Antimicrobial Resistance Profiles, Virulence Determinants, and Biofilm Formation in Enterococci Isolated from Rhesus Macaques (Macaca mulatta): A Potential Threat for Wildlife in Bangladesh?
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
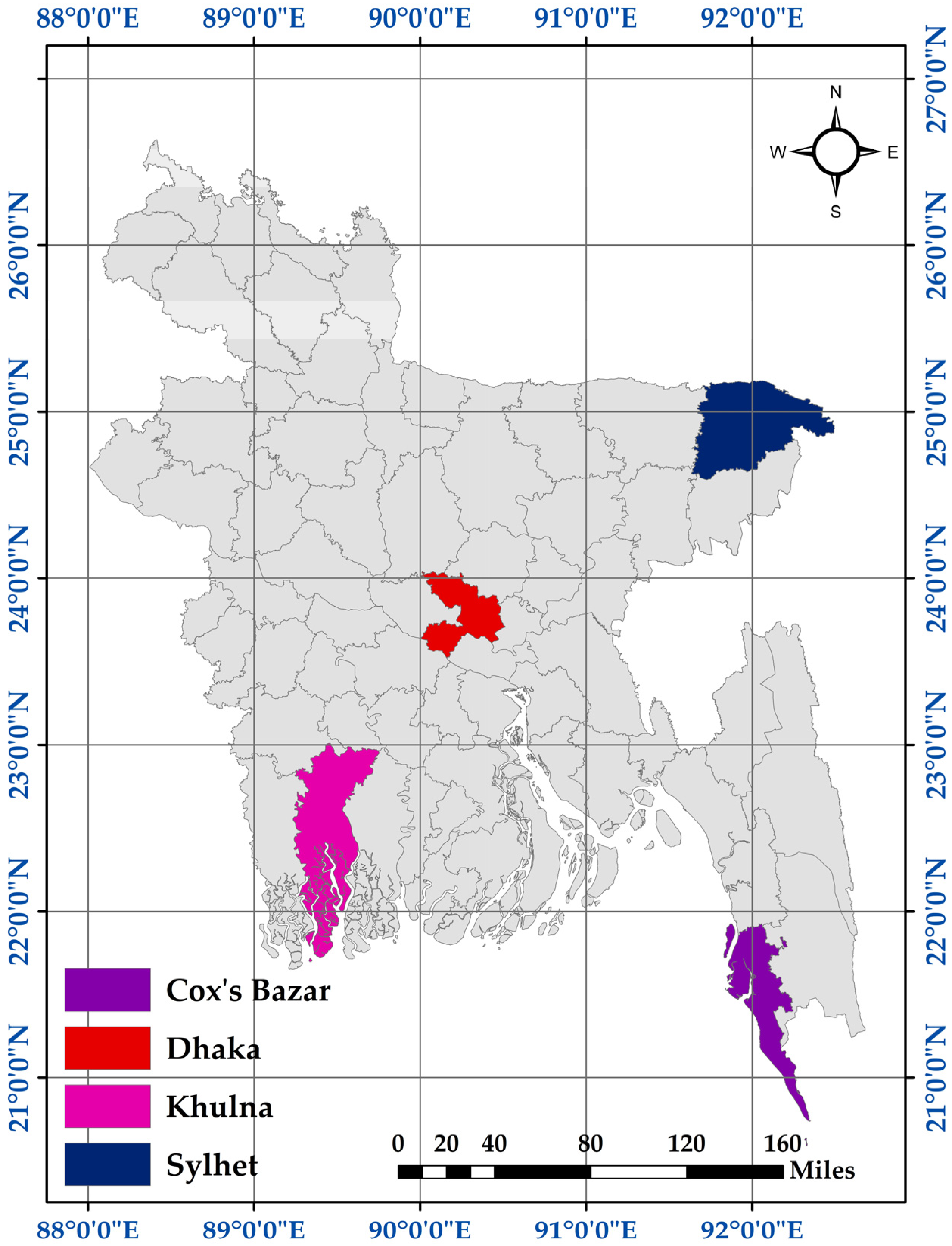
2.1. Sample Information
2.2. Isolation of Enterococci
2.3. Molecular Detection of Enterococci
2.4. Biofilm Formation Capability of Enterococci
2.5. Detection of Virulence Genes in Enterococci
2.6. Antimicrobial Susceptibility Test
2.7. Statistical Analysis
3. Results
3.1. Occurrence of Enterococci
3.2. Characteristics of Enterococcus faecalis
3.2.1. Biofilm-Forming Ability of E. faecalis
3.2.2. Occurrence of Virulence Genes in E. faecalis
3.2.3. Antibiogram Profiles of E. faecalis
3.3. Characteristics of Enterococcus faecium
3.3.1. Biofilm-Forming Ability of E. Faecium
3.3.2. Occurrence of Virulence Genes in E. faecium
3.3.3. Antibiogram Profiles of E. faecium
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rahman, M.T.; Sobur, M.A.; Islam, M.S.; Ievy, S.; Hossain, M.J.; El Zowalaty, M.E.; Rahman, A.T.; Ashour, H.M. Zoonotic diseases: Etiology, impact, and control. Microorganisms 2020, 8, 1405. [Google Scholar] [CrossRef] [PubMed]
- Galán-Acedo, C.; Arroyo-Rodríguez, V.; Andresen, E.; Arasa-Gisbert, R. Ecological traits of the world’s primates. Sci. Data 2019, 6, 55. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Rahman, M.K.; Uddin, M.H.; Rahman, M.M.; Chowdhury, M.N.; Hassan, M.M.; Magalhaes, R.S.; Islam, A. Prevalence and diversity of gastrointestinal parasites in free-ranging rhesus macaques (Macaca mulatta) in different land gradients of Bangladesh. Am. J. Primatol. 2022, 84, e23345. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.K.; Hassan, M.M.; Islam, S.; Rostal, M.K.; Uddin, M.H.; Hagan, E.; Samad, M.A.; Flora, M.S.; Epstein, J.H.; Islam, A. Characterization and epidemiology of antimicrobial resistance patterns of Salmonella spp. and Staphylococcus spp. in free-ranging rhesus macaque (Macaca mulatta) at high-risk interfaces with people and livestock in Bangladesh. Front. Vet. Sci. 2023, 10, 1103922. [Google Scholar] [CrossRef] [PubMed]
- Grassotti, T.T.; de Angelis Zvoboda, D.; da Fontoura Xavier Costa, L.; De Araujo, A.J.G.; Pereira, R.I.; Soares, R.O.; Wagner, P.G.C.; Frazzon, J.; Frazzon, A.P.G. Antimicrobial Resistance Profiles in Enterococcus spp. Isolates From Fecal Samples of Wild and Captive Black Capuchin Monkeys (Sapajus nigritus) in South Brazil. Front. Microbiol. 2018, 9, 2366. [Google Scholar] [CrossRef]
- van den Berg, S.; van Wamel, W.J.; Snijders, S.V.; Ouwerling, B.; de Vogel, C.P.; Boelens, H.A.; Willems, R.J.; Huijsdens, X.W.; Verreck, F.A.; Kondova, I.; et al. Rhesus macaques (Macaca mulatta) are natural hosts of specific Staphylococcus aureus lineages. PLoS ONE 2011, 6, e26170. [Google Scholar] [CrossRef]
