Bacillus spp. Potentiate the Virulence and Intracellular Invasion of A. paragallinarum in Chickens
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Coculture of Various Bacillus Strains and A. paragallinarum
2.2. Hemolytic Activity Assessment of Bacillus Strains
2.3. Coculture of Bacillus Strains and A. paragallinarum In Vitro
2.4. NAD Measurement
2.5. Antibiotic Susceptibility Testing
2.6. DNA Sequencing and Genome Analysis
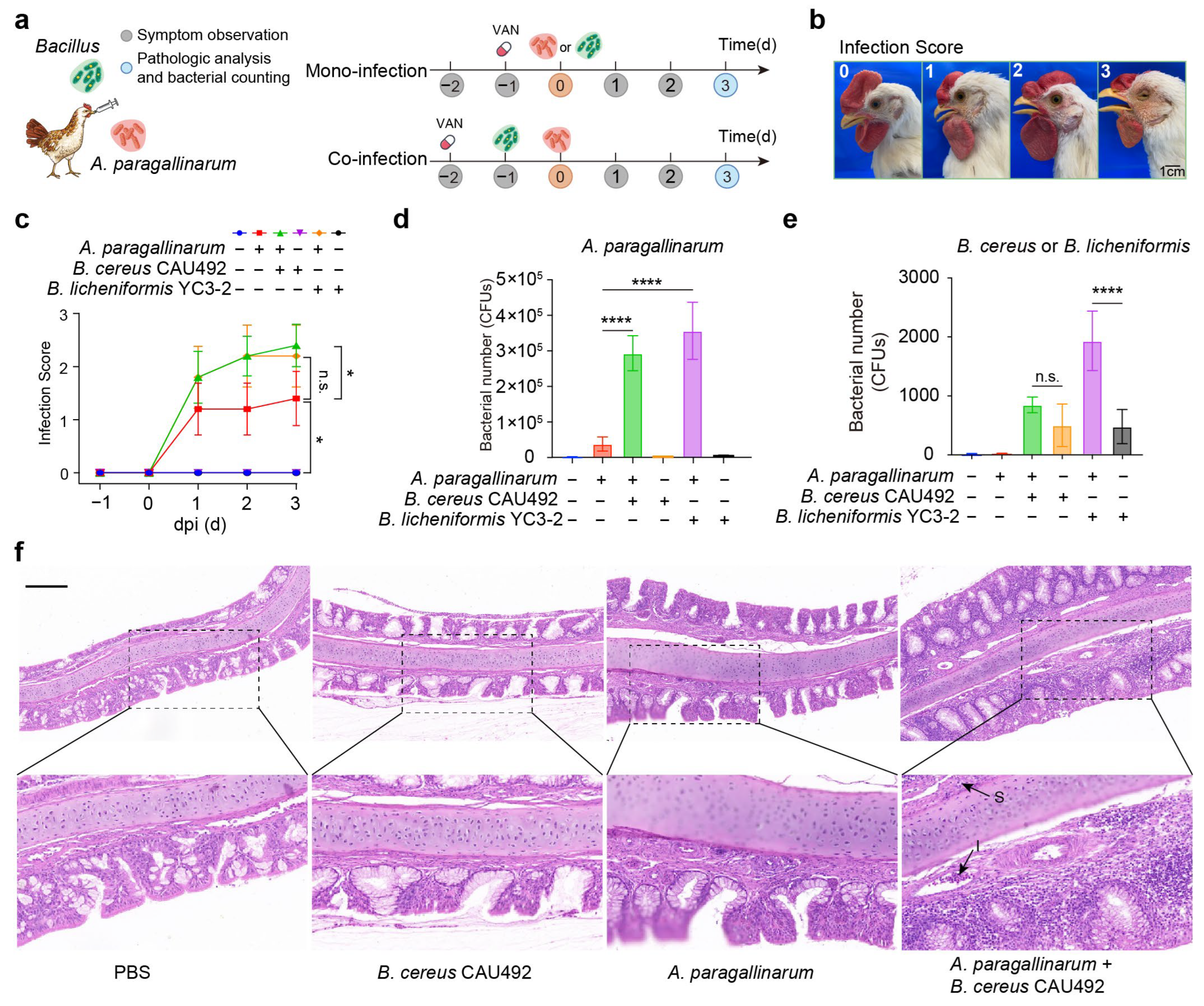
2.7. Infection Challenge Experiments in Birds
2.8. Statistical Analysis
3. Results
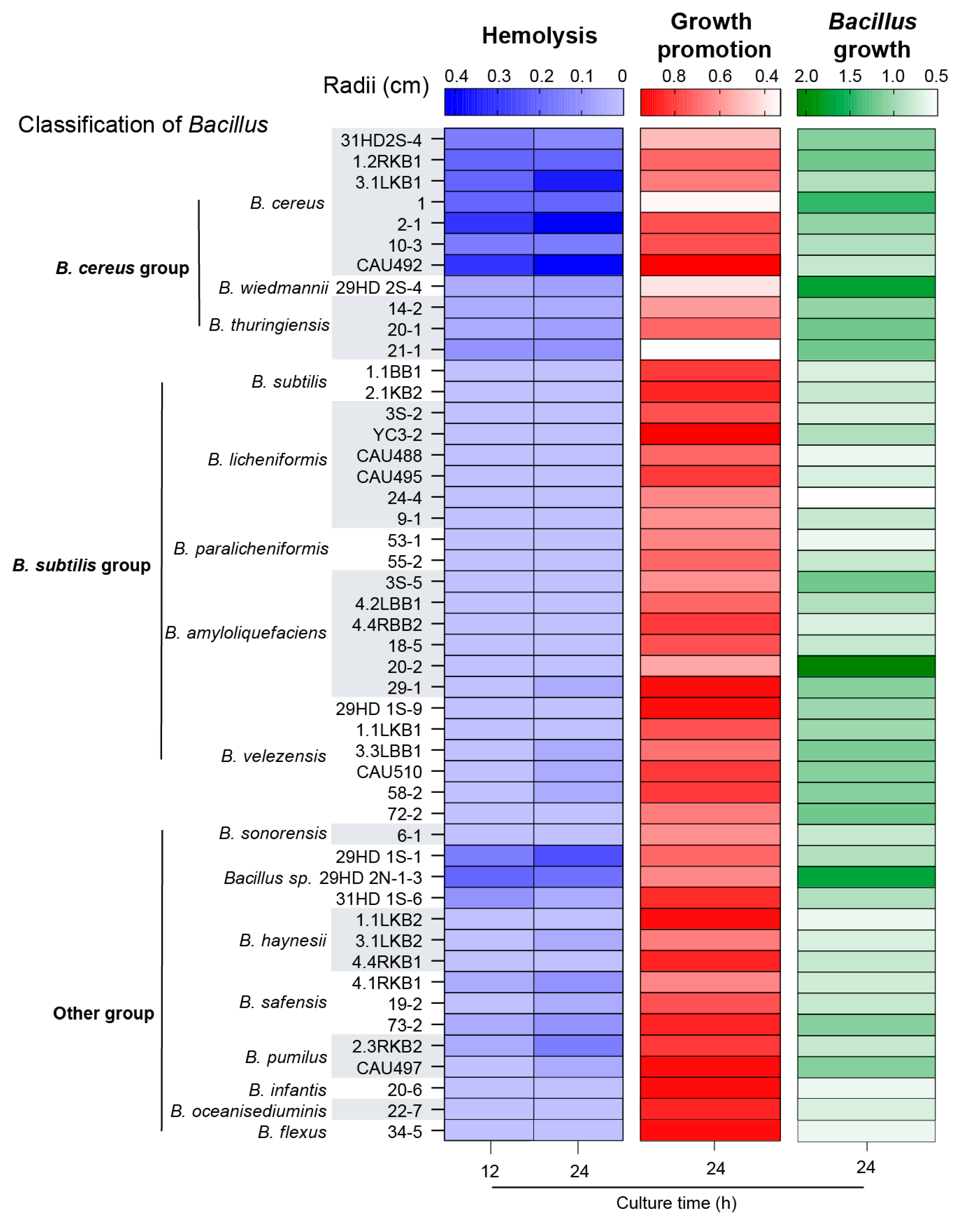
3.1. Bacillus Facilitates the Growth of A. paragallinarum Under NAD-Deficiency Conditions
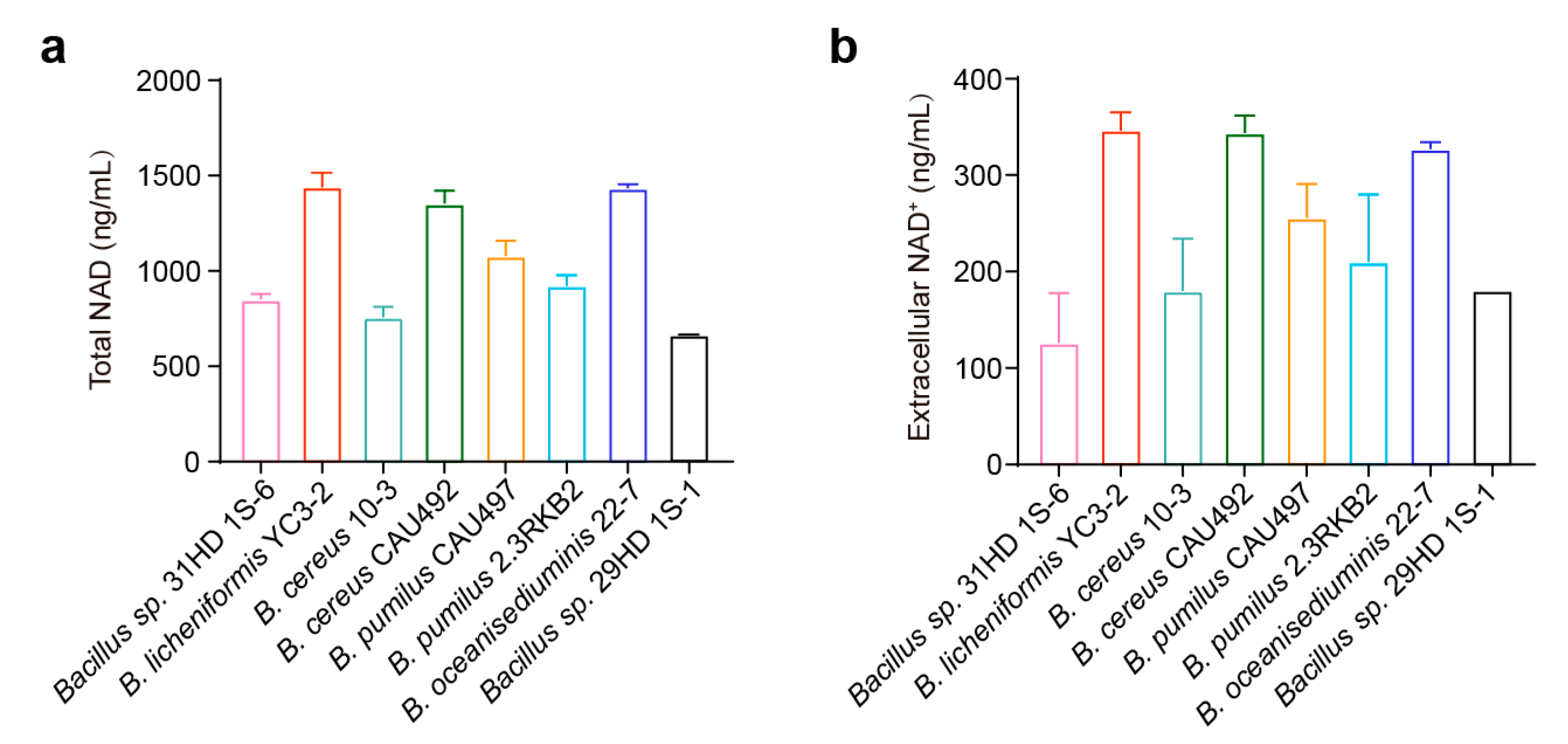
3.2. NAD Derived from Bacillus Promotes the Growth of A. paragallinarum
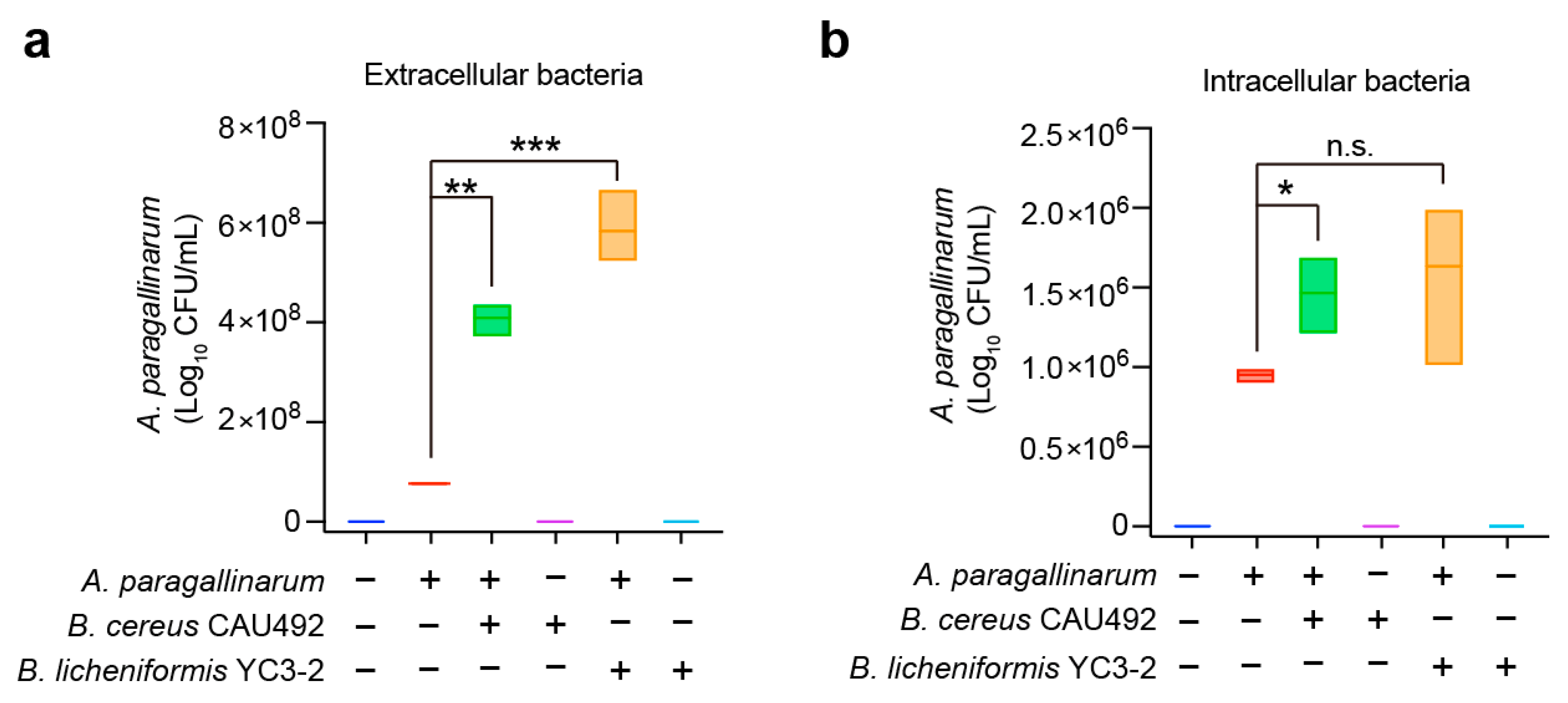
3.3. Bacillus Enhances the Invasion of A. paragallinarum In Vitro
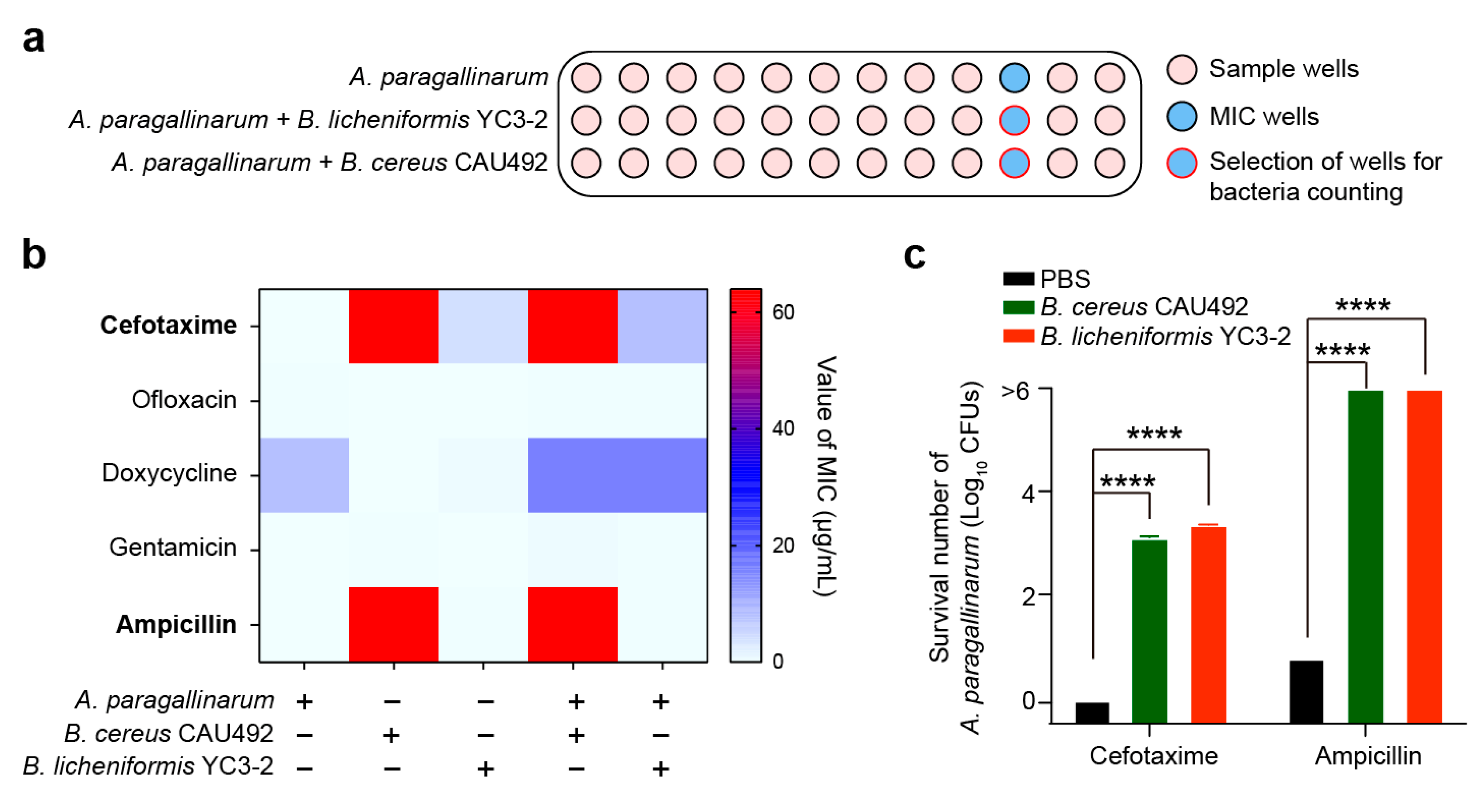
3.4. Bacillus spp. Confer Protection on A. paragallinarum Against Antibiotics
3.5. Bacillus Aggravates the Disease Severity in A. paragallinarum-Infected Chickens
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CLSI | Clinical and Laboratory Standards Institute |
| NAD+ | Nicotinamide adenine dinucleotide |
| MIC | Minimum inhibitory concentration |
| McF | McFarland turbidity |
| MOI | Multiplicity of infection |
References
- Tay, W.H.; Chong, K.K.; Kline, K.A. Polymicrobial-Host Interactions during Infection. J. Mol. Biol. 2016, 428, 3355–3371. [Google Scholar] [CrossRef]
- Pathak, A.; Angst, D.C.; Leon-Sampedro, R.; Hall, A.R. Antibiotic-degrading resistance changes bacterial community structure via species-specific responses. ISME J. 2023, 17, 1495–1503. [Google Scholar] [CrossRef] [PubMed]
