Proximal Abduction Ulnar Osteotomy (PAUL): Short- and Long-Term Evaluation in Dogs Presenting Medial Compartment Disease
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Selection
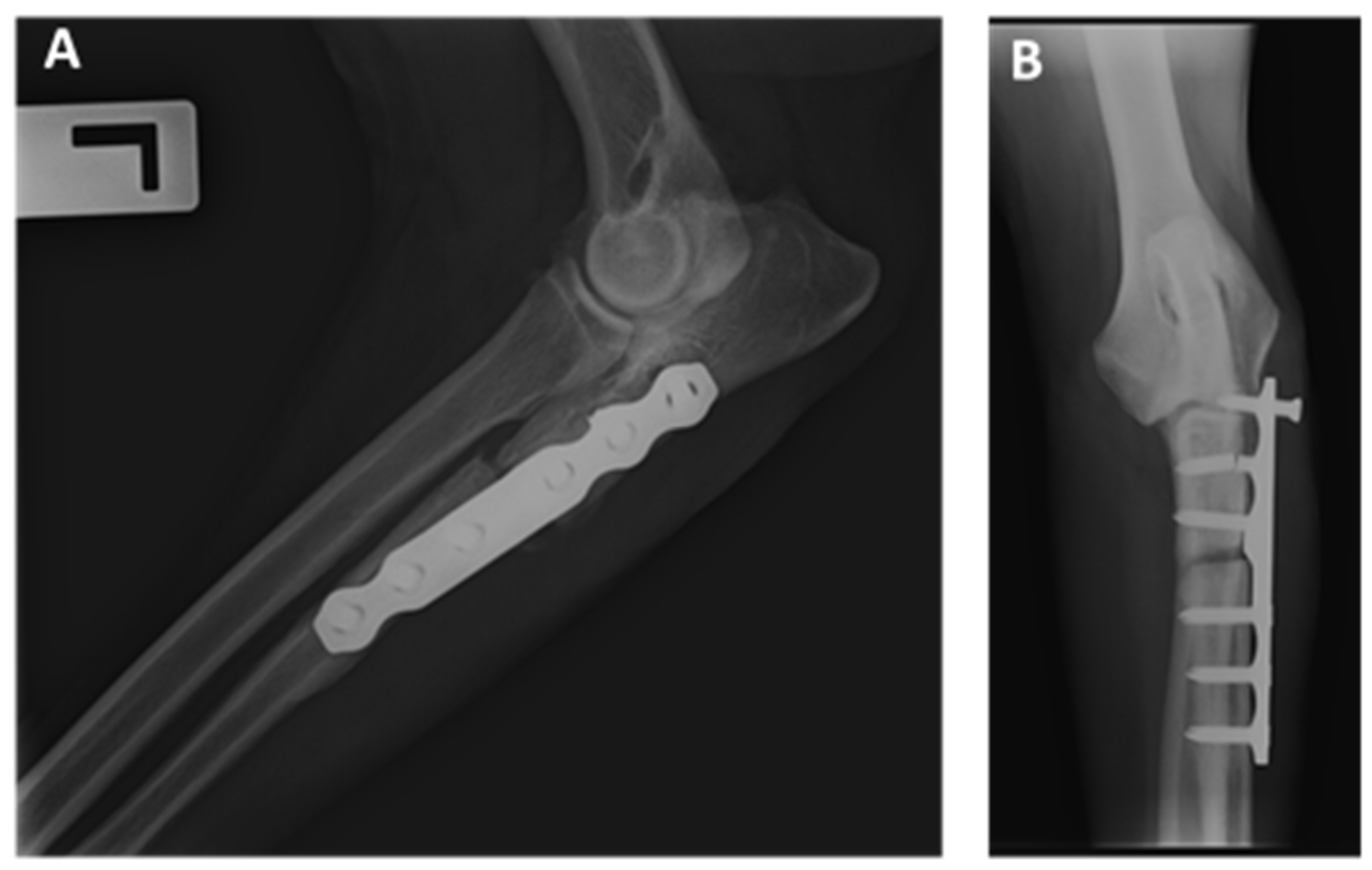
2.2. Surgical Procedure
2.3. Short-Term Clinical Evaluation
2.4. Mid- to Long-Term Clinical Evaluation
2.5. Short-, Mid- and Long-Term Questionnaire
2.6. Statistical Analysis
3. Results
3.1. Case Selection
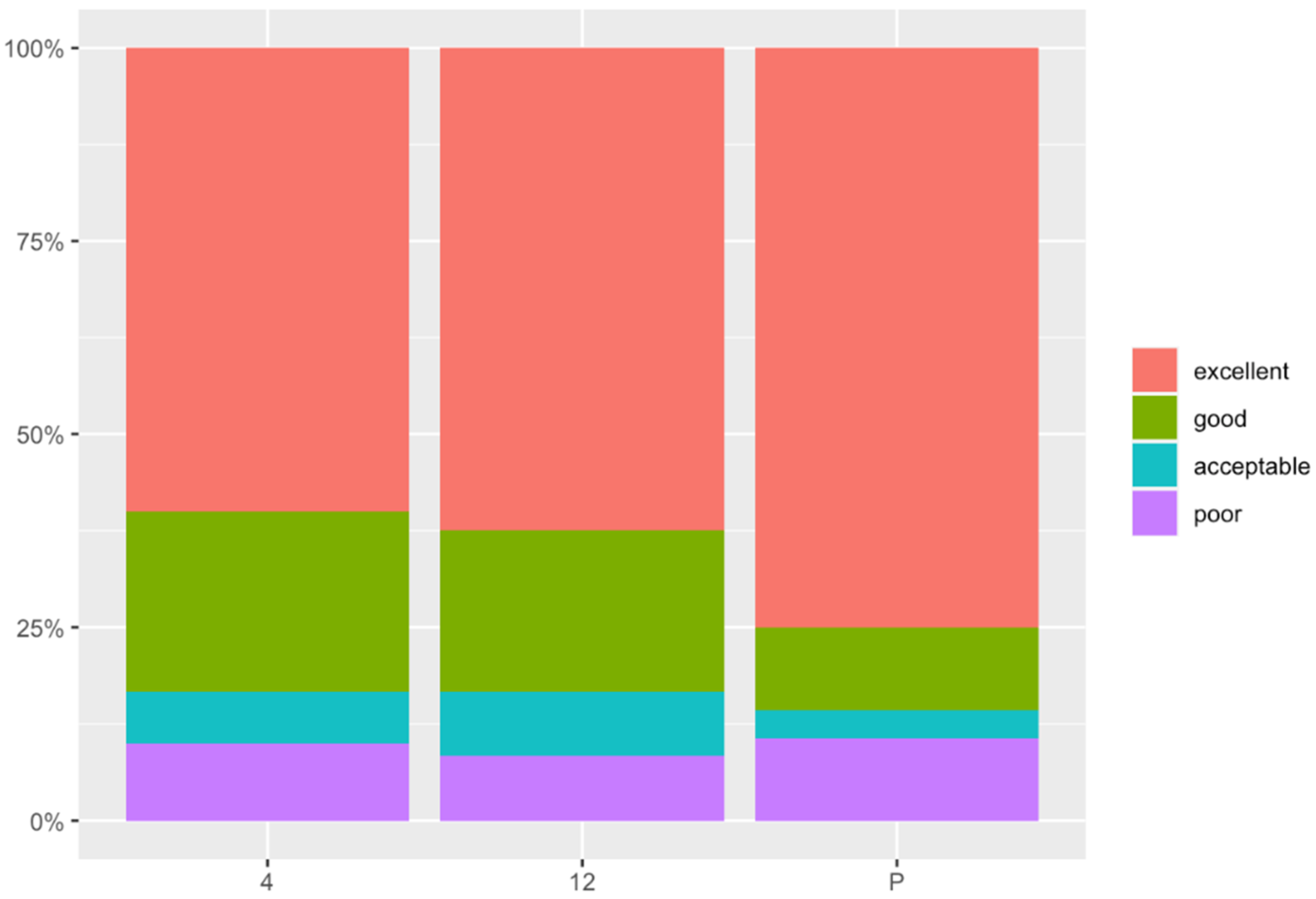
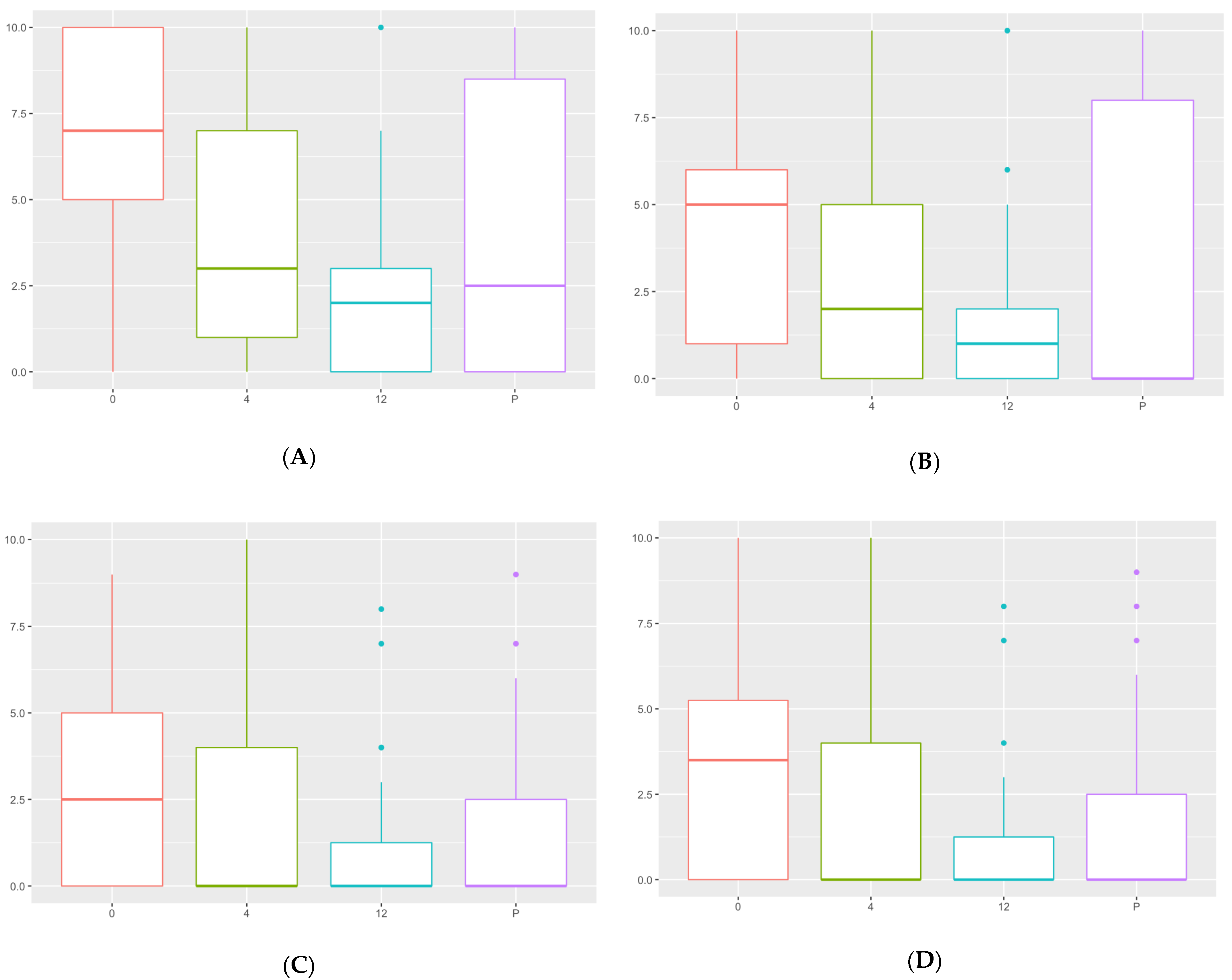
3.2. Postoperative Owner Assessment
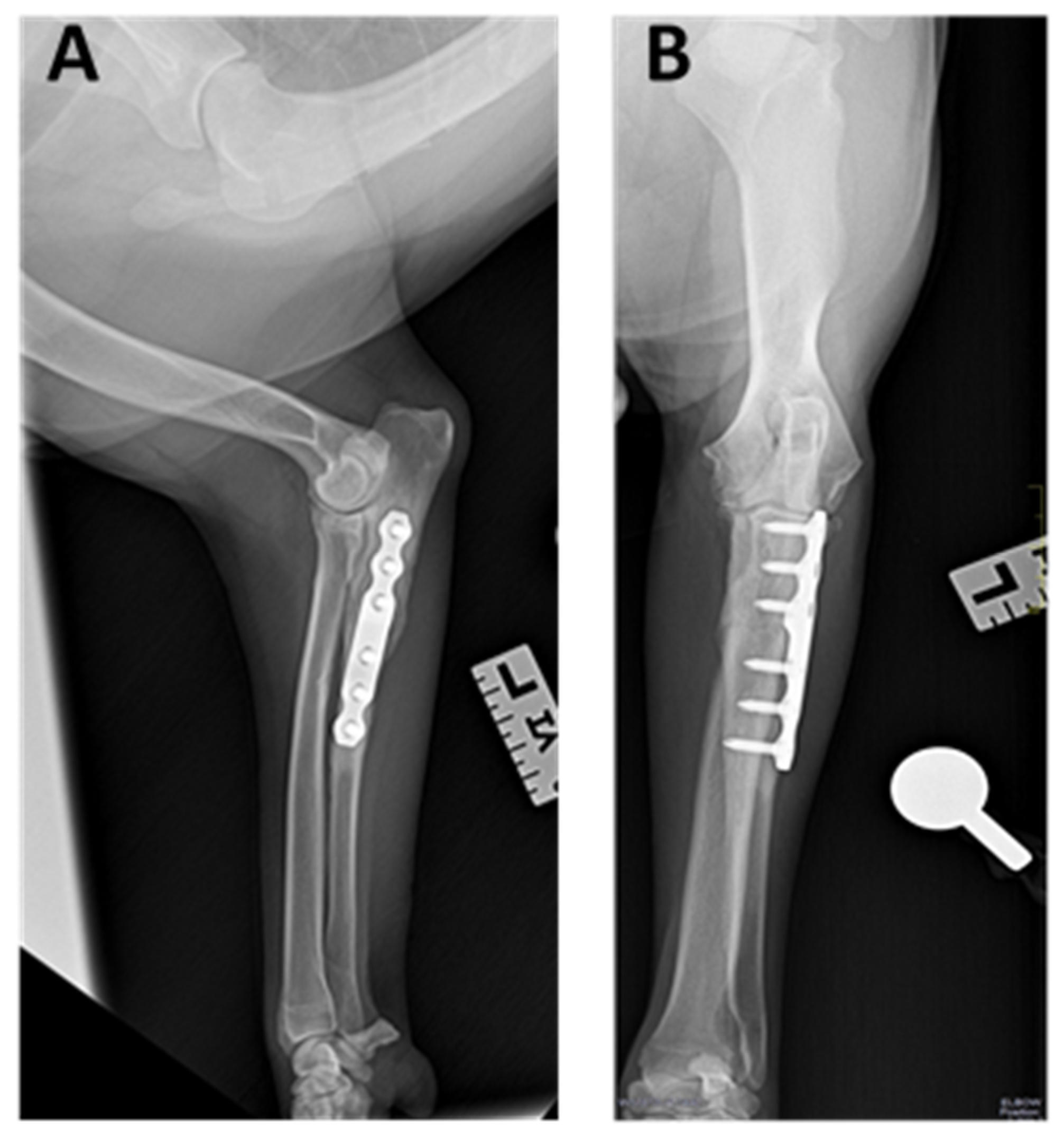
3.3. Radiographic Outcomes
3.4. Minor and Major Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Animal name: | Forelimb: |
| Surname: | Data surgical: |
| Breed: | Age at surgery: |
| Weight: | Size of the plate: |
| Sex: | Plate step: |
| Time 0 (before Surgery) | Time 4 Months (after Surgery) | Time 12 Months (after Surgery) | Present | |
| How well can your dog walk without pain? 0: not painful 10: painful | ||||
| How well can your dog run without pain? 0: not painful 10: painful | ||||
| How well can your dog climb UP stairs? 0: very well 10: poorly | ||||
| How well can your dog climb DOWN stairs? 0: very well 10: poorly | ||||
