Self-Reported Utilization of International (ACVIM Consensus) Guidelines and the Latest Clinical Trial Results on the Treatment of Dogs with Various Stages of Myxomatous Mitral Valve Degeneration: A Survey among Veterinary Practitioners
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
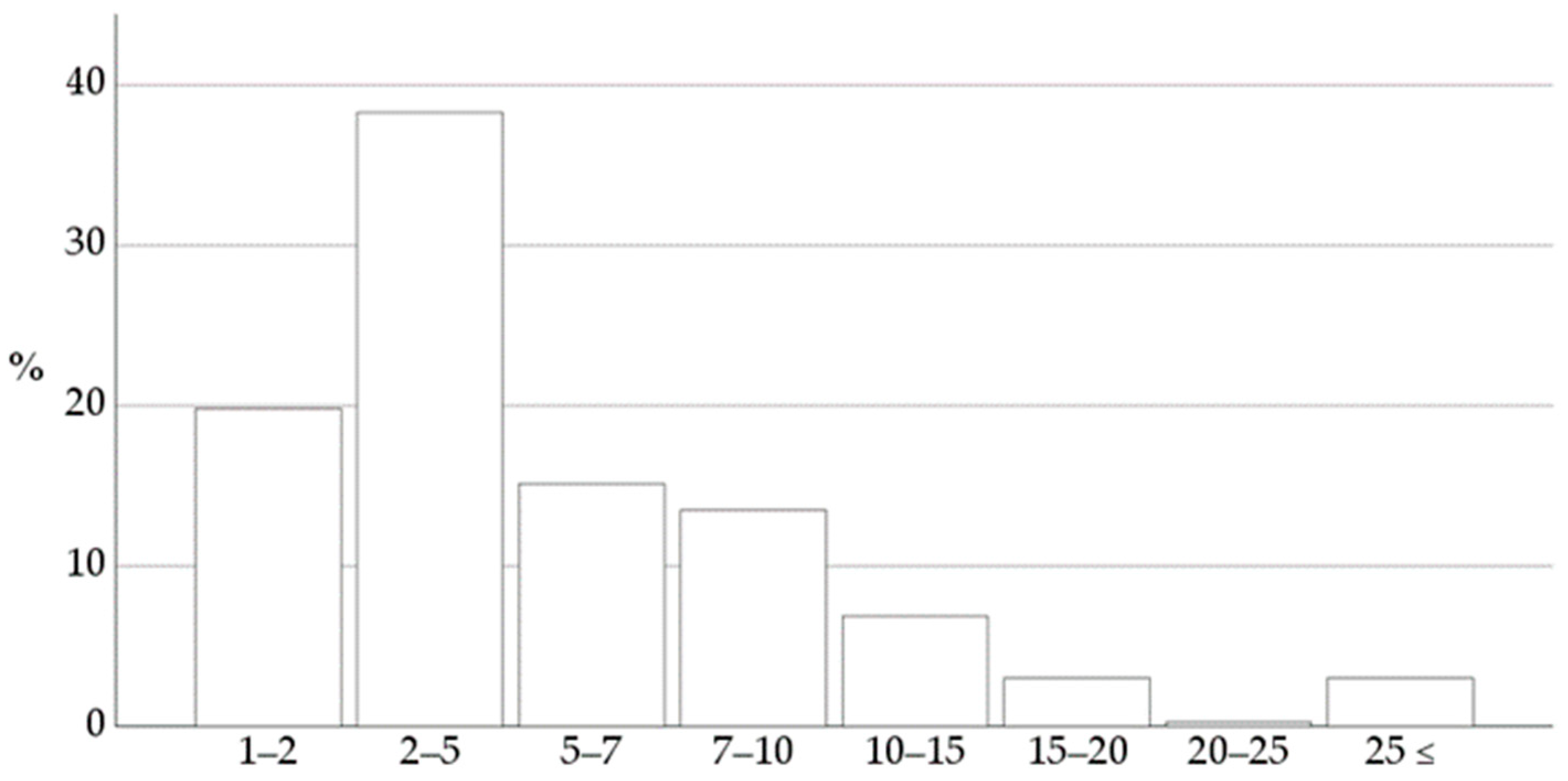
3.1. Characteristics of Respondents
3.2. Utilizing the ACVIM Consensus Guidelines for Staging of Myxomatous Mitral Valve Degeneration
3.3. Pharmacological Recommendation for Dogs with Myxomatous Mitral Valve Degeneration
3.3.1. Pimobendan
3.3.2. Angiotensin-Converting Enzyme Inhibitors
3.4. Treatment Recommendations for Dogs with Stage B1 Degenerative Mitral Valve Disease
3.5. Treatment Recommendations for Dogs with Stage B2 Degenerative Mitral Valve Disease
3.6. Treatment Recommendations for Dogs with Stage C Degenerative Mitral Valve Disease
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Borgarelli, M.; Buchanan, J.W. Historical review, epidemiology and natural history of degenerative mitral valve disease. J. Vet. Cardiol. 2012, 14, 93–101. [Google Scholar] [CrossRef]
- Mattin, M.J.; Boswood, A.; Church, D.B.; Brodbelt, D.C. Prognostic factors in dogs with presumed degenerative mitral valve disease attending primary-care veterinary practices in the United Kingdom. J. Vet. Intern. Med. 2018, 33, 432–444. [Google Scholar] [CrossRef]
- Ljungvall, I.; Rishniw, M.; Porciello, F.; Ferasin, L.; Ohad, D.G. Murmur intensity in small-breed dogs with myxomatous mitral valve disease reflects disease severity. J. Small Anim. Pract. 2014, 55, 545–550. [Google Scholar] [CrossRef]
- Keene, B.W.; Atkins, C.E.; Bonagura, J.D.; Fox, P.R.; Häggström, J.; Fuentes, V.L.; Oyama, M.A.; Rush, J.E.; Stepien, R.; Uechi, M. ACVIM consensus guidelines for the diagnosis and treatment of myxomatous mitral valve disease in dogs. J. Vet. Intern. Med. 2019, 33, 1127–1140. [Google Scholar] [CrossRef]
- Franchini, A.; Abbott, J.A.; Tyrrell, W.; Rosenthal, S.; Lahmers, S.; Menciotti, G.; Crosara, S.; Häggström, J.; Borgarelli, M. Predictors of reoccurrence of congestive signs within 180 days after successful treatment of the first episode of congestive heart failure in dogs with myxomatous mitral valve disease. J. Vet. Cardiol. 2021, 34, 112–119. [Google Scholar] [CrossRef]