- Pearl Mizrahi, S.; Goyal, A.; Gore, J. Community interactions drive the evolution of antibiotic tolerance in bacteria. Proc. Natl. Acad. Sci. USA 2023, 120, e2209043119. [Google Scholar] [CrossRef] [PubMed]
- Abushaheen, M.A.; Muzaheed; Fatani, A.J.; Alosaimi, M.; Mansy, W.; George, M.; Acharya, S.; Rathod, S.; Divakar, D.D.; Jhugroo, C.; et al. Antimicrobial resistance, mechanisms and its clinical significance. Dis. Mon. 2020, 66, 100971. [Google Scholar] [CrossRef] [PubMed]
- Kost, C.; Patil, K.R.; Friedman, J.; Garcia, S.L.; Ralser, M. Metabolic exchanges are ubiquitous in natural microbial communities. Nat. Microbiol. 2023, 8, 2244–2252. [Google Scholar] [CrossRef]
- Semenec, L.; Cain, A.K.; Dawson, C.J.; Liu, Q.; Dinh, H.; Lott, H.; Penesyan, A.; Maharjan, R.; Short, F.L.; Hassan, K.A.; et al. Cross-protection and cross-feeding between Klebsiella pneumoniae and Acinetobacter baumannii promotes their co-existence. Nat. Commun. 2023, 14, 702. [Google Scholar] [CrossRef]
- Oliveira, M.; Cunha, E.; Tavares, L.; Serrano, I.P. aeruginosa interactions with other microbes in biofilms during co-infection. AIMS Microbiol. 2023, 9, 612–646. [Google Scholar] [CrossRef]
- Bottery, M.J.; Pitchford, J.W.; Friman, V.P. Ecology and evolution of antimicrobial resistance in bacterial communities. ISME J. 2021, 15, 939–948. [Google Scholar] [CrossRef]
- Kim, H.-J.; Na, S.W.; Alodaini, H.A.; Al-Dosary, M.A.; Nandhakumari, P.; Dyona, L. Prevalence of multidrug-resistant bacteria associated with polymicrobial infections. J. Infect. Public. Health 2021, 14, 1864–1869. [Google Scholar] [CrossRef]
