Abstract
Introduction: Stroke is the fifth leading cause of death and long-term disability in the United States. The current guideline for stroke management includes a 25 min timeframe from door-to-computed tomography time (DTCT). However, sociodemographic backgrounds may impact the DTCT in acute stroke patients. Methods: This was a retrospective, multicenter, cohort study between January 2018 and August 2022 throughout North Texas. The primary endpoint was DTCT ≤ 25 min upon arrival to hospital for all patients suspected of acute ischemic stroke. Results: During the study period, a total of 23,364 patients were included. Only 4468 patients (19.1%) had DTCT times less than or equal to 25 min, and 16,464 patients (70.5%) had DTCT times more than 25 min. In our cohort, Black (OR 1.35; 95% CI 1.23–1.49) and Asian patients (OR 1.33; 95% CI 1.01–1.74) were more likely to have DTCT > 25 min compared to White patients. Hispanic patients (OR 1.20; 95% CI 1.07–1.34) were more likely to have DTCT > 25 min compared to non-Hispanics. Patients presenting during the COVID (OR 1.45; 95% CI 1.34–1.57) and post-COVID period (OR 1.46; 95% CI 1.30–1.65) were more likely to have DTCT > 25 min compared to the pre-COVID period. Conclusions: We demonstrated a discrepancy in DTCT time for acute ischemic stroke patients based on their race and ethnic population and an increase in DTCT time after the start of COVID-19, which has persisted after the pandemic. These diverse factors highlight the complex interplay of logistical, organizational, and healthcare challenges that have influenced DTCT time.
1. Introduction
Stroke is the fifth leading cause of death and long-term disability in the United States, with an estimated prevalence of 7 million individuals affected as of 2019 [1,2]. Studies have shown that earlier administration of intravenous (IV) thrombolytic therapy has been associated with higher rates of favorable clinical outcomes in acute ischemic strokes [3] which is consistent with the Get With The Guidelines-Stroke (GWTG-S) quality improvement program recommendation of IV thrombolytic therapy within 60 min of arrival to the hospital (door-to-needle time, DTNT) [4]. Improved healthcare access and enhanced emergency stroke care protocols have led to a reduction in stroke-related mortality. Brain imaging is required before the administration of IV thrombolytic therapy, and the GWTG-S recommends computed tomography (CT) of the brain within 25 min of arrival to the hospital (door-to-CT time (DTCT) ≤ 25 min) [3], making the achievement of this guideline a precursor to achieving good clinical outcomes. Protocols for stroke management established by the American Heart Association (AHA) and American Stroke Association (ASA) include a 25 min timeframe from door to CT time (DTCT) [5,6]. Minimizing any source of delay in imaging can significantly improve morbidity and mortality for patients experiencing stroke.
In a prior analysis of data from the GWTG-S quality improvement program, only 41.8% of patients with ischemic stroke achieved DTCT ≤ 25 min, with a range of 0% to 100% across hospitals [3]. Since then, a systematic review in 2021 highlighted many factors that are associated with delayed DTCT, including clinical presentation of posterior circulation stroke, presence of nausea or vomiting, and assessment-related delays [7]. Specific factors that have been found to be associated with imaging-related delays include lack of CT scanner availability, airway, or hemodynamic compromise, and waiting for renal function testing [7]. Recent studies focus on the last known well-to-arrival time and neighborhood-level socioeconomic status [8,9]. Despite improved knowledge on barriers to DTCT, there is relatively limited literature assessing the role of sociodemographic factors, and of the literature that exists, there is conflicting evidence regarding the effects of ethnicity, race, sex, age, and disability [3,7,10,11,12,13].
Few studies have examined race/ethnic differences in secondary stroke care metrics, such as DTCT time, despite well-established disparities in acute stroke care [7]. The most recent study regarding this topic was published in 2021 using the Florida Stroke Registry [7]. The results revealed significant disparities in receiving DTCT ≤ 25 that affect female, Black, and non-Hispanic patients who had strokes, despite notable improvements in this acute stroke care metric from 2010 to 2018. To our knowledge, there have been no studies of this kind done in Texas. According to 2021 United States Census Bureau data, Texas has a particularly high percentage of Hispanic or Latino residents (39.7%), compared to only 26.4% in Florida, which may influence the data. Further research into the relationship between sociodemographic factors and achievement of GWTG-S guidelines will help to target specific interventions that will be essential in eliminating racial/ethnic disparities in stroke health care.
Besides different patient demographics, Emergency Departments (ED) faced unprecedented challenges, including increased patient volumes, resource constraints, and rigorous infection control protocols during COVID-19 times. Adapting to these challenges likely increased the DTCT in acute stroke patients. Yoshimoto et al. demonstrated that patients during the pandemic had a 2 min longer median door-to-imaging time [14]. Siegler et al. also showcased that patients treated during COVID-19 were less likely to receive thrombolysis within 60 min of arrival [15]. Kobayashi et al. showed door-to-balloon time for ST elevation myocardial infarction patients was significantly prolonged during the pandemic [16]. A recent systematic review in 2022 highlighted COVID-19 screening processes, the need for chest CT scans, and multidisciplinary consultation as influencing factors for DTCT and intravenous thrombolysis treatment times [7,17].
