Buprenorphine Versus Methadone in Female New Zealand White Rabbits Undergoing Balanced Anaesthesia for Calvaria Surgery
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Animals
2.3. Anaesthesia Management
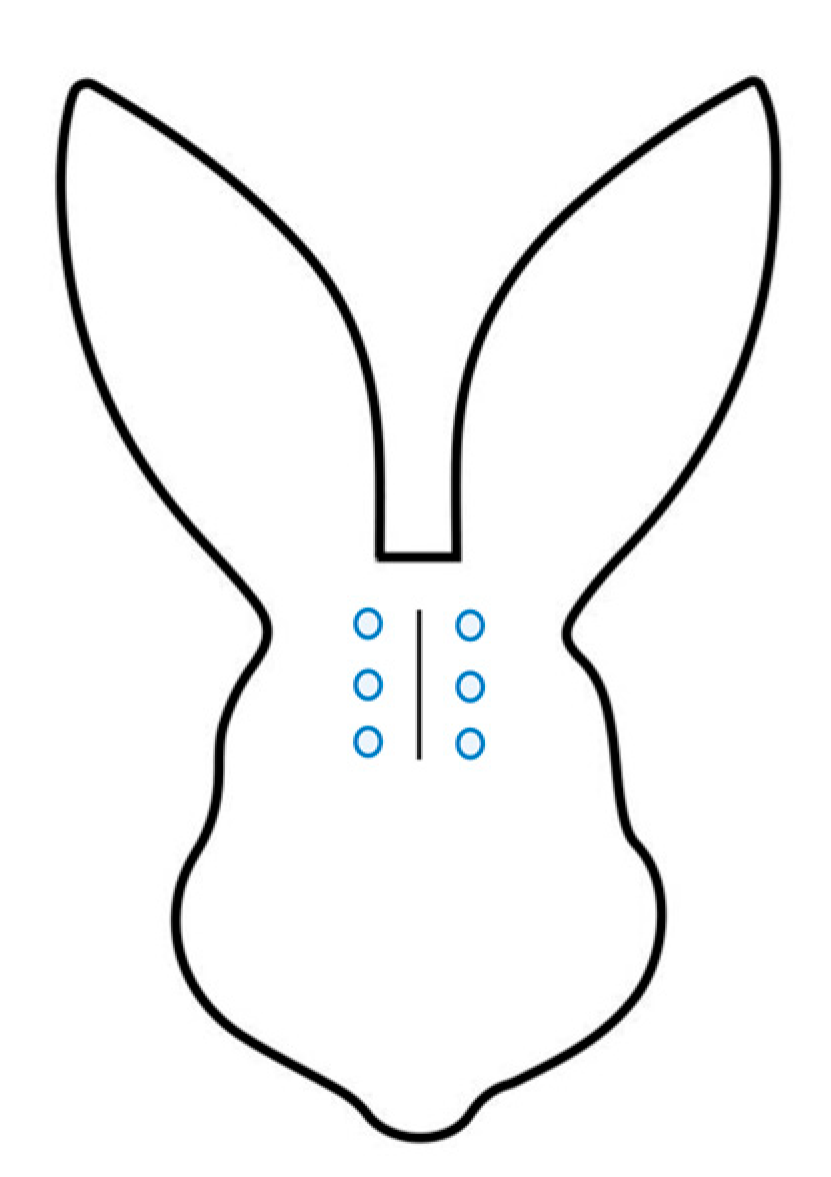
2.4. Surgery
2.5. Postoperative Management and Pain Assessment
2.6. Sample Size Calculation and Data Management
3. Results
3.1. Sedation, Intraoperative Nociception, and Respiratory Effects
3.2. Recovery and Postoperative Pain Assessment
4. Discussion
- (1)
- (2)
- The modality of pain assessment. Males were single-housed before and after the procedure. Single-housed rabbits are generally less active but more restless than are their group-housed counterparts [27] and tend to develop abnormal patterns of locomotion and resting [28]; therefore, falsely high pain scores could have been assigned. Moreover, the trial from Raillard et al. [7] was a descriptive trial and therefore not blinded, and the presence of multiple observers might also have acted as a confounder.
