Bacterial Meningitis in Buffaloes in Brazil
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
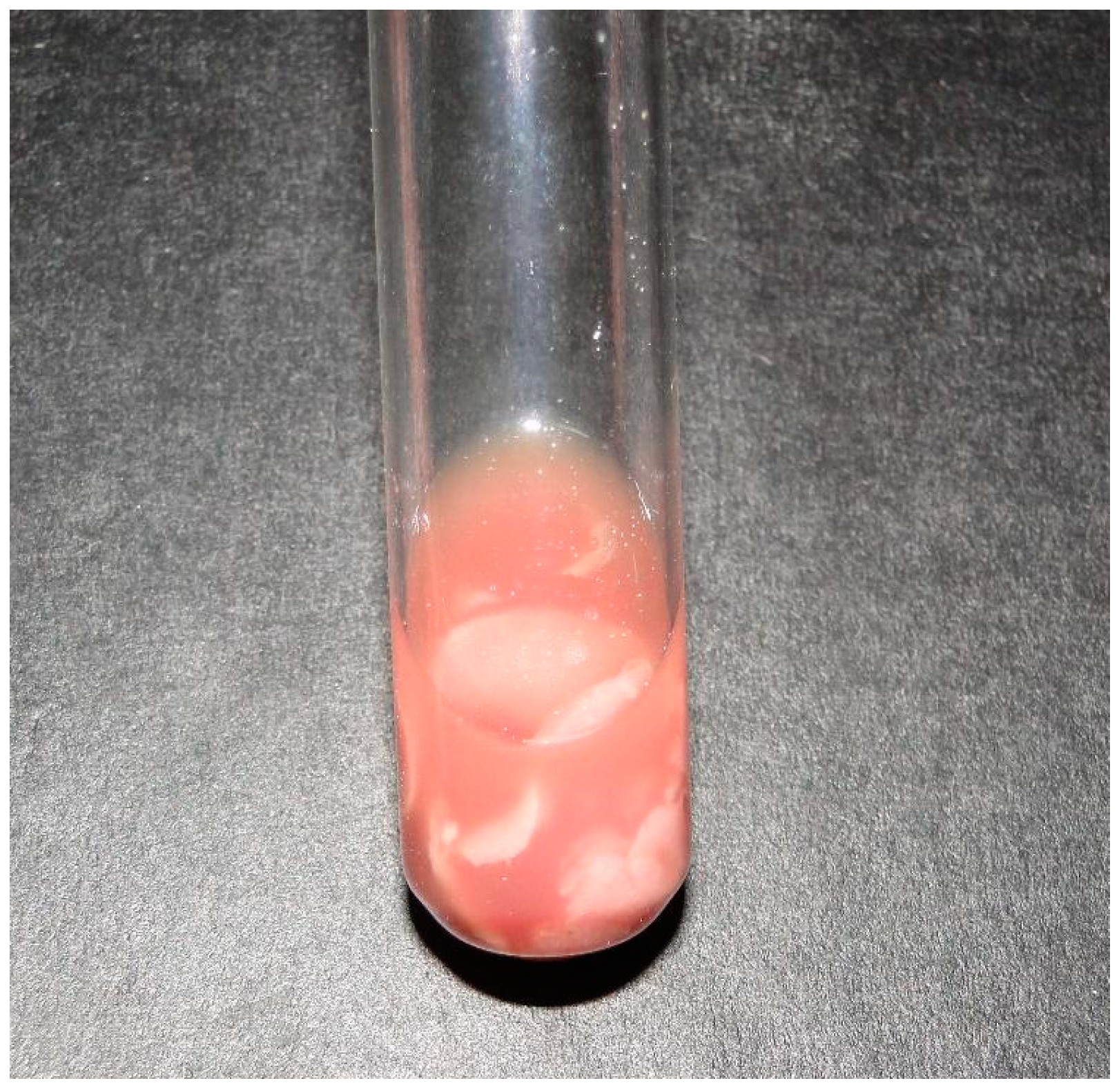
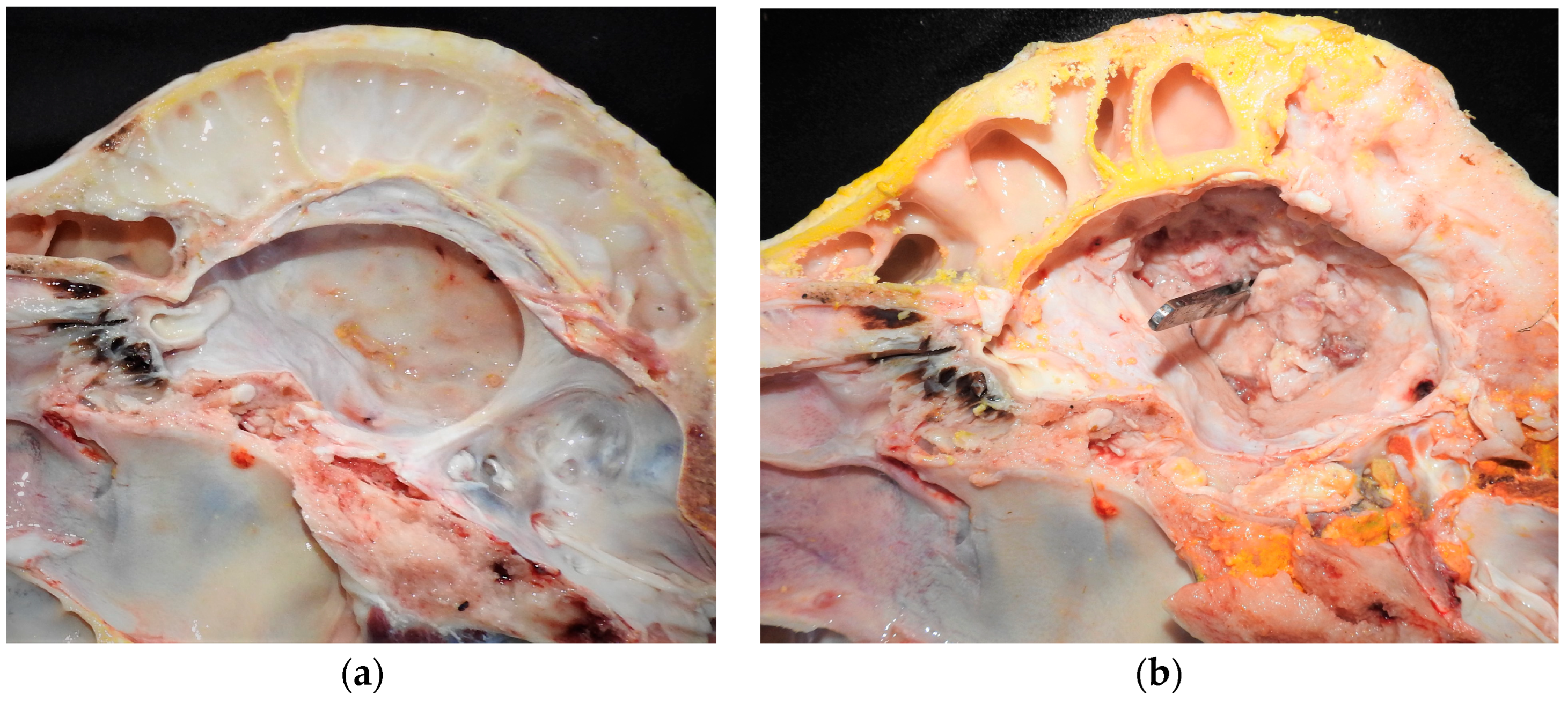
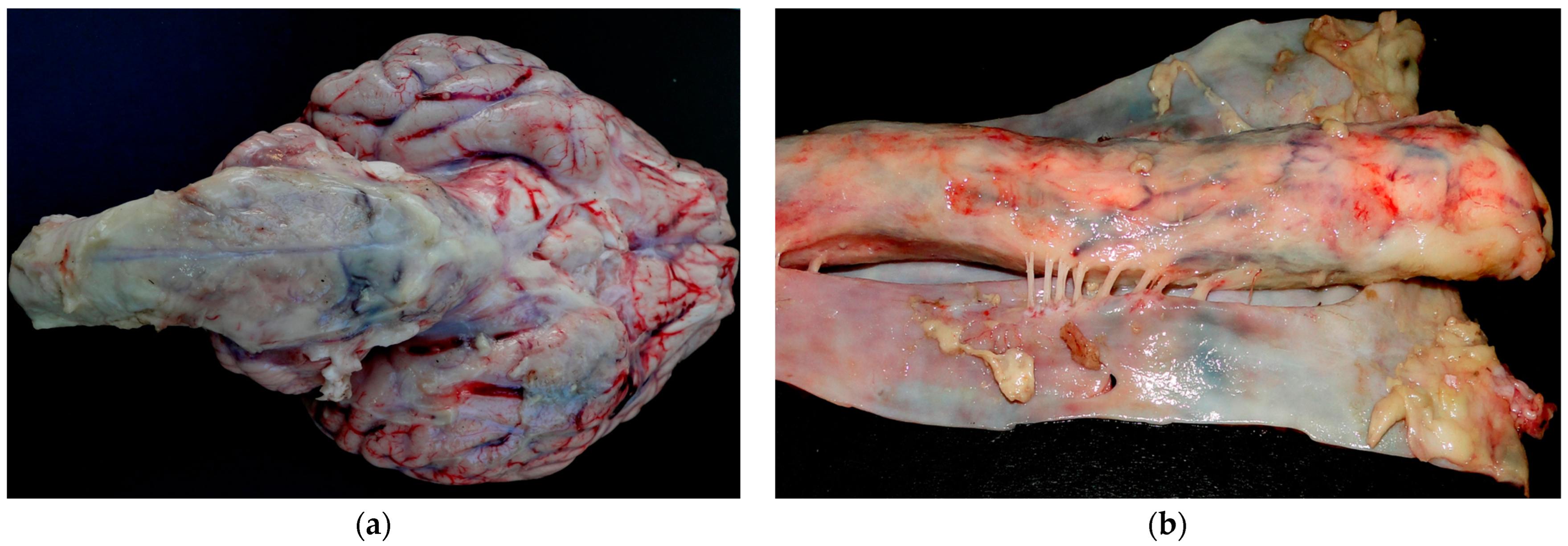
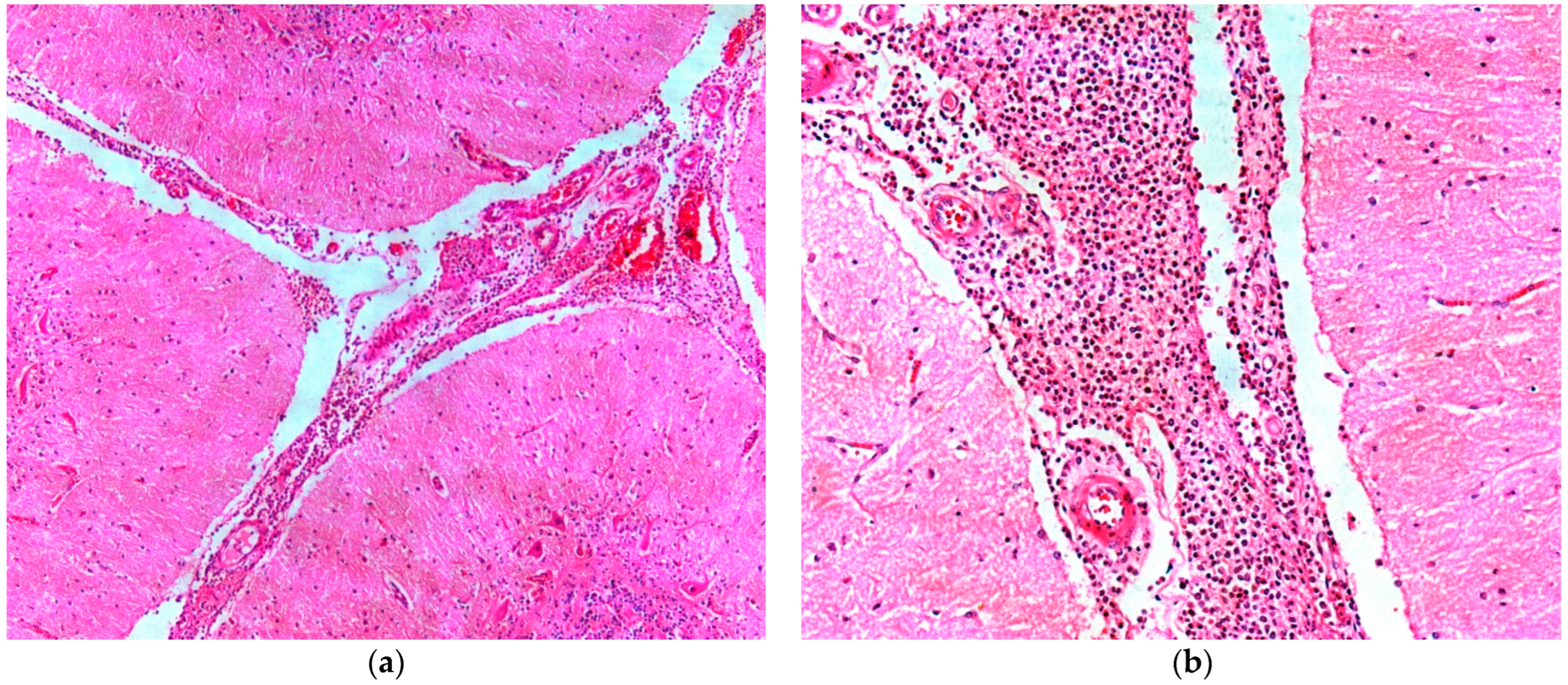
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lima, E.F.; Riet-Correa, F.; Castro, R.S.; Gomes, A.A.B.; Lima, F.S. Sinais clínicos, distribuição das lesões no sistema nervoso e epidemiologia da raiva em herbívoros na região Nordeste do Brasil. Pesq. Vet. Bras. 2005, 25, 250–264. [Google Scholar] [CrossRef][Green Version]
- Rondelli, L.A.S.; Silva, G.S.; Bezerra, K.S.; Rondelli, A.L.H.; Lima, S.R.; Furlan, F.H.; Pescador, C.A.; Colodel, E.C. Doenças de bovinos em Mato Grosso diagnosticadas no Laboratório de Patologia Veterinária da UFMT (2005–2014). Pesq. Vet. Bras. 2017, 37, 432–440. [Google Scholar] [CrossRef]
- Galiza, G.J.N.; Silva, M.L.C.R.; Dantas, A.F.M.; Simões, S.V.D.; Riet-Correa, F. Doenças do sistema nervoso de bovinos no semiárido nordestino. Pesq. Vet. Bras. 2010, 30, 267–276. [Google Scholar] [CrossRef]