- Cordero, O.; Wildschutte, H.; Kirkup, B.; Proehl, S.; Ngo, L.; Hussain, F.; Le Roux, F.; Mincer, T.; Polz, M. Ecological populations of bacteria act as socially cohesive units of antibiotic production and resistance. Science 2012, 337, 1228–1231. [Google Scholar] [CrossRef]
- Man, W.H.; de Steenhuijsen Piters, W.A.; Bogaert, D. The microbiota of the respiratory tract: Gatekeeper to respiratory health. Nat. Rev. Microbiol. 2017, 15, 259–270. [Google Scholar] [CrossRef]
- Jeong, O.M.; Kang, M.S.; Blackall, P.J.; Jeon, B.W.; Kim, J.H.; Jeong, J.; Lee, H.J.; Kim, D.W.; Kwon, Y.K.; Kim, J.H. Genotypic divergence of Avibacterium paragallinarum isolates with different growth requirements for nicotinamide adenine dinucleotide. Avian Pathol. 2020, 49, 153–160. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, Y.; Yang, H.; Li, Q.; Gong, X.; Zhang, G.; Zhu, K. Resident bacteria contribute to opportunistic infections of the respiratory tract. PLoS Pathog. 2021, 17, e1009436. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Chen, Y.; Wu, Y.; Wang, Y.; Zhu, K. Commensal bacteria contribute to the growth of multidrug-resistant Avibacterium paragallinarum in chickens. Front. Microbiol. 2022, 13, 1010584. [Google Scholar] [CrossRef] [PubMed]
- Arreguin-Nava, M.A.; Graham, B.D.; Adhikari, B.; Agnello, M.; Selby, C.M.; Hernandez-Velasco, X.; Vuong, C.N.; Solis-Cruz, B.; Hernandez-Patlan, D.; Latorre, J.D.; et al. Evaluation of in ovo Bacillus spp. based probiotic administration on horizontal transmission of virulent Escherichia coli in neonatal broiler chickens. Poult. Sci. 2019, 98, 6483–6491. [Google Scholar] [CrossRef]
