Clinical Study on the Application of Acupuncture in the Postoperative Rehabilitation of Dogs Affected by Acute Thoracolumbar Disc Herniation
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
- Presence of myelopathy secondary to thoracolumbar disc extrusion (T3–L3), diagnosed by a certified neurologist;
- Diagnostic confirmation of disc extrusion through magnetic resonance imaging (MRI);
- Surgical decompression via hemilaminectomy or mini-hemilaminectomy;
- Application of a physiotherapy protocol in the postoperative period, with hospitalization at the center or day-hospital attendance from Monday to Friday;
- Non-ambulatory paraparetic patients with preservation of deep pain sensation;
- Completion of at least three acupuncture sessions (for Group A);
- Minimum physiotherapy duration of at least 10 days to assess gait recovery;
- Absence of comorbidities (e.g., orthopedic conditions, other neurological disorders, metabolic diseases) or any other condition likely to negatively affect functional recovery (e.g., severely compromised patients following traumatic events, patients who underwent surgical revision due to complications in the immediate postoperative period).
- Incomplete medical records or lack of documentation regarding the exact time of observed gait recovery.
2.2. Parameters of Interest
2.3. Rehabilitation Protocol
2.4. Statistical Analysis
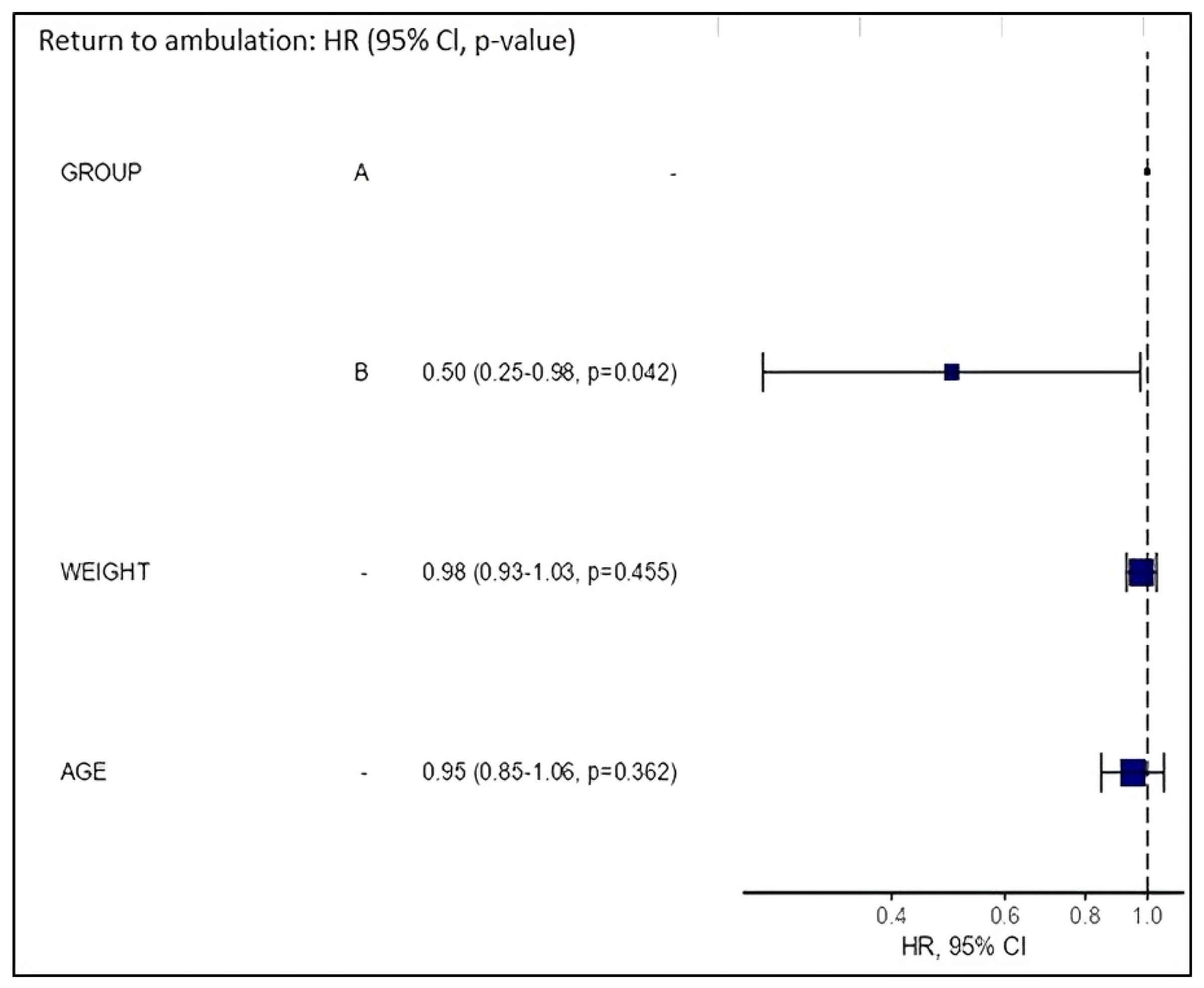
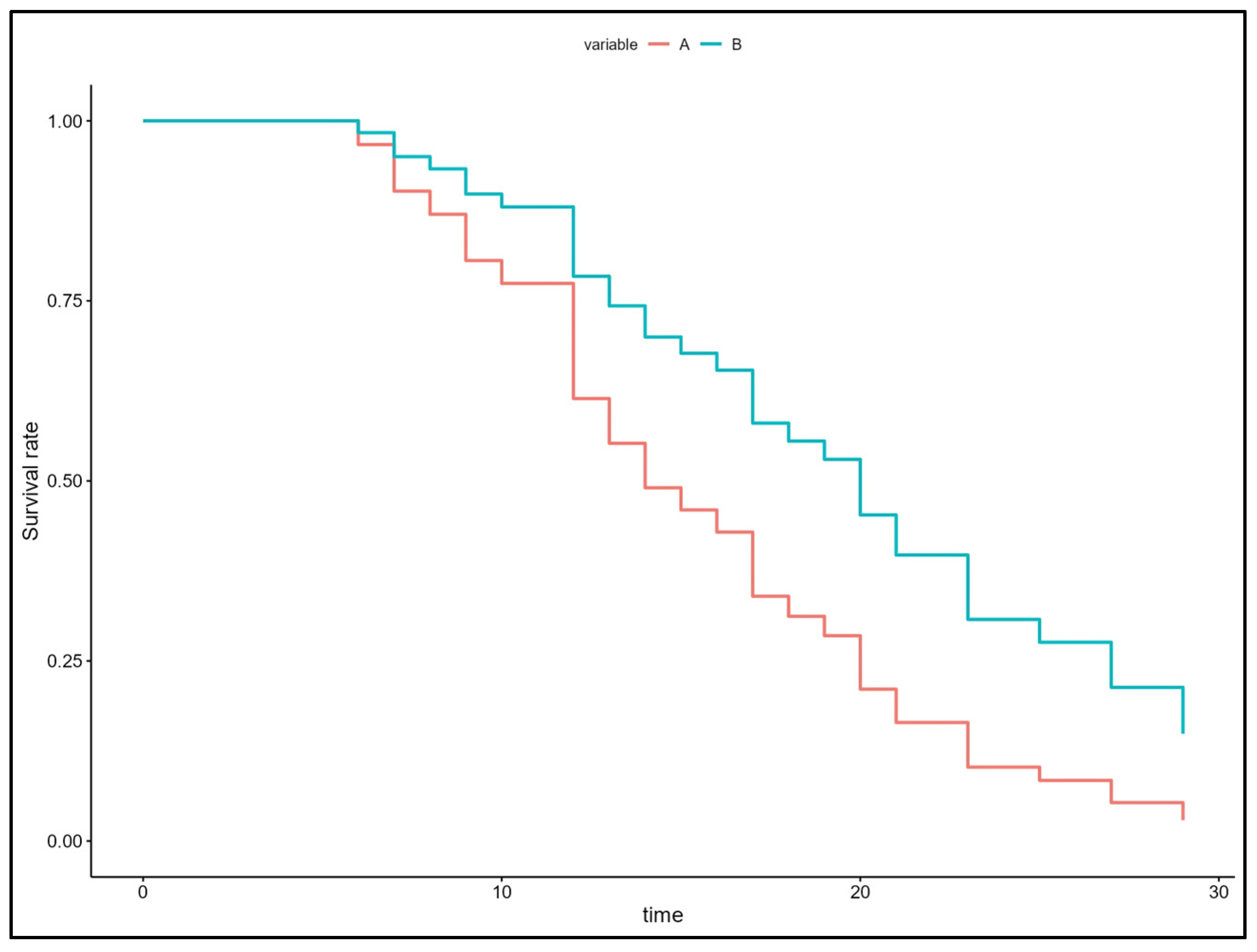
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lindley, S.; Cummings, M. Electroacupuncture and related techniques. In Essentials of Western Veterinary Acupuncture, 1st ed.; Blackwell Publishing Ltd.: Oxford, UK, 2006; p. 183. [Google Scholar]
- Harrison, T.M.; Churgin, S.M. Acupuncture and traditional Chinese veterinary medicine in zoological and exotic animal medicine: A review and introduction of methods. Vet. Sci. 2022, 9, 74. [Google Scholar] [CrossRef]
- Eul-Matern, C. Acupuncture for Dogs and Cats: A Pocket Atlas, 2nd ed.; Thieme: New York, NY, USA, 2022; pp. 1–404. [Google Scholar]
- Huntingford, J.L.; Petty, M.C. Evidence-Based Application of Acupuncture for Pain Management in Companion Animal Medicine. Vet. Sci. 2022, 9, 252. [Google Scholar] [CrossRef] [PubMed]