These diverse factors highlight the complex interplay of logistical, organizational, and healthcare challenges that have influenced DTCT time. However, sociodemographic factors remain insufficiently examined and are crucial to healthcare equality [18]. Identifying disparities can help address inequities and ensure that all patients, regardless of background, receive timely care. Of the literature that addresses barriers to DTCT, there is conflicting evidence regarding the effects of ethnicity, race, sex, age, and disability. Polineni et al. demonstrated that women and Black patients were less likely to achieve DTCT goals [7]. De Havenon et al. showed that increased death rates were associated with social deprivation index, urban location, unemployment rate, and proportion of Black race and Hispanic ethnicity [19]. This retrospective multicohort center study aimed to investigate the association between sociodemographic disparities and DTCT time in patients with acute ischemic stroke (AIS) in North Texas. Additionally, we examined the impact of COVID-19 across different pandemic periods to assess its influence on stroke care disparities.
2. Methods
2.1. Study Design and Setting
This is a retrospective, multicenter, cohort study conducted from 1 January 2018 to 16 August 2022 in five urban EDs of Baylor Scott & White Healthcare System in North Texas. Potential patient encounters were initially identified through a search of the electronic medical record (EMR) of all study sites by using the International Classification of Disease-10 (ICD-10) codes specific to the primary diagnosis of acute ischemic stroke and transient ischemic attack. The Baylor Scott & White Health Institutional Review Board approved this project (reference ID: 022-169) and exempted the requirement for informed consent due to the retrospective and non-invasive nature of the study. This article followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. We adhered to all tenets of the Declaration of Helsinki.
2.2. Participants Selection
The study encompassed an urban patient population enrolled in the Baylor Scott & White Health Care System. These EDs were affiliated with both community and teaching hospitals and included trauma center designation levels I through IV located in urban areas. Adult patients (18 years or older) who presented with stroke-like symptoms based on the ED code stroke protocol were included in the study. The suspected diagnosis of acute ischemic stroke was made by the emergency physician. Per AHA/ASA guidelines, stroke is recognized per the “FAST” algorithm. The signs include facial droop, arm weakness, slurred speech, and time of onset [20]. Patients were excluded from the study if they were under the age of 18, arrived at the hospital over 24 h symptom onset, were diagnosed with stroke sub-types other than ischemic, had concomitant traumatic injury, or had significant missing data. A team of research staff reviewed the EMR to ensure eligibility and collect data. Information was ascertained on each patient encounter, including patient demographics, medical history, vital signs, laboratory values, treatment course, and clinical outcomes. If a patient presented more than once during the study period, data from only the first presentation were retained for analysis.
2.3. Outcome Measure
The primary endpoint was DTCT ≤ 25 min upon arrival at the hospital for all patients suspected of acute ischemic stroke. We followed guidelines from the US Centers for Disease Control and Prevention to classify patients’ self-identified race and ethnicity into the following categories: Race (White, Black, Asian, and others) and ethnicity (Hispanic vs. non-Hispanic) [7]. The secondary outcome was the association between DTCT and patient age, gender, comorbidities, and COVID period. COVID status was classified as pre-COVID, COVID, and post-COVID. Pre-COVID was defined as any time before March 2020. COVID was defined as anytime between March 2020 and February 2022. Post-COVID was defined as any time after February 2022.
2.4. Data Collection
Data for this study were systematically retrieved from the Electronic Medical Records (EMR) system, which was consistently used across all EDs involved in the research. The data collected comprised a wide range of patient-specific information, including demographic characteristics, smoking history, and relevant medical history. Additional details such as vital signs (e.g., blood pressure, heart rate, respiratory rate, and temperature), ED length of stay, laboratory test results, radiology findings, and clinical outcomes were all included in the dataset. The data were extracted from the EHR database by a trained research investigator, who ensured consistency and accuracy across all variables. The collected data were then entered into a secure, encrypted Microsoft Excel spreadsheet (Microsoft Excel 2010; Microsoft Corporation, Seattle, WA, USA) for further processing and analysis. The encrypted spreadsheet was subsequently reviewed and verified by multiple co-investigators of the study team, who conducted thorough checks to ensure the accuracy and completeness of the data before proceeding with the analysis. This multi-step review process helped to minimize errors and guarantee the reliability of the data collected from the diverse range of EDs involved in the study.
2.5. Statistical Analysis
In the univariable analysis, continuous variables were presented as means with SD, and categorical variables were presented as frequencies with percentages. The Student’s t-test and the Pearson chi-square test were used to compare the differences for continuous and categorical variables, respectively. Multivariate logistic regression was performed to evaluate the factors associated with delayed DTCT time, including COVID status, race, ethnicity, and sex disparities. A p-value < 0.05 was considered statistically significant. All statistical analyses were performed using Stata software (StataCorp. 2023. Stata Statistical Software: Release 18. College Station, TX, USA: StataCorp LLC. software).
The odds ratio (OR) was selected to measure the association between variables and the primary outcome. Multivariable logistic regression analyses were performed to examine the associations between independent variables and outcomes. All available independent variables were considered in the regression model, regardless of whether they were scored as significant by univariate analyses. The stepwise variable selection procedure, with iterations between the forward and backward steps, was applied to obtain the final regression model. Significance levels for entry and to stay were set at 0.15 to avoid exclusion of potential candidate variables. The final regression model was determined by sequentially excluding individual variables with a p-value > 0.05 until all regression coefficients were significant.
