Relationship between Cardiovascular Risk Factors and Composite Cardiovascular Outcomes in Patients Hospitalized with Takotsubo Syndrome: A Nationwide Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Extraction and Study Population
2.2. Outcomes and Data Synthesis
2.3. Statistical Analysis
3. Results
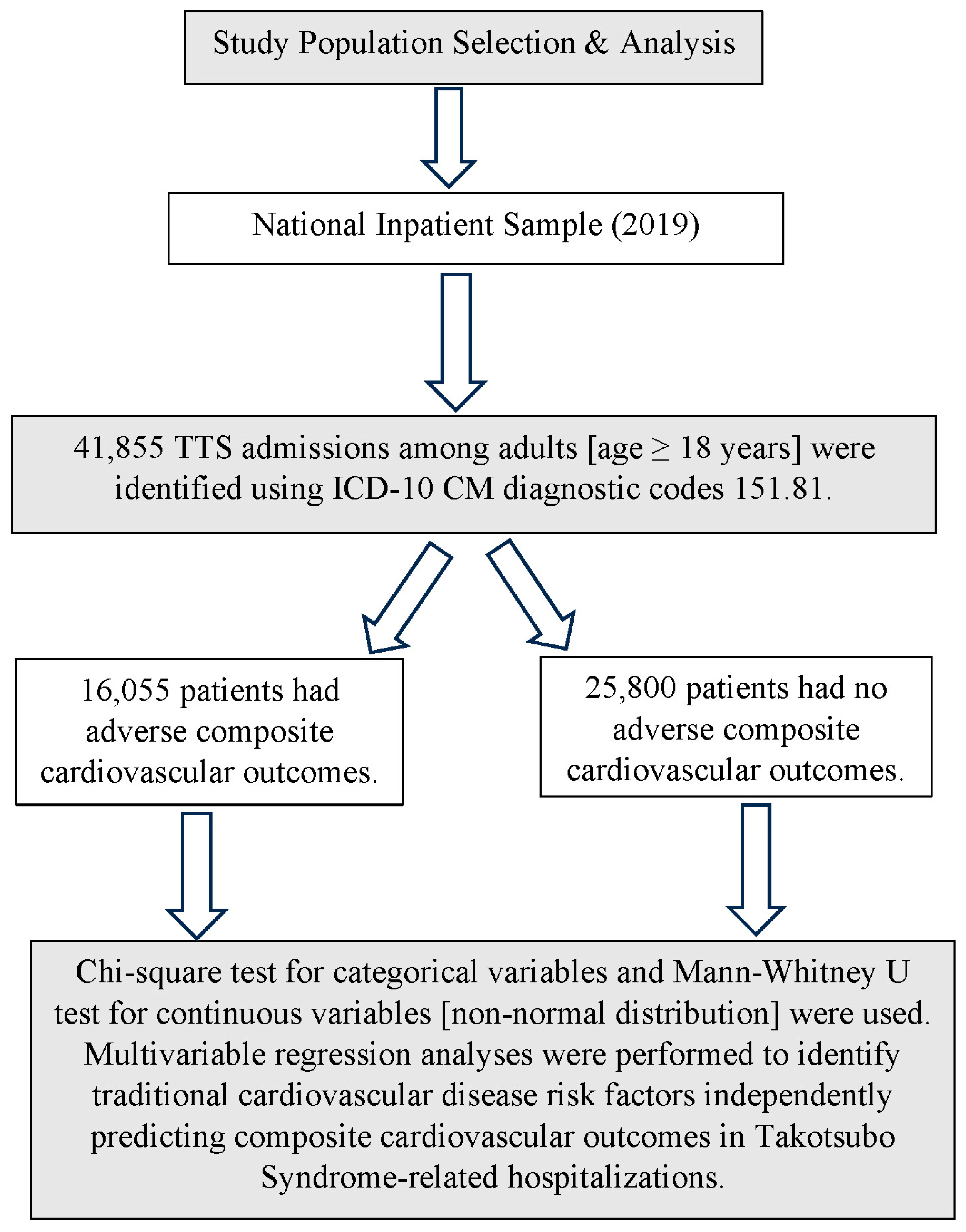
3.1. Study Selection
3.2. Baseline Characteristics
3.3. CVD Risk Factors and Their Effect on Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ghadri, J.-R.; Wittstein, I.S.; Prasad, A.; Sharkey, S.; Dote, K.; Akashi, Y.J.; Cammann, V.L.; Crea, F.; Galiuto, L.; Desmet, W.; et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur. Heart J. 2018, 39, 2032–2046. [Google Scholar] [CrossRef] [PubMed]
- Khera, R.; Light-McGroary, K.; Zahr, F.; Horwitz, P.A.; Girotra, S. Trends in hospitalization for takotsubo cardiomyopathy in the United States. Am. Heart J. 2016, 172, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.; Ram, P.; Lo, K.B.U.; Sirinvaravong, N.; Patel, B.; Tripathi, B.; Patil, S.; Figueredo, V.M. Etiologies, predictors, and economic impact of readmission within 1 month among patients with takotsubo cardiomyopathy. Clin. Cardiol. 2018, 41, 916–923. [Google Scholar] [CrossRef]
- Singh, S.; Desai, R.; Gandhi, Z.; Fong, H.K.; Doreswamy, S.; Desai, V.; Chockalingam, A.; Mehta, P.K.; Sachdeva, R.; Kumar, G. Takotsubo Syndrome in Patients with COVID-19: A Systematic Review of Published Cases. SN Compr. Clin. Med. 2020, 2, 2102–2108. [Google Scholar] [CrossRef]
- Jabri, A.; Kalra, A.; Kumar, A.; Alameh, A.; Adroja, S.; Bashir, H.; Nowacki, A.S.; Shah, R.; Khubber, S.; Kanaa’n, A.; et al. Incidence of Stress Cardiomyopathy during the Coronavirus Disease 2019 Pandemic. JAMA Netw. Open 2020, 3, e2014780. [Google Scholar] [CrossRef]
- Ahmed, S.K.; Mohamed, M.G.; Essa, R.A.; Dabou, E.A.A.R.; Abdulqadir, S.O.; Omar, R.M. Global reports of takotsubo (stress) cardiomyopathy following COVID-19 vaccination: A systematic review and meta-analysis. Int. J. Cardiol. Heart Vasc. 2022, 43, 101108. [Google Scholar]
- Pelliccia, F.; Parodi, G.; Greco, C.; Antoniucci, D.; Brenner, R.; Bossone, E.; Cacciotti, L.; Capucci, A.; Citro, R.; Delmas, C.; et al. Comorbidities Frequency in Takotsubo Syndrome: An International Collaborative Systematic Review Including 1109 Patients. Am. J. Med. 2015, 128, 654.e11–654.e19. [Google Scholar] [CrossRef]