- Wright, B.D. Acupuncture for the Treatment of Animal Pain. Vet. Clin. N. Am. Small Anim. Pract. 2019, 49, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Fry, L.M.; Neary, S.M.; Sharrock, J.; Rychel, J.K. Acupuncture for analgesia in veterinary medicine. Top. Companion Anim. Med. 2014, 29, 35–42. [Google Scholar] [CrossRef]
- Habacher, G.; Pittler, M.H.; Ernst, E. Effectiveness of acupuncture in veterinary medicine: Systematic review. J. Vet. Intern. Med. 2006, 20, 480–488. [Google Scholar] [CrossRef]
- Sumida, J.M.; Matera, J.M.; Hayashi, A.M. Randomized single-blinded prospective comparison between ozone therapy and electroacupuncture for canine thoracolumbar disk disease. Res. Vet. Sci. 2023, 161, 173–179. [Google Scholar] [CrossRef]
- Bernardini, M. Neurologia Del Cane e Del Gatto, 2nd ed.; Poletto Editore: Milan, Italy, 2010; pp. 254–266. [Google Scholar]
- Olby, N.J.; Moore, S.A.; Brisson, B.; Fenn, J.; Flegel, T.; Kortz, G.; Lewis, M.; Tipold, A. ACVIM consensus statement on diagnosis and management of acute canine thoracolumbar intervertebral disc extrusion. J. Vet. Intern. Med. 2022, 36, 1570–1596. [Google Scholar] [CrossRef]
- Lewis, M.J.; Granger, N.; Jeffery, N.D.; Canine Spinal Cord Injury Consortium (CANSORT-SCI). Emerging and adjunctive therapies for spinal cord injury following acute canine intervertebral disc herniation. Front. Vet. Sci. 2020, 7, 579933. [Google Scholar] [CrossRef]
- Spinella, G.; Bettella, P.; Riccio, B.; Okonji, S. Overview of the current literature on the most common neurological diseases in dogs with a particular focus on rehabilitation. Vet. Sci. 2022, 9, 429. [Google Scholar] [CrossRef]
- Frank, L.R.; Roynard, P.F.P. Veterinary Neurologic Rehabilitation: The Rationale for a Comprehensive Approach. Top. Companion Anim. Med. 2018, 33, 49–57. [Google Scholar] [CrossRef]
- Hayashi, A.M.; Matera, J.M.; De Campos Fonseca Pinto, A.C.B. Evaluation of electroacupuncture treatment for thoracolumbar intervertebral disk disease in dogs. J. Am. Vet. Med. Assoc. 2007, 231, 913–918. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.C.; Lee, J.Y.; Moon, Y.J.; Kim, S.W.; Oh, T.H.; Yune, T.Y. Acupuncture-mediated inhibition of inflammation facilitates significant functional recovery after spinal cord injury. Neurobiol. Dis. 2010, 39, 272–282. [Google Scholar] [CrossRef]