3. Results
3.1. Patient Characteristics
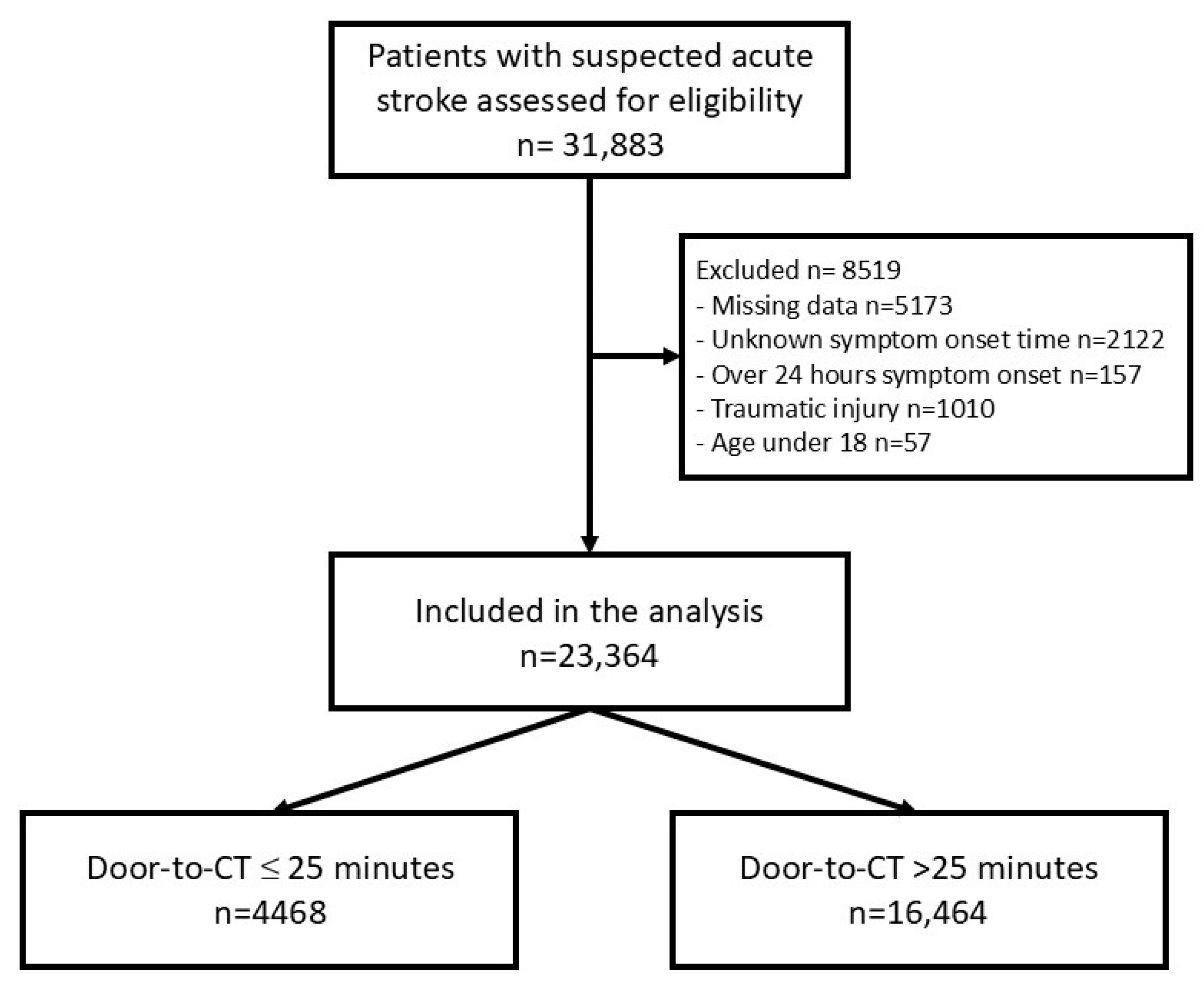
During the study period, a total of 31,883 patient encounters met eligibility criteria. Of these, 23,364 encounters were included in the final analysis (Figure 1). The mean age of the participants was 69 ± 15 years with a nearly even gender distribution, as 49.7% of the participants were male. A majority were White (n = 17,345, 74.2%), 20.3% were Black (n = 4745), 1.9% were Asian (n = 454), and 13.5% were Hispanic ethnicity (n = 2807) (Table 1). 4468 patients (19.1%) had DTCT times less than or equal to 25 min, and 16,464 patients (70.5%) had DTCT times more than 25 min. There were significant differences between the two groups in terms of patient age, race/ethnicity, Emergency Severity Index (ESI), and underlying chronic comorbidities, including dementia, chronic renal disease, and chronic liver disease. Patients in the pre-COVID, COVID, and post-COVID phases were 6852 (29.3%), 13,593 (58.2%), and 2919 (12.5%), respectively (Table 1).
Figure 1.
Flow chart of patient selection.

Table 1.
Patient characteristics.
3.2. Outcome Measures
Multivariable logistic regression analysis is shown in Table 2. Black (OR 1.35; 95% CI 1.23–1.49) and Asian patients (OR 1.33; 95% CI 1.01–1.74) were more likely to have DTCT > 25 min compared to White patients. Hispanic patients (OR 1.20; 95% CI 1.07–1.34) were more likely to have DTCT > 25 min compared to non-Hispanic patients. Patients with chronic liver cirrhosis (OR 1.31; 95% CI 1.16–1.49) and chronic renal disease (OR 1.13; 95% CI 1.04–1.22) were more likely to have DTCT greater than 25 min. Patients evaluated during COVID (OR 1.45; 95% CI 1.34–1.57) and post-COVID (OR 1.46; 95% CI 1.30–1.65) were more likely to have DTCT > 25 min compared to patients evaluated in the pre-COVID period.