| What is your dog´s exercise tolerance (ability to go for walks without stopping or tiring)? 0: Copes fine with long walks 10: Struggles on short walks | ||||
| How well can your dog sit down without pain or hesitation 0: very well 10: poorly | ||||
| How well can your dog lie down without pain or hesitation? 0: very well 10: poorly | ||||
| How well can your dog rise on front legs without pain or hesitation? 0: very well 10: poorly | ||||
| Does your dog nod his/her head at walk? 0: not at all 10: lots | ||||
| Does your dog nod his/her head at run? 0: not at all 10: lots | ||||
| How would you grade the success of the operation? 0: poor 10: excellent | ||||
| Would you have this operation done again in the same circunstances? 0: never 10: definitely |
References
- Samoy, Y.; Van Ryssen, B.; Gielen, I.; Walschot, N.; Van Bree, H. Elbow incongruity in the dog. Vet. Comp. Orthop. Traumatol. 2006, 1, 1–8. [Google Scholar]
- Fitzpatrick, N.; Bertran, J.; Solano, M.A. Sliding humeral osteotomy: Medium-term objective outcome measures and reduction of complications with a modified technique. Vet. Surg. 2015, 44, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Wendelburg, K.M.; Beale, B.S. Medium and long term evaluation of sliding humeral osteotomy in dogs. Vet. Surg. 2014, 43, 804–813. [Google Scholar] [CrossRef] [PubMed]