- Elesber, A.A.; Prasad, A.; Lennon, R.J.; Wright, R.S.; Lerman, A.; Rihal, C.S. Four-Year Recurrence Rate and Prognosis of the Apical Ballooning Syndrome. J. Am. Coll. Cardiol. 2007, 50, 448–452. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.-H.; Chu, C.-S.; Lin, T.-H.; Lee, K.-T.; Sheu, S.-H.; Lai, W.-T. Lipid Paradox in Acute Myocardial Infarction—The Association with 30-Day In-Hospital Mortality. Crit. Care Med. 2015, 43, 1255–1264. [Google Scholar] [CrossRef]
- Patel, U.; Desai, R.; Faisaluddin, M.; Fong, H.K.; Singh, S.; Patel, S.; Kumar, G.; Sachdeva, R. Prevalence and impact of takotsubo syndrome in hospitalizations for acute ischemic stroke. Bayl. Univ. Med. Cent. Proc. 2021, 35, 156–161. [Google Scholar] [CrossRef]
- Santoro, F.; Ieva, R.; Musaico, F.; Ferraretti, A.; Triggiani, G.; Tarantino, N.; Di Biase, M.; Brunetti, N.D. Lack of Efficacy of Drug Therapy in Preventing Takotsubo Cardiomyopathy Recurrence: A Meta-analysis. Clin. Cardiol. 2014, 37, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, A.; Kumar, G.; Pant, S.; Rihal, C.; Murugiah, K.; Mehta, J.L. Prevalence of Takotsubo cardiomyopathy in the United States. Am. Heart J. 2012, 164, 66–71. [Google Scholar] [CrossRef] [PubMed]
- El-Battrawy, I.; Santoro, F.; Stiermaier, T.; Möller, C.; Guastafierro, F.; Novo, G.; Novo, S.; Mariano, E.; Romeo, F.; Romeo, F.; et al. Incidence and Clinical Impact of Recurrent Takotsubo Syndrome: Results from the GEIST Registry. J. Am. Heart Assoc. 2019, 8, e010753. [Google Scholar] [CrossRef]
- Madias, J.E. Low prevalence of diabetes mellitus in patients with Takotsubo syndrome: A plausible ‘protective’ effect with pathophysiologic connotations. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Stiermaier, T.; Santoro, F.; El-Battrawy, I.; Möller, C.; Graf, T.; Novo, G.; Santangelo, A.; Mariano, E.; Romeo, F.; Caldarola, P.; et al. Prevalence and Prognostic Impact of Diabetes in Takotsubo Syndrome: Insights from the International, Multicenter GEIST Registry. Diabetes Care 2018, 41, 1084–1088. [Google Scholar] [CrossRef] [PubMed]
- Zalewska-Adamiec, M.; Bachorzewska-Gajewska, H.; Tomaszuk-Kazberuk, A.; Nowak, K.; Drozdowski, P.; Bychowski, J.; Krynicki, R.; Musial, W.J.; Dobrzycki, S. Takotsubo cardiomyopathy: Serious early complications and two-year mortality—A 101 case study. Neth. Heart J. 2016, 24, 511–519. [Google Scholar] [CrossRef]
- Yerasi, C.; Tripathi, B.; Banga, S.; McNown, C.; Jonnalagadda, A.K.; Al-Qaisi, S.; Miryala, V.; Nafisi, S.; Waksman, R.; Ben-Dor, I. Predictors of 90-Day Readmission and in-Hospital Mortality in Takotsubo Cardiomyopathy: An Analysis of 28,079 Index Admissions. Cardiovasc. Revasc. Med. 2019, 20, 973–979. [Google Scholar] [CrossRef]