- Gordon, S.G.; Saunders, A.B.; Wesselowski, S.R. Asymptomatic canine degenerative valve disease: Diagnosis and current and future therapies. Vet. Clin. N. Am. Small Anim. Pract. 2022, 52, 819–840. [Google Scholar] [CrossRef]
- Borgarelli, M.; Savarino, P.; Crosara, S.; Santilli, R.A.; Chiavegato, D.; Poggi, M.; Bellino, C.; La Rosa, G.; Zanatta, R.; Haggstrom, J.; et al. Survival characteristics and prognostic variables of dogs with mitral regurgitation attributable to myxomatous valve disease. J. Vet. Intern. Med. 2008, 22, 120–128. [Google Scholar] [CrossRef]
- Boswood, A.; Häggström, J.; Gordon, S.G.; Wess, G.; Stepien, R.L.; Oyama, M.A.; Keene, B.W.; Bonagura, J.; MacDonald, K.A.; Patteson, M.; et al. Effect of pimobendan in dogs with preclinical myxomatous mitral valve disease and cardiomegaly: The EPIC study—A randomized clinical trial. J. Vet. Intern. Med. 2016, 30, 1765–1779. [Google Scholar] [CrossRef]
- Boswood, A.; Gordon, S.G.; Häggström, J.; Wess, G.; Stepien, R.L.; Oyama, M.A.; Keene, B.W.; Bonagura, J.; MacDonald, K.A.; Patteson, M.; et al. Longitudinal analysis of quality of life, clinical, radiographic, echocardiographic, and laboratory variables in dogs with preclinical myxomatous mitral valve disease receiving pimobendan or placebo: The EPIC study. J. Vet. Intern. Med. 2018, 32, 72–85. [Google Scholar] [CrossRef]
- Borgarelli, M.; Ferasin, L.; Lamb, K.; Bussadori, C.; Chiavegato, D.; D’Agnolo, G.; Migliorini, F.; Poggi, M.; Santilli, R.A.; Guillot, E.; et al. DELay of appearance of symptoms of canine degenerative mitral valve disease treated with spironolactone and benazepril: The DELAY study. J. Vet. Cardiol. 2020, 27, 34–53. [Google Scholar] [CrossRef]
- Kvart, C.; Häggström, J.; Pedersen, H.D.; Hansson, K.; Eriksson, A.; Järvinen, A.K.; Tidholm, A.; Bsenko, K.; Ahlgren, E.; Ilves, M.; et al. Efficacy of enalapril for prevention of congestive heart failure in dogs with myxomatous valve disease and asymptomatic mitral regurgitation. J. Vet. Intern. Med. 2002, 16, 80–88. [Google Scholar] [CrossRef]
- Atkins, C.E.; Keene, B.W.; Brown, W.A.; Coats, J.R.; Crawford, M.; DeFrancesco, T.C.; Edwards, N.J.; Fox, P.R.; Lehmkuhl, L.B.; Luethy, M.W.; et al. Results of the veterinary enalapril trial to prove reduction in onset of heart failure in dogs chronically treated with enalapril alone for compensated, naturally occurring mitral valve insufficiency. J. Am. Vet. Med. Assoc. 2007, 231, 1061–1069. [Google Scholar] [CrossRef]
