Polyamine-Based Nanostructures Share Polyamine Transport Mechanisms with Native Polyamines and Their Analogues: Significance for Polyamine-Targeted Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Lines and Culture Conditions
2.2. Cell Viability Assays
2.3. Polyamine-Based Nanoparticle Synthesis
2.4. Analysis of Intracellular Native Polyamine Concentrations, Polyamine Analogue Concentrations and Catabolic Polyamine Enzyme Activity
2.5. DFMO Growth Curves and Nanopolyamine Co-Treatment
2.6. Polyamine Transport Inhibition
2.7. Statistical Analysis
3. Results
3.1. Polyamine Transport-Deficient Cells Are Resistant to Nanopolyamine and Polyamine Analogue-Induced Cytotoxicity
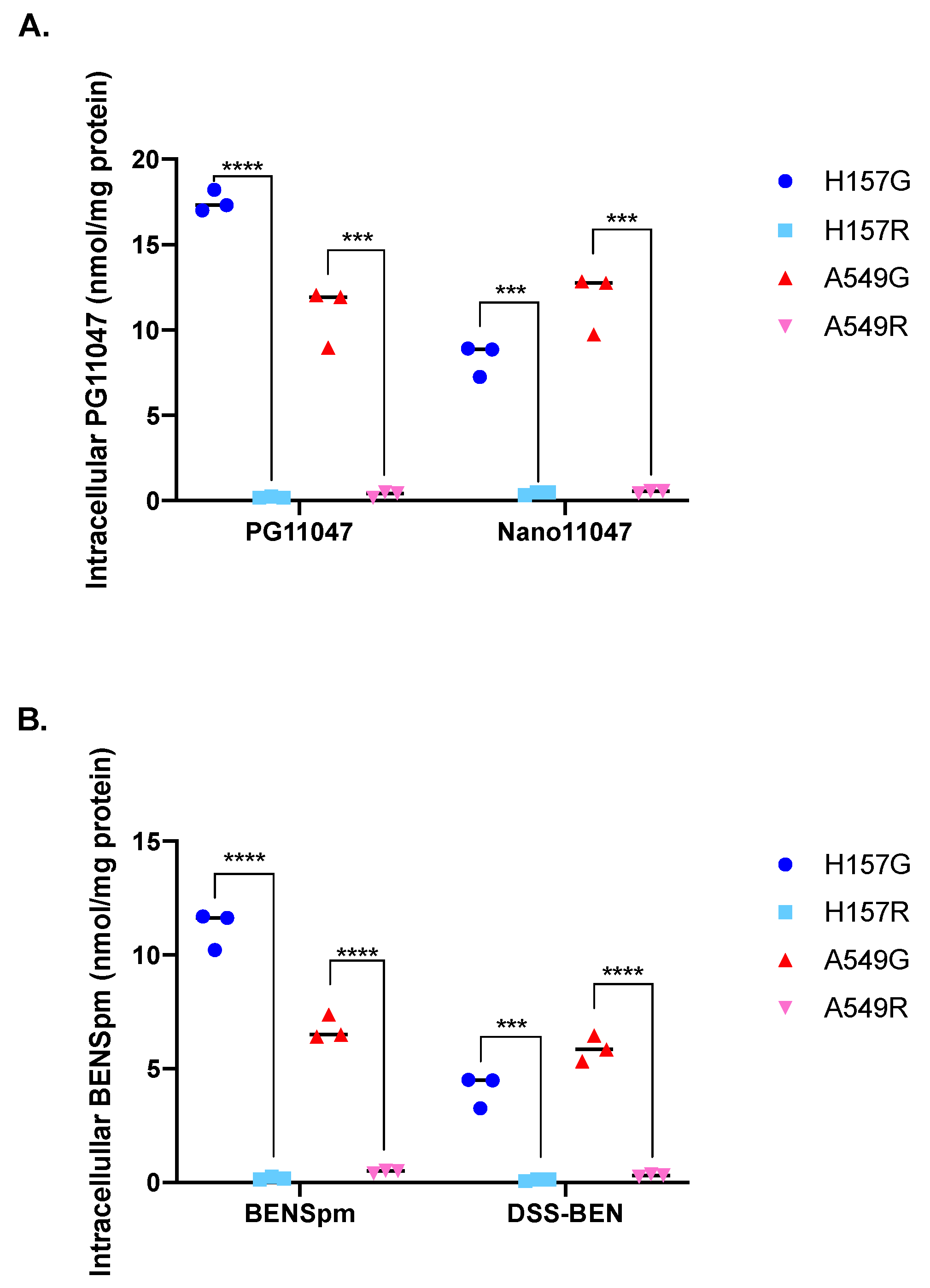
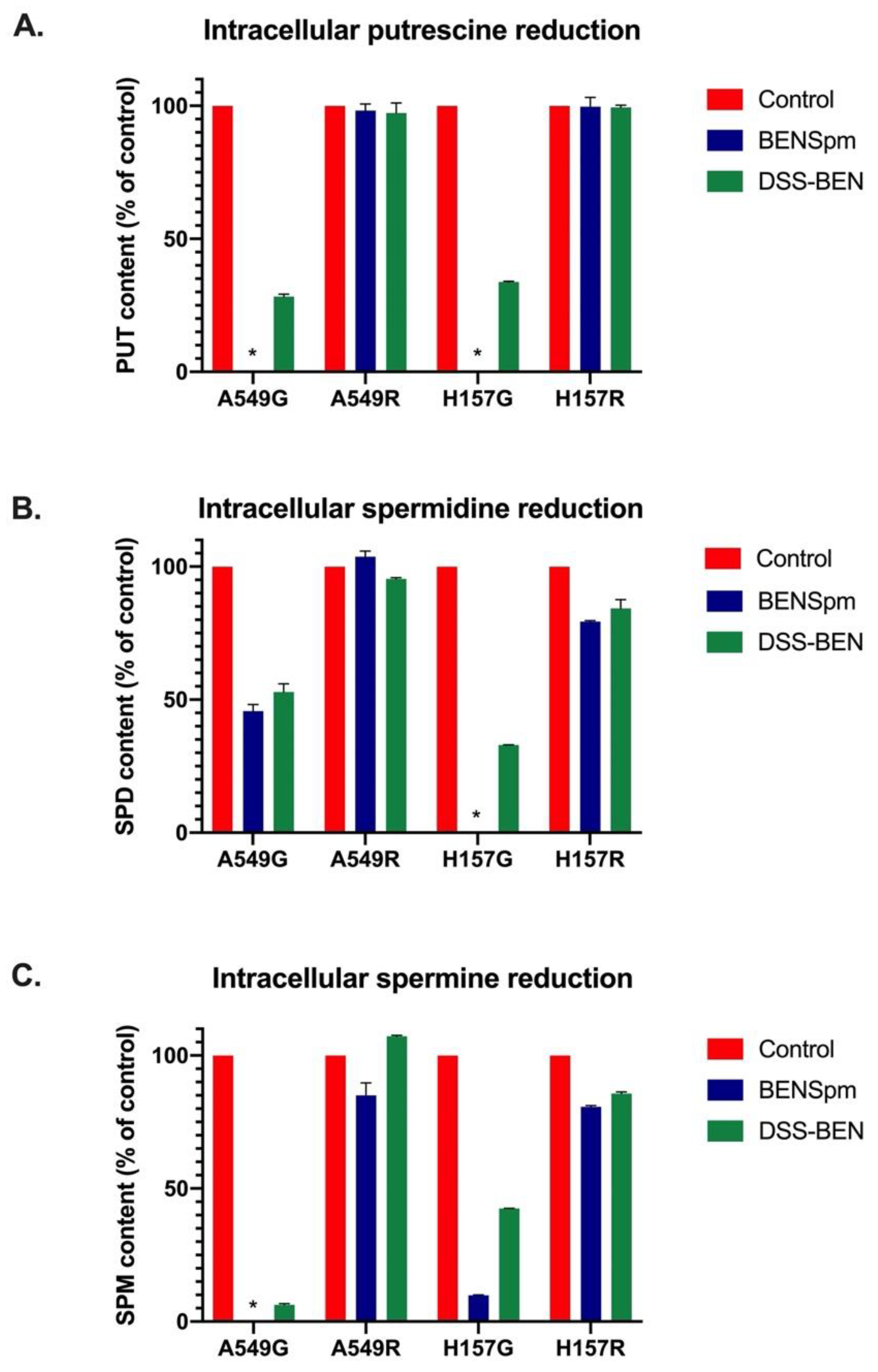
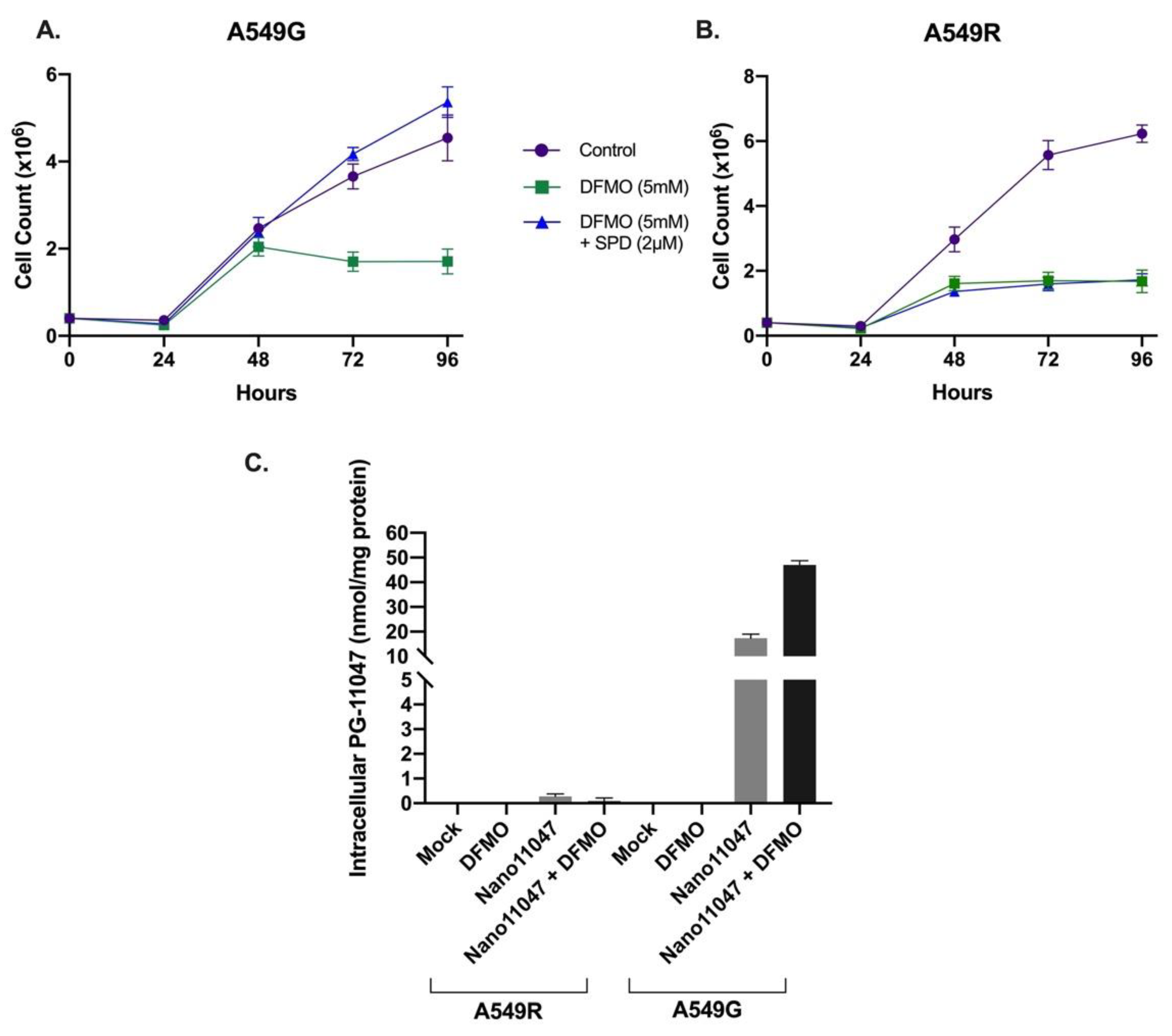
3.2. Polyamine Transport-Deficient Cells Are Unable to Accumulate Nanopolyamines or Their Parent Compounds
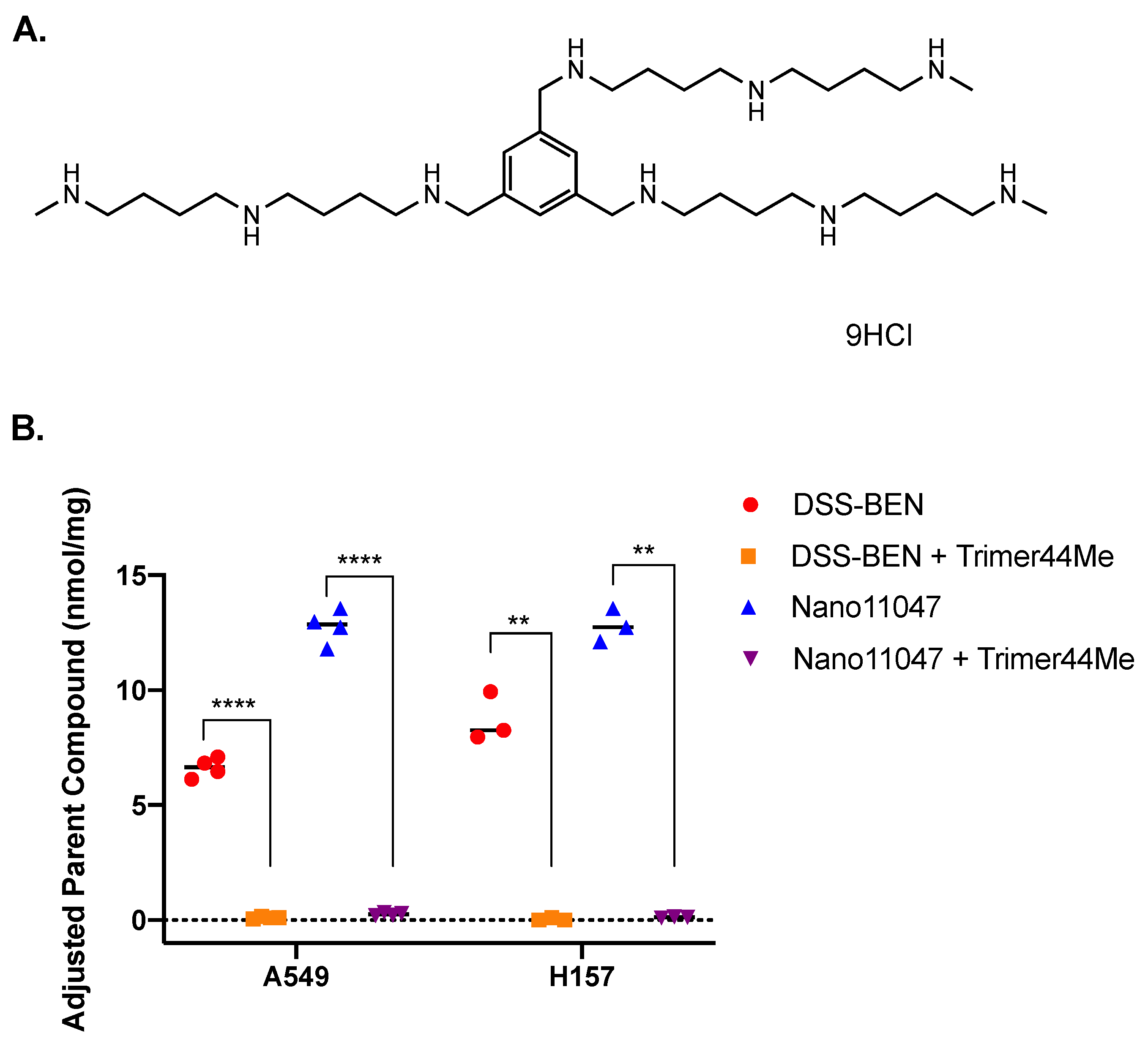
3.3. Effects of Polyamine Transport System Modulators on Uptake of Nanopolyamines
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pegg, A.E.; McCann, P.P. Polyamine metabolism and function. Am. J. Physiol.—Cell Physiol. 1982, 243, C212–C221. [Google Scholar] [CrossRef] [PubMed]
- Tabor, C.W.; Tabor, H. Polyamines in microorganisms. Microbiol. Rev. 1985, 49, 81–99. [Google Scholar] [CrossRef] [PubMed]