- Han, H.-J.; Yoon, H.-Y.; Kim, J.-Y.; Jang, H.-Y.; Lee, B.; Choi, S.H.; Jeong, S.-W. Clinical effect of additional electroacupuncture on thoracolumbar intervertebral disc herniation in 80 paraplegic dogs. Am. J. Chin. Med. 2010, 38, 1015–1025. [Google Scholar] [CrossRef]
- Roynard, P.; Frank, L.; Xie, H.; Fowler, M. Acupuncture for small animal neurologic disorders. Vet. Clin. N. Am. Small Anim. Pract. 2018, 48, 201–219. [Google Scholar] [CrossRef]
- Santos, B.P.; Joaquim, J.G.; Cassu, R.N.; Pantoja, J.C.; Luna, S.P.L. Effects of Acupuncture in the Treatment of Dogs with Neurological Sequels of Distemper Virus. J. Acupunct. Meridian Stud. 2022, 15, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.; Liebel, F.X.; Fadda, A.; Lazzerini, K.; Harcourt-Brown, T. Same-day surgery may reduce the risk of losing pain perception in dogs with thoracolumbar disc extrusion. J. Small Anim. Pract. 2020, 61, 442–448. [Google Scholar] [CrossRef]
- Bennaim, M.; Porato, M.; Jarleton, A.; Hamon, M.; Carroll, J.D.; Gommeren, K.; Balligand, M. Preliminary evaluation of the effects of photobiomodulation therapy and physical rehabilitation on early postoperative recovery of dogs undergoing hemilaminectomy for treatment of thoracolumbar intervertebral disk disease. Am. J. Vet. Res. 2017, 78, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Khammar, A.; Yarahmadi, M.; Madadizadeh, F. What is analysis of covariance (ancova) and how to correctly report its results in medical research? Iran. J. Public Health 2020, 49, 1016–1017. [Google Scholar] [CrossRef]
- Ferreira, A.; Correia, J.; Jaggy, A. Thoracolumbar disc disease in 71 paraplegic dogs: Influence of rate of onset and duration of clinical signs on treatment results. J. Small Anim. Pract. 2002, 43, 158–163. [Google Scholar] [CrossRef]
- Jia, Q.; Wang, Y.; Pang, H.; Fan, K.; Xie, H.; Lin, J. Retrospective study of acupuncture treatment for canine thoracolumbar intervertebral disc herniation. One Health Adv. 2023, 1, 22. [Google Scholar] [CrossRef]
- Aikawa, T.; Fujita, H.; Kanazono, S.; Shibata, M.; Yoshigae, Y. Long-term neurologic outcome of hemilaminectomy and disk fenestration for treatment of dogs with thoracolumbar intervertebral disk herniation: 831 cases (2000–2007). J. Am. Vet. Med. Assoc. 2012, 241, 1617–1626. [Google Scholar] [CrossRef] [PubMed]