- Bernay, F.; Bland, J.M.; Häggström, J.; Baduel, L.; Combes, B.; Lopez, A.; Kaltsatos, V. Efficacy of spironolactone on survival in dogs with naturally occurring mitral regurgitation caused by myxomatous mitral valve disease. J. Vet. Intern. Med. 2010, 24, 331–341. [Google Scholar] [CrossRef]
- Häggström, J.; Boswood, A.; O’grady, M.; Jöns, O.J.; Smith, S.; Swift, S.; Borgarelli, M.; Gavaghan, B.; Kresken, J.-G.; Patteson, M.; et al. Effect of pimobendan or benazepril hydrochloride on survival times in dogs with congestive heart failure caused by naturally occurring myxomatous mitral valve disease: The QUEST study. J. Vet. Intern. Med. 2008, 22, 1124–1135. [Google Scholar] [CrossRef]
- BENCH (BENazepril in Canine Heart disease) Study Group; Pouchelon, J.L.; King, J.; Martignoni, L.; Chetboul, V.; Lugardon, B.; Rousselot, J.F.; Corlouer, J.P.; Bussadori, C.; Piette, M.H.; et al. The Effect of benazepril on survival times and clinical signs of dogs with congestive heart failure: Results of a multicenter, prospective, randomized, double-blinded, placebo-controlled, long-term clinical trial. J. Vet. Cardiol. 1999, 1, 7–18. [Google Scholar] [CrossRef]
- Sisson, D.D. Acute and short-term hemodynamic, echocardiographic, and clinical effects of enalapril maleate in dogs with naturally acquired heart failure: Results of the Invasive Multicenter PROspective Veterinary Evaluation of Enalapril study: The IMPROVE Study Group. J. Vet. Intern. Med. 1995, 9, 234–242. [Google Scholar] [CrossRef]
- Besche, B.; Blondel, T.; Guillot, E.; Garelli-Paar, C.; Oyama, M.A. Efficacy of oral torasemide in dogs with degenerative mitral valve disease and new onset congestive heart failure: The CARPODIEM study. J. Vet. Intern. Med. 2020, 34, 1746–1758. [Google Scholar] [CrossRef]
- Wess, G.; Kresken, J.G.; Wendt, R.; Gaugele, J.; Killich, M.; Keller, L.; Simak, J.; Holler, P.; Bauer, A.; Küchenhof, H.; et al. Efficacy of adding ramipril (VAsotop) to the combination of furosemide (Lasix) and pimobendan (VEtmedin) in dogs with mitral valve degeneration: The VALVE trial. J. Vet. Intern. Med. 2020, 34, 2232–2241. [Google Scholar] [CrossRef]