- Sanches, A.W.D.; Langohr, I.M.; Stigger, A.L.; Barros, C.S.L. Doenças do sistema nervosa central em bovinos no sul do Brasil. Pesq. Vet. Bras. 2000, 20, 113–118. [Google Scholar] [CrossRef]
- Barbosa, J.D.; Brito, M.F.; Bomjardim, H.A.; Duarte, M.D.; Barbosa, C.C.; Silveira, N.S.S.; Oliveira, C.M.C.; Salvarani, F.M. Compressive lesions in the central nervous system of buffaloes. Pesq. Vet. Bras. 2022, 42, e07060. [Google Scholar] [CrossRef]
- Prado, R.G.S.; Domiciano, T.A.O.; Paredes, L.J.A.; Bezerra Junior, P.S.; Pereira, W.L.A.; Cerqueira, V.D.; Driemeier, D.; Riet-Correa, G. Nervous formo f listeriosis in buffaloes. Pesq. Vet. Bras. 2019, 39, 299–303. [Google Scholar] [CrossRef]
- Konradt, G.; Bassuino, D.M.; Prates, K.S.; Bianchi, M.V.; Snel, G.G.M.; Sonne, L.; Driemeier, D.; Pavarini, S.P. Suppurative infectious diseases of the central nervous system in domestic ruminants. Pesq. Vet. Bras. 2017, 37, 820–828. [Google Scholar] [CrossRef]
- Loretti, A.P.; Ilha, M.R.S.; Riet-Correa, G.; Driemeier, D.; Colodel, E.M.; Barros, C.S.L. Síndrome do abscesso pituitário em bezerros associada ao uso de tabuleta nasal para desmame interrompido. Pesq. Vet. Bras. 2003, 23, 39–46. [Google Scholar] [CrossRef]