- Pegg, A.E. Polyamine metabolism and its importance in neoplastic growth and a target for chemotherapy. Cancer Res. 1988, 48, 759–774. [Google Scholar] [PubMed]
- Belting, M.; Mani, K.; Jönsson, M.; Cheng, F.; Sandgren, S.; Jonsson, S.; Ding, K.; Delcros, J.G.; Fransson, L.A. Glypican-1 is a vehicle for polyamine uptake in mammalian cells: A pivital role for nitrosothiol-derived nitric oxide. J. Biol. Chem. 2003, 278, 47181–47189. [Google Scholar] [CrossRef] [PubMed]
- Uemura, T.; Yerushalmi, H.F.; Tsaprailis, G.; Stringer, D.E.; Pastorian, K.E.; Hawel, L.; Byus, C.V.; Gerner, E.W. Identification and characterization of a diamine exporter in colon epithelial cells. J. Biol. Chem. 2008, 283, 26428–26435. [Google Scholar] [CrossRef] [PubMed]
- Soulet, D.; Gagnon, B.; Rivest, S.; Audette, M.; Poulin, R. A fluorescent probe of polyamine transport accumulates into intracellular acidic vesicles via a two-step mechanism. J. Biol. Chem. 2004, 279, 49355–49366. [Google Scholar] [CrossRef]
- Pegg, A.E. Mammalian polyamine metabolism and function. IUBMB Life 2009, 61, 880–894. [Google Scholar] [CrossRef]
- Uemura, T.; Stringer, D.E.; Blohm-Mangone, K.A.; Gerner, E.W. Polyamine transport is mediated by both endocytic and solute carrier transport mechanisms in the gastrointestinal tract. Am. J. Physiol.—Gastrointest. Liver Physiol. 2010, 299, G517–G522. [Google Scholar] [CrossRef]