Table 2.
Multivariable logistic regression analysis for risk factors of having a DTCT of greater than 25 min.
4. Discussion
This study offers crucial insights into the disparities in acute ischemic stroke care, particularly concerning DTCT times, which directly impact the timely administration of life-saving interventions like tPA and thrombectomy. Our findings underscore a significant racial and ethnic inequality, revealing that Black, Asian, and Hispanic patients experience notably longer door-to-CT times compared to other groups, deviating from the best practice guidelines. The identification of these disparities is vital for healthcare systems aiming to optimize stroke care. Moreover, our study highlights the significant role that the patient race and the post-COVID healthcare environment play in influencing these delays. Our findings suggest that delays in DTCT times have not returned to pre-pandemic levels, indicating that systemic challenges remain even after the acute phase of the pandemic. Moreover, racial and ethnic disparities persist across all time periods, reinforcing the need for equity-focused interventions in stroke care. These results not only call attention to the urgent need for targeted interventions to address these inequities but also offer a roadmap for future research and policy development aimed at improving stroke outcomes across all patient populations.
In our study, Black (OR 1.35; 95% CI 1.23–1.49) and Asian patients (OR 1.33; 95% CI 1.01–1.74) were more likely to have DTCT > 25 min compared to White patients, and Hispanic patients (OR 1.20; 95% CI 1.07–1.34) were more likely to have DTCT > 25 min compared to non-Hispanic patients. Previously, multiple studies have demonstrated similar results [3,7,10,11,12,13,21]; however, others have also reported shorter DTCT times for Hispanic patients. This could be explained through systemic and personal factors. At the system level, implicit bias due to relative lack of diversity [22], socioeconomic status, geographic distance, limited access to health care, and lower rates of arrival by EMT services have been proposed as possible causes. On the personal level, delays in DTCT are often attributed to gaps in medical literacy, family support and connection, delays in recognition of symptoms by patient or medical staff, variation in mode of arrival to the hospital, and difficulties presented using in-person or virtual translation services [7,23,24,25,26]. For example, it can be difficult to rapidly communicate the intricacies of symptom timing and evolution across language barriers [27]. Thus, even though considerable efforts may be put forth by medical staff, critical moments may be lost waiting for an interpreter rephrasing questions to accurately screen for stroke-like symptoms [3,7,21,28,29,30,31,32]. However, further research is needed to elucidate the most impactful causes of these disparities.
DTCT times were also significantly affected by the COVID-19 pandemic. In our study, we found that patients presenting during COVID (OR 1.45; 95% CI 1.34–1.57) and post-COVID (OR 1.46; 95% CI 1.30–1.65) were more likely to have DTCT > 25 min compared to the pre-COVID period. Though stroke protocols did not change during this time, and stroke volume may have decreased [33], it is apparent that the delivery of care before COVID was different than during and post-COVID. However, in our literature review, there has been inconsistency in the results. Most studies found no statistically significant change in DTCT time [33,34,35,36,37,38]. One abstract presented at the International Stroke Conference 2022 showed shortened DTCT by 1 min [39]. Another study found improvements in DTCT times during the pandemic [40]. However, they either failed to achieve statistical significance or lacked peer review. Two other studies reported increased DTCT times. Katsanos et al. studied a different population who received tPA or mechanical thrombectomy [41]. Hu et al. showed a 2 min difference but did not provide the percentage of patients that achieved the 25 min DTCT goal [42]. Our study is the first showing a significant delay in DTCT time using a large sample size after the pandemic.
The COVID pandemic forced EDs to incorporate numerous changes in the delivery of medical care. Changes in workflow, including COVID screening, extra precaution with personal protective equipment, and mandatory masking [43], may contribute to the delay in DTCT we observed. Today the turnover time for COVID screening can be as high, which has dramatically decreased since the beginning of the pandemic [44]. Moreover, the mandatory use of masks helped prevent the spread of airborne pathogens but made communication more challenging. Masking may have hindered the ability of healthcare personnel to accurately triage and examine patients, especially in those presenting with facial droop or slurred speech [45,46,47,48,49]. Other studies suggest increased respiratory, gastrointestinal, or systemic symptom screening by both ED triage and stroke teams, concern over isolation precautions, donning of PPE, and overall increased caution during every phase of patient care were all possible sources of delays [41].
The COVID pandemic also led to increased ED boarding and increased provider burnout [50,51,52,53]. Increased ED crowdedness has been shown to negatively impact DTCT times [54,55]. Additionally, many institutions were short-staffed during the pandemic, and health care workers were working more frequently or for longer hours [56,57,58,59]. Increased ED boarding and rate of burn out may have had a synergistic effect on the increased DTCT time we observed in our study.