- Nizeyi, J.B.; Innocent, R.B.; Erume, J.; Kalema, G.R.; Cranfield, M.R.; Graczyk, T.K. Campylobacteriosis, salmonellosis, and shigellosis in free-ranging human-habituated mountain gorillas of Uganda. J. Wildl. Dis. 2001, 37, 239–244. [Google Scholar] [CrossRef]
- Ramos, S.; Silva, V.; Dapkevicius, M.D.L.E.; Igrejas, G.; Poeta, P. Enterococci, from harmless bacteria to a pathogen. Microorganisms 2020, 8, 1118. [Google Scholar] [CrossRef]
- Udo, E.E.; Al-Sweih, N.; Phillips, O.A.; Chugh, T.D. Species prevalence and antibacterial resistance of enterococci isolated in Kuwait hospitals. J. Med. Microbiol. 2003, 52, 163–168. [Google Scholar] [CrossRef]
- Woźniak-Biel, A.; Bugla-Płoskońska, G.; Burdzy, J.; Korzekwa, K.; Ploch, S.; Wieliczko, A. Antimicrobial resistance and biofilm formation in Enterococcus spp. isolated from humans and turkeys in Poland. Microb. Drug Resist. 2019, 25, 277–286. [Google Scholar] [CrossRef]
- Jett, B.D.; Huycke, M.M.; Gilmore, M.S. Virulence of enterococci. Clin. Microbiol. Rev. 1994, 7, 462–478. [Google Scholar] [CrossRef]
- Ballah, F.M.; Islam, M.S.; Rana, M.L.; Ferdous, F.B.; Ahmed, R.; Pramanik, P.K.; Karmoker, J.; Ievy, S.; Sobur, M.A.; Siddique, M.P.; et al. Phenotypic and Genotypic Detection of Biofilm-Forming Staphylococcus aureus from Different Food Sources in Bangladesh. Biology 2022, 11, 949. [Google Scholar] [CrossRef]
- Lewis, C.M.; Zervos, M.J. Clinical manifestations of enterococcal infection. Eur. J. Clin. Microbiol. Infect. Dis. 1990, 9, 111–117. [Google Scholar] [CrossRef]
- Hashem, Y.A.; Amin, H.M.; Essam, T.M.; Yassin, A.S.; Aziz, R.K. Biofilm formation in enterococci: Genotype-phenotype correlations and inhibition by vancomycin. Sci. Rep. 2017, 7, 5733. [Google Scholar] [CrossRef]
- Hashem, Y.A.; Abdelrahman, K.A.; Aziz, R.K. Phenotype–genotype correlations and distribution of key virulence factors in Enterococcus faecalis isolated from patients with urinary tract infections. Infect. Drug Resist. 2021, 14, 1713–1723. [Google Scholar] [CrossRef]
- Gajewska, J.; Chajęcka-Wierzchowska, W.; Byczkowska-Rostkowska, Z.; Saki, M. Biofilm Formation Capacity and Presence of Virulence Determinants among Enterococcus Species from Milk and Raw Milk Cheeses. Life 2023, 13, 495. [Google Scholar] [CrossRef]
- Stępień-Pyśniak, D.; Hauschild, T.; Kosikowska, U.; Dec, M.; Urban-Chmiel, R. Biofilm formation capacity and presence of virulence factors among commensal Enterococcus spp. from wild birds. Sci. Rep. 2019, 9, 11204. [Google Scholar] [CrossRef]
- Islam, M.S.; Rahman, M.T. A Comprehensive Review on Bacterial Vaccines Combating Antimicrobial Resistance in Poultry. Vaccines 2023, 11, 616. [Google Scholar] [CrossRef]
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Davies, J.; Davies, D. Origins and evolution of antibiotic resistance. Microbiol. Mol. Biol. Rev. 2010, 74, 417–433. [Google Scholar] [CrossRef]