- Barthélémy, N.P.; Griffon, D.J.; Ragetly, G.R.; Carrera, I.; Schaeffer, D.J. Short- and long-term outcomes after arthroscopic treatment of young large breed dogs with medial compartment disease of the elbow. Vet. Surg. 2014, 43, 935–943. [Google Scholar] [CrossRef] [PubMed]
- Cook, C.R.; Cook, J.L. Diagnostic imaging of canine elbow dysplasia: A review. Vet. Surg. 2009, 38, 144–153. [Google Scholar] [CrossRef]
- Fitzpatrick, N.; Yeadon, R.; Smith, T.; Schulz, K. Techniques of application and initial clinical experience with sliding humeral osteotomy for treatment of medial compartment disease of the canine elbow. Vet. Surg. 2009, 38, 261–278. [Google Scholar] [CrossRef]
- Fitzpatrick, N.; Yeadon, R. Working algorithm for treatment decision making for developmental disease of the medial compartment of the elbow in dogs. Vet. Surg. 2009, 38, 285–300. [Google Scholar] [CrossRef]
- Coppieters, E.; Gielen, I.; Verhoeven, G.; Van Vynckt, D.; Van Ryssen, B. Erosion of the medial compartment of the canine elbow: Occurrence, diagnosis and currently available treatment options. Vet. Comp. Orthop. Traumatol. 2015, 28, 9–18. [Google Scholar]