- Jeffery, N.D.; Barker, A.K.; Hu, H.Z.; Alcott, C.J.; Kraus, K.H.; Scanlin, E.M.; Granger, N.; Levine, J.M. Factors associated with recovery from paraplegia in dogs with loss of pain perception in the pelvic limbs following intervertebral disk herniation. J. Am. Vet. Med. Assoc. 2016, 248, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Langerhuus, L.; Miles, J. Proportion recovery and times to ambulation for non-ambulatory dogs with thoracolumbar disc extrusions treated with hemilaminectomy or conservative treatment: A systematic review and meta-analysis of case-series studies. Vet. J. 2017, 220, 7–16. [Google Scholar] [CrossRef]
- Shaw, T.A.; De Risio, L.; Laws, E.J.; Rose, J.H.; Harcourt-Brown, T.R.; Granger, N. Prognostic factors associated with recovery of ambulation and urinary continence in dogs with acute lumbosacral spinal cord injury. J. Vet. Intern. Med. 2017, 31, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Bruno, E.; Canal, S.; Antonucci, M.; Bernardini, M.; Balducci, F.; Musella, V.; Mussoni, M.; Spinella, G. Perilesional photobiomodulation therapy and physical rehabilitation in post-operative recovery of dogs surgically treated for thoracolumbar disk extrusion. BMC Vet. Res. 2020, 16, 120. [Google Scholar] [CrossRef]
- Davis, G.J.; Brown, D.C. Prognostic indicators for time to ambulation after surgical decompression in nonambulatory dogs with acute thoracolumbar disk extrusions: 112 cases. Vet. Surg. 2002, 31, 513–518. [Google Scholar] [CrossRef]
- Ruddle, T.L.; Allen, D.A.; Schertel, E.R.; Barnhart, M.D.; Wilson, E.R.; Lineberger, J.A.; Klocke, N.W.; Lehenbauer, T.W. Outcome and prognostic factors in nonambulatory Hansen Type I intervertebral disc extrusions: 308 cases. Vet. Comp. Orthop. Traumatol. 2006, 19, 29–34. [Google Scholar]
- Zidan, N.; Sims, C.; Fenn, J.; Williams, K.; Griffith, E.; Early, P.J.; Mariani, C.L.; Munana, K.R.; Guevar, J.; Olby, N.J. A randomized, blinded, prospective clinical trial of postoperative rehabilitation in dogs after surgical decompression of acute thoracolumbar intervertebral disc herniation. J. Vet. Intern. Med. 2018, 32, 1133–1144. [Google Scholar] [CrossRef]
- Hady, L.L.; Schwarz, P.D. Recovery times for dogs undergoing thoracolumbar hemilaminectomy with fenestration and physical rehabilitation: A review of 113 cases. J. Vet. Med. Anim. Health 2015, 7, 278–289. [Google Scholar] [CrossRef]
