Abnormal Fetal Lung of Hoxa1−/− Piglets Is Rescued by Maternal Feeding with All-Trans Retinoic Acid
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals and Sample Collection
2.2. Selection of Lung Samples
2.3. Enzyme-Linked Immunosorbent Assay (ELISA)
2.4. Histological Morphology
2.5. Immunofluorescence Staining
2.6. Immunohistochemistry Staining
2.7. Image Acquisition
2.8. Quantitative Real-Time PCR
2.9. Statistical Analysis
3. Results
3.1. Concentration of Inflammatory Factors in Lung Tissue
3.2. Histological Appearances
3.3. Development of Alveolar Epithelial Cells
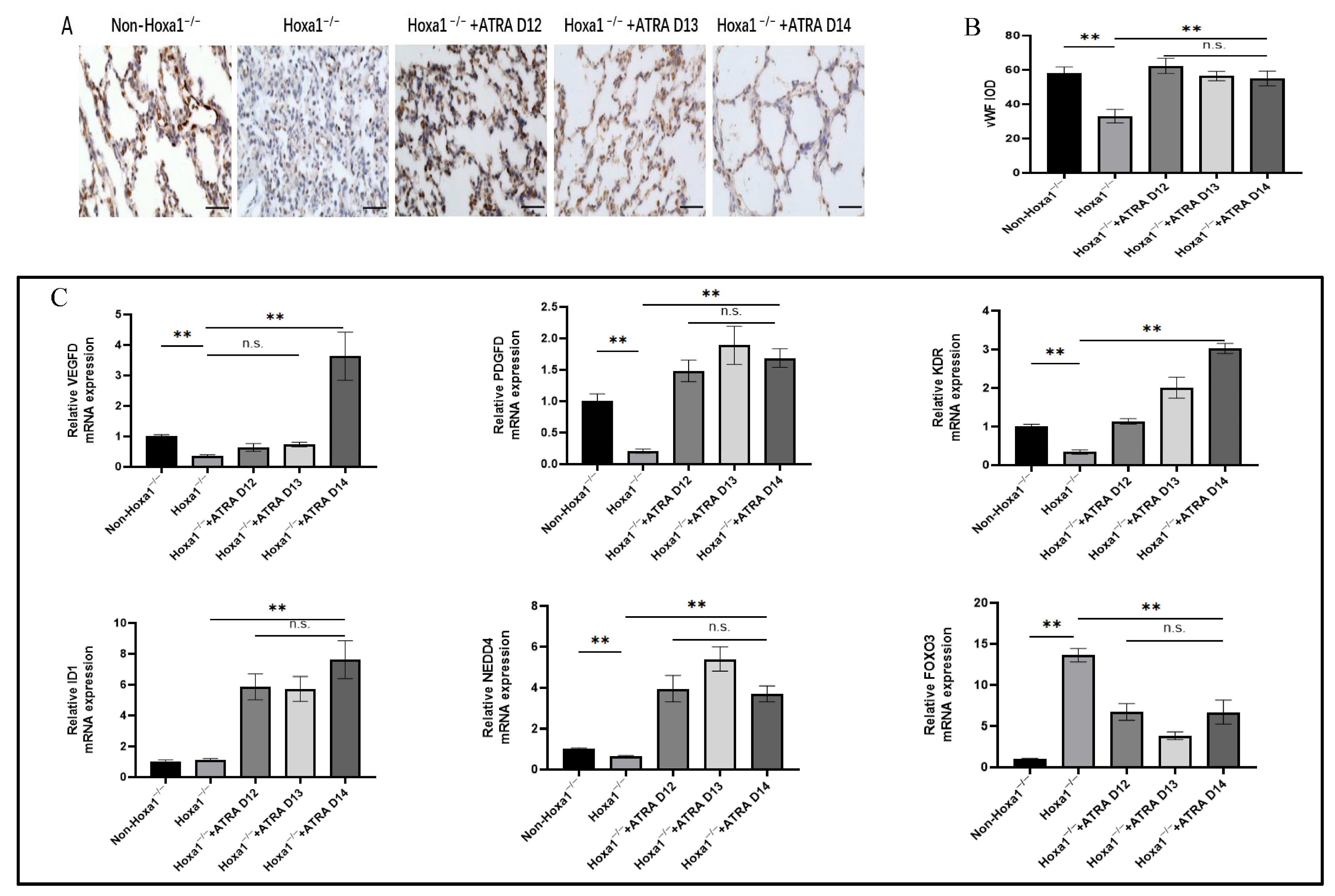
3.4. Development of Microvessels in the Lungs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tang, K.; Rossiter, H.B.; Wagner, P.D.; Breen, E.C. Lung-targeted VEGF inactivation leads to emphysema phenotype in mice. J. Appl. Physiol. 2004, 97, 1559–1566. [Google Scholar] [CrossRef] [PubMed]
- Guillot, L.; Nathan, N.; Tabary, O.; Thouvenin, G.; Le Rouzic, P.; Corvol, H.; Amselem, S.; Clement, A. Alveolar epithelial cells: Master regulators of lung homeostasis. Int. J. Biochem. Cell Biol. 2013, 45, 2568–2573. [Google Scholar] [CrossRef]
- Ma, T.H.; Fukuda, N.; Song, Y.L.; Matthay, M.A.; Verkman, A.S. Lung fluid transport in aquaporin-5 knockout mice. J. Clin. Investig. 2000, 105, 93–100. [Google Scholar] [CrossRef]
- Perl, A.K.T.; Wert, S.E.; Nagy, A.; Lobe, C.G.; Whitsett, J.A. Early restriction of peripheral and proximal cell lineages during formation of the lung. Proc. Natl. Acad. Sci. USA 2002, 99, 10482–10487. [Google Scholar] [CrossRef]
- Rock, J.R.; Hogan, B.L. Epithelial progenitor cells in lung development, maintenance, repair, and disease. Annu. Rev. Cell Dev. Biol. 2011, 27, 493–512. [Google Scholar] [CrossRef] [PubMed]
- Baybutt, R.C.; Smith, B.W.; Donskaya, E.V.; Hu, L.; Li, T.; Wang, W.Q. The proliferative effects of retinoic acid on primary cultures of adult rat type II pneumocytes depend upon cell density. Vitr. Cell Dev. Biol.—Anim. 2009, 46, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Gortner, L.; Hilgendorff, A.; Bähner, T.; Ebsen, M.; Reiss, I.; Rudloff, S. Hypoxia-induced intrauterine growth retardation: Effects on pulmonary development and surfactant protein transcription. Biol. Neonatol. 2005, 88, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Rozance, P.J.; Seedorf, G.J.; Brown, A.; Roe, G.B.; O’Meara, M.C.; Gien, J.; Tang, J.R.; Abman, S.H. Intrauterine growth restriction decreases pulmonary alveolar and vessel growth and causes pulmonary artery endothelial cell dysfunction in vitro in fetal sheep. Am. J. Physiol. Lung Cell Mol. Physiol. 2011, 301, L860–L871. [Google Scholar] [CrossRef]