- Martínez, J.L. Antibiotics and antibiotic resistance genes in natural environments. Science 2008, 321, 365–367. [Google Scholar] [CrossRef] [PubMed]
- Robinson, T.P.; Bu, D.P.; Carrique-Mas, J.; Fèvre, E.M.; Gilbert, M.; Grace, D.; Hay, S.I.; Jiwakanon, J.; Kakkar, M.; Kariuki, S.; et al. Antibiotic resistance is the quintessential One Health issue. Trans. R. Soc. Trop. Med. Hyg. 2016, 110, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Rahman, A.T.; Hassan, J.; Rahman, M.T. Extended-spectrum beta-lactamase in Escherichia coli isolated from humans, animals, and environments in Bangladesh: A One Health perspective systematic review and meta-analysis. One Health 2023, 16, 100526. [Google Scholar] [CrossRef] [PubMed]
- Hasan, B.; Järhult, J.D. Absence of vancomycin-resistant enterococci among highly ESBL-positive crows (Corvus splendens) foraging on hospital waste in Bangladesh. Infect. Ecol. Epidemiol. 2015, 5, 29761. [Google Scholar] [CrossRef] [PubMed]
- Hollenbeck, B.L.; Rice, L.B. Intrinsic and acquired resistance mechanisms in Enterococcus. Virulence 2012, 3, 421–569. [Google Scholar] [CrossRef]
- Banik, A.; Mohammad, N.; Akter, T.; Fatema, K.; Abony, M. Prevalence, identification and antibiotic susceptibility of Enterococcus Species isolated from chicken and pigeon meat in Gazipur area of Bangladesh. Open J. Med. Microbiol. 2018, 8, 74–83. [Google Scholar] [CrossRef]
- Roy, K.; Islam, M.S.; Paul, A.; Ievy, S.; Talukder, M.; Sobur, M.A.; Ballah, F.M.; Khan, M.S.R.; Rahman, M.T. Molecular detection and antibiotyping of multi-drug resistant Enterococcus faecium from healthy broiler chickens in Bangladesh. Vet. Med. Sci. 2022, 8, 200–210. [Google Scholar] [CrossRef]
- Sagor, M.S.; Hossain, M.S.; Islam, T.; Mahmud, M.A.; Miah, M.S.; Karim, M.R.; Giasuddin, M.; Samad, M.A. Phenotypic and genotypic antibiotic resistance and virulence profiling of Enterococcus faecalis isolated from poultry at two major districts in Bangladesh. Pak. Vet. J. 2022, 42, 153–160. [Google Scholar]
- Bag, M.A.S.; Arif, M.; Riaz, S.; Khan, M.S.R.; Islam, M.S.; Punom, S.A.; Ali, M.W.; Begum, F.; Islam, M.S.; Rahman, M.T.; et al. Antimicrobial resistance, virulence profiles, and public health significance of Enterococcus faecalis isolated from clinical mastitis of cattle in Bangladesh. BioMed Res. Int. 2022, 2022, 8101866. [Google Scholar] [CrossRef]
- Roy, S.; Aung, M.S.; Paul, S.K.; Ahmed, S.; Haque, N.; Khan, E.R.; Barman, T.K.; Islam, A.; Abedin, S.; Sultana, C.; et al. Drug resistance determinants in clinical isolates of Enterococcus faecalis in Bangladesh: Identification of oxazolidinone resistance gene optrA in ST59 and ST902 lineages. Microorganisms 2020, 8, 1240. [Google Scholar] [CrossRef]
- Samad, M.A.; Sagor, M.S.; Hossain, M.S.; Karim, M.R.; Mahmud, M.A.; Sarker, M.S.; Shownaw, F.A.; Mia, Z.; Card, R.M.; Agunos, A.; et al. High prevalence of vancomycin non-susceptible and multi-drug resistant enterococci in farmed animals and fresh retail meats in Bangladesh. Vet. Res. Commun. 2022, 46, 811–822. [Google Scholar] [CrossRef]