- Coffman, M.; Guillot, E.; Blondel, T.; Garelli-Paar, C.; Feng, S.; Heartsill, S.; Atkins, C.E. Clinical efficacy of a benazepril and spironolactone combination in dogs with congestive heart failure due to myxomatous mitral valve disease: The BEnazepril Spironolactone STudy (BESST). J. Vet. Intern. Med. 2021, 35, 1673–1687. [Google Scholar] [CrossRef]
- Peddle, G.D.; Singletary, G.E.; Reynolds, C.A.; Trafny, D.J.; MacHen, M.C.; Oyama, M.A. Effect of torsemide and furosemide on clinical, laboratory, radiographic and quality of life variables in dogs with heart failure secondary to mitral valve disease. J. Vet. Cardiol. 2012, 14, 253–259. [Google Scholar] [CrossRef]
- BENCH (BENazepril in Canine Heart disease) Study Group; Pouchelon, J.L.; King, J.; Martignoni, L.; Chetboul, V.; Lugardon, B.; Rousselot, J.F.; Corlouer, J.P.; Bussadori, C.; Piette, M.H.; et al. Long-term tolerability of benazepril in dogs with congestive heart failure. J. Vet. Cardiol. 2004, 6, 7–13. [Google Scholar] [CrossRef]
- Ettinger, S.J.; Benitz, A.M.; Ericsson, G.F.; Cifelli, S.; Jernigan, A.D.; Longhofer, S.L.; Trimboli, W.; Hanson, P.D. Effects of enalapril maleate on survival of dogs with naturally acquired heart failure. The Long-Term Investigation of Veterinary Enalapril (LIVE) Study Group. J. Am. Vet. Med. Assoc. 1998, 213, 1573–1577. [Google Scholar] [CrossRef]
- Allen, J.W.; Phipps, K.L.; Llamas, A.A.; Barrett, K.A. Left atrial decompression as a palliative minimally invasive treatment for congestive heart failure caused by myxomatous mitral valve disease in dogs: 17 cases (2018–2019). J. Am. Vet. Med. Assoc. 2021, 258, 638–647. [Google Scholar] [CrossRef]
- Atkins, C.; Bonagura, J.; Ettinger, S.; Fox, P.; Gordon, S.; Häggström, J.; Hamlin, R.; Keene, B.; Luis-Fuentes, V.; Stepien, R. Guidelines for the diagnosis and treatment of canine chronic valvular heart disease. J. Vet. Intern. Med. 2009, 23, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- van Staveren, M.D.B.; Muis, E.; Szatmári, V. Self-reported utilization of international guidelines for staging dogs with myxomatous mitral valve degeneration: A survey among veterinary practitioners. Vet. Sci. 2023, 10, 687. [Google Scholar] [CrossRef] [PubMed]
- van Vuuren, D.; Vlaanderen, M.; Pomp, M.; Geelen, J. SEO Arbeidsmarkt Dierenartsen. Available online: www.seo.nl (accessed on 4 January 2024).