- Cui, Y.; Wang, S.; Ding, S.; Shen, J.; Zhu, K. Toxins and mobile antimicrobial resistance genes in Bacillus probiotics constitute a potential risk for One Health. J. Hazard. Mater. 2020, 382, 121266. [Google Scholar] [CrossRef] [PubMed]
- Deng, F.; Chen, Y.; Sun, T.; Wu, Y.; Su, Y.; Liu, C.; Zhou, J.; Deng, Y.; Wen, J. Antimicrobial resistance, virulence characteristics and genotypes of Bacillus spp. from probiotic products of diverse origins. Food Res. Int. 2021, 139, 109949. [Google Scholar] [CrossRef]
- A, A.J.; Suresh, A. Oral microbial shift induced by probiotic Bacillus coagualans along with its clinical perspectives. J. Oral. Biol. Craniofacial Res. 2023, 13, 398–402. [Google Scholar] [CrossRef]
- Morales-Erasto, V.; Falconi-Agapito, F.; Luna-Galaz, G.A.; Saravia, L.E.; Montalvan-Avalos, A.; Soriano-Vargas, E.E.; Fernandez-Diaz, M. Coinfection of Avibacterium paragallinarum and Ornithobacterium rhinotracheale in Chickens from Peru. Avian Dis. 2016, 60, 75–78. [Google Scholar] [CrossRef]
- O’Meara, S. Antimicrobial resistance. Nature 2020, 586, S49. [Google Scholar] [CrossRef]
- Mestre, A.; Poulin, R.; Hortal, J. A niche perspective on the range expansion of symbionts. Biol. Rev. Camb. Philos. Soc. 2020, 95, 491–516. [Google Scholar] [CrossRef] [PubMed]
- Ona, L.; Giri, S.; Avermann, N.; Kreienbaum, M.; Thormann, K.M.; Kost, C. Obligate cross-feeding expands the metabolic niche of bacteria. Nat. Ecol. Evol. 2021, 5, 1224–1232. [Google Scholar] [CrossRef] [PubMed]
- Ponomarova, O.; Patil, K.R. Metabolic interactions in microbial communities: Untangling the Gordian knot. Curr. Opin. Microbiol. 2015, 27, 37–44. [Google Scholar] [CrossRef]