- Lau, S.F.; Wolschrijn, C.F.; Hazewinkel, H.A.W.; Siebelt, M.; Voorhout, G. The early development of medial coronoid disease in growing Labrador retrievers: Radiographic, computed tomographic, necropsy and micro-computed tomographic findings. Vet. J. 2013, 197, 724–730. [Google Scholar] [CrossRef]
- Fitzpatrick, N.; Garcia, T.C.; Daryani, A.; Bertran, J.; Watari, S.; Hayashi, K. Micro-CT structural analysis of the canine medial coronoid disease. Vet. Surg. 2016, 45, 336–346. [Google Scholar] [CrossRef]
- Fitzpatrick, N.; Smith, T.J.; Evans, R.B.; Yeadon, R. Radiographic and arthroscopic findings in the elbow joints of 263 dogs with medial coronoid disease. Vet. Surg. 2009, 38, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Lau, S.F.; Theyse, L.F.H.; Voorhout, G.; Hazewinkel, H.A.W. Radiographic, computed tomographic, and arthroscopic findings in Labrador retrievers with medial coronoid disease. Vet. Surg. 2015, 44, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Moores, A.P.; Benigni, L.; Lamb, C.R. Computed tomography versus arthroscopy for detection of canine elbow dysplasia lesions. Vet. Surg. 2008, 37, 390–398. [Google Scholar] [CrossRef] [PubMed]