- Joss-Moore, L.A.; Wang, Y.; Yu, X.; Campbell, M.S.; Callaway, C.W.; McKnight, R.A.; Wint, A.; Dahl, M.J.; Dull, R.O.; Albertine, K.H.; et al. IUGR decreases elastin mRNA expression in the developing rat lung and alters elastin content and lung compliance in the mature rat lung. Physiol. Genom. 2011, 43, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Besnard, V.; Nabeyrat, E.; Henrion-Caude, A.; Chadelat, K.; Perin, L.; Le Bouc, Y.; Clement, A. Protective role of retinoic acid from antiproliferative action of TNF-α on lung epithelial cells. Am. J. Physiol. Lung Cell Mol. Physiol. 2002, 282, L863–L871. [Google Scholar] [CrossRef]
- Sugimoto, K.; Takayasu, H.; Nakazawa, N.; Montedonico, S.; Puri, P. Prenatal treatment with retinoic acid accelerates type 1 alveolar cell proliferation of the hypoplastic lung in the nitrofen model of congenital diaphragmatic hernia. J. Pediatr. Surg. 2008, 43, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Massaro, G.D.; Massaro, D. Postnatal treatment with retinoic acid increases the number of pulmonary alveoli in rats. Am. J. Physiol. 1996, 270, L305–L310. [Google Scholar] [CrossRef]
- Gao, R.-W.; Kong, X.-Y.; Zhu, X.-X.; Zhu, G.-Q.; Ma, J.-S.; Liu, X.-X. Retinoic acid promotes primary fetal alveolar epithelial type II cell proliferation and differentiation to alveolar epithelial type I cells. Vitr. Cell Dev. Biol.—Anim. 2015, 51, 479–487. [Google Scholar] [CrossRef] [PubMed]
- James, M.L.; Ross, A.C.; Bulger, A.; Philips, J.B.; Ambalavanan, N. Vitamin A and retinoic acid act synergistically to increase lung retinyl esters during normoxia and reduce hyperoxic lung injury in newborn mice. Pediatr. Res. 2010, 67, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Londhe, V.A.; Maisonet, T.M.; Lopez, B.; Shin, B.-C.; Huynh, J.; Devaskar, S.U. Retinoic acid rescues alveolar hypoplasia in the calorie-restricted developing rat lung. Am. J. Respir. Cell Mol. Biol. 2013, 48, 179–187. [Google Scholar] [CrossRef]
- Chen, F.; Cao, Y.; Qian, J.; Shao, F.; Niederreither, K.; Cardoso, W.V. A retinoic acid–dependent network in the foregut controls formation of the mouse lung primordium. J. Clin. Investig. 2010, 120, 2040–2048. [Google Scholar] [CrossRef] [PubMed]
- Cheung, C.Y.; Anderson, D.F.; Rouzaire, M.; Blanchon, L.; Sapin, V.; Brace, R.A. Retinoic acid pathway regulation of vascular endothelial growth factor in ovine amnion. Reprod. Sci. 2019, 26, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, A.F.; Gonçalves, F.L.L.; Figueira, R.L.; Scorletti, F.; Peiró, J.L.; Sbragia, L. Combined antenatal therapy with retinoic acid and tracheal occlusion in a rat model of congenital diaphragmatic hernia. Pediatr. Surg. Int. 2016, 32, 591–598. [Google Scholar] [CrossRef]