- Akter, T.; Foysal, M.J.; Alam, M.; Ehsan, R.; Paul, S.I.; Momtaz, F.; Siddik, M.A.; Tay, A.C.Y.; Fotedar, R.; Gupta, S.K.; et al. Involvement of Enterococcus species in streptococcosis of Nile tilapia in Bangladesh. Aquaculture 2021, 531, 735790. [Google Scholar] [CrossRef]
- Akter, T.; Haque, M.N.; Ehsan, R.; Paul, S.I.; Foysal, M.J.; Tay, A.C.Y.; Islam, M.T.; Rahman, M.M. Virulence and antibiotic-resistance genes in Enterococcus faecalis associated with streptococcosis disease in fish. Sci. Rep. 2023, 13, 1551. [Google Scholar] [CrossRef]
- Islam, M.S.; Paul, A.; Talukder, M.; Roy, K.; Sobur, M.A.; Ievy, S.; Nayeem, M.M.H.; Rahman, S.; Nazir, K.N.H.; Hossain, M.T.; et al. Migratory birds travelling to Bangladesh are potential carriers of multi-drug resistant Enterococcus spp., Salmonella spp., and Vibrio spp. Saudi J. Biol. Sci. 2021, 28, 5963–5970. [Google Scholar] [CrossRef]
- Facklam, R.R.; da Carvalho, M.G.S.; Teixeira, L.M. History, Taxonomy, Biochemical Characteristics, and Antibiotic Susceptibility Testing of Enterococci. In The Enterococci; American Society of Microbiology: Washington, DC, USA, 2002; pp. 1–54. [Google Scholar]
- Dutka-Malen, S.; Evers, S.; Courvalin, P. Detection of glycopeptide resistance genotypes identification to the species level of clinically relevant enterococci by PCR. J. Clin. Microbiol. 1995, 33, 24–27. [Google Scholar] [CrossRef]
- Randall, L.P.; Cooles, S.W.; Osborn, M.K.; Piddock, L.J.V.; Woodward, M.J. Antibiotic resistance genes integrons multiple antibiotic resistance in thirty-five serotypes of Salmonella enterica isolated from humans animals in the UK. J. Antimicrob. Chemother. 2004, 53, 208–216. [Google Scholar] [CrossRef]
- Islam, M.S.; Nayeem, M.M.H.; Sobur, M.A.; Ievy, S.; Islam, M.A.; Rahman, S.; Kafi, M.A.; Ashour, H.M.; Rahman, M.T. Virulence determinants and multidrug resistance of Escherichia coli isolated from migratory birds. Antibiotics 2021, 10, 190. [Google Scholar] [CrossRef]
- Arciola, C.R.; Baldassarri, L.; Montanaro, L. Presence of icaA and icaD genes and slime production in a collection of staphylococcal strains from catheter-associated infections. J. Clin. Microbiol. 2001, 39, 2151–2156. [Google Scholar] [CrossRef]
- Freeman, D.J.; Falkiner, F.R.; Keane, C.T. New method for detecting slime production by coagulase negative staphylococci. J. Clin. Pathol. 1989, 42, 872–874. [Google Scholar] [CrossRef]
- Dhanalakshmi, T.A.; Venkatesha, D.; Nusrath, A.; Asharani, N. Evaluation of Phenotypic Methods for Detection of Biofilm Formation in Uropathogens. Natl. J. Lab. Med. 2018, 7, MO06–MO11. [Google Scholar]
- M100-S32; Performance Standards for Antimicrobial Susceptibility Testing. Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2022.