- Ahuja, K.R.; Nazir, S.; Jain, V.; Isogai, T.; Saad, A.M.; Verma, B.R.; Shekhar, S.; Kumar, R.; Eltahawy, E.A.; Madias, J.E. Takotsubo syndrome: Does “Diabetes Paradox” exist? Heart Lung 2021, 50, 316–322. [Google Scholar] [CrossRef]
- Syed, M.; Osman, M.; Alharbi, A.; Khan, M.U.; Munir, M.B.; Balla, S. Comparison of Outcomes in Patients with Takotsubo Syndrome With-vs-Without Cardiogenic Shock. Am. J. Cardiol. 2020, 136, 24–31. [Google Scholar] [CrossRef]
- Madias, J.E. “Obesity paradox” and takotsubo syndrome. Int. J. Cardiol. Cardiovasc. Risk Prev. 2022, 15, 200152. [Google Scholar] [CrossRef]
- Dias, A.; Franco, E.; Rubio, M.; Koshkelashvili, N.; Bhalla, V.; Amanullah, S.; Hebert, K.; Figueredo, V.M. Takotsubo Syndrome: Does it matter if you have diabetes mellitus? Int. J. Cardiol. 2016, 224, 398–399. [Google Scholar] [CrossRef]
- Dias, A. Incidence and predictors of stroke during the index event in an ethnically diverse Takotsubo cardiomyopathy population. Funct. Neurol. 2016, 31, 157–162. [Google Scholar] [CrossRef]
- Li, P.; Lu, X.; Teng, C.; Hadley, M.; Cai, P.; Dai, Q.; Wang, B. The Association between Hyperlipidemia and In-Hospital Outcomes in Takotsubo Cardiomyopathy. Diabetes Metab. Syndr. Obes. Targets Ther. 2021, 14, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Van Lenten, B.J.; Fogelman, A.M.; Haberland, M.E.; Edwards, P.A. The role of lipoproteins and receptor-mediated endocytosis in the transport of bacterial lipopolysaccharide. Proc. Natl. Acad. Sci. USA 1986, 83, 2704–2708. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.S.; Dillon, C.F.; Carroll, M.; Illoh, K.; Ostchega, Y. Effects of Statins on Serum Inflammatory Markers: The U.S. National Health and Nutrition Examination Survey 1999–2004. J. Atheroscler. Thromb. 2010, 17, 1176–1182. [Google Scholar] [CrossRef]
- Santoro, F.; Tarantino, N.; Ferraretti, A.; Ieva, R.; Musaico, F.; Guastafierro, F.; Di Martino, L.; Di Biase, M.; Brunetti, N.D. Serum interleukin 6 and 10 levels in Takotsubo cardiomyopathy: Increased admission levels may predict adverse events at follow-up. Atherosclerosis 2016, 254, 28–34. [Google Scholar] [CrossRef]
- Horwich, T.B.; Hamilton, M.A.; MacLellan, W.; Fonarow, G.C. Low serum total cholesterol is associated with marked increase in mortality in advanced heart failure. J. Card. Fail. 2002, 8, 216–224. [Google Scholar] [CrossRef]