- Gallot, D.; Coste, K.; Jani, J.; Roubliova, X.; Marceau, G.; Velemir, L.; Verheyen, A.; Lemery, D.; Sapin, V.; Deprest, J. Effects of maternal retinoic acid administration in a congenital diaphragmatic hernia rabbit model. Pediatr. Pulmonol. 2008, 43, 594–603. [Google Scholar] [CrossRef] [PubMed]
- Prat, C.; Bouvier, D.; Comptour, A.; Marceau, G.; Belville, C.; Clairefond, G.; Blanc, P.; Gallot, D.; Blanchon, L.; Sapin, V. All-trans-retinoic acid regulates aquaporin-3 expression and related cellular membrane permeability in the human amniotic environment. Placenta 2015, 36, 881–887. [Google Scholar] [CrossRef]
- Su, G.; Guo, D.; Chen, J.; Liu, M.; Zheng, J.; Wang, W.; Zhao, X.; Yin, Q.; Zhang, L.; Zhao, Z.; et al. A distal enhancer maintaining Hoxa1 expression orchestrates retinoic acid-induced early ESCs differentiation. Nucleic Acids Res. 2019, 47, 6737–6752. [Google Scholar] [CrossRef] [PubMed]
- Qiao, R.; He, Y.; Pan, B.; Xiao, S.; Zhang, X.; Li, J.; Zhang, Z.; Hong, Y.; Xing, Y.; Ren, J. Understanding the molecular mechanisms of human microtia via a pig model of HOXA1 syndrome. Dis. Model. Mech. 2015, 8, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Ceballos, E.; Chambon, P.; Gudas, L.J. Differences in gene expression between wild type and hoxa1 knockout embryonic stem cells after retinoic acid treatment or leukemia inhibitory factor (LIF) removal. J. Biol. Chem. 2005, 280, 16484–16498. [Google Scholar] [CrossRef]
- Zhou, H.; Chen, Y.; Hu, Y.; Gao, S.; Lu, W.; He, Y. Administration of all-trans retinoic acid to pregnant sows improves the developmental defects of hoxa1−/− fetal pigs. Front. Vet.-Sci. 2021, 7, 618660. [Google Scholar] [CrossRef]
- Gao, C.; Li, R.; Huan, J.; Li, W. Caveolin-1 siRNA increases the pulmonary microvascular and alveolar epithelial permeability in rats. J. Trauma 2011, 70, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Blufstein, A.; Behm, C.; Gahn, J.; Uitz, O.; Naumovska, I.; Moritz, A.; Rausch-Fan, X.; Andrukhov, O. Synergistic effects triggered by simultaneous Toll-like receptor-2 and -3 activation in human periodontal ligament stem cells. J. Periodontol. 2019, 90, 1190–1201. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Winkelmann, E.R.; Zhu, S.; Ru, W.; Mays, E.; Silvas, J.A.; Vollmer, L.L.; Gao, J.; Peng, B.-H.; Bopp, N.E.; et al. Peli1 facilitates virus replication and promotes neuroinflammation during West Nile virus infection. J. Clin. Investig. 2018, 128, 4980–4991. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-H.; Park, Y.-S.; Jung, T.T.; Yeo, S.-W.; Choi, Y.-C.; Jeon, E. Effect of Tumor necrosis factor-alpha on experimental otitis media with effusion. Laryngoscope 2001, 111, 728–733. [Google Scholar] [CrossRef]
