deep Intratumoral Penetration and Treatment. Adv. Funct. Mater. 2022, 32, 2205043. [Google Scholar] [CrossRef]
- Fang, J.; Islam, R.; Islam, W.; Yin, H.; Subr, V.; Etrych, T.; Ulbrich, K.; Maeda, H. Augmentation of EPR Effect and Efficacy of Anticancer Nanomedicine by Carbon Monoxide Generating Agents. Pharmaceutics 2019, 11, 343. [Google Scholar] [CrossRef]
- Huang, Y.; Yu, M.; Zheng, J. Charge barriers in the kidney elimination of engineered nanoparticles. Proc. Natl. Acad. Sci. USA 2024, 121, e2403131121. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Yuan, L.; Chou, W.-C.; Cheng, Y.-H.; He, C.; Monteiro-Riviere, N.A.; Riviere, J.E.; Lin, Z. Meta-Analysis of Nanoparticle Distribution in Tumors and Major Organs in Tumor-Bearing Mice. ACS Nano 2023, 17, 19810–19831. [Google Scholar] [CrossRef]
- Maeda, H.; Wu, J.; Sawa, T.; Matsumura, Y.; Hori, K. Tumor vascular permeability and the EPR effect in macromolecular therapeutics: A review. J. Control. Release 2000, 65, 271–284. [Google Scholar] [CrossRef] [PubMed]
- Stylianopoulos, T.; Jain, R.K. Design considerations for nanotherapeutics in oncology. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 1893–1907. [Google Scholar] [CrossRef]
- Ghosh, R.; Kumar, M.; Kumar, S.; Komal, K.; Sharma, R.; Kurmi, B.D. Small molecule therapeutics for receptor-mediated targeting through liposomes in breast cancer treatment: A comprehensive review. Bioorg. Chem. 2025, 160, 108442. [Google Scholar] [CrossRef]
- Sun, X.; Liu, K.; Lu, S.; He, W.; Du, Z. Targeted Therapy and Immunotherapy for Heterogeneous Breast Cancer. Cancers 2022, 14, 5456. [Google Scholar] [CrossRef]
- Zheng, H.; Siddharth, S.; Parida, S.; Wu, X.; Sharma, D. Tumor Microenvironment: Key Players in Triple Negative Breast Cancer Immunomodulation. Cancers 2021, 13, 3357. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.-M.; Paulishak, W.; Oladejo, M.; Wood, L. Dynamic tumor microenvironment, molecular heterogeneity, and distinct immunologic portrait of triple-negative breast cancer: An impact on classification and treatment approaches. Breast Cancer 2023, 30, 167–186. [Google Scholar] [CrossRef] [PubMed]
- Normanno, N.; De Luca, A.; Bianco, C.; Strizzi, L.; Mancino, M.; Maiello, M.R.; Carotenuto, A.; De Feo, G.; Caponigro, F.; Salomon, D.S. Epidermal growth factor receptor (EGFR) signaling in cancer. Gene 2006, 366, 2–16. [Google Scholar] [CrossRef] [PubMed]
- Wan, G.; Chen, X.; Gou, R.; Guan, C.; Chen, J.; Wang, Q.; Wu, W.; Chen, H.; Zhang, Q.; Wang, H. Platelet membrane-based biochemotactic-targeting nanoplatform combining PDT with EGFR inhibition therapy for the treatment of breast cancer. Biomater. Sci. 2024, 12, 691–709. [Google Scholar] [CrossRef]
- Carmeliet, P.; Jain, R. Angiogenesis in cancer and other diseases. Nature 2000, 407, 249–257. [Google Scholar] [CrossRef]
- Hicklin, D.J.; Ellis, L.M. Role of the Vascular Endothelial Growth Factor Pathway in Tumor Growth and Angiogenesis. J. Clin. Oncol. 2005, 23, 1011–1027. [Google Scholar] [CrossRef]
- Sen, P.; Ghosh, S.S. Targeting Cross-Talks of Notch and VEGF to Tweak the EMT and EPT Dynamics in Triple Negative Breast Cancer Cells. Adv. Ther. 2024, 7, 2400059. [Google Scholar] [CrossRef]
- Sun, L.; Liu, H.; Ye, Y.; Lei, Y.; Islam, R.; Tan, S.; Tong, R.; Miao, Y.-B.; Cai, L. Smart nanoparticles for cancer therapy. Signal Transduct. Target. Ther. 2023, 8, 418. [Google Scholar] [CrossRef]
- Saharkhiz, S.; Nasri, N.; Naderi, N.; Dini, G.; Ghalehshahi, S.S.; Firoozbakht, F. Evaluating a targeted Palbociclib-Trastuzumab loaded smart niosome platform for treating HER2 positive breast cancer cells. Int. J. Pharm. X 2024, 7, 100237. [Google Scholar] [CrossRef]