5. Limitation
There are several limitations to our study. Firstly, due to the retrospective study design and the inability to control for unmeasured confounders, we are limited to reporting associations rather than establishing causality. Unmeasured confounding factors, such as ED crowding, variations in staffing, and differences in hospital protocols, could have influenced DTCT times. Second, the analysis was limited to our healthcare system in North Texas and may have limited external generalizability to other regions. However, our results are consistent with prior studies, including those from large regional datasets, suggesting these disparities are widespread and not due to local practice patterns [7]. We believe it is important to re-emphasize this race/ethnic disparity in CVA management from our cohort. Thirdly, we were not able to identify patients’ mode of arrival to the hospital, the time between symptom onset and arrival, or patients’ spoken language due to the data set presentation in our system based on the limitation of the retrospective design. Fourthly, our data only consists of months after the COVID pandemic. Further effects of the pandemic and recovery from the pandemic cannot be monitored or illustrated with our current data and the retrospective setting. Our study did not include data regarding patient outcomes, so we are unable to assess how these changes in DTCT time affected our patients’ recovery. Lastly, while our study focuses on stroke care disparities rather than incidence rates, we recognize that post-COVID conditions, including increased vascular inflammation and coagulopathy, may contribute to a higher burden of stroke. Future studies are still needed on these topics.
6. Conclusions
We demonstrated a discrepancy in DTCT time for acute ischemic stroke patients based on their race and ethnic population. Black and Asian patients were more likely to have DTCT > 25 min compared to White patients, and Hispanic patients were more likely to have DTCT > 25 min compared to non-Hispanic patients. An increase in DTCT time was observed after the start of COVID-19, which has persisted after the pandemic.
Author Contributions
Conceptualization, A.S., T.D., M.D. and E.H.C.; methodology, C.-F.T.T., A.S., D.H., J.S. and J.W.; formal analysis, E.H.C.; investigation, C.-F.T.T., A.S., T.D., M.D., J.W. and E.H.C.; resources, A.S., D.H., M.D. and E.H.C.; data curation, M.K., D.H., J.S. and E.H.C.; writing—original draft preparation, Y.-L.H., C.-F.T.T. and M.K.; writing—review and editing, Y.-L.H., A.S., T.D., D.H., M.D., J.S., J.W. and E.H.C.; supervision, E.H.C.; project administration, E.H.C. All authors have read and agreed to the published version of the manuscript.
Funding
No external funding received.
Institutional Review Board Statement
This study was approved by the Baylor Scott & White Health Institutional Review Board (IRB reference #022-169).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not publicly available.
Conflicts of Interest
All authors declare that they have no conflicts of interest.
References
- Renedo, D.; Acosta, J.N.; Leasure, A.C.; Sharma, R.; Krumholz, H.M.; de Havenon, A.; Alahdab, F.; Aravkin, A.Y.; Aryan, Z.; Bärnighausen, T.W.; et al. Burden of Ischemic and Hemorrhagic Stroke Across the US from 1990 to 2019. JAMA Neurol. 2024, 81, 394–404. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Tong, X.; Schieb, L.; Coronado, F.; Merritt, R. Stroke Mortality Among Black and White Adults Aged ≥35 Years Before and During the COVID-19 Pandemic—United States, 2015–2021. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.G.; Hellkamp, A.S.; Olson, D.; Smith, E.E.; Schwamm, L.H. Predictors of rapid brain imaging in acute stroke: Analysis of the Get with the Guidelines-Stroke program. Stroke 2012, 43, 1279–1284. [Google Scholar] [CrossRef]
- Association, A.H. Get with the Guideline-Stroke. Available online: https://www.heart.org/en/professional/quality-improvement/get-with-the-guidelines/get-with-the-guidelines-stroke (accessed on 13 February 2025).
- Jauch, E.C.; Saver, J.L.; Adams, H.P., Jr.; Bruno, A.; Connors, J.J.; Demaerschalk, B.M.; Khatri, P.; McMullan, P.W., Jr.; Qureshi, A.I.; Rosenfield, K.; et al. Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013, 44, 870–947. [Google Scholar] [CrossRef]