- Seder, R.A.; Darrah, P.A.; Roederer, M. T-cell quality in memory and protection: Implications for vaccine design. Nat. Rev. Immunol. 2008, 8, 247–258. [Google Scholar] [CrossRef]
- Friedland, Y.D.; Lee-Pullen, T.F.; Nathan, E.A.; Watts, R.; Keelan, J.A.; Payne, M.S.; Ireland, D.J. T cell cytokine responses to stimulation with Ureaplasma parvum in pregnancy. J. Reprod. Immunol. 2016, 116, 93–97. [Google Scholar] [CrossRef]
- Chau, J.; Moza, D.; Hossain, N.; Lee, J.K.; Bienenstock, J.; Karimi, K. Increased production of IFN-γ by natural killer cells triggered with bone marrow-derived dendritic cells cultured in the presence of retinoic acid. Eur. J. Pharmacol. 2013, 715, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Baggiolini, M.; Walz, A.; Kunkel, S.L. Neutrophil-activating peptide-1/interleukin 8, a novel cytokine that activates neutrophils. J. Clin. Investig. 1989, 84, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Mukaida, N.; Harada, A.; Yasumoto, K.; Matsushima, K. Properties of pro-inflammatory cell type-specific leukocyte chemotactic cytokines, interleukin 8 (IL-8) and monocyte chemotactic and activating factor (MCAF). Microbiol. Immunol. 1992, 36, 773–789. [Google Scholar] [CrossRef]
- Zielnik-Jurkiewicz, B.; Stankiewicz-Szymczak, W. Pro-inflammatory interleukins in middle ear effusions from atopic and non-atopic children with chronic otitis media with effusion. Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 1369–1378. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.J.; George, C.L.; Snyder, J.M.; Acarregui, M.J. Retinoic acid and erythropoietin maintain alveolar development in mice treated with an angiogenesis inhibitor. Am. J. Respir. Cell Mol. Biol. 2005, 33, 622–628. [Google Scholar] [CrossRef]
- Ng-Blichfeldt, J.-P.; Alçada, J.; Montero, M.A.; Dean, C.H.; Griesenbach, U.; Griffiths, M.J.; Hind, M. Deficient retinoid-driven angiogenesis may contribute to failure of adult human lung regeneration in emphysema. Thorax 2017, 72, 510–521. [Google Scholar] [CrossRef]
- Li, N.; Xu, Y.; Zhang, H.; Gao, L.; Li, J.; Wang, Y.; Gao, Z.; Pan, X.; Liu, X.; Li, X.; et al. Excessive retinoic acid impaired proliferation and differentiation of human fetal palatal chondrocytes (hFPCs). Birth Defects Res. B Dev. Reprod. Toxicol. 2014, 101, 276–282. [Google Scholar] [CrossRef]
- Li, Y.; Wongsiriroj, N.; Blaner, W.S. The multifaceted nature of retinoid transport and metabolism. Hepatobiliary Surg. Nutr. 2014, 3, 126–139. [Google Scholar] [CrossRef]