- Yang, C.; Wang, W.; Gao, Y.; Yin, L.; Pan, K.; Chen, D.; Yang, F.; Xing, N. Sonodynamic Therapy by Reactive Oxygen Species Generation-Responsive Pseudo-Semiconducting Polymer Nanoparticles Combined with a Fibroblast Growth Factor Receptor Inhibitor for Enhancing Immunotherapy in Bladder Cancer. ACS Appl. Mater. Interfaces 2025, 17, 9125–9139. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Zhao, Z.; Wang, H.; Liu, Y.; Xu, Y.; Zhang, J.; Chen, B.; Li, L.; Zhao, Y. P-Glycoprotein Antibody Decorated Porous Hydrogel Particles for Capture and Release of Drug-Resistant Tumor Cells. Adv. Healthc. Mater. 2019, 8, 1900136. [Google Scholar] [CrossRef]
- Ahmadi, M.; Ritter, C.A.; von Woedtke, T.; Bekeschus, S.; Wende, K. Package delivered: Folate receptor-mediated transporters in cancer therapy and diagnosis. Chem. Sci. 2024, 15, 1966–2006. [Google Scholar] [CrossRef]
- Wibowo, A.S.; Singh, M.; Reeder, K.M.; Carter, J.J.; Kovach, A.R.; Meng, W.; Ratnam, M.; Zhang, F.; Dann, C.E. Structures of human folate receptors reveal biological trafficking states and diversity in folate and antifolate recognition. Proc. Natl. Acad. Sci. USA 2013, 110, 15180–15188. [Google Scholar] [CrossRef]
- Ghosh, T.; Mandal, M.; Shee, M.; Das, T.K.; Mandal, M.; Banerji, P.; Das, N.C. Fabrication of Folic Acid-Derived Carbon Dot-Conjugated Chitosan Nanospheres as Theragnostic Agents for pH-Responsive Anticancer Drug Delivery. ACS Appl. Bio Mater. 2025, 8, 3096–3110. [Google Scholar] [CrossRef]
- Liu, Y.; Xinyi, C.; Theodore, E.; Benjamina, E.; Alicia, C.; Anthony, C.; Karagiannis, S.N. Folate receptor alpha for cancer therapy: An antibody and antibody-drug conjugate target coming of age. mAbs 2025, 17, 2470309. [Google Scholar] [CrossRef] [PubMed]
- Figini, M.; Ferri, R.; Mezzanzanica, D.; Bagnoli, M.; Luison, E.; Miotti, S.; Canevari, S. Reversion of transformed phenotype in ovarian cancer cells by intracellular expression of anti folate receptor antibodies. Gene Ther. 2003, 10, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- Scaranti, M.; Cojocaru, E.; Banerjee, S.; Banerji, U. Exploiting the folate receptor α in oncology. Nat. Rev. Clin. Oncol. 2020, 17, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, R.; Patra, C.R.; Earl, A.; Wang, S.; Katarya, A.; Lu, L.; Kizhakkedathu, J.N.; Yaszemski, M.J.; Greipp, P.R.; Mukhopadhyay, D.; et al. Attaching folic acid on gold nanoparticles using noncovalent interaction via different polyethylene glycol backbones and targeting of cancer cells. Nanomed. Nanotechnol. Biol. Med. 2007, 3, 224–238. [Google Scholar] [CrossRef]
- Ramezani Farani, M.; Azarian, M.; Heydari Sheikh Hossein, H.; Abdolvahabi, Z.; Mohammadi Abgarmi, Z.; Moradi, A.; Mousavi, S.M.; Ashrafizadeh, M.; Makvandi, P.; Saeb, M.R.; et al. Folic Acid-Adorned Curcumin-Loaded Iron Oxide Nanoparticles for Cervical Cancer. ACS Appl. Bio Mater. 2022, 5, 1305–1318. [Google Scholar] [CrossRef]
- Fathima, E.; Nallamuthu, I.; Anand, T.; Naika, M.; Khanum, F. Enhanced cellular uptake, transport and oral bioavailability of optimized folic acid-loaded chitosan nanoparticles. Int. J. Biol. Macromol. 2022, 208, 596–610. [Google Scholar] [CrossRef]
- Rostami, N.; Nikzad, A.; Shaybani, S.; Noei, H.; Ghebleh, A.; Alidadi, M.; Abbasi, H.; Bencherif, S.A. Engineering Folic Acid-Modified Nanoparticles to Enhance Letrozole’s Anticancer Action. Macromol. Biosci. 2025, 25, 2400558. [Google Scholar] [CrossRef]
- Jafarpour, N.; Nikpassand, M.; Faramarzi, M. Conjugation of folic acid onto poly (acrylic acid-co-allylamine)-grafted mesoporous silica nanoparticles for controlled methotrexate delivery. J. Drug Deliv. Sci. Technol. 2024, 96, 105667. [Google Scholar] [CrossRef]
- Zhang, Z.; Jia, J.; Lai, Y.; Ma, Y.; Weng, J.; Sun, L. Conjugating folic acid to gold nanoparticles through glutathione for targeting and detecting cancer cells. Biorg. Med. Chem. 2010, 18, 5528–5534. [Google Scholar] [CrossRef]