- Giri, S.; Ona, L.; Waschina, S.; Shitut, S.; Yousif, G.; Kaleta, C.; Kost, C. Metabolic dissimilarity determines the establishment of cross-feeding interactions in bacteria. Curr. Biol. 2021, 31, 5547–5557.E6. [Google Scholar] [CrossRef]
- Zhu, J.; Chen, Y.; Imre, K.; Arslan-Acaroz, D.; Istanbullugil, F.R.; Fang, Y.; Ros, G.; Zhu, K.; Acaroz, U. Mechanisms of probiotic Bacillus against enteric bacterial infections. One Health Adv. 2023, 1, 21. [Google Scholar] [CrossRef]
- Cui, Y.; Zhu, J.; Li, P.; Guo, F.; Yang, B.; Su, X.; Zhou, H.; Zhu, K.; Xu, F. Assessment of probiotic Bacillus velezensis supplementation to reduce Campylobacter jejuni colonization in chickens. Poult. Sci. 2024, 103, 103897. [Google Scholar] [CrossRef]
- Sid, H.; Benachour, K.; Rautenschlein, S. Co-infection with Multiple Respiratory Pathogens Contributes to Increased Mortality Rates in Algerian Poultry Flocks. Avian Dis. 2015, 59, 440–446. [Google Scholar] [CrossRef]
- Samy, A.; Naguib, M.M. Avian Respiratory Coinfection and Impact on Avian Influenza Pathogenicity in Domestic Poultry: Field and Experimental Findings. Vet. Sci. 2018, 5, 23. [Google Scholar] [CrossRef]
- Wu, Z.; Chen, C.; Zhang, Q.; Bao, J.; Fan, Q.; Li, R.; Ishfaq, M.; Li, J. Arachidonic acid metabolism is elevated in Mycoplasma gallisepticum and Escherichia coli co-infection and induces LTC4 in serum as the biomarker for detecting poultry respiratory disease. Virulence 2020, 11, 730–738. [Google Scholar] [CrossRef]
- Mouahid, M.; Bisgaard, M.; Morley, A.J.; Mutters, R.; Mannheim, W. Occurrence of V-factor (NAD) independent strains of Haemophilus paragallinarum. Vet. Microbiol. 1992, 31, 363–368. [Google Scholar] [CrossRef]