- Barros, C.S.L.; Driemeier, D.; Dutra, I.S.; Lemos, R.A.A. Doenças do Sistema Nervoso de Bovinos no Brasil; Vallée: Montes Claros, Brasil, 2006. [Google Scholar]
- Lemos, R.A.A.; Brum, K.B. Meningite Bacteriana. In Doenças de Ruminantes e Equídeos, 4th ed.; Riet-Correa, F., Schild, A.L., Lemos, R.A.A., Borges, J.R.J., Mendonça, F.S., Machado, M., Eds.; Medvet: São Paulo, Brasil, 2022; Volume 1. [Google Scholar]
- Margineda, C.A.; O’Toole, D.; Prieto, M.; Uzal, F.A.; Zielinski, G.C. Histophilus somni myocarditis and leptomeningitis in feedlot cattle: Case report and occurrence in South America. J. Vet. Diagn. Investig. 2019, 31, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Bowen, R. Meningite. In Medicina Interna de Grandes Animais, 3rd ed.; Smith, B.P., Ed.; Manole: Barueri, Brasil, 2006; pp. 896–900. [Google Scholar]
- McGavin, M.D.; Zachary, J.F. Bases da Patologia em Veterinária, 4th ed.; Elsevier: Rio de Janeiro, Brasil, 2009. [Google Scholar]
- Dirksen, G.; Gründer, H.D.; Stöber, M. Rosenberger Exame Clínico dos Bovinos, 3rd ed.; Guanabara Koogan: Rio de Janeiro, Brasil, 1993. [Google Scholar]
- Schalm, O.W.; Jain, N.C. Schalm’s Veterinary Hematology, 4th ed.; Lea and Febiger: Philadelphia, PA, USA, 1986. [Google Scholar]