- Fuster, M.G.; Wang, J.; Fandiño, O.; Víllora, G.; Paredes, A.J. Folic Acid-Decorated Nanocrystals as Highly Loaded Trojan Horses to Target Cancer Cells. Mol. Pharm. 2024, 21, 2781–2794. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Ge, Z.; Pang, Y. Conjugating folate on superparamagnetic Fe3O4@Au nanoparticles using click chemistry. J. Solid State Chem. 2015, 222, 37–43. [Google Scholar] [CrossRef]
- Kumar, A.; Lale, S.V.; Aji Alex, M.R.; Choudhary, V.; Koul, V. Folic acid and trastuzumab conjugated redox responsive random multiblock copolymeric nanocarriers for breast cancer therapy: In-vitro and in-vivo studies. Colloids Surf. B Biointerfaces 2017, 149, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Pandit, P.; Bhagat, S.; Rananaware, P.; Mohanta, Z.; Kumar, M.; Tiwari, V.; Singh, S.; Brahmkhatri, V.P. Iron oxide nanoparticle encapsulated; folic acid tethered dual metal organic framework-based nanocomposite for MRI and selective targeting of folate receptor expressing breast cancer cells. Microporous Mesoporous Mater. 2022, 340, 112008. [Google Scholar] [CrossRef]
- Rodero, C.F.; Luiz, M.T.; Sato, M.R.; Boni, F.; Fernandes, G.F.S.; dos Santos, J.L.; Martinez-Lopez, A.L.; Irache, J.M.; Chorilli, M. Rapamycin-loaded nanostructured lipid carrier modified with folic acid intended for breast cancer therapy. Int. J. Pharm. 2025, 668, 124954. [Google Scholar] [CrossRef]
- Nabawi, H.M.S.; Abdelazem, A.Z.; El Rouby, W.M.A.; El-Shahawy, A.A.G. A potent formula against triple-negative breast cancer—Sorafenib-carbon nanotubes-folic acid: Targeting, apoptosis triggering, and bioavailability enhancing. Biotechnol. Appl. Biochem. 2025, 72, 86–103. [Google Scholar] [CrossRef]
- Safwat, S.; Ishak, R.A.H.; Hathout, R.M.; Mortada, N.D. Bioinspired caffeic acid-laden milk protein-based nanoparticles targeting folate receptors for breast cancer treatment. Ther. Deliv. 2025, 16, 43–61. [Google Scholar] [CrossRef]
- Varvarà, P.; Mauro, N.; Cavallaro, G. Targeted NIR-triggered doxorubicin release using carbon dots–poly(ethylene glycol)–folate conjugates for breast cancer treatment. Nanoscale Adv. 2025, 7, 862–875. [Google Scholar] [CrossRef]
- Srinivasarao, M.; Galliford, C.V.; Low, P.S. Principles in the design of ligand-targeted cancer therapeutics and imaging agents. Nat. Rev. Drug Discov. 2015, 14, 203–219. [Google Scholar] [CrossRef]
- Yan, S.; Na, J.; Liu, X.; Wu, P. Different Targeting Ligands-Mediated Drug Delivery Systems for Tumor Therapy. Pharmaceutics 2024, 16, 248. [Google Scholar] [CrossRef]
- Haribabu, V.; Sharmiladevi, P.; Akhtar, N.; Farook, A.S.; Girigoswami, K.; Girigoswami, A. Label free ultrasmall fluoromagnetic ferrite-clusters for targeted cancer imaging and drug delivery. Curr. Drug Deliv. 2019, 16, 233–241. [Google Scholar] [CrossRef]
- Mohammadi Barzelighi, H.; Bakhshi, B.; Daraei, B.; Mirzaei, A. Investigating the effect of rAzurin loaded mesoporous silica nanoparticles enwrapped with chitosan-folic acid on breast tumor regression in BALB/C mice. Int. J. Biol. Macromol. 2025, 300, 139245. [Google Scholar] [CrossRef]
- Okuyucu, C.E.; Kalaycioglu, G.D.; Ozden, A.K.; Aydogan, N. Chemosensitizer Loaded NIR-Responsive Nanostructured Lipid Carriers: A Tool for Drug-Resistant Breast Cancer Synergistic Therapy. ACS Appl. Bio Mater. 2025, 8, 2167–2181. [Google Scholar] [CrossRef]
- Pandey, P.; Arya, D.K.; Kumar, A.; Kaushik, A.; Mishra, Y.K.; Rajinikanth, P.S. Dual ligand functionalized pH-sensitive liposomes for metastatic breast cancer treatment: In vitro and in vivo assessment. J. Mater. Chem. B 2025, 13, 2682–2694. [Google Scholar] [CrossRef]