- Burton, N.J.; Owen, M.R.; Kirk, L.S.; Toscano, M.J.; Colborne, G.R. Conservative versus arthroscopic management for medial coronoid process disease in dogs: A prospective gait evaluation. Vet. Surg. 2011, 40, 972–980. [Google Scholar] [CrossRef] [PubMed]
- Mason, D.R.; Schulz, K.S.; Fujita, Y.; Kass, P.H.; Stover, S.M. Measurement of humeroradial and humeroulnar transarticular joint forces in the canine elbow joint after humeral wedge and humeral slide osteotomies. Vet. Surg. 2008, 37, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Tichenor, M.; Millis, D. Treatment of medial compartment disease of the canine elbow using proximal abduction ulnar osteotomy procedure and a custom kyon plate. Vet. Comp. Orthop. Traumatol. 2014, 4, A31–A32. [Google Scholar]
- Caron, A.; Fitzpatrick, N. Bi-Oblique Dynamic Proximal Ulnar Osteotomy: Surgical Technique and Clinical Outcome in 86 Dogs. Vet. Surg. 2016, 45, 356–363. [Google Scholar] [CrossRef]
- Ortiz, S.; Moratalla, V.; Alegre, D.; Navarro, P.; Soler, C.; Serra, C.I. Medial compartment disease of the canine elbow. Evaluation of dog’s owners satisfaction undergoing proximal abducting ulnar osteotomy. Preliminary study. Clin. Vet. Peq. Anim. 2017, 37, 33–41. [Google Scholar]