- Ruttenstock, E.; Doi, T.; Dingemann, J.; Puri, P. Prenatal administration of retinoic acid upregulates insulin-like growth factor receptors in the nitrofen-induced hypoplastic lung. Birth Defects Res. B Dev. Reprod. Toxicol. 2011, 92, 148–151. [Google Scholar] [CrossRef]
- Shu, W.; Guttentag, S.; Wang, Z.; Andl, T.; Ballard, P.; Lu, M.M.; Piccolo, S.; Birchmeier, W.; Whitsett, J.A.; Millar, S.E.; et al. Wnt/β-catenin signaling acts upstream of N-myc, BMP4, and FGF signaling to regulate proximal–distal patterning in the lung. Dev. Biol. 2005, 283, 226–239. [Google Scholar] [CrossRef]
- Nomura, J.; Horie, I.; Seto, M.; Nagai, K.; Hisatsune, A.; Miyata, T.; Isohama, Y. All-trans retinoic acid increases expression of aquaporin-5 and plasma membrane water permeability via transactivation of Sp1 in mouse lung epithelial cells. Biochem. Biophys. Res. Commun. 2006, 351, 1048–1053. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Hooper, S.B.; Armugam, A.; Dawson, N.; Ferraro, T.; Jeyaseelan, K.; Thiel, A.; Koukoulas, I.; Wintour, E.M. Aquaporin gene expression and regulation in the ovine fetal lung. J. Physiol. 2003, 551, 503–514. [Google Scholar] [CrossRef]
- Torday, J.S.; Rehan, V.K. Testing for fetal lung maturation: A biochemical “window” to the developing fetus. Clin. Lab. Med. 2003, 23, 361–383. [Google Scholar] [CrossRef] [PubMed]
- Boase, N.A.; Rychkov, G.Y.; Townley, S.L.; Dinudom, A.; Candi, E.; Voss, A.K.; Tsoutsman, T.; Semsarian, C.; Melino, G.; Koentgen, F.; et al. Respiratory distress and perinatal lethality in Nedd4-2-deficient mice. Nat. Commun. 2011, 2, 287. [Google Scholar] [CrossRef] [PubMed]
- George, U.M.; Ashna, U.; Kumar, S.S.P.; Nandkumar, A.M. Effect of tobacco extract on surfactant synthesis and its reversal by retinoic acid—Role of cell–cell interactions in vitro. Vitr. Cell Dev. Biol.—Anim. 2013, 49, 260–269. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.Y.; Ciechanowicz, A.K.; Kaplan, A.R.; Wang, L.; Zhang, P.-X.; Lu, Y.-C.; Tobin, R.E.; Tobin, B.A.; Cohn, L.; Zeiss, C.J.; et al. Surfactant protein C dampens inflammation by decreasing JAK/STAT activation during lung repair. Am. J. Lung Physiol. Cell Mol. Physiol. 2018, 314, L882–L892. [Google Scholar] [CrossRef] [PubMed]
- Sehlmeyer, K.; Ruwisch, J.; Roldan, N.; Lopez-Rodriguez, E. Alveolar dynamics and beyond—The importance of surfactant protein C and cholesterol in lung homeostasis and fibrosis. Front. Physiol. 2020, 11, 386. [Google Scholar] [CrossRef]
- Ito, Y.; Mason, R.J. The effect of interleukin-13 (IL-13) and interferon-γ (IFN-γ) on expression of surfactant proteins in adult human alveolar type II cells in vitro. Respir. Res. 2010, 11, 157. [Google Scholar] [CrossRef]