- Buchanan, J.W.; Bücheler, J. Vertebral scale system to measure canine heart size in radiographs. J. Am. Vet. Med. Assoc. 1995, 206, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Malcolm, E.L.; Visser, L.C.; Philips, K.L.; Johnson, L.R. Diagnostic value of vertebral left atrial size as determined from thoracic radiographs for assessment of left atrial size in dogs with myxomatous mitral valve disease. J. Am. Vet. Med. Assoc. 2018, 253, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Wesselowski, S.; Gordon, S.G.; Meddaugh, N.; Saunders, A.B.; Häggström, J.; Cusack, K.; Janacek, B.W.; Matthews, D.J. Prediction of clinically important acquired cardiac disease without an echocardiogram in large breed dogs using a combination of clinical, radiographic and electrocardiographic variables. J. Vet. Cardiol. 2022, 40, 126–141. [Google Scholar] [CrossRef] [PubMed]
- Wilshaw, J.; Rosenthal, S.L.; Wess, G.; Dickson, D.; Bevilacqua, L.; Dutton, E.; Deinert, M.; Abrantes, R.; Schneider, I.; Oyama, M.A.; et al. Accuracy of history, physical examination, cardiac biomarkers, and biochemical variables in identifying dogs with stage B2 degenerative mitral valve disease. J. Vet. Intern. Med. 2021, 35, 755–770. [Google Scholar] [CrossRef]
- Rasmussen, C.E.; Falk, T.; Zois, N.E.; Moesgaard, S.G.; Häggström, J.; Pedersen, H.D.; Åblad, B.; Nilsen, H.Y.; Olsen, L.H. Heart rate, heart rate variability, and arrhythmias in dogs with myxomatous mitral valve disease. J. Vet. Intern. Med. 2012, 26, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Baisan, R.A.; Vulpe, V.; Ohad, D.G. Short-term heart rate variability in healthy dogs and dogs in various stages of degenerative mitral valve disease evaluated before pharmacotherapy. Vet. J. 2021, 274, 105704. [Google Scholar] [CrossRef] [PubMed]
- Häggström, J.; Hamlin, R.L.; Hansson, K.; Kvart, C. Heart rate variability in relation to severity of mitral regurgitation in Cavalier King Charles spaniels. J. Small Anim. Pract. 1996, 37, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Ineson, D.L.; Freeman, L.M.; Rush, J.E. Clinical and laboratory findings and survival time associated with cardiac cachexia in dogs with congestive heart failure. J. Vet. Intern. Med. 2019, 33, 1902–1908. [Google Scholar] [CrossRef] [PubMed]
- Häggström, J.; Kvart, C.; Hansson, K. Heart sounds and murmurs: Changes related to severity of chronic valvular disease in the Cavalier King Charles spaniel. J. Vet. Intern. Med. 1995, 9, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Duler, L.; Visser, L.C.; Jackson, K.N.; Phillips, K.L.; Pollard, R.E.; Wanamaker, M.W. Evaluation of radiographic predictors of left heart enlargement in dogs with known or suspected cardiovascular disease. Vet. Radiol. Ultrasound 2021, 62, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Ross, E.S.; Visser, L.C.; Sbardellati, N.; Potter, B.M.; Ohlendorf, A.; Scansen, B.A. Utility of vertebral left atrial size and vertebral heart size to aid detection of congestive heart failure in dogs with respiratory signs. J. Vet. Intern. Med. 2023, 37, 2021–2029. [Google Scholar] [CrossRef] [PubMed]
- Lofstedt, J. Confidence and competence of recent veterinary graduates—Is there a problem? Can. Vet. J. 2003, 44, 359–360. [Google Scholar] [PubMed]
- Bode, E.F.; Mederska, E.; Hodgkiss-Geere, H.; Radford, A.D.; Singleton, D.A. Analysis of canine cardiovascular therapeutic agent prescriptions using electronic health records in primary care veterinary practices in the United Kingdom. J. Vet. Cardiol. 2022, 39, 35–45. [Google Scholar] [CrossRef]