- Desai, R.; Edusa, S.; Reyaz, N.; Venkata, V.S.; Puli, S.; Jain, A. Seasonal variation in in-hospital outcomes of Takotsubo-syndrome-related admissions: A National Inpatient Analysis, 2019. Int. J. Cardiol. Cardiovasc. Risk Prev. 2023, 16, 200164. [Google Scholar] [CrossRef] [PubMed]
- Kanaoka, K.; Okayama, S.; Terasaki, S.; Nakano, T.; Ishii, M.; Nakai, M.; Onoue, K.; Nishimura, K.; Yasuda, S.; Tsujita, K.; et al. Role of climatic factors in the incidence of Takotsubo syndrome: A nationwide study from 2012 to 2016. ESC Heart Fail. 2020, 7, 2629–2636. [Google Scholar] [CrossRef]
| Variable | TTS with Composite Outcomes | p-Value | ||
|---|---|---|---|---|
| No (n = 25,800) | Yes (n = 16,055) | |||
| Admission Age (years) | Median [IQR] | 67 (58–76) | 72 (61–80) | <0.001 |
| Sex n (%) | Male | 3830 (14.8) | 3650 (22.7) | <0.001 |
| Female | 21,970 (85.2) | 12,405 (77.3) | <0.001 | |
| Race n (%) | White | 20,240 (78.44) | 12,705 (79.1) | <0.001 |
| Black | 2125 (8.3) | 1170 (7.3) | <0.001 | |
| Hispanic | 1670 (6.5) | 930 (5.8) | <0.001 | |
| Asian or Pacific Islander | 490 (1.9) | 335 (2.1) | <0.001 | |
| Native American | 130 (0.5) | 120 (0.8) | <0.001 | |
| Median Household Income National Quartile for Patient ZIP Code n (%) | 0–25th | 6560 (25.9) | 3840 (24.3) | <0.001 |
| 26–50th | 6615 (26.1) | 3940 (24.9) | <0.001 | |
| 51–75th | 6740 (26.6) | 4265 (27.0) | <0.001 | |
| 76–100th | 5445 (21.5) | 3775 (23.9) | <0.001 | |
| Primary Expected Payer n (%) | Medicare | 15,720 (61.0) | 10,850 (67.6) | <0.001 |
| Medicaid | 2850 (11.1) | 1415 (8.8) | <0.001 | |
| Private including HMO | 5820 (22.6) | 3045 (19.0) | <0.001 | |
| Self-Pay | 810 (3.1) | 355 (2.2) | <0.001 | |
| No Charges | 25 (0.1) | 325 (2.0) | <0.001 | |
| Comorbidities n (%) | Hypertension | 16,520 (64.0) | 9915 (61.8) | <0.001 |
| Diabetes | 5730 (22.2) | 3800 (23.7) | 0.001 | |
| Hyperlipidemia | 12,540 (48.6) | 6965 (43.4) | <0.001 | |
| Obesity | 3015 (11.7) | 1870 (11.6) | 0.905 | |
| Peripheral vascular disease | 2230 (8.6) | 1935 (12.1) | <0.001 | |
| Prior myocardial infarction | 3060 (11.9) | 1670 (10.4) | <0.001 | |
| Prior PCI | 95 (0.4) | 65 (0.4) | 0.555 | |
| Prior CABG | 1155 (4.5) | 785 (4.9) | 0.051 | |
| Tobacco use disorder | 5115 (19.8) | 2453 (15.2) | <0.001 | |
| Drug Abuse | 1515 (5.9) | 785 (4.9) | <0.001 | |
| Alcohol Abuse | 1560 (6.0) | 860 (5.4) | 0.003 | |
| Disposition of patient n (%) | Routine | 16,370 (63.4) | 5665 (35.3) | <0.001 |
| Transfer to short-term hospital | 580 (2.2) | 490 (3.1) | <0.001 | |