- Ha, C.H.; Hur, W.; Lee, S.J.; Lee, H.B.; Kim, D.H.; Seong, G.H. Targeted photothermal cancer therapy using surface-modified transition metal dichalcogenides. J. Photochem. Photobiol. A Chem. 2025, 459, 116062. [Google Scholar] [CrossRef]
- Ly, H.Q.; Nguyen, Q.T.; Vu, H.P.; Nguyen, V.T. Development and evaluation of folate-gelatin-poloxamer P407 copolymer nanogels for enhanced co-delivery of paclitaxel and curcumin in breast cancer therapy. Colloid Polym. Sci. 2025, 303, 261–276. [Google Scholar] [CrossRef]
- Hashemi, A.; Aliasgari, D.; Abbasi, H.; Baghbani-Arani, F. Synthesis and Application of Zr MOF UiO-66 Decorated with Folic Acid-Conjugated Poly Ethylene Glycol as a Strong Nanocarrier for the Targeted Drug Delivery of Epirubicin. J. Clust. Sci. 2025, 36, 51. [Google Scholar] [CrossRef]
- Aslam, A.; Perveen, K.; Berger, M.R.; Zepp, M.; Klika, K.D.; Hameed, A.; Masood, F. Folic acid-grafted poly-3-hydroxybutyrate nanoparticles for enhanced pH-sensitive paclitaxel delivery and cancer cell targeting. Colloids Surf. Physicochem. Eng. Asp. 2025, 710, 136141. [Google Scholar] [CrossRef]
- Rajana, N.; Sandeep Chary, P.; Bhavana, V.; Deshmukh, R.; Dukka, K.; Sharma, A.; Kumar Mehra, N. Targeted delivery and apoptosis induction of CDK-4/6 inhibitor loaded folic acid decorated lipid-polymer hybrid nanoparticles in breast cancer cells. Int. J. Pharm. 2024, 651, 123787. [Google Scholar] [CrossRef]
- Kunjiappan, S.; Panneerselvam, T.; Pavadai, P.; Balakrishnan, V.; Pandian, S.R.K.; Palanisamy, P.; Sankaranarayanan, M.; Kabilan, S.J.; Sundaram, G.A.; Tseng, W.-L.; et al. Fabrication of folic acid-conjugated pyrimidine-2(5H)-thione-encapsulated curdlan gum-PEGamine nanoparticles for folate receptor targeting breast cancer cells. Int. J. Biol. Macromol. 2024, 277, 134406. [Google Scholar] [CrossRef]
- Radhakrishna, G.K.; Ramesh, S.H.; Almeida, S.D.; Sireesha, G.; Ramesh, S.; Theivendren, P.; Kumar, A.S.K.; Chidamabaram, K.; Ammunje, D.N.; Kunjiappan, S.; et al. Capsaicin-Entangled Multi-Walled Carbon Nanotubes Against Breast Cancer: A Theoretical and Experimental Approach. J. Clust. Sci. 2024, 35, 2849–2869. [Google Scholar] [CrossRef]
- Nigro, A.; Frattaruolo, L.; Fava, M.; De Napoli, I.; Greco, M.; Comandè, A.; De Santo, M.; Pellegrino, M.; Ricci, E.; Giordano, F.; et al. Bortezomib-Loaded Mesoporous Silica Nanoparticles Selectively Alter Metabolism and Induce Death in Multiple Myeloma Cells. Cancers 2020, 12, 2709. [Google Scholar] [CrossRef] [PubMed]
- Amsaveni, G.; Farook, A.S.; Haribabu, V.; Murugesan, R.; Girigoswami, A. Engineered multifunctional nanoparticles for DLA cancer cells targeting, sorting, MR imaging and drug delivery. Adv. Sci. Eng. Med. 2013, 5, 1340–1348. [Google Scholar] [CrossRef]
- Harini, K.; Girigoswami, K.; Pallavi, P.; Gowtham, P.; Prabhu, A.D.; Girigoswami, A. Advancement of magnetic particle imaging in diagnosis and therapy. Adv. Nat. Sci. Nanosci. Nanotechnol. 2024, 15, 023002. [Google Scholar] [CrossRef]
- Gowtham, P.; Girigoswami, K.; Pallavi, P.; Harini, K.; Gurubharath, I.; Girigoswami, A. Alginate-Derivative Encapsulated Carbon Coated Manganese-Ferrite Nanodots for Multimodal Medical Imaging. Pharmaceutics 2022, 14, 2550. [Google Scholar] [CrossRef]
- Tagde, P.; Kulkarni, G.T.; Mishra, D.K.; Kesharwani, P. Recent advances in folic acid engineered nanocarriers for treatment of breast cancer. J. Drug Deliv. Sci. Technol. 2020, 56, 101613. [Google Scholar] [CrossRef]
- Zhang, H.; Li, J.; Hu, Y.; Shen, M.; Shi, X.; Zhang, G. Folic acid-targeted iron oxide nanoparticles as contrast agents for magnetic resonance imaging of human ovarian cancer. J. Ovarian Res. 2016, 9, 19. [Google Scholar] [CrossRef]