- Greenberg, S.M.; Ziai, W.C.; Cordonnier, C.; Dowlatshahi, D.; Francis, B.; Goldstein, J.N.; Hemphill, J.C., 3rd; Johnson, R.; Keigher, K.M.; Mack, W.J.; et al. 2022 Guideline for the Management of Patients with Spontaneous Intracerebral Hemorrhage: A Guideline from the American Heart Association/American Stroke Association. Stroke 2022, 53, e282–e361. [Google Scholar] [CrossRef] [PubMed]
- Polineni, S.P.; Perez, E.J.; Wang, K.; Gutierrez, C.M.; Walker, J.; Foster, D.; Dong, C.; Asdaghi, N.; Romano, J.G.; Sacco, R.L.; et al. Sex and Race-Ethnic Disparities in Door-to-CT Time in Acute Ischemic Stroke: The Florida Stroke Registry. J. Am. Heart Assoc. 2021, 10, e017543. [Google Scholar] [CrossRef]
- Ferrone, N.G.; Sanmartin, M.X.; O’Hara, J.; Ferrone, S.R.; Wang, J.J.; Katz, J.M.; Sanelli, P.C. Ten-Year Trends in Last Known Well to Arrival Time in Acute Ischemic Stroke Patients: 2014 to 2023. Stroke 2025, 56, 49169. [Google Scholar] [CrossRef]
- Forman, R.; Okumu, R.; Mageid, R.; Baker, A.; Neu, D.; Parker, R.; Peyravi, R.; Schindler, J.L.; Sansing, L.H.; Sheth, K.N.; et al. Association of Neighborhood-Level Socioeconomic Factors with Delay to Hospital Arrival in Patients with Acute Stroke. Neurology 2024, 102, e207764. [Google Scholar] [CrossRef]
- Oluwole, S.A.; Wang, K.; Dong, C.; Ciliberti-Vargas, M.A.; Gutierrez, C.M.; Yi, L.; Romano, J.G.; Perez, E.; Tyson, B.A.; Ayodele, M.; et al. Disparities and Trends in Door-to-Needle Time: The FL-PR CReSD Study (Florida-Puerto Rico Collaboration to Reduce Stroke Disparities). Stroke 2017, 48, 2192–2197. [Google Scholar] [CrossRef]
- Sharobeam, A.; Jones, B.; Walton-Sonda, D.; Lueck, C.J. Factors delaying intravenous thrombolytic therapy in acute ischaemic stroke: A systematic review of the literature. J. Neurol. 2021, 268, 2723–2734. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.A.; Duncan, P.W.; Nguyen-Huynh, M.N.; Ogedegbe, O.G. Interventions Targeting Racial/Ethnic Disparities in Stroke Prevention and Treatment. Stroke 2020, 51, 3425–3432. [Google Scholar] [CrossRef]
- Yoshimoto, T.; Shiozawa, M.; Koge, J.; Inoue, M.; Koga, M.; Ihara, M.; Toyoda, K. Evaluation of Workflow Delays in Stroke Reperfusion Therapy: A Comparison between the Year-Long Pre-COVID-19 Period and the with-COVID-19 Period. J. Atheroscler. Thromb. 2022, 29, 1095–1107. [Google Scholar] [CrossRef] [PubMed]
- Siegler, J.E.; Zha, A.M.; Czap, A.L.; Ortega-Gutierrez, S.; Farooqui, M.; Liebeskind, D.S.; Desai, S.M.; Hassan, A.E.; Starosciak, A.K.; Linfante, I.; et al. Influence of the COVID-19 Pandemic on Treatment Times for Acute Ischemic Stroke: The Society of Vascular and Interventional Neurology Multicenter Collaboration. Stroke 2021, 52, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Sakakura, K.; Jinnouchi, H.; Taniguchi, Y.; Tsukui, T.; Watanabe, Y.; Yamamoto, K.; Seguchi, M.; Wada, H.; Fujita, H. Comparison of door-to-balloon time and in-hospital outcomes in patients with ST-elevation myocardial infarction between before versus after COVID-19 pandemic. Cardiovasc. Interv. Ther. 2022, 37, 641–650. [Google Scholar] [CrossRef]
- Gu, S.; Li, J.; Shen, H.; Dai, Z.; Bai, Y.; Zhang, S.; Zhao, H.; Zhou, S.; Yu, Y.; Tang, W. The impact of COVID-19 pandemic on treatment delay and short-term neurological functional prognosis for acute ischemic stroke during the lockdown period. Front. Neurol. 2022, 13, 998758. [Google Scholar] [CrossRef]
- Ikeme, S.; Kottenmeier, E.; Uzochukwu, G.; Brinjikji, W. Evidence-Based Disparities in Stroke Care Metrics and Outcomes in the United States: A Systematic Review. Stroke 2022, 53, 670–679. [Google Scholar] [CrossRef]
- de Havenon, A.; Zhou, L.W.; Johnston, K.C.; Dangayach, N.S.; Ney, J.; Yaghi, S.; Sharma, R.; Abbasi, M.; Delic, A.; Majersik, J.J.; et al. Twenty-Year Disparity Trends in United States Stroke Death Rate by Age, Race/Ethnicity, Geography, and Socioeconomic Status. Neurology 2023, 101, e464–e474. [Google Scholar] [CrossRef]
- Chugh, C. Acute Ischemic Stroke: Management Approach. Indian. J. Crit. Care Med. 2019, 23, S140–S146. [Google Scholar] [CrossRef]
- Jacobs, B.S.; Birbeck, G.; Mullard, A.J.; Hickenbottom, S.; Kothari, R.; Roberts, S.; Reeves, M.J. Quality of hospital care in African American and white patients with ischemic stroke and TIA. Neurology 2006, 66, 809–814. [Google Scholar] [CrossRef]
- Price, S. Help Wanted: Texas’ Physician Growth Strong, But Recruitment, Diversity still Needed. Available online: www.texmed.org/Template.aspx?id=60809 (accessed on 11 January 2025).