- Roy, U.K.; Rial, N.S.; Kachel, K.L.; Gerner, E.W. Activated K-RAS increases polyamine uptake in human colon cancer cells through modulation of caveolar endocytosis. Mol. Carcinog 2008, 47, 538–553. [Google Scholar] [CrossRef]
- van Veen, S.; Martin, S.; Van den Haute, C.; Benoy, V.; Lyons, J.; Vanhoutte, R.; Kahler, J.P.; Decuypere, J.P.; Gelders, G.; Lambie, E.; et al. ATP13A2 deficiency disrupts lysosomal polyamine export. Nature 2020, 578, 419–424. [Google Scholar] [CrossRef]
- Sekhar, V.; Andl, T.; Phanstiel, O. ATP13A3 facilitates polyamine transport in human pancreatic cancer cells. Sci. Rep. 2022, 12, 4045. [Google Scholar] [CrossRef] [PubMed]
- Hamouda, N.N.; Van den Haute, C.; Vanhoutte, R.; Sannerud, R.; Azfar, M.; Mayer, R.; Cortés Calabuig, Á.; Swinnen, J.V.; Agostinis, P.; Baekelandt, V.; et al. ATP13A3 is a major component of the enigmatic mammalian polyamine transport system. J. Biol. Chem. 2021, 296, 100182. [Google Scholar] [CrossRef] [PubMed]
- Wallace, H.M.; Fraser, A.V. Inhibitors of polyamine metabolism: Review article. Amino Acids 2004, 26, 353–365. [Google Scholar] [CrossRef] [PubMed]
- Zahedi, K.; Barone, S.; Soleimani, M. Polyamines and Their Metabolism: From the Maintenance of Physiological Homeostasis to the Mediation of Disease. Med. Sci. 2022, 10, 38. [Google Scholar] [CrossRef]
- Nakanishi, S.; Cleveland, J.L. Polyamine Homeostasis in Development and Disease. Med. Sci. 2021, 9, 28. [Google Scholar] [CrossRef]