- Nabeyrat, E.; Besnard, V.; Corroyer, S.; Cazals, V.; Clement, A. Retinoic acid-induced proliferation of lung alveolar epithelial cells: Relation with the IGF system. Am. J. Physiol. Lung Cell Mol. Physiol. 1998, 275, 71–79. [Google Scholar] [CrossRef]
- Nabeyrat, E.; Corroyer, S.; Epaud, R.; Besnard, V.; Cazals, S.; Clement, A. Retinoic acid-induced proliferation of lung alveolar epithelial cells is linked to p21CIP 1downregulation. Am. J. Physiol. Lung Cell Mol. Physiol. 2000, 278, L42–L50. [Google Scholar] [CrossRef]
- Yun, E.J.; Lorizio, W.; Seedorf, G.; Abman, S.H.; Vu, T.H. VEGF and endothelium-derived retinoic acid regulate lung vascular and alveolar development. Am. J. Physiol. Lung Cell Mol. Physiol. 2016, 310, L287–L298. [Google Scholar] [CrossRef] [PubMed]
- Lassus, P.; Turanlati, M.; Heikkilä, P.; Andersson, L.C.; Nupponen, I.; Sarnesto, A.; Andersson, S. Pulmonary vascular endothelial growth factor and flt-1 in fetuses, in acute and chronic lung disease, and persistent pulmonary hypertension of the newborn. Am. J. Respir. Crit. Care Med. 2001, 164, 1981–1987. [Google Scholar] [CrossRef] [PubMed]
- Borkham-Kamphorst, E.; Meurer, S.K.; Van de Leur, E.; Haas, U.; Tihaa, L.; Weiskirchen, R. PDGF-D signaling in portal myofibroblasts and hepatic stellate cells proves identical to PDGF-B via both PDGF receptor type α and β. Cell Signal. 2015, 27, 1305–1314. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Yuan, W.; Wu, L.; Tang, Q.; Xia, Q.; Ji, J.; Liu, Z.; Ma, Z.; Zhou, Z.; Cheng, Y.; et al. PDGF-D promotes cell growth, aggressiveness, angiogenesis and EMT transformation of colorectal cancer by activation of Notch1/Twist1 pathway. Oncotarget 2017, 8, 9961–9973. [Google Scholar] [CrossRef] [PubMed]
- Pontén, A.; Folestad, E.B.; Pietras, K.; Eriksson, U. Platelet-derived growth factor D Induces cardiac fibrosis and proliferation of vascular smooth muscle cells in heart-specific transgenic mice. Circ. Res. 2005, 97, 1036–1045. [Google Scholar] [CrossRef] [PubMed]
- Kurasawa, K.; Arai, S.; Owada, T.; Maezawa, R.; Kumano, K.; Fukuda, T. Autoantibodies against platelet-derived growth factor receptor alpha in patients with systemic lupus erythematosus. Mod. Rheumatol. 2010, 20, 458–465. [Google Scholar] [CrossRef]
- Ma, J.; Zhao, Y.; Sun, L.; Sun, X.; Zhao, X.; Sun, X.; Qian, H.; Xu, W.; Zhu, W. Exosomes derived from Akt-modified human umbilical cord mesenchymal stem cells improve cardiac regeneration and promote angiogenesis via activating platelet-derived growth factor D. Stem Cells Transl. Med. 2017, 6, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Fredriksson, L.; Li, X.; Eriksson, U. PDGF-D is a potent transforming and angiogenic growth factor. Oncogene 2003, 22, 1501–1510. [Google Scholar] [CrossRef]