- Eissa, A.; Krass, I.; Bajorek, B.V. Optimizing the management of acute ischaemic stroke: A review of the utilization of intravenous recombinant tissue plasminogen activator (tPA). J. Clin. Pharm. Ther. 2012, 37, 620–629. [Google Scholar] [CrossRef] [PubMed]
- Addo, J.; Ayerbe, L.; Mohan, K.M.; Crichton, S.; Sheldenkar, A.; Chen, R.; Wolfe, C.D.; McKevitt, C. Socioeconomic status and stroke: An updated review. Stroke 2012, 43, 1186–1191. [Google Scholar] [CrossRef]
- Marshall, I.J.; Wang, Y.; Crichton, S.; McKevitt, C.; Rudd, A.G.; Wolfe, C.D. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 2015, 14, 1206–1218. [Google Scholar] [CrossRef] [PubMed]
- Lachkhem, Y.; Rican, S.; Minvielle, É. Understanding delays in acute stroke care: A systematic review of reviews. Eur. J. Public. Health 2018, 28, 426–433. [Google Scholar] [CrossRef]
- Al Shamsi, H.; Almutairi, A.G.; Al Mashrafi, S.; Al Kalbani, T. Implications of Language Barriers for Healthcare: A Systematic Review. Oman Med. J. 2020, 35, e122. [Google Scholar] [CrossRef]
- Clark, J.R.; Shlobin, N.A.; Batra, A.; Liotta, E.M. The Relationship Between Limited English Proficiency and Outcomes in Stroke Prevention, Management, and Rehabilitation: A Systematic Review. Front. Neurol. 2022, 13, 790553. [Google Scholar] [CrossRef]
- Attenello, F.J.; Adamczyk, P.; Wen, G.; He, S.; Zhang, K.; Russin, J.J.; Sanossian, N.; Amar, A.P.; Mack, W.J. Racial and socioeconomic disparities in access to mechanical revascularization procedures for acute ischemic stroke. J. Stroke Cerebrovasc. Dis. 2014, 23, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Buus, S.; Schmitz, M.L.; Cordsen, P.; Johnsen, S.P.; Andersen, G.; Simonsen, C.Z. Socioeconomic Inequalities in Reperfusion Therapy for Acute Ischemic Stroke. Stroke 2022, 53, 2307–2316. [Google Scholar] [CrossRef]
- Scheppers, E.; van Dongen, E.; Dekker, J.; Geertzen, J.; Dekker, J. Potential barriers to the use of health services among ethnic minorities: A review. Fam. Pract. 2006, 23, 325–348. [Google Scholar] [CrossRef]
- Flores, G. The impact of medical interpreter services on the quality of health care: A systematic review. Med. Care Res. Rev. 2005, 62, 255–299. [Google Scholar] [CrossRef]
- Jasne, A.S.; Chojecka, P.; Maran, I.; Mageid, R.; Eldokmak, M.; Zhang, Q.; Nystrom, K.; Vlieks, K.; Askenase, M.; Petersen, N.; et al. Stroke Code Presentations, Interventions, and Outcomes Before and During the COVID-19 Pandemic. Stroke 2020, 51, 2664–2673. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Nguyen, T.N.; Wellington, J.; Mofatteh, M.; Yao, W.; Hu, Z.; Kuang, Q.; Wu, W.; Wang, X.; Sun, Y.; et al. Shortening Door-to-Needle Time by Multidisciplinary Collaboration and Workflow Optimization During the COVID-19 Pandemic. J. Stroke Cerebrovasc. Dis. 2022, 31, 106179. [Google Scholar] [CrossRef] [PubMed]
- Banfield, W.H.; Elghawy, O.; Dewanjee, A.; Brady, W.J. Impact of COVID-19 on emergency department management of stroke and STEMI. A narrative review. Am. J. Emerg. Med. 2022, 57, 91–97. [Google Scholar] [CrossRef]
- Camporesi, J.; Strumia, S.; Di Pilla, A.; Paolucci, M.; Orsini, D.; Assorgi, C.; Cacciuttolo, M.G.; Specchia, M.L. Stroke pathway performance assessment: A retrospective observational study. BMC Health Serv. Res. 2023, 23, 1391. [Google Scholar] [CrossRef]
- Rivera, R.; Amudio, C.; Cruz, J.P.; Brunetti, E.; Catalan, P.; Sordo, J.G.; Echeverria, D.; Badilla, L.; Chamorro, A.; Gonzalez, C.; et al. The impact of a two-year long COVID-19 public health restriction program on mechanical thrombectomy outcomes in a stroke network. J. Stroke Cerebrovasc. Dis. 2023, 32, 107138. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, G.; Zhu, Y.; Song, H.; Ren, Y.; Liu, Y.; Ma, Q. Impact of the COVID-19 pandemic on emergent stroke care in Beijing, China. Sci. Rep. 2023, 13, 4429. [Google Scholar] [CrossRef]
- Rose, D.Z.; Registry, F.S.; Wang, K.; Gardener, H.; Gutierrez, C.M.; Koch, S.; Dong, C.; Foster, D.; Jameson, A.; Rundek, T.; et al. Abstract WP26: Covid Pandemic Versus Pre-pandemic Care of Stroke Patients within the Florida Stroke Registry. Stroke 2022, 53, AWP26. [Google Scholar] [CrossRef]
- Srivastava, P.K.; Zhang, S.; Xian, Y.; Xu, H.; Rutan, C.; Alger, H.M.; Walchok, J.G.; Williams, J.H.; de Lemos, J.A.; Decker-Palmer, M.R.; et al. Treatment and Outcomes of Patients with Ischemic Stroke During COVID-19: An Analysis from Get with The Guidelines-Stroke. Stroke 2021, 52, 3225–3232. [Google Scholar] [CrossRef]