- (3)
- The differences in multimodal analgesic management. In our trial, meloxicam was injected IV at a dose of 0.5 mg kg−1. Meloxicam is a well used and tested NSAID in companion animals, including rabbits [29]; however, different dosages have been suggested. The most studied way of administration in rabbits is oral, and dosages up to 1.5 mg kg−1 have been tested [30]. Dosages of 0.2–0.3 mg Kg−1 were initially advised by Carpenter et al. [31], but later it was concluded from the same research group that a dose of 1 mg kg−1 PO may be necessary to achieve clinically effective circulating concentrations of meloxicam in rabbits [32]. The bioavailability of meloxicam in rabbits is not known, and the dosage of 1 mg kg−1 should be proven safe also if injected IV. Based on the current available data, though, it might be speculated that a dose of 0.3 mg kg−1 SC, used also by Raillard et al. [7], is insufficient for preventing postoperative inflammatory pain. Whether buprenorphine and meloxicam have a synergistic effect, as suggested by Goldschlager et al. [33], was not tested in surgical invasive models in rabbits and was not within the focus of our investigation. The role played by local anaesthesia in our results might be significant, but the little information available regarding ropivacaine in rabbits does not allow an extensive discussion or comparison with the effect of lidocaine. A long duration of sensitive nerve block (beyond 300 min) was found after injection of ropivacaine (0.4% up to 0.8 mL kg−1) for axillary brachial plexus nerve block in rabbits [34]. Ropivacaine (0.2%) injected intrathecally was deemed effective in 50% of rabbits but safe in terms of hemodynamic variations [35]. It can be expected that the injection of ropivacaine into the periosteum brought about more profound sensitive block than the sole peri-incisional injection of lidocaine. Periosteal single-injection blocks have been used in humans, with success, to reduce distal radius fractures [36,37] and sternal fractures [38], but evidence regarding rabbits is currently lacking. The antinociceptive effect of local analgesia might have contributed to blunt the intraoperative differences between group B and group M. However, the extent of this effect could only be proven by including in the study two further groups receiving methadone or buprenorphine without ropivacaine. Multimodal analgesia in rabbits is still a largely under-researched field [29]; however, it is recommended in many books, articles [4], and conference proceedings on rabbit pain and analgesia. As the beneficial effect of balanced anaesthesia and multimodal analgesia is well known in other species, and there is no evidence against it in rabbits, the authors did decide to stick to this approach; this was also carried out due to ethical concerns.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PK | Pharmacokinetic |
| ASA | American Society of Anesthesiologists physical status |
| EMLA | Eutectic mixture of local anaesthetics |
References
- ALURES Statistics. ALURES Statistics-Section 1: Numbers of Animals Used for Research, Testing, Routine Production and Education and Training Purposes—EU Statistics Database on the Use of Animals for Scientific Purposes. Available online: http://ec.europa.eu/eurostat/data/database (accessed on 20 February 2025).
- Hedenqvist, P.; Trbakovic, A.; Thor, A.; Ley, C.; Ekman, S.; Jensen-Waern, M. Carprofen neither reduces postoperative facial expression scores in rabbits treated with buprenorphine nor alters long term bone formation after maxillary sinus grafting. Res. Vet. Sci. 2016, 107, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Keown, A.J.; Farnworth, M.J.; Adams, N.J. Attitudes towards perception and management of pain in rabbits and guinea pigs by a sample of veterinarians in New Zealand. N. Z. Vet. J. 2011, 59, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Coulter, C.A.; Flecknell, P.A.; Leach, M.C.; Richardson, C.A. Reported analgesic administration to rabbits undergoing experimental surgical procedures. BMC Vet. Res. 2011, 21, 12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barter, L.S. Rabbit analgesia. Vet. Clin. N. Am. Exot. Anim. Pract. 2011, 14, 93–104. [Google Scholar] [CrossRef] [PubMed]
- KuKanich, B.; Wiese, A.J. Veterinary Anaesthesia and Analgesia, the Fifth Edition of Lumb and Jones; John Wiley & Sons: Hoboken, NJ, USA, 2015; pp. 220–221. [Google Scholar]
- Raillard, M.; Detotto, C.; Grepper, S.; Beslac, O.; Fujioka-Kobayashi, M.; Schaller, B.; Saulacic, N. Anaesthetic and Perioperative Management of 14 Male New Zealand White Rabbits for Calvarial Bone Surgery. Animals 2019, 9, 896. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Drewes, A.M.; Jensen, R.D.; Nielsen, L.M.; Droney, J.; Christrup, L.L.; Arendt-Nielsen, L.; Riley, J.; Dahan, A. Differences between opioids: Pharmacological, experimental, clinical and economical perspectives. Br. J. Clin. Pharmacol. 2013, 75, 60–78. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ebert, B.; Thorkildsen, C.; Andersen, S.; Christrup, L.L.; Hjeds, H. Opioid analgesics as noncompetitive N-methyl-D-aspartate (NMDA) antagonists. Biochem. Pharmacol. 1998, 56, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Touzot-Jourde, G.; Nino, V.; Holopherne-Doran, D. Comparison of methadone and morphine sedation and analgesia in the NZW rabbit: 24.6. J. Vet. Pharmacol. Ther. 2015, 38, 70–71. [Google Scholar]
- Di Girolamo, N.; Scarabelli, S. Practical approach to rabbits anaesthesia. In Proceedings of the ExoticsCon Virtual 2020, Virtual, 11 September–3 October 2020. [Google Scholar]
- Pathak, D.; Di Girolamo, N.; Maranville, R.; Womble, W.; Sypniewski, L.; Hanzlicek, A.; Brandão, J. Effects of injectable analgesics on selected gastrointestinal physiological parameters in rabbits. In Proceedings of the ExoticsCon Virtual 2020, Virtual, 11 September–3 October 2020. [Google Scholar]
- Randomization.com. Former. Available online: www.randomization.com (accessed on 30 August 2018).