- Uutela, M.; Wirzenius, M.; Paavonen, K.; Rajantie, I.; He, Y.; Karpanen, T.; Lohela, M.; Wiig, H.; Salven, P.; Pajusola, K.; et al. PDGF-D induces macrophage recruitment, increased interstitial pressure, and blood vessel maturation during angiogenesis. Blood 2004, 104, 3198–3204. [Google Scholar] [CrossRef]
- Wang, Z.; Kong, D.; Banerjee, S.; Li, Y.; Adsay, N.V.; Abbruzzese, J.; Sarkar, F.H. Down-regulation of platelet-derived growth factor-D inhibits cell growth and angiogenesis through inactivation of notch-1 and nuclear factor-κB signaling. Cancer Res. 2007, 67, 11377–11385. [Google Scholar] [CrossRef]
- Gladh, H.; Folestad, E.B.; Muhl, L.; Ehnman, M.; Tannenberg, P.; Lawrence, A.-L.; Betsholtz, C.; Eriksson, U. Mice lacking platelet-derived growth factor D display a mild vascular phenotype. PLoS ONE 2016, 11, e0152276. [Google Scholar] [CrossRef]
- Pereda, J.; Sulz, L.; Martin, S.S.; Godoy-Guzmán, C. The human lung during the embryonic period: Vasculogenesis and primitive erythroblasts circulation. J. Anat. 2013, 222, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Clerch, L.B.; Baras, A.S.; Massaro, G.D.C.; Hoffman, E.P.; Massaro, D. DNA microarray analysis of neonatal mouse lung connects regulation of KDR with dexamethasone-induced inhibition of alveolar formation. Am. J. Physiol. Lung Cell Mol. Physiol. 2004, 286, L411–L419. [Google Scholar] [CrossRef] [PubMed]
- Shao, Y.; Jiang, Z.; He, D.; Shen, J. NEDD4 attenuates phosgene-induced acute lung injury through the inhibition of Notch1 activation. J. Cell Mol. Med. 2022, 26, 2831–2840. [Google Scholar] [CrossRef] [PubMed]
- Yanpallewar, S.; Wang, T.; Koh, D.C.I.; Quarta, E.; Fulgenzi, G.; Tessarollo, L. Nedd4-2 haploinsufficiency causes hyperactivity and increased sensitivity to inflammatory stimuli. Sci. Rep. 2016, 6, 32957. [Google Scholar] [CrossRef] [PubMed]
- Bouzeyen, R.; Haoues, M.; Barbouche, M.-R.; Singh, R.; Essafi, M. FOXO3 transcription factor regulates IL-10 expression in mycobacteria-infected macrophages, tuning their polarization and the subsequent adaptive immune response. Front. Immunol. 2019, 10, 2922. [Google Scholar] [CrossRef] [PubMed]
- Potente, M.; Urbich, C.; Sasaki, K.I.; Hofmann, W.K.; Heeschen, C.; Aicher, A.; Kollipara, R.; Depinho, R.A.; Zeiher, A.M.; Dimmeler, S. Involvement of Foxo transcription factors in angiogenesis and postnatal neovascularization. J. Clin. Investig. 2005, 115, 2382–2392. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Du, W.W.; Li, X.; Yee, A.J.; Yang, B.B. Foxo3 activity promoted by non-coding effects of circular RNA and Foxo3 pseudogene in the inhibition of tumor growth and angiogenesis. Oncogene 2016, 35, 3919–3931. [Google Scholar] [CrossRef]