- Bauer, A.T.; Kirby, W.M.M.; Sherris, J.C.; Turck, M. Antibiotic susceptibility testing by a standardized single disc method. Am. J. Clin. Pathol. 1966, 45, 149–158. [Google Scholar] [CrossRef]
- Sweeney, M.T.; Lubbers, B.V.; Schwarz, S.; Watts, J.L. Applying definitions for multidrug resistance, extensive drug resistance and pandrug resistance to clinically significant livestock and companion animal bacterial pathogens. J. Antimicrob. Chemother. 2018, 73, 1460–1463. [Google Scholar] [CrossRef] [PubMed]
- Krumperman, P.H. Multiple antibiotic resistance indexing of Escherichia coli to identify high-risk sources of fecal contamination of foods. Appl. Environ. Microbiol. 1983, 46, 165–170. [Google Scholar] [CrossRef]
- Brown, L.D.; Cai, T.T.; DasGupta, A. Interval estimation for a binomial proportion. Stat. Sci. 2001, 16, 101–133. [Google Scholar] [CrossRef]
- Mo, S.S.; Urdahl, A.M.; Madslien, K.; Sunde, M.; Nesse, L.L.; Slettemeås, J.S.; Norström, M. What does the fox say? Monitoring antimicrobial resistance in the environment using wild red foxes as an indicator. PLoS ONE 2018, 13, e0198019. [Google Scholar] [CrossRef] [PubMed]
- Price, K.D. Bacterial infections in cynomolgus monkeys given small molecule immunomodulatory antagonists. J. Immunotoxicol. 2010, 7, 128–137. [Google Scholar] [CrossRef]
- Jin, L.; Hinde, K.; Tao, L. Species diversity and relative abundance of lactic acid bacteria in the milk of rhesus monkeys (Macaca mulatta). J. Med. Primatol. 2011, 40, 52–58. [Google Scholar] [CrossRef]
- Grassotti, T.T.; Zvoboda, D.D.A.; Costa, L.D.F.X.; Christiano, F.D.P.; Mann, M.B.; Wagner, P.G.C.; Campos, A.A.S.; Frazzon, J.; Frazzon, A.P.G. Intra and inter-monkey transmission of bacteria in wild black capuchins monkeys (Sapajus nigritus): A preliminary study. Braz. J. Biol. 2021, 82, e237460. [Google Scholar] [CrossRef]
- Grassotti, T.T.; Kothe, C.I.; Prichula, J.; Mohellibi, N.; Mann, M.B.; Wagner, P.G.C.; Campos, F.S.; Campos, A.A.S.; Frazzon, J.; Frazzon, A.P.G. Fecal bacterial communities of wild black capuchin monkeys (Sapajus nigritus) from the Atlantic Forest biome in Southern Brazil are divergent from those of other non-human primates. Curr. Res. Microb. Sci. 2021, 2, 100048. [Google Scholar] [CrossRef]
- Dworniczek, E.; Piwowarczyk, J.; Seniuk, A.; Gościniak, G. Enterococcus–virulence and susceptibility to photodynamic therapy of clinical isolates from Lower Silesia, Poland. Scand. J. Infect. Dis. 2014, 46, 846–853. [Google Scholar] [CrossRef]
- Vu, B.; Chen, M.; Crawford, R.J.; Ivanova, E.P. Bacterial extracellular polysaccharides involved in biofilm formation. Molecules 2009, 14, 2535–2554. [Google Scholar] [CrossRef]
- Hentzer, M.; Riedel, K.; Rasmussen, T.B.; Heydorn, A.; Andersen, J.B.; Parsek, M.R.; Rice, S.A.; Eberl, L.; Molin, S.; Høiby, N.; et al. Inhibition of quorum sensing in Pseudomonas aeruginosa biofilm bacteria by a halogenated furanone compound. Microbiology 2002, 148, 87–102. [Google Scholar] [CrossRef]
- Liu, X.; Yao, H.; Zhao, X.; Ge, C. Biofilm Formation and Control of Foodborne Pathogenic Bacteria. Molecules 2023, 28, 2432. [Google Scholar] [CrossRef]
- Tibúrcio, A.A.C.M.; Paiva, A.D.; Pedrosa, A.L.; Rodrigues, W.F.; da Silva, R.B.; Oliveira, A.G. Effect of sub-inhibitory concentrations of antibiotics on biofilm formation and expression of virulence genes in penicillin-resistant, ampicillin-susceptible Enterococcus faecalis. Heliyon 2022, 8, e11154. [Google Scholar] [CrossRef]
- Fisher, K.; Phillips, C. The ecology, epidemiology and virulence of Enterococcus. Microbiology 2009, 155, 1749–1757. [Google Scholar] [CrossRef]
- Soares, R.O.; Fedi, A.C.; Reiter, K.C.; Caierão, J.; d’Azevedo, P.A. Correlation between biofilm formation and gelE, esp, and agg genes in Enterococcus spp. clinical isolates. Virulence 2014, 5, 634–637. [Google Scholar] [CrossRef]