| Other transfers including SNF, ICF | 4525 (17.5) | 4280 (26.7) | <0.001 | |
| Home healthcare | 4005 (15.5) | 2750 (17.1) | <0.001 | |
| Length of Hospital stay (days) | Median [IQR] | 3 (2–6) | 6 (3–11) | <0.001 |
| Total charges (USD) | Median [IQR] | 44,966 (28,306–80,076) | 78,309 (41,253–165,892) | <0.001 |
| Risk Factor | Odds Ratio | 95 Confidence Interval | p-Value | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Hypertension, complicated | Yes vs. No | 1.14 | 1.02 | 1.29 | 0.027 |
| Hypertension, uncomplicated | Yes vs. No | 0.65 | 0.58 | 0.73 | <0.001 |
| Diabetes with complications | Yes vs. No | 1.18 | 1.02 | 1.36 | 0.027 |
| Diabetes w/o complications | Yes vs. No | 0.87 | 0.73 | 1.04 | 0.117 |
| Hyperlipidemia | Yes vs. No | 0.76 | 0.68 | 0.83 | <0.001 |
| Obesity | Yes vs. No | 1.14 | 0.98 | 1.32 | 0.089 |
| Tobacco Use Disorder | Yes vs. No | 0.84 | 0.74 | 0.96 | 0.012 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Damarlapally, N.; Desai, R.; Sawhney, A.; Verma, J.; Singh Klair, H.; Kolli, D.; Singh Sibia, B.; Chalasani, V.; Reddy, R.; Kolli, J.; et al. Relationship between Cardiovascular Risk Factors and Composite Cardiovascular Outcomes in Patients Hospitalized with Takotsubo Syndrome: A Nationwide Analysis. Med. Sci. 2023, 11, 62. https://doi.org/10.3390/medsci11030062
Damarlapally N, Desai R, Sawhney A, Verma J, Singh Klair H, Kolli D, Singh Sibia B, Chalasani V, Reddy R, Kolli J, et al. Relationship between Cardiovascular Risk Factors and Composite Cardiovascular Outcomes in Patients Hospitalized with Takotsubo Syndrome: A Nationwide Analysis. Medical Sciences. 2023; 11(3):62. https://doi.org/10.3390/medsci11030062
Chicago/Turabian StyleDamarlapally, Nanush, Rupak Desai, Aanchal Sawhney, Jyoti Verma, Harroop Singh Klair, Dhanush Kolli, Birimroz Singh Sibia, Vardhan Chalasani, Rasya Reddy, Jithin Kolli, and et al. 2023. "Relationship between Cardiovascular Risk Factors and Composite Cardiovascular Outcomes in Patients Hospitalized with Takotsubo Syndrome: A Nationwide Analysis" Medical Sciences 11, no. 3: 62. https://doi.org/10.3390/medsci11030062
APA StyleDamarlapally, N., Desai, R., Sawhney, A., Verma, J., Singh Klair, H., Kolli, D., Singh Sibia, B., Chalasani, V., Reddy, R., Kolli, J., Ogbu, I., & Gummadi, J. (2023). Relationship between Cardiovascular Risk Factors and Composite Cardiovascular Outcomes in Patients Hospitalized with Takotsubo Syndrome: A Nationwide Analysis. Medical Sciences, 11(3), 62. https://doi.org/10.3390/medsci11030062