- Paudel, S.; Hess, M.; Hess, C. Coinfection of Avibacterium paragallinarum and Gallibacterium anatis in Specific-Pathogen-Free Chickens Complicates Clinical Signs of Infectious Coryza, Which Can Be Prevented by Vaccination. Avian Dis. 2017, 61, 55–63. [Google Scholar] [CrossRef]
- Shimizu, M. NAD(+)/NADH homeostasis affects metabolic adaptation to hypoxia and secondary metabolite production in filamentous fungi. Biosci. Biotechnol. Biochem. 2018, 82, 216–224. [Google Scholar] [CrossRef]
- Arjes, H.A.; Vo, L.; Dunn, C.M.; Willis, L.; DeRosa, C.A.; Fraser, C.L.; Kearns, D.B.; Huang, K.C. Biosurfactant-mediated membrane depolarization maintains viability during oxygen depletion in Bacillus subtilis. Curr. Biol. 2020, 30, 1011–1022.e6. [Google Scholar] [CrossRef] [PubMed]
- Choi, D. NADH-Reductive Stress in Cancer Cell Proliferation. Mol. Cells 2023, 46, 473–475. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Yoon, H. Mitochondrial sirtuins: Energy dynamics and cancer metabolism. Mol. Cells 2024, 47, 100029. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; He, Y.; She, Q.; Larese-Casanova, P.; Li, P.; Chai, Y. Heterogeneity in respiratory electron transfer and adaptive iron utilization in a bacterial biofilm. Nat. Commun. 2019, 10, 3702. [Google Scholar] [CrossRef]
- Cui, Y.; Liu, Y.; Liu, X.; Xia, X.; Ding, S.; Zhu, K. Evaluation of the Toxicity and Toxicokinetics of Cereulide from an Emetic Bacillus cereus Strain of Milk Origin. Toxins 2016, 8, 156. [Google Scholar] [CrossRef]
- Galdino, A.C.M.; Vaillancourt, M.; Celedonio, D.; Huse, K.; Doi, Y.; Lee, J.S.; Jorth, P. Evolved bacterial siderophore-mediated antibiotic cross-protection. Res. Sq. 2023. [Google Scholar] [CrossRef]