- Amadio, A.; Corriveau, K.M.; Norby, B.O.; Stephenson, T.R.; Saunders, W.B. Effect of proximal abducting ulnar osteotomy (PAUL) on frontal plane thoracic limb alignment: An ex vivo canine study. Vet. Surg. 2020, 49, 1437–1448. [Google Scholar] [CrossRef]
- Pfeil, I.; Tepic, S. Proximal ulnar osteotomy for elbow dysplasia. In Proceedings of the Kyon Symposium, Zurich, Switzerland, 13–14 October 2010. [Google Scholar]
- McConkey, M.J.; Valenzano, D.M.; Wei, A. Effect of the Proximal Abducting Ulnar Osteotomy on Intra-Articular Pressure Distribution and Contact Mechanics of Congruent and Incongruent Canine Elbows Ex Vivo. Vet. Surg. 2016, 45, 347–355. [Google Scholar] [CrossRef]
- Coghill, F.J.; Ho-Eckart, L.K.; Baltzer, W.I. Mid- to Long-Term Outcome after Arthroscopy and Proximal Abducting Ulnar Osteotomy versus Arthroscopy Alone in Dogs with Medial Compartment Disease: Thirty Cases. Vet. Comp. Orthop. Traumatol. 2021, 34, 085–090. [Google Scholar] [CrossRef] [PubMed]
- Reid, J.; Nolan, A.M.; Hughes, J.M.L.; Lascelles, D.; Pawson, P.; Scott, E.M. Development of the short-form Glasgow Composite Measure Pain Scale (CMPS-SF) and derivation of an analgesic intervention score. Anim. Welf. 2007, 16, 97–104. [Google Scholar]
- R Core Team. R. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 29 December 2021).