- Vijayakumar, V.; Rathinam, T. Nanofibers in Biomedical Applications: Recent Developments and Challenges. Biomed. Mater. Devices 2025. [Google Scholar] [CrossRef]
- Theivendren, P.; Pavadai, P.; Kunjiappan, S.; Ravi, K.; Kiruthiga, N.; Chidamabaram, K.; Alagarsamy, S.; Reddy, N.B. Emerging therapeutic strategies and opportunities in targeting protein pathways for breast cancer treatment: A critical review. Nanotechnology 2025, 36, 232001. [Google Scholar] [CrossRef]
- Hosseinabadi, S.Z.; Safari, S.; Mirzaei, M.; Mohammadi, E.; Amini, S.M.; Mehravi, B. Folic acid decorated mesoporous silica nanospheres loaded with gadolinium for breast cancer cell imaging. Adv. Nat. Sci. Nanosci. Nanotechnol. 2020, 11, 045010. [Google Scholar] [CrossRef]
- Chávez-García, D.; Juárez-Moreno, K.; Campos, C.H.; Alderete, J.B.; Hirata, G.A. Upconversion rare earth nanoparticles functionalized with folic acid for bioimaging of MCF-7 breast cancer cells. J. Mater. Res. 2018, 33, 191–200. [Google Scholar] [CrossRef]
- Gunduz, U.; Keskin, T.; Tansık, G.; Mutlu, P.; Yalcın, S.; Unsoy, G.; Yakar, A.; Khodadust, R.; Gunduz, G. Idarubicin-loaded folic acid conjugated magnetic nanoparticles as a targetable drug delivery system for breast cancer. Biomed. Pharmacother. 2014, 68, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Heidari Majd, M.; Asgari, D.; Barar, J.; Valizadeh, H.; Kafil, V.; Abadpour, A.; Moumivand, E.; Mojarrad, J.S.; Rashidi, M.R.; Coukos, G.; et al. Tamoxifen loaded folic acid armed PEGylated magnetic nanoparticles for targeted imaging and therapy of cancer. Colloids Surf. B Biointerfaces 2013, 106, 117–125. [Google Scholar] [CrossRef]
- Cheng, C.-Y.; Ou, K.-L.; Huang, W.-T.; Chen, J.-K.; Chang, J.-Y.; Yang, C.-H. Gadolinium-Based CuInS2/ZnS Nanoprobe for Dual-Modality Magnetic Resonance/Optical Imaging. ACS Appl. Mater. Interfaces 2013, 5, 4389–4400. [Google Scholar] [CrossRef] [PubMed]
- Mortezazadeh, T.; Gholibegloo, E.; Alam, N.R.; Dehghani, S.; Haghgoo, S.; Ghanaati, H.; Khoobi, M. Gadolinium (III) oxide nanoparticles coated with folic acid-functionalized poly(β-cyclodextrin-co-pentetic acid) as a biocompatible targeted nano-contrast agent for cancer diagnostic: In vitro and in vivo studies. Magn. Reson. Mater. Phys. Biol. Med. 2019, 32, 487–500. [Google Scholar] [CrossRef]
- Zhang, G.; Gao, J.; Qian, J.; Zhang, L.; Zheng, K.; Zhong, K.; Cai, D.; Zhang, X.; Wu, Z. Hydroxylated Mesoporous Nanosilica Coated by Polyethylenimine Coupled with Gadolinium and Folic Acid: A Tumor-Targeted T1 Magnetic Resonance Contrast Agent and Drug Delivery System. ACS Appl. Mater. Interfaces 2015, 7, 14192–14200. [Google Scholar] [CrossRef]
- Ledermann, J.A.; Canevari, S.; Thigpen, T. Targeting the folate receptor: Diagnostic and therapeutic approaches to personalize cancer treatments. Ann. Oncol. 2015, 26, 2034–2043. [Google Scholar] [CrossRef] [PubMed]
- Vergote, I.; Leamon, C.P. Vintafolide: A novel targeted therapy for the treatment of folate receptor expressing tumors. Ther. Adv. Med. Oncol. 2015, 7, 206–218. [Google Scholar] [CrossRef]
- Chelariu-Raicu, A.; Vu, T.C.; Umamaheswaran, S.; Stur, E.; Hanjra, P.; Han, Y.; Hu, M.; Lin, J.; Lawson, B.C.; Liu, J.; et al. IMGN853 Induces Autophagic Cell Death in Combination Therapy for Ovarian Cancer. Cancer Res. Commun. 2025, 5, 512–526. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Shen, J.; Streaker, E.D.; Lockwood, M.; Zhu, Z.; Low, P.S.; Dimitrov, D.S. A folate receptor beta-specific human monoclonal antibody recognizes activated macrophage of rheumatoid patients and mediates antibody-dependent cell-mediated cytotoxicity. Arthritis Res. Ther. 2011, 13, R59. [Google Scholar] [CrossRef] [PubMed]