- Casero, R.A.; Murray Stewart, T.; Pegg, A.E. Polyamine metabolism and cancer: Treatments, challenges and opportunities. Nat. Rev. Cancer 2018, 18, 681–695. [Google Scholar] [CrossRef]
- Gerner, E.W.; Meyskens, F.L. Polyamines and cancer: Old molecules, new understanding. Nat. Rev. Cancer 2004, 4, 781–792. [Google Scholar] [CrossRef]
- Russell, D.; Snyder, S.H. Amine synthesis in rapidly growing tissues: Ornithine decarboxylase activity in regenerating rat liver, chick embryo, and various tumors. Proc. Natl. Acad. Sci. USA 1968, 60, 1420–1427. [Google Scholar] [CrossRef]
- Casero, R.A.; Woster, P.M. Terminally alkylated polyamine analogues as chemotherapeutic agents. J. Med. Chem. 2001, 44, 1–26. [Google Scholar] [CrossRef]
- Reddy, V.K.; Valasinas, A.; Sarkar, A.; Basu, H.S.; Marton, L.J.; Frydman, B. Conformationally restricted analogues of 1N,12N-bisethylspermine: Synthesis and growth inhibitory effects on human tumor cell lines. J. Med. Chem. 1998, 41, 4723–4732. [Google Scholar] [CrossRef]
- Hahm, H.A.; Ettinger, D.S.; Bowling, K.; Hoker, B.; Chen, T.L.; Zabelina, Y.; Casero, R.A. Phase I study of N(1),N(11)-diethylnorspermine in patients with non-small cell lung cancer. Clin. Cancer Res. 2002, 8, 684–690. [Google Scholar] [PubMed]