- Xu, H.; Tan, C.; Li, C.; Li, J.; Han, Y.; Tang, Y.; Lei, C.; Wang, H. ESBL- Escherichia coli extracellular vesicles mediate bacterial resistance to beta-lactam and mediate horizontal transfer of bla(CTX-M-55). Int. J. Antimicrob. Agents 2024, 63, 107145. [Google Scholar] [CrossRef]
- Galdino, A.C.M.; Vaillancourt, M.; Celedonio, D.; Huse, K.; Doi, Y.; Lee, J.S.; Jorth, P. Siderophores promote cooperative interspecies and intraspecies cross-protection against antibiotics in vitro. Nat. Microbiol. 2024, 9, 631–646. [Google Scholar] [CrossRef]
- Lee, K.; Lee, K.M.; Kim, D.; Yoon, S.S. Molecular Determinants of the Thickened Matrix in a Dual-Species Pseudomonas aeruginosa and Enterococcus faecalis Biofilm. Appl. Environ. Microbiol. 2017, 83, e01182-17. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Ruelens, P.; Farr, A.D.; de Visser, J.; Baraban, L. Population dynamics of cross-protection against beta-lactam antibiotics in droplet microreactors. Front. Microbiol. 2023, 14, 1294790. [Google Scholar] [CrossRef] [PubMed]
- Perlin, M.H.; Clark, D.R.; McKenzie, C.; Patel, H.; Jackson, N.; Kormanik, C.; Powell, C.; Bajorek, A.; Myers, D.A.; Dugatkin, L.A.; et al. Protection of Salmonella by ampicillin-resistant Escherichia coli in the presence of otherwise lethal drug concentrations. Proc. Biol. Sci. 2009, 276, 3759–3768. [Google Scholar] [CrossRef] [PubMed]
- Falcon Garcia, C.; Kretschmer, M.; Lozano-Andrade, C.N.; Schonleitner, M.; Dragos, A.; Kovacs, A.T.; Lieleg, O. Metal ions weaken the hydrophobicity and antibiotic resistance of Bacillus subtilis NCIB 3610 biofilms. NPJ Biofilms Microbiomes 2020, 6, 1. [Google Scholar] [CrossRef]