- Klein, S.; Nolte, I.; Rumstedt, K.; Sehn, M.; Raue, J.F.; Weiner, F.; Treese, J.S.; Beyerbach, M.; Bach, J.-P. The effect of treatment with pimobendan in dogs with preclinical mitral valve disease—A placebo-controlled double-blinded crossover study. BMC Vet. Res. 2021, 17, 310. [Google Scholar] [CrossRef]
- Oyama, M.A.; Scansen, B.A.; Boswood, A.; Goldfeder, G.; Rosenthal, S.; Cober, R.; LaFauci, K.; Friese, R.C.; Gomes, M.; Chang, Y.R.; et al. Effect of a specially formulated diet on progression of heart enlargement in dogs with subclinical degenerative mitral valve disease. J. Vet. Intern. Med. 2023, 37, 1323–1330. [Google Scholar] [CrossRef]
- Wesselowski, S.; Blake, A.B.; Gordon, S.G.; Suchodolski, J.S.; Steiner, J.M. Whole blood and plasma taurine reference intervals in adult Cavalier King Charles Spaniels and correlations between taurine concentration, diet and mitral valve disease. J. Am. Vet. Med. Assoc. 2022, 260, S71–S76. [Google Scholar] [CrossRef] [PubMed]
- Chetboul, V.; Lefebvre, H.P.; Sampedrano, C.C.; Gouni, V.; Saponaro, V.; Serres, F.; Concordat, D.; Nicolle, A.P.; Pouchelon, J. Comparative adverse cardiac effects of pimobendan and benazepril monotherapy in dogs with mild degenerative mitral valve disease: A prospective, controlled, blinded, and randomized study. J. Vet. Intern. Med. 2007, 21, 742–753. [Google Scholar] [CrossRef]
- Franchini, A.; Borgarelli, M.; Abbott, J.A.; Menciotti, G.; Crosara, S.; Häggström, J.; Lahmers, S.; Rosenthal, S.; Tyrrell, W. The Longitudinal Outcome Of canine (K9) myxomatous Mitral valve disease (LOOK-Mitral) registry: Baseline treatment characteristics. J. Vet. Cardiol. 2022, 41, 99–120. [Google Scholar] [CrossRef]
- Donati, P.; Tarducci, A.; Zanatta, R.; Verdier, N.; Belerenian, G.; Cordero, I.; Villalta, C.; Franco, J.; Tarragona, L. Angiotensin-converting enzyme inhibitors in preclinical myxomatous mitral valve disease in dogs: Systematic review and meta-analysis. J. Small Anim. Pract. 2022, 63, 362–371. [Google Scholar] [CrossRef]
- Hammond, H.H.; Ames, M.K.; Domenig, O.; Scansen, B.A.; Tsang Yang, N.; Wilson, M.D.; Sunshine, E.; Brunk, K.; Masters, A. The classical and alternative circulating renin-angiotensin system in normal dogs and dogs with stage B1 and B2 myxomatous mitral valve disease. J. Vet. Intern. Med. 2023, 37, 875–886. [Google Scholar] [CrossRef] [PubMed]
- Häggström, J.; Hansson, K.; Karlberg, B.E.; Kvart, C.; Madej, A.; Olsson, K. Effects of long-term treatment with enalapril or hydralazine on the renin-angiotensin-aldosterone system and fluid balance in dogs with naturally acquired mitral valve regurgitation. Am. J. Vet. Res. 1996, 57, 1645–1652. [Google Scholar] [CrossRef] [PubMed]
- Ames, M.K.; Atkins, C.E.; Pitt, B. The renin-angiotensin-aldosterone system and its suppression. J. Vet. Intern. Med. 2019, 33, 363–382. [Google Scholar] [CrossRef] [PubMed]
- Kittleson, M.D.; Bonagura, J.D. Letter to the editor. J. Vet. Intern. Med. 2010, 24, 1245–1246. [Google Scholar] [CrossRef]
- Ames, M.K.; Atkins, C.E.; Eriksson, A.; Hess, A.M. Aldosterone breakthrough in dogs with naturally occurring myxomatous mitral valve disease. J. Vet. Cardiol. 2017, 19, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Uechi, M.; Matsuoka, M.; Kuwajima, E.; Kaneko, T.; Yamashita, K.; Fukushima, U.; Ishikawa, Y. The effects of the loop diuretics furosemide and torasemide on diuresis in dogs and cats. J. Vet. Med. Sci. 2003, 65, 1057–1061. [Google Scholar] [CrossRef] [PubMed]
- Knauf, H.; Mutschler, E. Clinical pharmacokinetics and pharmacodynamics of torasemide. Clin. Pharma 1998, 34, 1–24. [Google Scholar] [CrossRef] [PubMed]
- MSD Manual. Available online: https://www.msdvetmanual.com/pharmacology/systemic-pharmacotherapeutics-of-the-cardiovascular-system/diuretics-for-use-in-animals (accessed on 14 December 2023).