- Lynn, R.C.; Poussin, M.; Kalota, A.; Feng, Y.; Low, P.S.; Dimitrov, D.S.; Powell, D.J., Jr. Targeting of folate receptor β on acute myeloid leukemia blasts with chimeric antigen receptor-expressing T cells. Blood 2015, 125, 3466–3476. [Google Scholar] [CrossRef] [PubMed]
- Fernández, M.; Javaid, F.; Chudasama, V. Advances in targeting the folate receptor in the treatment/imaging of cancers. Chem. Sci. 2018, 9, 790–810. [Google Scholar] [CrossRef]
- Boshnjaku, V.; Shim, K.-W.; Tsurubuchi, T.; Ichi, S.; Szany, E.V.; Xi, G.; Mania-Farnell, B.; McLone, D.G.; Tomita, T.; Mayanil, C.S. Nuclear localization of folate receptor alpha: A new role as a transcription factor. Sci. Rep. 2012, 2, 980. [Google Scholar] [CrossRef]
- Abdelaal, A.M.; Sohal, I.S.; Iyer, S.; Sudarshan, K.; Kothandaraman, H.; Lanman, N.A.; Low, P.S.; Kasinski, A.L. A first-in-class fully modified version of miR-34a with outstanding stability, activity, and anti-tumor efficacy. Oncogene 2023, 42, 2985–2999. [Google Scholar] [CrossRef]
- Li, W.; Wang, Y.; Liu, X.; Wu, S.; Wang, M.; Turowski, S.G.; Spernyak, J.A.; Tracz, A.; Abdelaal, A.M.; Sudarshan, K.; et al. Developing Folate-Conjugated miR-34a Therapeutic for Prostate Cancer: Challenges and Promises. Int. J. Mol. Sci. 2024, 25, 2123. [Google Scholar] [CrossRef]
- Mohanty, V.; Shah, A.; Allender, E.; Siddiqui, M.R.; Monick, S.; Ichi, S.; Mania-Farnell, B.; McLone, D.G.; Tomita, T.; Mayanil, C.S. Folate Receptor Alpha Upregulates Oct4, Sox2 and Klf4 and Downregulates miR-138 and miR-let-7 in Cranial Neural Crest Cells. Stem Cells 2016, 34, 2721–2732. [Google Scholar] [CrossRef]
- DeCarlo, A.; Malardier-Jugroot, C.; Szewczuk, M.R. Folic Acid-Functionalized Nanomedicine: Folic Acid Conjugated Copolymer and Folate Receptor Interactions Disrupt Receptor Functionality Resulting in Dual Therapeutic Anti-Cancer Potential in Breast and Prostate Cancer. Bioconjug. Chem. 2021, 32, 512–522. [Google Scholar] [CrossRef]
- Zhu, W.T.; Zeng, X.F.; Yang, H.; Jia, M.L.; Zhang, W.; Liu, W.; Liu, S.Y. Resveratrol Loaded by Folate-Modified Liposomes Inhibits Osteosarcoma Growth and Lung Metastasis via Regulating JAK2/STAT3 Pathway. Int. J. Nanomed. 2023, 18, 2677–2691. [Google Scholar] [CrossRef]
- Bukowski, K.; Rogalska, A.; Marczak, A. Folate Receptor Alpha—A Secret Weapon in Ovarian Cancer Treatment? Int. J. Mol. Sci. 2024, 25, 11927. [Google Scholar] [CrossRef] [PubMed]
- Xiao, D.; Dong, J.; Xie, F.; Feng, X.; Wang, J.; Xu, X.; Tang, B.; Sun, C.; Wang, Y.; Zhong, W.; et al. Polyvalent folate receptor-targeting chimeras for degradation of membrane proteins. Nat. Chem. Biol. 2025, 21, 1731–1741. [Google Scholar] [CrossRef]
- Hansen, M.F.; Greibe, E.; Skovbjerg, S.; Rohde, S.; Kristensen, A.C.M.; Jensen, T.R.; Stentoft, C.; Kjær, K.H.; Kronborg, C.S.; Martensen, P.M. Folic acid mediates activation of the pro-oncogene STAT3 via the Folate Receptor alpha. Cell. Signal. 2015, 27, 1356–1368. [Google Scholar] [CrossRef]
- Su, L.; Xia, W.; Shen, T.; Liang, Q.; Wang, W.; Li, H.; Jiao, J. H2A.Z.1 crosstalk with H3K56-acetylation controls gliogenesis through the transcription of folate receptor. Nucleic Acids Res. 2018, 46, 8817–8831. [Google Scholar] [CrossRef]
- Nawaz, F.Z.; Kipreos, E.T. Emerging roles for folate receptor FOLR1 in signaling and cancer. Trends Endocrinol. Metab. 2022, 33, 159–174. [Google Scholar] [CrossRef]
- Zhu, M.; Yang, X.; You, J.; Zheng, L.; Yi, C.; Huang, Y. Nanobiotechnology-mediated radioimmunotherapy treatment for triple-negative breast cancer. MedComm—Biomater. Appl. 2023, 2, e32. [Google Scholar] [CrossRef]
- Kefayat, A.; Ghahremani, F.; Motaghi, H.; Mehrgardi, M.A. Investigation of different targeting decorations effect on the radiosensitizing efficacy of albumin-stabilized gold nanoparticles for breast cancer radiation therapy. Eur. J. Pharm. Sci. 2019, 130, 225–233. [Google Scholar] [CrossRef]