- Cao, M.; Helmann, J.D. Regulation of the Bacillus subtilis bcrC bacitracin resistance gene by two extracytoplasmic function sigma factors. J. Bacteriol. 2002, 184, 6123–6129. [Google Scholar] [CrossRef]
- Yang, S.; Fan, K.; Lin, W.; Wang, J.; Lin, M.; Yang, S.; Jiang, Y.; Huang, X.; Chen, W.; Huang, C. Identification of a multiple drug-resistance gene island in the Haemophilus parasuis chromosome. J. Glob. Antimicrob. Resist. 2020, 22, 422–425. [Google Scholar] [CrossRef]
- Lancashire, J.F.; Terry, T.D.; Blackall, P.J.; Jennings, M.P. Plasmid-encoded Tet B tetracycline resistance in Haemophilus parasuis. Antimicrob. Agents Chemother. 2005, 49, 1927–1931. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, J.; Liu, Y.; Gao, T.; Chen, Y.; Yang, K.; Liu, W.; Zhu, K.; Zhou, D. Bacillus spp. Potentiate the Virulence and Intracellular Invasion of A. paragallinarum in Chickens. Animals 2025, 15, 2076. https://doi.org/10.3390/ani15142076
Zhu J, Liu Y, Gao T, Chen Y, Yang K, Liu W, Zhu K, Zhou D. Bacillus spp. Potentiate the Virulence and Intracellular Invasion of A. paragallinarum in Chickens. Animals. 2025; 15(14):2076. https://doi.org/10.3390/ani15142076
Chicago/Turabian StyleZhu, Jiajia, Ying Liu, Ting Gao, Yunsheng Chen, Keli Yang, Wei Liu, Kui Zhu, and Danna Zhou. 2025. "Bacillus spp. Potentiate the Virulence and Intracellular Invasion of A. paragallinarum in Chickens" Animals 15, no. 14: 2076. https://doi.org/10.3390/ani15142076
APA StyleZhu, J., Liu, Y., Gao, T., Chen, Y., Yang, K., Liu, W., Zhu, K., & Zhou, D. (2025). Bacillus spp. Potentiate the Virulence and Intracellular Invasion of A. paragallinarum in Chickens. Animals, 15(14), 2076. https://doi.org/10.3390/ani15142076