- Wess, G.; Glaus, T. Response to letter to the editor regarding “Efficacy of adding ramipril (VAsotop) to the combination of furosemide (Lasix) and pimobendan (VEtmedin) in dogs with mitral valve degeneration: The VALVE trial”. J. Vet. Intern. Med. 2021, 35, 700–702. [Google Scholar] [CrossRef] [PubMed]
- Chetboul, V.; Pouchelon, J.-L.; Menard, J.; Blanc, J.; Desquilbet, L.; Petit, A.; Rougier, S.; Lucats, L.; Woehrle, F. Short-term efficacy and safety of torasemide and furosemide in 366 dogs with degenerative mitral valve disease: The TEST Study. J. Vet. Intern. Med. 2017, 31, 1629–1642. [Google Scholar] [CrossRef]
- Griffiths, L.G.; Orton, C.E.; Boon, J.A. Evaluation of techniques and outcomes of mitral valve repair in dogs. J. Am. Vet. Med. Assoc. 2004, 224, 1941–1945. [Google Scholar] [CrossRef]
- Uechi, M.; Mizukoshi, T.; Mizuno, T.; Mizuno, M.; Harada, K.; Ebisawa, T.; Takeuchi, J.; Sawada, T.; Uchida, S.; Shinoda, A.; et al. Mitral valve repair under cardiopulmonary bypass in small-breed dogs: 48 cases (2006–2009). J. Am. Vet. Med. Assoc. 2012, 240, 1194–1201. [Google Scholar] [CrossRef]
- Matsuura, K.; Yoshida, T.; Yamada, S.; Aboshi, Y.; Yotsuida, H.; Yaginuma, Y.; Hasegawa, M. The outcome of surgical mitral valve repair with loop-in-loop technique in dogs with different stage myxomatous mitral valve disease. J. Vet. Cardiol. 2022, 42, 74–82. [Google Scholar] [CrossRef]
- Bristow, P.; Markovic, L.E. Mitral valve repair—The development and rise of options in the veterinary world. Vet. Clin. N. Am. Small Anim. Pract. 2023, 53, 1343–1352. [Google Scholar] [CrossRef]
- Liu, B.; Leach, S.B.; Pan, W.; Zheng, F.; Jia, L.; Zhou, X.; Li, J. Preliminary outcome of a novel edge-to-edge closure device to manage mitral regurgitation in dogs. Front. Vet. Sci. 2020, 7, 597879. [Google Scholar] [CrossRef]
| Stage B1 MMVD | Survey Respondents | ACVIM Guidelines, 2019 |
|---|---|---|
| No therapy | 93% | 100% |
| Therapy | 7% | 0% |
| Pimobendan | 93% | |
| ACE inhibitors | 0% | |
| Loop diuretics | 15% | |
| Spironolactone | 0% |
| Stage B2 MMVD | Survey Respondents | ACVIM Guidelines, 2019 |
|---|---|---|
| Therapy: Yes | 84% | 100% |
| Pimobendan total | 98% | 100% |
| Pimobendan monotherapy | 81% | 50% of panelists |
| ACE inhibitors total | 4% | 50% of panelists |
| ACE inhibitor monotherapy | 1% | 0% |
| Loop diuretics total | 14% | 0% |
| Loop diuretics monotherapy | 1% | 0% |
| Spironolactone total | 1% | 0% |
| Spironolactone monotherapy | 0% | 0% |
| Combinations | ||
| Pimobendan + loop diuretic | 13% | 0% |
| Pimobendan + ACE inhibitor | 2% | 50% |
| Pimobendan + ACE inhibitor + loop diuretic | 1% | 0% |