- Cheng, K.; Sano, M.; Jenkins, C.H.; Zhang, G.; Vernekohl, D.; Zhao, W.; Wei, C.; Zhang, Y.; Zhang, Z.; Liu, Y.; et al. Synergistically Enhancing the Therapeutic Effect of Radiation Therapy with Radiation Activatable and Reactive Oxygen Species-Releasing Nanostructures. ACS Nano 2018, 12, 4946–4958. [Google Scholar] [CrossRef] [PubMed]
- Guzik, P.; Siwowska, K.; Fang, H.-Y.; Cohrs, S.; Bernhardt, P.; Schibli, R.; Müller, C. Promising potential of [177Lu]Lu-DOTA-folate to enhance tumor response to immunotherapy—A preclinical study using a syngeneic breast cancer model. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 984–994. [Google Scholar] [CrossRef]
- Assaraf, Y.G.; Leamon, C.P.; Reddy, J.A. The folate receptor as a rational therapeutic target for personalized cancer treatment. Drug Resist. Updates 2014, 17, 89–95. [Google Scholar] [CrossRef]
- Siu, M.K.Y.; Kong, D.S.H.; Chan, H.Y.; Wong, E.S.Y.; Ip, P.P.C.; Jiang, L.; Ngan, H.Y.S.; Le, X.-F.; Cheung, A.N.Y. Paradoxical Impact of Two Folate Receptors, FRα and RFC, in Ovarian Cancer: Effect on Cell Proliferation, Invasion and Clinical Outcome. PLoS ONE 2012, 7, e47201. [Google Scholar] [CrossRef]
- Sega, E.I.; Low, P.S. Tumor detection using folate receptor-targeted imaging agents. Cancer Metastasis Rev. 2008, 27, 655–664. [Google Scholar] [CrossRef]
- Morris, R.T.; Joyrich, R.N.; Naumann, R.W.; Shah, N.P.; Maurer, A.H.; Strauss, H.W.; Uszler, J.M.; Symanowski, J.T.; Ellis, P.R.; Harb, W.A. Phase II study of treatment of advanced ovarian cancer with folate-receptor-targeted therapeutic (vintafolide) and companion SPECT-based imaging agent (99mTc-etarfolatide)†. Ann. Oncol. 2014, 25, 852–858. [Google Scholar] [CrossRef]
- Pribble, P.; Edelman, M.J. EC145: A novel targeted agent for adenocarcinoma of the lung. Expert Opin. Investig. Drugs 2012, 21, 755–761. [Google Scholar] [CrossRef]
- Lu, Y.; Low, P.S. Folate-mediated delivery of macromolecular anticancer therapeutic agents. Adv. Drug Deliv. Rev. 2002, 54, 675–693. [Google Scholar] [CrossRef]
- Ibrahim, M.; Fathalla, Z.; Fatease, A.A.; Alamri, A.H.; Abdelkader, H. Breast cancer epidemiology, diagnostic barriers, and contemporary trends in breast nanotheranostics and mechanisms of targeting. Expert Opin. Drug Deliv. 2024, 21, 1735–1754. [Google Scholar] [CrossRef] [PubMed]
- Bou-Dargham, M.J.; Draughon, S.; Cantrell, V.; Khamis, Z.I.; Sang, Q.A. Advancements in Human Breast Cancer Targeted Therapy and Immunotherapy. J. Cancer 2021, 12, 6949–6963. [Google Scholar] [CrossRef] [PubMed]
- Necela, B.M.; Crozier, J.A.; Andorfer, C.A.; Lewis-Tuffin, L.; Kachergus, J.M.; Geiger, X.J.; Kalari, K.R.; Serie, D.J.; Sun, Z.; Moreno-Aspitia, A.; et al. Folate receptor-α (FOLR1) expression and function in triple negative tumors. PLoS ONE 2015, 10, e0122209. [Google Scholar] [CrossRef]
- Türeli, N.G.; Türeli, A.E. Chapter 11—Upscaling and GMP production of pharmaceutical drug delivery systems. In Drug Delivery Trends; Shegokar, R., Ed.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 215–229. [Google Scholar]
- Nehal, N.; Rohilla, A.; Sartaj, A.; Baboota, S.; Ali, J. Folic acid modified precision nanocarriers: Charting new frontiers in breast cancer management beyond conventional therapies. J. Drug Target. 2024, 32, 855–873. [Google Scholar] [CrossRef]



| Nanostructures/Modifications | Chemotherapeutics/Payloads | Potential Applications | Limitations | Ref. |
|---|---|---|---|---|
| Janus nanostructure composed of liposomes and porous and amorphous zeolitic imidazole framework (AZIF-8) | AZIF-8 encapsulated with Dox & Liposomes with mitoxantrone coated with cell membrane & aptamer | Dual-targeted breast cancer therapy with the least side effects, tumor suppression in BALB/c mice | Complex synthesis and safety concern | [68] |