- Creaven, P.J.; Perez, R.; Pendyala, L.; Meropol, N.J.; Loewen, G.; Levine, E.; Berghorn, E.; Raghavan, D. Unusual central nervous system toxicity in a phase I study of N1N11 diethylnorspermine in patients with advanced malignancy. Investig. New Drugs 1997, 15, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Bergeron, R.J.; Müller, R.; Bussenius, J.; McManis, J.S.; Merriman, R.L.; Smith, R.E.; Yao, H.; Weimar, W.R. Synthesis and evaluation of hydroxylated polyamine analogues as antiproliferatives. J. Med. Chem. 2000, 43, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Holbert, C.E.; Foley, J.R.; Murray Stewart, T.; Casero, R.A. Expanded Potential of the Polyamine Analogue SBP-101 (Diethyl Dihydroxyhomospermine) as a Modulator of Polyamine Metabolism and Cancer Therapeutic. Int. J. Mol. Sci. 2022, 23, 6798. [Google Scholar] [CrossRef]
- Tebbutt, N.C.; Kotasek, D.; Borad, M.J.; Borazanci, E.H.; Smith, S.L.; Shah, A.K.; Walker, M.J.; Cullen, M.T.; Gagnon, S. A phase 1 safety study of SBP-101, a polyamine metabolic inhibitor, for pancreatic ductal adenocarcinoma (PDA). J. Clin. Oncol. 2018, 36, e16231. [Google Scholar] [CrossRef]
- Therapeutics, P. A Randomized, Double-Blind, Placebo-Controlled Study of Nab-Paclitaxel and Gemcitabine with or without SBP-101 in Subjects Previously Untreated for Metastatic Pancreatic Ductal Adenocarcinoma. Updated February 24, 2022. Identifier: NCT05254171. Available online: https://clinicaltrials.gov/ct2/show/NCT05254171 (accessed on 15 May 2022).