- Mair, P.; Wilcox, R.R. Robust Statistical Methods in R Using the WRS2 Package. Behav. Res. Methods 2020, 52, 464–488. [Google Scholar] [CrossRef]
- Meyer-Lindenberg, A.; Langhann, A.; Fehr, M.; Nolte, I. Arthrotomy versus arthroscopy in the treatment of the fragment medial coronoid process of the ulna (FCP) in 421 dogs. Vet. Comp. Orthop. Traumatol. 2003, 16, 204–210. [Google Scholar]
- Fitzpatrick, N.; Smith, T.J.; Evans, R.B.; O’Riordan, J.; Yeadon, R. Subtotal coronoid ostectomy for treatment of medial coronoid disease in 263 dogs. Vet. Surg. 2009, 38, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Samoy, Y.C.A.; Bakker, E.; Van Vynckt, D.; Coppieters, E.; Van Bree, H.; Van Ryssen, B. Arthroscopic treatment of fragmented coronoid process with severe elbow incongruity. Vet. Comp. Orthop. Traumatol. 2013, 1, 27–33. [Google Scholar]
- Coppieters, E.; Seghers, H.; Verhoeven, G.; Samoy, Y.; De Bakker, E.; Van Ryssen, B. Arthroscopic, computed tomography, and radiographic findings in 25 dogs with lameness after arthroscopic treatment of medial coronoid disease. Vet. Surg. 2016, 45, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Vezzoni, A.; Benjamino, K. Canine Elbow Dysplasia: Ununited Anconeal Process, Osteochondritis Dissecans, and Medial Coronoid Process Disease. Vet. Clin. Small Anim. 2021, 51, 439–474. [Google Scholar] [CrossRef] [PubMed]
- Michelsen, J. Canine elbow dysplasia: Aetiopathogenesis and current treatment recommendations. Vet. J. 2013, 196, 12–19. [Google Scholar] [CrossRef]
- Bruecker, K.A.; Benjamino, K.; Vezzoni, A.; Walls, C.; Wendelburg, K.L.; Follette, C.M.; Guillou, R. Canine Elbow Dysplasia Medial Compartment Disease and Osteoarthritis. Vet. Clin. Small Anim. 2021, 51, 475–515. [Google Scholar] [CrossRef]
- Danielski, A.; Krekis, A.; Yeadon, R.; Solano, M.A.; Parkin, T.; Vezzoni, A. Complications after proximal abducting ulnar osteotomy and prognostic factors in 66 dogs. Vet. Surg. 2022, 51, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Puccio, M.; Marino, D.J.; Stefanacci, J.D.; McKenna, B. Clinical evaluation and long-term follow-up of dogs having coronoidectomy for elbow incongruity. J. Am. Anim. Hosp. Assoc. 2003, 39, 473–478. [Google Scholar] [CrossRef] [PubMed]


| Case | Breed | Sex | Weight (Kg) | Forelimb | Age Surgery (Months) | Size Plate (Number) | Plate Step (mm) | Follow-up (Months) |
|---|---|---|---|---|---|---|---|---|
| 1 | German Shepherd | Female | 27 | Right | 10 | 9 | 3 | 12 |
| 2 | German Shepherd | Female | 32 | Left | 14 | 10 | 3 | 12 |
| 3 | Labrador Retriever | Male | 23 | Right | 10 | 9 | 3 | 12 |
| 4 | Labrador Retriever | Male | 26 | Left | 14 | 9 | 3 | 12 |
| 5 | Pitbull Terrier | Female | 32 | Left | 30 | 9 | 3 | 61 |
| 6 | Golden Retriever | Male | 30 | Left | 18 | 9 | 3 | 12 |
| 7 | American Bulldog | Male | 43 | Right | 24 | 10 | 3 | 55 |
| 8 | Newfoundland | Male | 49 | Right | 13 | 11 | 3 | 57 |
| 9 | Newfoundland | Male | 50.5 | Left | 20 | 11 | 3 | 51 |
| 10 | Pitbull Terrier | Female | 24 | Right | 10 | 9 | 3 | 53 |
| 11 | Mixed | Male | 32.4 | Left | 7 | 10 | 3 | 4 |
| 12 | Australian Shepherd | Male | 41 | Left | 7 | 10 | 2 | 39 |
| 13 | Labrador Retriever | Male | 35.8 | Left | 11 | 10 | 2 | 12 |