| Pimobendan + loop diuretic + spironolactone | 1% | 0% |
| Stage C MMVD | Survey Respondents | ACVIM Guidelines, 2019 |
|---|---|---|
| Therapy: Yes | 100% | 100% |
| Pimobendan (pimo) total | 78% | 100% |
| ACE inhibitors (ACE-i) total | 17% | 100% |
| Loop diuretics total | 100% | 100% |
| Furosemide (furo) | 82% | 100% |
| Torasemide (tora) | 36% | Some cases instead of furosemide |
| Spironolactone (spiro) total | 11% | Adjunct therapy |
| Combinations: | ||
| Pimo + furo | 35% | 0% |
| Pimo + tora | 13% | 0% |
| Pimo + furo + tora | 9% | 0% |
| Pimo + ACE-i + furo | 9% | 100% |
| Furo + tora | 4% | 0% |
| Pimo + ACE-i + furo + spiro | 3% | Adjunct therapy |
| Pimo + furo + spiro | 3% | 0% |
| Pimo + ACE-i + furo + spiro + tora | 2% | 0% |
| Pimo + furo + spiro + tora | 2% | 0% |
| ACE-i + furo | 2% | 0% |
| Pimo + ACE-i + furo + tora | 1% | 0% |
| Pimo + ACE-i + spiro + tora | 1% | Some cases |
| Pimo + ACE-i + tora | 1% | Some cases |
| Pimo + spiro + tora | 1% | 0% |
| Furo + spiro + tora | 1% | 0% |
| ACE-i + tora | 0.3% | 0% |
| Other: | For atrial fibrillation | |
| Euthanasia | 2% | |
| Digoxin | 0.3% | |
| Immediate referral | 0.3% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Staveren, M.D.B.; Muis, E.; Szatmári, V. Self-Reported Utilization of International (ACVIM Consensus) Guidelines and the Latest Clinical Trial Results on the Treatment of Dogs with Various Stages of Myxomatous Mitral Valve Degeneration: A Survey among Veterinary Practitioners. Animals 2024, 14, 772. https://doi.org/10.3390/ani14050772
van Staveren MDB, Muis E, Szatmári V. Self-Reported Utilization of International (ACVIM Consensus) Guidelines and the Latest Clinical Trial Results on the Treatment of Dogs with Various Stages of Myxomatous Mitral Valve Degeneration: A Survey among Veterinary Practitioners. Animals. 2024; 14(5):772. https://doi.org/10.3390/ani14050772
Chicago/Turabian Stylevan Staveren, Marie D. B., Esther Muis, and Viktor Szatmári. 2024. "Self-Reported Utilization of International (ACVIM Consensus) Guidelines and the Latest Clinical Trial Results on the Treatment of Dogs with Various Stages of Myxomatous Mitral Valve Degeneration: A Survey among Veterinary Practitioners" Animals 14, no. 5: 772. https://doi.org/10.3390/ani14050772
APA Stylevan Staveren, M. D. B., Muis, E., & Szatmári, V. (2024). Self-Reported Utilization of International (ACVIM Consensus) Guidelines and the Latest Clinical Trial Results on the Treatment of Dogs with Various Stages of Myxomatous Mitral Valve Degeneration: A Survey among Veterinary Practitioners. Animals, 14(5), 772. https://doi.org/10.3390/ani14050772