- Therapeutics, P. Phase 1A/1B Dose Escalation and Expansion Study of SBP-101 in Combination with Nab-Paclitaxel and Gemcitabine in Subjects with Previously Untreated Metastatic Pancreatic Ductal Adenocarcinoma. Updated 25 May 2022. Identifier: NCT03412799. Available online: https://www.clinicaltrials.gov/ct2/show/NCT03412799 (accessed on 12 June 2022).
- Goyal, L.; Supko, J.G.; Berlin, J.; Blaszkowsky, L.S.; Carpenter, A.; Heuman, D.M.; Hilderbrand, S.L.; Stuart, K.E.; Cotler, S.; Senzer, N.N.; et al. Phase 1 study of N(1),N(11)-diethylnorspermine (DENSPM) in patients with advanced hepatocellular carcinoma. Cancer Chemother Pharm. 2013, 72, 1305–1314. [Google Scholar] [CrossRef]
- Streiff, R.R.; Bender, J.F. Phase 1 study of N1-N11-diethylnorspermine (DENSPM) administered TID for 6 days in patients with advanced malignancies. Investig. New Drugs 2001, 19, 29–39. [Google Scholar] [CrossRef]
- Murray Stewart, T.; Desai, A.A.; Fitzgerald, M.L.; Marton, L.J.; Casero, R.A. A phase I dose-escalation study of the polyamine analog PG-11047 in patients with advanced solid tumors. Cancer Chemother. Pharm. 2020, 85, 1089–1096. [Google Scholar] [CrossRef]
- Hacker, A.; Marton, L.J.; Sobolewski, M.; Casero, R.A. In vitro and in vivo effects of the conformationally restricted polyamine analogue CGC-11047 on small cell and non-small cell lung cancer cells. Cancer Chemother. Pharm. 2008, 63, 45–53. [Google Scholar] [CrossRef]
- Dredge, K.; Kink, J.A.; Johnson, R.M.; Bytheway, I.; Marton, L.J. The polyamine analog PG11047 potentiates the antitumor activity of cisplatin and bevacizumab in preclinical models of lung and prostate cancer. Cancer Chemother. Pharm. 2009, 65, 191–195. [Google Scholar] [CrossRef]
- Xie, Y.; Murray-Stewart, T.; Wang, Y.; Yu, F.; Li, J.; Marton, L.J.; Casero, R.A.; Oupický, D. Self-immolative nanoparticles for simultaneous delivery of microRNA and targeting of polyamine metabolism in combination cancer therapy. J. Control. Release 2017, 246, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Alexander, E.T.; Mariner, K.; Donnelly, J.; Phanstiel, O.; Gilmour, S.K. Polyamine Blocking Therapy Decreases Survival of Tumor-Infiltrating Immunosuppressive Myeloid Cells and Enhances the Antitumor Efficacy of PD-1 Blockade. Mol. Cancer Ther. 2020, 19, 2012–2022. [Google Scholar] [CrossRef] [PubMed]
- Gitto, S.B.; Pandey, V.; Oyer, J.L.; Copik, A.J.; Hogan, F.C.; Phanstiel, O.; Altomare, D.A. Difluoromethylornithine Combined with a Polyamine Transport Inhibitor Is Effective against Gemcitabine Resistant Pancreatic Cancer. Mol. Pharm. 2018, 15, 369–376. [Google Scholar] [CrossRef]
- Dong, Y.; Zhu, Y.; Li, J.; Zhou, Q.H.; Wu, C.; Oupický, D. Synthesis of bisethylnorspermine lipid prodrug as gene delivery vector targeting polyamine metabolism in breast cancer. Mol. Pharm. 2012, 9, 1654–1664. [Google Scholar] [CrossRef][Green Version]
- Zhu, Y.; Li, J.; Kanvinde, S.; Lin, Z.; Hazeldine, S.; Singh, R.K.; Oupický, D. Self-immolative polycations as gene delivery vectors and prodrugs targeting polyamine metabolism in cancer. Mol. Pharm. 2015, 12, 332–341. [Google Scholar] [CrossRef]