- Hodgson, M.; Bevan, J.; Evans, R.; Johnson, T. Influence of in-house rehabilitation on the postoperative outcome of dogs with intervertebral disk herniation. Vet. Surg. 2017, 46, 566–573. [Google Scholar] [CrossRef]
- Yang, J.W.; Jeong, S.M.; Seo, K.M.; Nam, T.C. Effects of corticosteroid and electroacupuncture on experimental spinal cord injury in dogs. J. Vet. Sci. 2003, 4, 97. [Google Scholar] [CrossRef]
- Joaquim, J.G.F.; Luna, S.P.L.; Brondani, J.T.; Torelli, S.R.; Rahal, S.C.; De Paula Freitas, F. Comparison of decompressive surgery, electroacupuncture, and decompressive surgery followed by electroacupuncture for the treatment of dogs with intervertebral disk disease with long-standing severe neurologic deficits. J. Am. Vet. Med. Assoc. 2010, 236, 1225–1229. [Google Scholar] [CrossRef]
- Liu, C.M.; Lin, C.T. Retrospective Study of a New Standardized Acupuncture Treatment Protocol on Thoracolumbar Spinal Cord Diseases in 84 Dogs. Pak. Vet. J. 2015, 35, 461–465. [Google Scholar]
- Dewey, C.; Xie, H. The scientific basis of acupuncture for veterinary pain management: A review based on relevant literature from the last two decades. Open Vet. J. 2021, 11, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Lao, L.; Ren, K.; Berman, B.M. Mechanisms of acupuncture–electroacupuncture on persistent pain. Anesthesiology 2014, 120, 482–503. [Google Scholar] [CrossRef]
- Martins, Â.; Gouveia, D.; Cardoso, A.; Carvalho, C.; Coelho, T.; Silva, C.; Viegas, I.; Gamboa, Ó.; Ferreira, A. A controlled clinical study of intensive neurorehabilitation in post-surgical dogs with severe acute intervertebral disc extrusion. Animals 2021, 11, 3034. [Google Scholar] [CrossRef]
- Brisson, B.A. Intervertebral disc disease in dogs. Vet. Clin. N. Am. Small Anim. Pract. 2010, 40, 829–858. [Google Scholar] [CrossRef]
- Draper, W.E.; Schubert, T.A.; Clemmons, R.M.; Miles, S.A. Low-level laser therapy reduces time to ambulation in dogs after hemilaminectomy: A preliminary study. J. Small Anim. Pract. 2012, 53, 465–469. [Google Scholar] [CrossRef]
- Olby, N.; Levine, J.; Harris, T.; Muñana, K.; Skeen, T.; Sharp, N. Long-term functional outcome of dogs with severe injuries of the thoracolumbar spinal cord: 87 cases (1996–2001). J. Am. Vet. Med. Assoc. 2003, 222, 762–769. [Google Scholar] [CrossRef]