- Bradbury, A.G.; Dickens, G.J. Appropriate handling of pet rabbits: A literature review. J. Small Anim. Pract. 2016, 57, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Raekallio, M.; Ansah, O.B.; Kuusela, E.; Vainio, O. Some factors influencing the level of clinical sedation induced by medetomidine in rabbits. J. Vet. Pharmacol. Therap. 2022, 25, 39–42. [Google Scholar] [CrossRef]
- Power and Sample Size. Compare 2 Proportions 2-Sample, 1-Sided|Power and Sample Size Calculators|HyLown. Available online: https://powerandsamplesize.com (accessed on 20 May 2018).
- Gardhouse, S.; Sanchez, A. Rabbit Sedation and Anesthesia. Vet. Clin. N. Am. Exot. Anim. Pract. 2022, 25, 181–210. [Google Scholar] [CrossRef] [PubMed]
- Flecknell, P.A.; Liles, J.H.; Wootton, R. Reversal of fentanyl/fluanisone neuroleptanalgesia in the rabbit using mixed agonist/antagonist opioids. Lab. Anim. 1989, 23, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Barter, L.S.; Hawkins, M.G.; Pypendop, B.H. Effects of fentanyl on isoflurane minimum alveolar concentration in New Zealand White rabbits (Oryctolagus cuniculus). Am. J. Vet. Res. 2015, 76, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Mofidi, A.; Vesal, N. Total intravenous anesthesia with Ketofol in rabbits: A comparison of the effects of constant rate infusion of midazolam, fentanyl or dexmedetomidine. BMC Vet. Res. 2024, 20, 253. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Costa, R.S.; Ciotti-McClallen, M.; Tilley, R.; Perry, S.; Maki, L.; Starks, D.; Stein, A.B. Intramuscular alfaxalone with or without buprenorphine or hydromorphone provides sedation with minimal adverse effects in healthy rabbits (Oryctolagus cuniculus) in a randomized blinded controlled trial. J. Am. Vet. Med. Assoc. 2022, 261, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Meredith, A. Bsava Small Animal Formulary. Part B: Exotic Pets, 9th ed.; BSAVA: England, UK, 2015. [Google Scholar]
- Pujol, J.; Vergneau-Grosset, C.; Beaudry, F.; Gaudette, F.; Vigneault, A.; Benedetti, I.C.C. Pharmacokinetics and innocuity of a single dose of intravenous, intramuscular, and subcutaneous methadone in the domestic rabbit (Oryctolagus cuniculus). J. Exot. Pet Med. 2023, 47, 41–46. [Google Scholar] [CrossRef]
- Askar, R.; Fredriksson, E.; Manell, E.; Hedeland, M.; Bondesson, U.; Bate, S.; Olsén, L.; Hedenqvist, P. Bioavailability of subcutaneous and intramuscular administrated buprenorphine in New Zealand White rabbits. BMC Vet. Res. 2020, 16, 436. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dong, H.; Sun, H.; Magal, E.; Ding, X.; Kumar, G.N.; Chen, J.J.; Johnson, E.J.; Manning, B.H. Inflammatory pain in the rabbit: A new, efficient method for measuring mechanical hyperalgesia in the hind paw. J. Neurosci. Methods 2008, 168, 76–87. [Google Scholar] [CrossRef] [PubMed]
- Sorge, R.E.; Totsch, S.K. Sex differences in Pain. J. Neurosci. Res. 2017, 95, 1271–1281. [Google Scholar] [CrossRef]
- Podberscek, A.L.; Blackshaw, J.K.; Beattie, A.W. The behavior of group penned and individually caged laboratory rabbits. Appl. Anim. Behav. Sci. 1991, 28, 353–363. [Google Scholar] [CrossRef]
- Di Vincenti, L., Jr.; Rehrig, A.N. The Social Nature of European Rabbits (Oryctolagus cuniculus). J. Am. Assoc. Lab. Anim. Sci. 2016, 55, 729–736. [Google Scholar] [PubMed] [PubMed Central]