- Pramanik, A.; Laha, D.; Pramanik, P.; Karmakar, P. A novel drug “copper acetylacetonate” loaded in folic acid-tagged chitosan nanoparticle for efficient cancer cell targeting. J. Drug Target. 2014, 22, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Nelemans, L.C.; Gurevich, L. Drug Delivery with Polymeric Nanocarriers-Cellular Uptake Mechanisms. Materials 2020, 13, 366. [Google Scholar] [CrossRef]
- Shao, D.; Xiao, L.; Ha, H.C.; Casero, R.A. Isolation of a polyamine transport deficient cell line from the human non-small cell lung carcinoma line NCI H157. J. Cell Physiol. 1996, 166, 43–48. [Google Scholar] [CrossRef]
- Kabra, P.M.; Lee, H.K.; Lubich, W.P.; Marton, L.J. Solid-phase extraction and determination of dansyl derivatives of unconjugated and acetylated polyamines by reversed-phase liquid chromatography: Improved separation systems for polyamines in cerebrospinal fluid, urine and tissue. J. Chromatogr. 1986, 380, 19–32. [Google Scholar] [CrossRef]
- Holbert, C.E.; Dunworth, M.; Foley, J.R.; Dunston, T.T.; Stewart, T.M.; Casero, R.A. Autophagy induction by exogenous polyamines is an artifact of bovine serum amine oxidase activity in culture serum. J. Biol. Chem. 2020, 295, 9061–9068. [Google Scholar] [CrossRef]
- Muth, A.; Madan, M.; Archer, J.J.; Ocampo, N.; Rodriguez, L.; Phanstiel, O. Polyamine transport inhibitors: Design, synthesis, and combination therapies with difluoromethylornithine. J. Med. Chem. 2014, 57, 348–363. [Google Scholar] [CrossRef] [PubMed]
- Byers, T.L.; Pegg, A.E. Regulation of polyamine transport in Chinese hamster ovary cells. J. Cell Physiol. 1990, 143, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Lessard, M.; Zhao, C.; Singh, S.M.; Poulin, R. Hormonal and feedback regulation of putrescine and spermidine transport in human breast cancer cells. J. Biol. Chem. 1995, 270, 1685–1694. [Google Scholar] [CrossRef] [PubMed]
- Seiler, N.; Dezeure, F. Polyamine transport in mammalian cells. Int. J. Biochem. 1990, 22, 211–218. [Google Scholar] [CrossRef]
- Porter, C.W.; Bergeron, R.J. Enzyme regulation as an approach to interference with polyamine biosynthesis—An alternative to enzyme inhibition. Adv. Enzym. Regul. 1988, 27, 57–79. [Google Scholar] [CrossRef]
- Heston, W.D.; Kadmon, D.; Fair, W.R. Growth inhibition of a prostate tumor by alpha-difluoromethylornithine and by cyclophosphamide. Cancer Lett. 1982, 16, 71–79. [Google Scholar] [CrossRef]
- Herr, H.W.; Kleinert, E.L.; Conti, P.S.; Burchenal, J.H.; Whitmore, W.F. Effects of alpha-difluoromethylornithine and methylglyoxal bis(guanylhydrazone) on the growth of experimental renal adenocarcinoma in mice. Cancer Res. 1984, 44, 4382–4385. [Google Scholar]
- Hyvönen, M.T.; Khomutov, M.; Vepsäläinen, J.; Khomutov, A.R.; Keinänen, T.A. α-Difluoromethylornithine-Induced Cytostasis is Reversed by Exogenous Polyamines, Not by Thymidine Supplementation. Biomolecules 2021, 11, 707. [Google Scholar] [CrossRef]
- Singh, A.B.; Thomas, T.J.; Thomas, T.; Singh, M.; Mann, R.A. Differential effects of polyamine homologues on the prevention of DL-alpha-difluoromethylornithine-mediated inhibition of malignant cell growth and normal immune response. Cancer Res. 1992, 52, 1840–1847. [Google Scholar]