- Anderson, A.C.; Jonas, D.; Huber, I.; Karygianni, L.; Wölber, J.; Hellwig, E.; Arweiler, N.; Vach, K.; Wittmer, A.; Al-Ahmad, A. Enterococcus faecalis from food, clinical specimens, and oral sites: Prevalence of virulence factors in association with biofilm formation. Front. Microbiol. 2016, 6, 1534. [Google Scholar] [CrossRef]
- Paganelli, F.L.; Willems, R.J.; Leavis, H.L. Optimizing future treatment of enterococcal infections: Attacking the biofilm? Trends Microbiol. 2012, 20, 40–49. [Google Scholar] [CrossRef]
- Sayah, R.S.; Kaneene, J.B.; Johnson, Y.; Miller, R. Patterns of antimicrobial resistance observed in Escherichia coli isolates obtained from domestic-and wild-animal fecal samples, human septage, and surface water. Appl. Environ. Microbiol. 2005, 71, 1394–1404. [Google Scholar] [CrossRef]
- Boneca, I.G.; Chiosis, G. Vancomycin resistance: Occurrence, mechanisms and strategies to combat it. Expert Opin. Ther. Targets 2003, 7, 311–328. [Google Scholar] [CrossRef]
- Fioriti, S.; Coccitto, S.N.; Cedraro, N.; Simoni, S.; Morroni, G.; Brenciani, A.; Mangiaterra, G.; Vignaroli, C.; Vezzulli, L.; Biavasco, F.; et al. Linezolid resistance genes in enterococci isolated from sediment and zooplankton in two Italian coastal areas. Appl. Environ. Microbiol. 2021, 87, e02958-20. [Google Scholar] [CrossRef] [PubMed]
- Arnold, K.E.; Williams, N.J.; Bennett, M. ‘Disperse abroad in the land’: The role of wildlife in the dissemination of antimicrobial resistance. Biol. Lett. 2016, 12, 20160137. [Google Scholar] [CrossRef] [PubMed]
- Oliveira de Araujo, G.; Huff, R.; Favarini, M.O.; Mann, M.B.; Peters, F.B.; Frazzon, J.; Guedes Frazzon, A.P. Multidrug resistance in enterococci isolated from wild pampas foxes (Lycalopex gymnocercus) and Geoffroy’s Cats (Leopardus geoffroyi) in the Brazilian Pampa Biome. Front. Vet. Sci. 2020, 7, 606377. [Google Scholar] [CrossRef] [PubMed]
- Høiby, N.; Bjarnsholt, T.; Givskov, M.; Molin, S.; Ciofu, O. Antibiotic resistance of bacterial biofilms. Int. J. Antimicrob. Agents 2010, 35, 322–332. [Google Scholar] [CrossRef]
- Uruén, C.; Chopo-Escuin, G.; Tommassen, J.; Mainar-Jaime, R.C.; Arenas, J. Biofilms as promoters of bacterial antibiotic resistance and tolerance. Antibiotics 2020, 10, 3. [Google Scholar] [CrossRef]
- Davies, D. Understanding biofilm resistance to antibacterial agents. Nat. Rev. Drug Discov. 2003, 2, 114–122. [Google Scholar] [CrossRef]
- Ballah, F.M.; Islam, M.S.; Rana, M.L.; Ullah, M.A.; Ferdous, F.B.; Neloy, F.H.; Ievy, S.; Sobur, M.A.; Rahman, A.T.; Khatun, M.M.; et al. Virulence Determinants and Methicillin Resistance in Biofilm-Forming Staphylococcus aureus from Various Food Sources in Bangladesh. Antibiotics 2022, 11, 1666. [Google Scholar] [CrossRef]
- Nowakiewicz, A.; Zięba, P.; Gnat, S.; Trościańczyk, A.; Osińska, M.; Łagowski, D.; Kosior-Korzecka, U.; Puzio, I. A significant number of multi-drug resistant Enterococcus faecalis in wildlife animals; long-term consequences and new or known reservoirs of resistance? Sci. Total Environ. 2020, 705, 135830. [Google Scholar] [CrossRef]
| Factors | Target Genes | Primer Sequences (5′–3′) | Annealing Tm (°C) | Size (bp) | Reference |
|---|---|---|---|---|---|
| Enterococcus faecalis | ddlE. faecalis | F: ATCAAGTACAGTTAGTCTTTA R: AACGATTCAAAGCTAACT | 48 | 942 | [36] |
| Enterococcus faecium | ddlE. faecium | F: GCAAGGCTTCTTAGAGA R: CATCGTGTAAGCTAACTTC | 50 | 550 | [36] |
| Virulence | agg | F: TCTTGGACACGACCCATGAT R: AGAAAGAACATCACCACGAGC | 58 | 413 | [14] |
| fsrA | F: CGTTCCGTCTCTCATAGTTA R: GCAGGATTTGAGGTTGCTAA | 53 | 474 | [14] | |
| fsrB | F: TAATCTAGGCTTAGTTCCCAC R: CTAAATGGCTCTGTCGTCTAG | 55 | 428 | [14] | |
| fsrC | F: GTGTTTTTGATTTCGCCAGAGA R: TATAACAATCCCCAACCGTG | 54 | 716 | [14] | |
| gelE | F: GGTGAAGAAGTTACTCTGAC R: GGTATTGAGTTATGAGGGGC | 52 | 704 | [14] | |
| sprE | F: CTGAGGACAGAAGACAAGAAG R: GGTTTTTCTCACCTGGATAG | 53 | 432 | [14] | |