| Age in Years | Weight (kg) | S-C (Days) | C-R (Days) | DEA (Days) | |
|---|---|---|---|---|---|
| Group A | 5.8 ± 2.9 (5) (4.31–7.24) | 12.3 ± 2.9 (12.3) (7.38–13.4) | 1.72 ± 2.08 (1) (0.69–2.76) | 3.28 ± 1.67 (3) a (2.45–4.11) | 15.06 ± 6.38 (13.5) (11.9–18.2) |
| Group B | 7.4 ± 3.6 (6) (5.83–8.95) | 12.3 ± 12.6 (7.5) (7.06–14.7) | 1.43 ± 1.97 (1) (0.58–2.29) | 4.96 ± 2.62 (5) a (3.82–6.09) | 18.1 ± 6.43 (18.5) (14.9–21.3) |
| GROUP | TEST | MATRIX | Age | Weight | S-C | C-R | T0 | DEA | N. Session |
|---|---|---|---|---|---|---|---|---|---|
| A | Spearman correlation p-value | Age | 0.1357 | 0.2084 | 0.7196 | 0.8362 | 0.5646 | 0.0086 * | |
| Weight | 0.1357 | 0.6725 | 0.3176 | 0.8366 | 0.5212 | 0.6521 | |||
| S-C | 0.2084 | 0.6725 | 0.1272 | 0.3698 | 0.5917 | 0.3027 | |||
| C-R | 0.7196 | 0.3176 | 0.1272 | 0.0184 | 0.4823 | 0.6063 | |||
| T0 | 0.8362 | 0.8366 | 0.3698 | 0.0184 | 0.7216 | 0.8096 | |||
| DEA | 0.5646 | 0.5212 | 0.5917 | 0.4823 | 0.7216 | 0.0012 | |||
| N. session | 0.0086 * | 0.6521 | 0.3027 | 0.6063 | 0.8096 | 0.0012 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antonucci, M.; Passarini, E.; Bruno, E.; Dalmonte, T.; Spinella, G. Clinical Study on the Application of Acupuncture in the Postoperative Rehabilitation of Dogs Affected by Acute Thoracolumbar Disc Herniation. Animals 2025, 15, 1154. https://doi.org/10.3390/ani15081154
Antonucci M, Passarini E, Bruno E, Dalmonte T, Spinella G. Clinical Study on the Application of Acupuncture in the Postoperative Rehabilitation of Dogs Affected by Acute Thoracolumbar Disc Herniation. Animals. 2025; 15(8):1154. https://doi.org/10.3390/ani15081154
Chicago/Turabian StyleAntonucci, Michela, Erika Passarini, Enrico Bruno, Thomas Dalmonte, and Giuseppe Spinella. 2025. "Clinical Study on the Application of Acupuncture in the Postoperative Rehabilitation of Dogs Affected by Acute Thoracolumbar Disc Herniation" Animals 15, no. 8: 1154. https://doi.org/10.3390/ani15081154
APA StyleAntonucci, M., Passarini, E., Bruno, E., Dalmonte, T., & Spinella, G. (2025). Clinical Study on the Application of Acupuncture in the Postoperative Rehabilitation of Dogs Affected by Acute Thoracolumbar Disc Herniation. Animals, 15(8), 1154. https://doi.org/10.3390/ani15081154