- Wang, C.; Delcros, J.G.; Biggerstaff, J.; Phanstiel, O. Molecular requirements for targeting the polyamine transport system. Synthesis and biological evaluation of polyamine-anthracene conjugates. J. Med. Chem. 2003, 46, 2672–2682. [Google Scholar] [CrossRef]
- Kaur, N.; Delcros, J.G.; Archer, J.; Weagraff, N.Z.; Martin, B.; Phanstiel Iv, O. Designing the polyamine pharmacophore: Influence of N-substituents on the transport behavior of polyamine conjugates. J. Med. Chem. 2008, 51, 2551–2560. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Twomey, M.; Machado, C.; Gomez, G.; Doshi, M.; Gesquiere, A.J.; Moon, J.H. Caveolae-mediated endocytosis of conjugated polymer nanoparticles. Macromol. Biosci. 2013, 13, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Pramanik, A.; Xu, Z.; Shamsuddin, S.H.; Khaled, Y.S.; Ingram, N.; Maisey, T.; Tomlinson, D.; Coletta, P.L.; Jayne, D.; Hughes, T.A.; et al. Affimer Tagged Cubosomes: Targeting of Carcinoembryonic Antigen Expressing Colorectal Cancer Cells Using. ACS Appl. Mater. Interfaces 2022, 14, 11078–11091. [Google Scholar] [CrossRef] [PubMed]
- Behzadi, S.; Serpooshan, V.; Tao, W.; Hamaly, M.A.; Alkawareek, M.Y.; Dreaden, E.C.; Brown, D.; Alkilany, A.M.; Farokhzad, O.C.; Mahmoudi, M. Cellular uptake of nanoparticles: Journey inside the cell. Chem. Soc. Rev. 2017, 46, 4218–4244. [Google Scholar] [CrossRef]
- Hillaireau, H.; Couvreur, P. Nanocarriers’ entry into the cell: Relevance to drug delivery. Cell. Mol. Life Sci. 2009, 66, 2873–2896. [Google Scholar] [CrossRef]


| Cell Line | Drug | IC50 |
|---|---|---|
| A549G | PG-11047 Nano11047 BENSpm DSS-BEN | 7.9 μM 28.4 μg/mL 1.6 μM 19.9 μg/mL |
| A549R | PG-11047 Nano11047 BENSpm DSS-BEN | >10 μM >25 μg/mL >10 μM >25 μg/mL |
| H157G | PG-11047 Nano11047 BENSpm DSS-BEN | 12.8 μM 13.9 μg/mL 2.9 μM 14.65 μg/mL |
| H157R | PG-11047 Nano11047 BENSpm DSS-BEN | >10 μM >25 μg/mL >10 μM >25 μg/mL |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holbert, C.E.; Foley, J.R.; Yu, A.; Murray Stewart, T.; Phanstiel, O., IV; Oupicky, D.; Casero, R.A., Jr. Polyamine-Based Nanostructures Share Polyamine Transport Mechanisms with Native Polyamines and Their Analogues: Significance for Polyamine-Targeted Therapy. Med. Sci. 2022, 10, 44. https://doi.org/10.3390/medsci10030044
Holbert CE, Foley JR, Yu A, Murray Stewart T, Phanstiel O IV, Oupicky D, Casero RA Jr. Polyamine-Based Nanostructures Share Polyamine Transport Mechanisms with Native Polyamines and Their Analogues: Significance for Polyamine-Targeted Therapy. Medical Sciences. 2022; 10(3):44. https://doi.org/10.3390/medsci10030044
Chicago/Turabian StyleHolbert, Cassandra E., Jackson R. Foley, Ao Yu, Tracy Murray Stewart, Otto Phanstiel, IV, David Oupicky, and Robert A. Casero, Jr. 2022. "Polyamine-Based Nanostructures Share Polyamine Transport Mechanisms with Native Polyamines and Their Analogues: Significance for Polyamine-Targeted Therapy" Medical Sciences 10, no. 3: 44. https://doi.org/10.3390/medsci10030044
APA StyleHolbert, C. E., Foley, J. R., Yu, A., Murray Stewart, T., Phanstiel, O., IV, Oupicky, D., & Casero, R. A., Jr. (2022). Polyamine-Based Nanostructures Share Polyamine Transport Mechanisms with Native Polyamines and Their Analogues: Significance for Polyamine-Targeted Therapy. Medical Sciences, 10(3), 44. https://doi.org/10.3390/medsci10030044