| Biomimetic nanocomplex combining cationic liposomes & macrophage-evolved exosomes | Docetaxel & Bcl-2 siRNA | ROS-responsive co-delivery induces apoptosis in tumor cells, increasing circulation half-life. | Long-term toxicity and immune response | [69] |
| Biodegradable chitosan nanoparticles | Tetraphenylchlorin conjugation, combining ferroptosis inducer RSL3 | Boosts cellular stress & respiration, with mesenchymal-like breast cancer cells showing high ferroptosis susceptibility | In vivo validation and safety issues | [70] |
| Self-assembled polymer made of amino-functionalized hydroxyethyl starch grafted with cholesterol. | Flucoxanthin & siRNA | Remodeled TME, synergistically killed tumor cells, reduced TNBC tumor burden, and inhibited lung metastasis. | Biocompatibility and clinical validation | [71] |
| PEGylated Mn-coordinated nanoparticles | Chlorin e6 and STING agonists MSA-2 | Phototherapeutic effect, induced immunogenic cell death, overcoming antitumor immunity. | Concentration-dependent manganese toxicity | [72] |
| FCPCV nanoparticles & CRISPR-Cas9 | sgRNA targeting CCL5 | Silenced CCL5, boosted CD8+ T cell activity, improved cytokine production, suppressed tumor, promising personalized breast cancer immunotherapy. | Off-target gene editing | [73] |
| Tetrahedral DNA nanoparticles | siOTUD6B and Dox | Controlled release & improved cellular uptake of Dox, inhibits metastasis | In vivo stability of DNA-based nanostructures | [74] |
| Human serum albumin (HAS)-α-tocopherol succinate nanoparticles | Lapatinib & letrozole | Inhibit tumor development and induce apoptosis. | Long-term safety | [75] |
| Chitosan nanoparticles | 5-FU and trastuzumab | Targeting SK-BR-3 cell line, 85.2% tumor inhibition, efficiently targeted breast cancer therapeutics. | Clinical validation and immunogenicity | [76] |
| Camouflaged liposomes functionalized with iRGDP. | Trastuzumab, Gefitinib, lycorine hydrochloride | Improved IC50 against MCF-7 cells, a potential multifaceted therapy against metastatic breast cancer. | Comprehensive pharmacokinetics and toxicity | [77] |
| Platelet membrane encapsulated biomimetic iron oxide nanoparticles | Paclitaxel | pH-responsive drug delivery, targeted magnetic hyperthermia, IC50 values reduced to 1 μg/mL & more than 92% tumor growth inhibition | In vivo safety and toxicity | [78] |
| Iron oxide nanoparticles | Curcumin | Photodynamic therapy mediated tumor cell death, with 32% cell viability at 30 mg/mL concentration. | Detailed mechanistic assessment | [79] |
| pH-responsive magnetic-chitosan core–shell nanoparticles | Methotrexate | pH-responsive drug release significantly enhanced the anticancer effect. | In vivo toxicity validation | [80] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Girigoswami, K.; Girigoswami, A. Breast Cancer Progression and Its Theranostic Management via Folate-Directed Targeting of Glycoprotein Receptor. Med. Sci. 2025, 13, 275. https://doi.org/10.3390/medsci13040275
Girigoswami K, Girigoswami A. Breast Cancer Progression and Its Theranostic Management via Folate-Directed Targeting of Glycoprotein Receptor. Medical Sciences. 2025; 13(4):275. https://doi.org/10.3390/medsci13040275
Chicago/Turabian StyleGirigoswami, Koyeli, and Agnishwar Girigoswami. 2025. "Breast Cancer Progression and Its Theranostic Management via Folate-Directed Targeting of Glycoprotein Receptor" Medical Sciences 13, no. 4: 275. https://doi.org/10.3390/medsci13040275
APA StyleGirigoswami, K., & Girigoswami, A. (2025). Breast Cancer Progression and Its Theranostic Management via Folate-Directed Targeting of Glycoprotein Receptor. Medical Sciences, 13(4), 275. https://doi.org/10.3390/medsci13040275