| ace | F: GAATGACCGAGAACGATGGC R: CTTGATGTTGGCCTGCTTCC | 58 | 615 | [14] | |
| pil | F: GAAGAAACCAAAGCACCTAC R: CTACCTAAGAAAAGAAACGCG | 53 | 620 | [14] | |
| cyl | F: TGGCGGTATTTTTACTGGAG R: TGAATCGCTCCATTTCTTC | 52 | 186 | [15] | |
| Antibiotic resistance | blaTEM | F: CATTTCCGTGTCGCCCTTAT R: TCCATAGTTGCCTGACTCCC | 56 | 793 | [37] |
| Sample ID | Biofilm Properties | Virulence Gene Pattern | Antibiogram Profiles | |
|---|---|---|---|---|
| Phenotype | Genotype | |||
| RM-1 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD | blaTEM |
| RM-2 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, TE, C | |
| RM-3 | Weak | agg, fsrB, fsrC, sprE, gelE | P, AMP, RD | |
| RM-4 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, VA, TE | |
| RM-5 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-8 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-10 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, VA | |
| RM-11 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-13 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-15 | Weak | pil, fsrB, fsrC, sprE, gelE | P, AMP, RD | blaTEM |
| RM-16 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-17 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA, C | blaTEM |
| RM-18 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-19 | Weak | agg, pil, fsrB, fsrC, sprE, gelE | P, AMP, RD | blaTEM |
| RM-20 | Weak | pil, fsrB, fsrC, sprE, gelE | P, AMP, RD | |
| RM-21 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, TE | blaTEM |
| RM-22 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD | blaTEM |
| RM-25 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE | P, AMP, RD, LZD, VA | |
| RM-27 | Intermediate | agg, pil, fsrA, fsrC, ace, sprE, gelE | P, AMP, RD, E, VA | blaTEM |
| RM-28 | Weak | agg, fsrB, fsrC, sprE, gelE | P, AMP, RD, E | blaTEM |
| RM-29 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, VA | |
| RM-31 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-32 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, LZD, VA | |
| RM-34 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-36 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE | P, AMP, RD, E, LZD | |
| RM-37 | Weak | agg, pil, fsrB, fsrC, sprE, gelE | P, AMP, RD, VA | blaTEM |
| RM-39 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-40 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD | |
| RM-41 | Weak | agg, pil, fsrB, fsrC, sprE, gelE | P, AMP, RD, E, TE | blaTEM |
| RM-42 | Weak | agg, pil, fsrB, fsrC, sprE, gelE | P, AMP, RD, LZD | |
| RM-43 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA, TE | blaTEM |
| RM-44 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE | P, AMP, RD, E, LZD | |
| RM-45 | Intermediate | agg, pil, fsrA, fsrB, ace, sprE, gelE | P, AMP, RD, VA, TE | |
| RM-46 | Intermediate | agg, pil, fsrA, fsrC, ace, sprE, gelE | P, AMP, RD, LZD, VA | blaTEM |
| RM-48 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, TE | blaTEM |
| RM-50 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, LZD | |
| RM-51 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, TE | blaTEM |
| RM-55 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, VA | |
| RM-56 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA, TE, C | blaTEM |
| RM-57 | Intermediate | agg, pil, fsrA, fsrC, ace, sprE, gelE | P, AMP, RD, LZD | |
| RM-61 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD | blaTEM |
| RM-62 | Weak | agg, pil, fsrB, fsrC, gelE | P, AMP, RD, E | blaTEM |
| RM-63 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, LZD | |
| RM-66 | Intermediate | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, LZD, VA | blaTEM |
| No. of Pattern | Antibiotic Resistance Patterns | No. of Antibiotics (Classes) | No. of Isolates | Overall MDR Isolates (%) | MAR Index |
|---|---|---|---|---|---|