| 14 | Golden Retriever | Male | 33 | Left | 11 | 10 | 2 | 34 |
| 15 | Mixed | Female | 22.6 | Right | 7 | 9 | 2 | 33 |
| 16 | Pitbull Terrier | Male | 32 | Right | 7 | 10 | 2 | 33 |
| 17 | Pitbull Terrier | Male | 24 | Right | 108 | 9 | 2 | 33 |
| 18 | Bernese Mountain | Male | 37 | Right | 18 | 10 | 2 | 33 |
| 19 | Pitbull Terrier | Male | 30.5 | Left | 11 | 10 | 2 | 30 |
| 20 | Argentin Dogo | Female | 30 | Right | 18 | 9 | 2 | 28 |
| 21 | Rottweiler | Female | 38 | Left | 24 | 10 | 2 | 27 |
| 22 | Mixed | Female | 27 | Left | 12 | 9 | 2 | 26 |
| 23 | Labrador Retriever | Male | 35.8 | Right | 24 | 10 | 2 | 4 |
| 24 | Mixed | Female | 21.1 | Left | 36 | 9 | 2 | 21 |
| 25 | German Shepherd | Male | 26.4 | Right | 43 | 9 | 2 | 20 |
| 26 | Pitbull Terrier | Male | 24 | Left | 119 | 9 | 2 | 20 |
| 27 | Labrador Retriever | Male | 39.7 | Right | 60 | 10 | 2 | 19 |
| 28 | Giant Schnauzer | Male | 43.1 | Left | 24 | 11 | 2 | 16 |
| 29 | Labrador Retriever | Female | 32 | Left | 84 | 9 | 2 | 14 |
| 30 | Labrador Retriever | Male | 35 | Left | 30 | 10 | 2 | 14 |
| 31 | Golden Retriever | Male | 41 | Left | 24 | 10 | 2 | 12 |
| 32 | Labrador Retriever | Male | 42 | Right | 48 | 10 | 2 | 4 |
| 33 | Caucasian Shepherd | Male | 35 | Left | 12 | 10 | 2 | 4 |
| T0 vs. T4 | T0 vs. T12 | T0 vs. TP | T4 vs. T12 | T4 vs. TP | T12 vs. TP | |
|---|---|---|---|---|---|---|
| A | <0.01 | <0.01 | <0.01 | 0.06 | 0.57 | 0.36 |
| B | 0.11 | <0.01 | 0.45 | 0.08 | 0.77 | 0.51 |
| C | 0.13 | <0.05 | 0.19 | 0.1 | 0.68 | 0.32 |
| D | <0.05 | <0.05 | 0.08 | 0.25 | 0.4 | 0.27 |
| E | 0.08 | 0.06 | 0.18 | 0.66 | 0.44 | 0.74 |
| F | 0.05 | 0.36 | 0.5 | 0.63 | 0.34 | 0.3 |
| G | 0.08 | 0.3 | 0.51 | 0.67 | 0.23 | 0.34 |
| H | 0.06 | 0.06 | <0.05 | 1 | 0.91 | 0.92 |
| I | <0.05 | <0.05 | 0.08 | 0.2 | 0.53 | 0.5 |
| J | 0.15 | 0.14 | 0.41 | 0.08 | 0.53 | 0.42 |
| K | - | - | - | 0.08 | 0.53 | 0.42 |
| L | - | - | - | 0.75 | 0.75 | 0.37 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ballester, C.O.; Canet, C.S.; García, J.I.R.; Salesa, N.F.; Canet, V.S.; Aguado, C.I.S. Proximal Abduction Ulnar Osteotomy (PAUL): Short- and Long-Term Evaluation in Dogs Presenting Medial Compartment Disease. Animals 2022, 12, 466. https://doi.org/10.3390/ani12040466
Ballester CO, Canet CS, García JIR, Salesa NF, Canet VS, Aguado CIS. Proximal Abduction Ulnar Osteotomy (PAUL): Short- and Long-Term Evaluation in Dogs Presenting Medial Compartment Disease. Animals. 2022; 12(4):466. https://doi.org/10.3390/ani12040466
Chicago/Turabian StyleBallester, Carolina Oliver, Carme Soler Canet, José Ignacio Redondo García, Nuria Fernández Salesa, Vicente Sifre Canet, and Claudio Iván Serra Aguado. 2022. "Proximal Abduction Ulnar Osteotomy (PAUL): Short- and Long-Term Evaluation in Dogs Presenting Medial Compartment Disease" Animals 12, no. 4: 466. https://doi.org/10.3390/ani12040466
APA StyleBallester, C. O., Canet, C. S., García, J. I. R., Salesa, N. F., Canet, V. S., & Aguado, C. I. S. (2022). Proximal Abduction Ulnar Osteotomy (PAUL): Short- and Long-Term Evaluation in Dogs Presenting Medial Compartment Disease. Animals, 12(4), 466. https://doi.org/10.3390/ani12040466