- Benato, L.; Rooney, N.J.; Murrell, J.C. Pain and analgesia in pet rabbits within the veterinary environment: A review. Vet. Anaesth. Analg. 2019, 46, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.V.; Chen, H.C.; Taylor, W.M. Pharmacokinetics of meloxicam in rabbits after single and repeat oral dosing. Comp. Med. 2006, 56, 63–67. [Google Scholar] [PubMed]
- Carpenter, J.W.; Pollock, C.G.; Koch, D.E.; Hunter, R.P. Single and multiple-dose pharmacokinetics of meloxicam after oral administration to the rabbit (Oryctolagus cuniculus). J. Zoo. Wildl. Med. 2009, 40, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Fredholm, D.V.; Carpenter, J.W.; KuKanich, B.; Kohles, M. Pharmacokinetics of meloxicam in rabbits after oral administration of single and multiple doses. Am. J. Vet. Res. 2013, 74, 636–641. [Google Scholar] [CrossRef] [PubMed]
- Goldschlager, G.B.; Gillespie, V.L.; Palme, R.; Baxter, M.G. Effects of multimodal analgesia with Low Dose buprenorphine and meloxicam on fecal glucocorticoid metabolites after surgery in New Zealand white rabbits (Oryctolagus cuniculus). J. Am. Assoc. Lab. Anim. Sci. 2013, 52, 571–576. [Google Scholar] [PubMed] [PubMed Central]
- Fonseca, C.; Server, A.; Esteves, M.; Barastegui, D.; Rosal, M.; Fontecha, C.G.; Soldado, F. An ultrasound-guided technique for axillary brachial plexus nerve block in rabbits. Lab Anim. 2015, 44, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Malinovsky, J.M.; Charles, F.; Baudrimont, M.; Péréon, Y.; Le Corre, P.; Pinaud, M.; Benhamou, D. Intrathecal ropivacaine in rabbits: Pharmacodynamic and neurotoxicologic study. Anesthesiology 2002, 97, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Tageldin, M.E.; Alrashid, M.; Khoriati, A.A.; Gadikoppula, S.; Atkinson, H.D. Periosteal nerve blocks for distal radius and ulna fracture manipulation—The technique and early results. J. Orthop. Surg. Res. 2015, 10, 134. [Google Scholar] [CrossRef]
- Beck, S.; Brunner-Parker, A.; Stamm, R.; Douglas, M.; Conboy, A. Periosteal block versus intravenous regional anesthesia for reduction of distal radius fractures: A randomized controlled trial. Acad. Emerg. Med. 2022, 29, 1213–1220. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Eid, M.; Goodman, B.; Womack, J.; Paul, B. Periosteal Infusion of Local Anesthetics as an Alternative to Bilateral Subpectoral Interfascial Plane Catheters in Patients With Sternal Fractures. Reg. Anesth. Pain. Med. 2017, 42, 415–416. [Google Scholar] [CrossRef] [PubMed]
- Rousseau-Blass, F.; Pang, D.S. Hypoventilation following oxygen administration associated with alfaxalone-dexmedetomidine-midazolam anesthesia in New Zealand White rabbits. Vet. Anaesth. Analg. 2020, 47, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Murphy, K.L.; Roughan, J.V.; Baxter, M.G.; Flecknell, P.A. Anaesthesia with a combination of ketamine and medetomidine in the rabbit: Effect of premedication with buprenorphine. Vet. Anaesth. Analg. 2010, 37, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, C.A.; Smith, L.J. Respiratory rates and arterial blood-gas tensions in healthy rabbits given buprenorphine, butorphanol, midazolam, or their combinations. J. Am. Assoc. Lab. Anim. Sci. 2011, 50, 205–211. [Google Scholar] [PubMed] [PubMed Central]