- Montenegro, M.I.A. Meningite bacteriana supurativa neonatal em bovinos. Master’s Dissertation, Escola Universitária Vasco da Gama, Coimbra, Portugal, 2022. [Google Scholar]
- Fecteau, G.; Smith, B.P.; George, L.W. Septicemia and meningitis in the newborn calf. Vet. Clin. N. Am. Food Anim. Pract. 2009, 25, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, L.M.A.; Câmara, A.C.L.; Oliveira, C.M.M.; Vale, A.M.; Batista, J.S.; Macedo, M.F.; Feijó, F.M.C. Meningoencefalite por Escherichia coli em cabrito. Acta Vet. Bras. 2014, 8, 91–95. [Google Scholar] [CrossRef]
- Silveira, G.L. Infecções Piogênicas do Sistema Nervoso Central de Ruminantes. Master’s Dissertation, Universidade Federal de Campina Grande, Campina Grande, Brasil, 2020. [Google Scholar]
- Brito, M.F.; Malafaia, P.; Barbosa, J.D.; Costa, N.A. Imperícia, Estresse, Negligência e Maus-Tratos: Um Atraso na Produção Animal no Brasil; Câmara Brasileira do Livro: São Paulo, Brasil, 2021; pp. 100–123. [Google Scholar]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbosa, J.D.; Bomjardim, H.d.A.; Barbosa, C.C.; Oliveira, C.M.C.; Costa, P.S.C.d.; Ferreira