| Enterococcus faecalis | |||||
| 1 | P, AMP, RD, E, LZD, VA, TE, C | 8 (7) | 1 | 39/44 (88.6) | 0.6 |
| 2 | P, AMP, RD, E, LZD, TE, C | 7 (6) | 1 | 0.5 | |
| 3 | P, AMP, RD, E, LZD, VA, C | 7 (6) | 1 | 0.5 | |
| 4 | P, AMP, RD, E, LZD, VA, TE | 7 (6) | 1 | 0.5 | |
| 5 | P, AMP, RD, E, VA, TE | 6 (5) | 1 | 0.5 | |
| 6 | P, AMP, RD, E, LZD, VA | 6 (5) | 9 | 0.5 | |
| 7 | P, AMP, RD, E, LZD | 5 (4) | 5 | 0.4 | |
| 8 | P, AMP, RD, LZD, VA | 5 (4) | 4 | 0.4 | |
| 9 | P, AMP, RD, E, VA | 5 (4) | 2 | 0.4 | |
| 10 | P, AMP, RD, VA, TE | 5 (4) | 1 | 0.4 | |
| 11 | P, AMP, RD, E, TE | 5 (4) | 3 | 0.4 | |
| 12 | P, AMP, RD, LZD | 4 (3) | 4 | 0.3 | |
| 13 | P, AMP, RD, TE | 4 (3) | 1 | 0.3 | |
| 14 | P, AMP, RD, E | 4 (3) | 2 | 0.3 | |
| 15 | P, AMP, RD, VA | 4 (3) | 3 | 0.3 | |
| 16 * | P, AMP, RD | 3 (2) | 5 * | 0.2 | |
| Enterococcus faecium | |||||
| 1 | P, AMP, RD, E, LZD, VA | 6 (5) | 7 | 15/15 (100) | 0.5 |
| 2 | P, AMP, RD, E, LZD | 5 (4) | 2 | 0.4 | |
| 3 | P, AMP, RD, E | 4 (3) | 6 | 0.3 | |
| Sample ID | Biofilm Properties | Virulence Gene Pattern | Antibiogram Profile | |
|---|---|---|---|---|
| Phenotype | Genotype | |||
| RM-4 | Intermediate | pil | P, AMP, RD, E | |
| RM-10 | Weak | - | P, AMP, RD, E | |
| RM-16 | Strong | fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-17 | Intermediate | fsrB | P, AMP, RD, E | blaTEM |
| RM-23 | Intermediate | pil, sprE | P, AMP, RD, E, LZD, VA | |
| RM-27 | Intermediate | pil, sprE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-29 | Intermediate | gelE | P, AMP, RD, E, LZD | blaTEM |
| RM-36 | Intermediate | fsrC | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-37 | Intermediate | fsrA | P, AMP, RD, E | |
| RM-39 | Strong | agg, pil, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-42 | Weak | - | P, AMP, RD, E | |
| RM-43 | Intermediate | fsrA, fsrB, fsrC, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-52 | Intermediate | fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD | blaTEM |
| RM-59 | Strong | agg, fsrA, fsrB, fsrC, ace, sprE, gelE | P, AMP, RD, E, LZD, VA | blaTEM |
| RM-67 | weak | - | P, AMP, RD, E | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferdous, F.B.; Islam, M.S.; Ullah, M.A.; Rana, M.L.; Punom, S.A.; Neloy, F.H.; Chowdhury, M.N.U.; Hassan, J.; Siddique, M.P.; Saha, S.; et al. Antimicrobial Resistance Profiles, Virulence Determinants, and Biofilm Formation in Enterococci Isolated from Rhesus Macaques (Macaca mulatta): A Potential Threat for Wildlife in Bangladesh? Animals 2023, 13, 2268. https://doi.org/10.3390/ani13142268
Ferdous FB, Islam MS, Ullah MA, Rana ML, Punom SA, Neloy FH, Chowdhury MNU, Hassan J, Siddique MP, Saha S, et al. Antimicrobial Resistance Profiles, Virulence Determinants, and Biofilm Formation in Enterococci Isolated from Rhesus Macaques (Macaca mulatta): A Potential Threat for Wildlife in Bangladesh? Animals. 2023; 13(14):2268. https://doi.org/10.3390/ani13142268
Chicago/Turabian StyleFerdous, Farhana Binte, Md. Saiful Islam, Md. Ashek Ullah, Md. Liton Rana, Sadia Afrin Punom, Fahim Haque Neloy, Mohammad Nizam Uddin Chowdhury, Jayedul Hassan, Mahbubul Pratik Siddique, Sukumar Saha, and et al. 2023. "Antimicrobial Resistance Profiles, Virulence Determinants, and Biofilm Formation in Enterococci Isolated from Rhesus Macaques (Macaca mulatta): A Potential Threat for Wildlife in Bangladesh?" Animals 13, no. 14: 2268. https://doi.org/10.3390/ani13142268
APA StyleFerdous, F. B., Islam, M. S., Ullah, M. A., Rana, M. L., Punom, S. A., Neloy, F. H., Chowdhury, M. N. U., Hassan, J., Siddique, M. P., Saha, S., & Rahman, M. T. (2023). Antimicrobial Resistance Profiles, Virulence Determinants, and Biofilm Formation in Enterococci Isolated from Rhesus Macaques (Macaca mulatta): A Potential Threat for Wildlife in Bangladesh? Animals, 13(14), 2268. https://doi.org/10.3390/ani13142268