- Pinho, R.H.; Justo, A.A.; Cima, D.S.; Fonseca, M.W.; Minto, B.W.; Rocha, F.D.L.; Leach, M.C.; Luna, S.P.L. Effects of Human Observer Presence on Pain Assessment Using Facial Expressions in Rabbits. J. Am. Assoc. Lab. Anim. Sci. 2023, 62, 81–86. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Parameter | Number of Animals with 20% Increase from Baseline Group M | Number of Animals with 20% Increase from Baseline Group B |
|---|---|---|
| HR | 1 | 1 |
| RR | 1 | 2 |
| BP | 0 | 0 |
| HR/RR | 1 | 2 |
| RR/BP | 2 | 1 |
| HR/BP | 0 | 1 |
| Parameter | Group M Median (Min–Max) n = 24 | Group B Median (Min–Max) n = 24 | p-Value |
|---|---|---|---|
| pH | 7.289 (7.233–7.379) | 7.293 (7.166–7.384) | 0.635 |
| FiO2 | 0.95 (86–98) | 0.95 (91–100) | 0.704 |
| paO2 (mmHg) | 365.5 (107–433) | 313 (90.8–441) | 0.132 |
| PaCO2 (mmHg) | 69.05 (51.5–98.3) | 74.1 (57.8–103) | 0.122 |
| cBase (Ecf)c | 7.6 (0.8–15) | 9 (3.1–15.6) | 0.03 * |
| cGlucose (mmol/L) | 16.65 (12.5–21.7) | 17.1 (14.3–20.6) | 0.248 |
| cLactate (mmol/L) | 0.5 (0.3–1.5) | 0.4 (0.2–1.2) | 0.453 |
| Time Point | Group M Median (Min–Max) | n = Number of Observations | Group B Median (Min–Max) | n = Number of Observations | p-Value (Mann Whitney Runk Sum Test) |
|---|---|---|---|---|---|
| sternal | 2 (1–3) | 24 | 2 (1–3) | 24 | 0.169 |
| 2 h | 2 (0–5) | 24 | 2 (0–6) | 24 | 0.228 |
| 4 h | 2 (1–4) | 20 | 1.5 (0–3) | 22 | 0.023 * |
| 6 h | 2 (0–5) | 17 | 1 (0–5) | 22 | 0.108 |
| 8 h | 2 (1–5) | 15 | 1 (0–3) | 21 | 0.014 * |
| 12 h | 1.5 (0–3) | 12 | 1 (0–3) | 18 | 0.471 |
| Parameter | Group M Median (Min–Max) n = 13 | Group B Median (Min–Max) n = 16 | p-Value |
|---|---|---|---|
| pH | 7.441 (7.354–7.520) | 7.444 (7.388–7.588) | 0.854 |
| PaCO2 (mmHg) | 52.5 (39.9–59.5) | 55.7 (45.6–63.2) | 0.28 |
| cBase (Ecf)c | 12.6 (6.75–14.75) | 13.85 (12.725–16.325) | 0.065 |
| cGlucose (mmol/L) | 17.4 (15.95–19.4) | 17.95 (17.4–19.8) | 0.312 |
| cLactate (mmol/L) | 1 (0.55–1.45) | 0.7 (0.625–875) | 0.376 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casoni, D.; Parodi, C.; Garcia Casalta, L.G.; Nettelbeck, K.; Spadavecchia, C. Buprenorphine Versus Methadone in Female New Zealand White Rabbits Undergoing Balanced Anaesthesia for Calvaria Surgery. Animals 2025, 15, 1843. https://doi.org/10.3390/ani15131843
Casoni D, Parodi C, Garcia Casalta LG, Nettelbeck K, Spadavecchia C. Buprenorphine Versus Methadone in Female New Zealand White Rabbits Undergoing Balanced Anaesthesia for Calvaria Surgery. Animals. 2025; 15(13):1843. https://doi.org/10.3390/ani15131843
Chicago/Turabian StyleCasoni, Daniela, Chiara Parodi, Luisana Gisela Garcia Casalta, Kay Nettelbeck, and Claudia Spadavecchia. 2025. "Buprenorphine Versus Methadone in Female New Zealand White Rabbits Undergoing Balanced Anaesthesia for Calvaria Surgery" Animals 15, no. 13: 1843. https://doi.org/10.3390/ani15131843
APA StyleCasoni, D., Parodi, C., Garcia Casalta, L. G., Nettelbeck, K., & Spadavecchia, C. (2025). Buprenorphine Versus Methadone in Female New Zealand White Rabbits Undergoing Balanced Anaesthesia for Calvaria Surgery. Animals, 15(13), 1843. https://doi.org/10.3390/ani15131843