- Katsanos, A.H.; de Sa Boasquevisque, D.; Al-Qarni, M.A.; Shawawrah, M.; McNicoll-Whiteman, R.; Gould, L.; Van Adel, B.; Sahlas, D.J.; Ng, K.K.H.; Perera, K.; et al. In-Hospital Delays for Acute Stroke Treatment Delivery during the COVID-19 Pandemic. Can. J. Neurol. Sci. 2021, 48, 59–65. [Google Scholar] [CrossRef]
- Hu, Q.; Hu, Y.; Gu, Y.; Song, X.; Shen, Y.; Lu, H.; Zhang, L.; Liu, P.; Wang, G.; Guo, C.; et al. Impact of the COVID-19 pandemic on acute stroke care: An analysis of the 24-month data from a comprehensive stroke center in Shanghai, China. CNS Neurosci. Ther. 2023, 29, 1898–1906. [Google Scholar] [CrossRef]
- Chou, E.; Hsieh, Y.L.; Wolfshohl, J.; Green, F.; Bhakta, T. Onsite telemedicine strategy for coronavirus (COVID-19) screening to limit exposure in ED. Emerg. Med. J. 2020, 37, 335–337. [Google Scholar] [CrossRef] [PubMed]
- Larremore, D.B.; Wilder, B.; Lester, E.; Shehata, S.; Burke, J.M.; Hay, J.A.; Tambe, M.; Mina, M.J.; Parker, R. Test sensitivity is secondary to frequency and turnaround time for COVID-19 screening. Sci. Adv. 2021, 7, abd5393. [Google Scholar] [CrossRef] [PubMed]
- Fessell, D.; Cherniss, C. Coronavirus Disease 2019 (COVID-19) and Beyond: Micropractices for Burnout Prevention and Emotional Wellness. J. Am. Coll. Radiol. 2020, 17, 746–748. [Google Scholar] [CrossRef]
- Carragher, D.J.; Hancock, P.J.B. Surgical face masks impair human face matching performance for familiar and unfamiliar faces. Cogn. Res. Princ. Implic. 2020, 5, 59. [Google Scholar] [CrossRef] [PubMed]
- Freud, E.; Stajduhar, A.; Rosenbaum, R.S.; Avidan, G.; Ganel, T. The COVID-19 pandemic masks the way people perceive faces. Sci. Rep. 2020, 10, 22344. [Google Scholar] [CrossRef]
- Pavlova, M.A.; Sokolov, A.A. Reading Covered Faces. Cereb. Cortex 2022, 32, 249–265. [Google Scholar] [CrossRef]
- Díaz-Agea, J.L.; Orcajada-Muñoz, I.; Leal-Costa, C.; Adánez-Martínez, M.G.; De Souza Oliveira, A.C.; Rojo-Rojo, A. How Did the Pandemic Affect Communication in Clinical Settings? A Qualitative Study with Critical and Emergency Care Nurses. Healthcare 2022, 10, 373. [Google Scholar] [CrossRef]
- Lasalvia, A.; Amaddeo, F.; Porru, S.; Carta, A.; Tardivo, S.; Bovo, C.; Ruggeri, M.; Bonetto, C. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: A cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open 2021, 11, e045127. [Google Scholar] [CrossRef]
- Petrino, R.; Riesgo, L.G.; Yilmaz, B. Burnout in emergency medicine professionals after 2 years of the COVID-19 pandemic: A threat to the healthcare system? Eur. J. Emerg. Med. 2022, 29, 279–284. [Google Scholar] [CrossRef]
- Griffin, G.; Krizo, J.; Mangira, C.; Simon, E.L. The impact of COVID-19 on emergency department boarding and in-hospital mortality. Am. J. Emerg. Med. 2023, 67, 5–9. [Google Scholar] [CrossRef]
- Kilaru, A.S.; Scheulen, J.J.; Harbertson, C.A.; Gonzales, R.; Mondal, A.; Agarwal, A.K. Boarding in US Academic Emergency Departments During the COVID-19 Pandemic. Ann. Emerg. Med. 2023, 82, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Reznek, M.A.; Murray, E.; Youngren, M.N.; Durham, N.T.; Michael, S.S. Door-to-Imaging Time for Acute Stroke Patients Is Adversely Affected by Emergency Department Crowding. Stroke 2017, 48, 49–54. [Google Scholar] [CrossRef]
- Tsai, M.T.; Yen, Y.L.; Su, C.M.; Hung, C.W.; Kung, C.T.; Wu, K.H.; Cheng, H.H. The influence of emergency department crowding on the efficiency of care for acute stroke patients. Int. J. Qual. Health Care 2016, 28, 774–778. [Google Scholar] [CrossRef] [PubMed]
- Yeo, I.H.; Kim, Y.J.; Kim, J.K.; Lee, D.E.; Choe, J.Y.; Kim, C.H.; Park, J.B.; Seo, K.S.; Park, S.Y.; Lee, S.H.; et al. Impact of the COVID-19 Pandemic on Emergency Department Workload and Emergency Care Workers’ Psychosocial Stress in the Outbreak Area. Medicina 2021, 57, 1274. [Google Scholar] [CrossRef] [PubMed]
- Khanal, P.; Devkota, N.; Dahal, M.; Paudel, K.; Joshi, D. Mental health impacts among health workers during COVID-19 in a low resource setting: A cross-sectional survey from Nepal. Global Health 2020, 16, 89. [Google Scholar] [CrossRef]
- Kim, J.H.; Yoon, J.; Kim, S.J.; Kim, J.Y.; Bahk, J.; Kim, S.S. Lack of compensation for COVID-19-related overtime work and its association with burnout among EMS providers in Korea. Epidemiol. Health 2023, 45, e2023058. [Google Scholar] [CrossRef]
- Pourmand, A.; Caggiula, A.; Barnett, J.; Ghassemi, M.; Shesser, R. Rethinking Traditional Emergency Department Care Models in a Post-Coronavirus Disease-2019 World. J. Emerg. Nurs. 2023, 49, 520–529.e2. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).