Filho, C.E.d.S.; Silveira, N.d.S.e.S.; Duarte, M.D.; Tondo, L.A.S.; Brito, M.d.F. Bacterial Meningitis in Buffaloes in Brazil. Animals 2024, 14, 505. https://doi.org/10.3390/ani14030505
Barbosa JD, Bomjardim HdA, Barbosa CC, Oliveira CMC, Costa PSCd, Ferreira Filho CEdS, Silveira NdSeS, Duarte MD, Tondo LAS, Brito MdF. Bacterial Meningitis in Buffaloes in Brazil. Animals. 2024; 14(3):505. https://doi.org/10.3390/ani14030505
Chicago/Turabian StyleBarbosa, José Diomedes, Henrique dos Anjos Bomjardim, Camila Cordeiro Barbosa, Carlos Magno Chaves Oliveira, Paulo Sérgio Chagas da Costa, Carlos Eduardo da Silva Ferreira Filho, Natália da Silva e Silva Silveira, Marcos Dutra Duarte, Luís Antônio Scalabrin Tondo, and Marilene de Farias Brito. 2024. "Bacterial Meningitis in Buffaloes in Brazil" Animals 14, no. 3: 505. https://doi.org/10.3390/ani14030505
APA StyleBarbosa, J. D., Bomjardim, H. d. A., Barbosa, C. C., Oliveira, C. M. C., Costa, P. S. C. d., Ferreira Filho, C. E. d. S., Silveira, N. d. S. e. S., Duarte, M. D., Tondo, L. A. S., & Brito, M. d. F. (2024). Bacterial Meningitis in Buffaloes in Brazil. Animals, 14(3), 505. https://doi.org/10.3390/ani14030505