| All-Trans Retinoic Acid Offered to Sows at Different DPC | Levels of All-Trans Retinoic Acid (mg/kg Body Weight) | Number of Sows in Different Groups | |
|---|---|---|---|
| Control group | 0 | 0 | 6 |
| Experimental group 1 | 12 | 4 | 2 |
| Experimental group 2 | 12 | 5 | 2 |
| Experimental group 3 | 12 | 6 | 2 |
| Experimental group 4 | 13 | 4 | 2 |
| Experimental group 5 | 13 | 5 | 2 |
| Experimental group 6 | 13 | 6 | 2 |
| Experimental group 7 | 14 | 4 | 2 |
| Experimental group 8 | 14 | 5 | 2 |
| Experimental group 9 | 14 | 6 | 2 |
| Genes | Accession Numbers | Primer Sequences (5′~3′) | Product Size (bp) |
|---|---|---|---|
| VEGFD | XM_001928382.5 | F AGATCCCAGAAGAAGATGGATGT | 198 |
| R ACAGACACACTCGCAACGAT | |||
| PDGFD | XM_021062718.1 | F TCAGTAACGGACCCCACTCT | 198 |
| R GCCGGTCCAGGTCAACTTT | |||
| KDR | XM_013997943.2 | F CTGCCTACCTCACCTGTTTC | 100 |
| R ACTGACTTAGAGAGTACCTGAT | |||
| ID1 | NM_001244700.1 | F GATCGCATCTTGTGTCGCTG | 101 |
| R GGTGCTTGGAAGGACCAGAG | |||
| NEDD4 | XM_021094899.1 | F TCTTGGGAGCTAGACTTTGAATCC | 146 |
| R AAAGAGGAACATCCACTTGACCT | |||
| FOXO3 | XM_021084231.1 | F CAGCAGCACAGTGTTTGGAC | 120 |
| R AGTGTCTGGTTGCCGTAGTG |
| IFN-γ (pg/mL) | TNF-α (pg/mL) | IL-8 (pg/mL) | |
|---|---|---|---|
| Non-Hoxa1−/− | 63.98 ± 7.54 a | 19.63 ± 1.24 c | 75.16 ± 1.13 bc |
| Hoxa1−/− | 33.24 ± 3.44 b | 18.73 ± 0.68 c | 39.18 ± 0.13 c |
| Hoxa1−/− + ATRA D12 | 38.36 ± 2.18 b | 22.85 ± 2.12 ab | 90.31 ± 0.13 b |
| Hoxa1−/− + ATRA D13 | 46.95 ± 3.74 b | 27.48 ± 1.14 a | 251.65 ± 22.40 a |
| Hoxa1−/− + ATRA D14 | 62.43 ± 4.52 a | 20.57 ± 1.50 bc | 73.49 ± 5.38 bc |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.; Zhou, H.; Wu, H.; Lu, W.; He, Y. Abnormal Fetal Lung of Hoxa1−/− Piglets Is Rescued by Maternal Feeding with All-Trans Retinoic Acid. Animals 2023, 13, 2850. https://doi.org/10.3390/ani13182850
Chen Y, Zhou H, Wu H, Lu W, He Y. Abnormal Fetal Lung of Hoxa1−/− Piglets Is Rescued by Maternal Feeding with All-Trans Retinoic Acid. Animals. 2023; 13(18):2850. https://doi.org/10.3390/ani13182850
Chicago/Turabian StyleChen, Yixin, Haimei Zhou, Huadong Wu, Wei Lu, and Yuyong He. 2023. "Abnormal Fetal Lung of Hoxa1−/− Piglets Is Rescued by Maternal Feeding with All-Trans Retinoic Acid" Animals 13, no. 18: 2850. https://doi.org/10.3390/ani13182850
APA StyleChen, Y., Zhou, H., Wu, H., Lu, W., & He, Y. (2023). Abnormal Fetal Lung of Hoxa1−/− Piglets Is Rescued by Maternal Feeding with All-Trans Retinoic Acid. Animals, 13(18), 2850. https://doi.org/10.3390/ani13182850





