Canine Seventh Lumbar Vertebra Fracture: A Systematic Review
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Aim and Literature Search Strategy
2.2. Study Selection
2.3. Data Extraction
3. Results
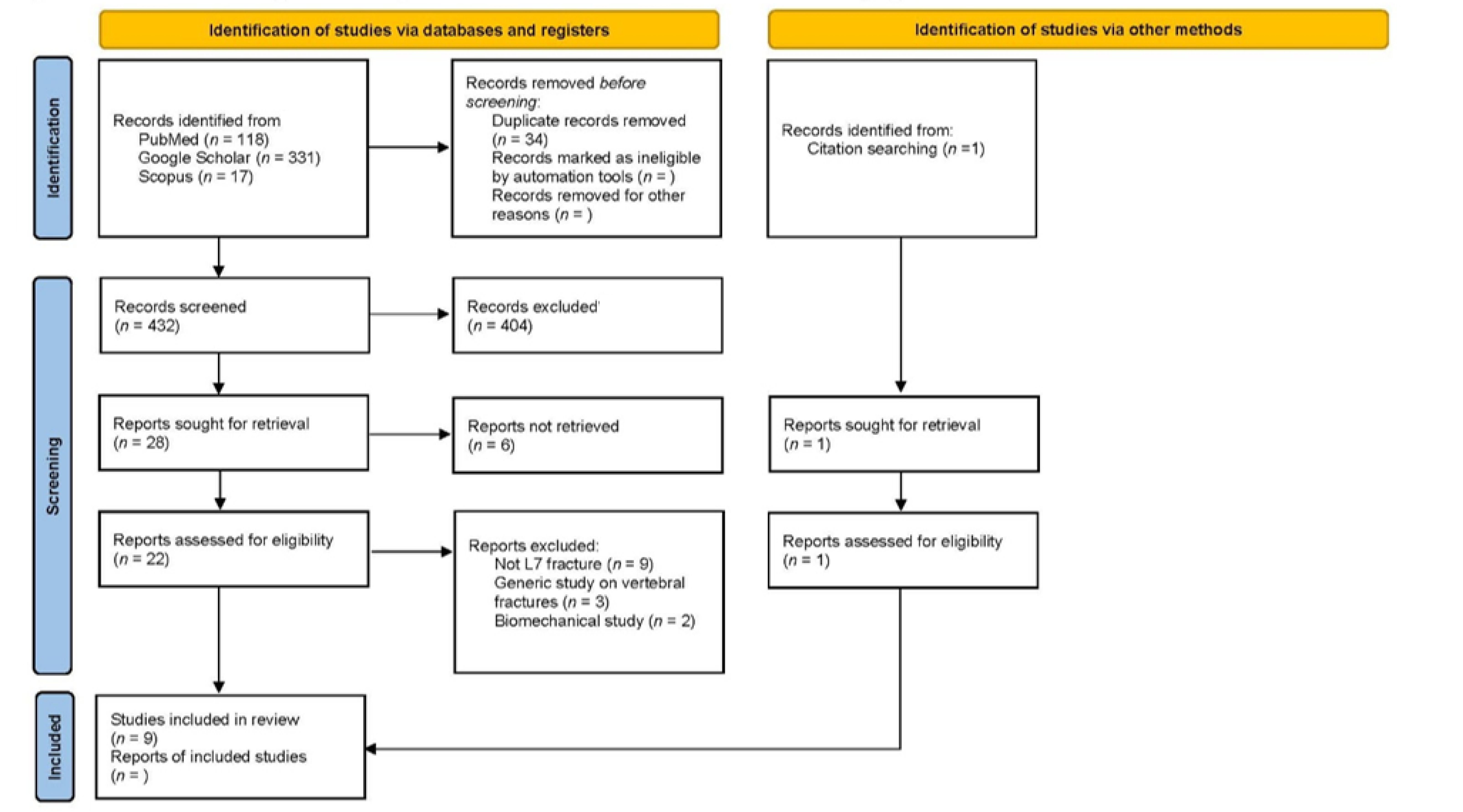
3.1. Database Review
3.2. Anatomical and Biomechanical Considerations
3.3. Clinical Presentation
3.4. Imaging
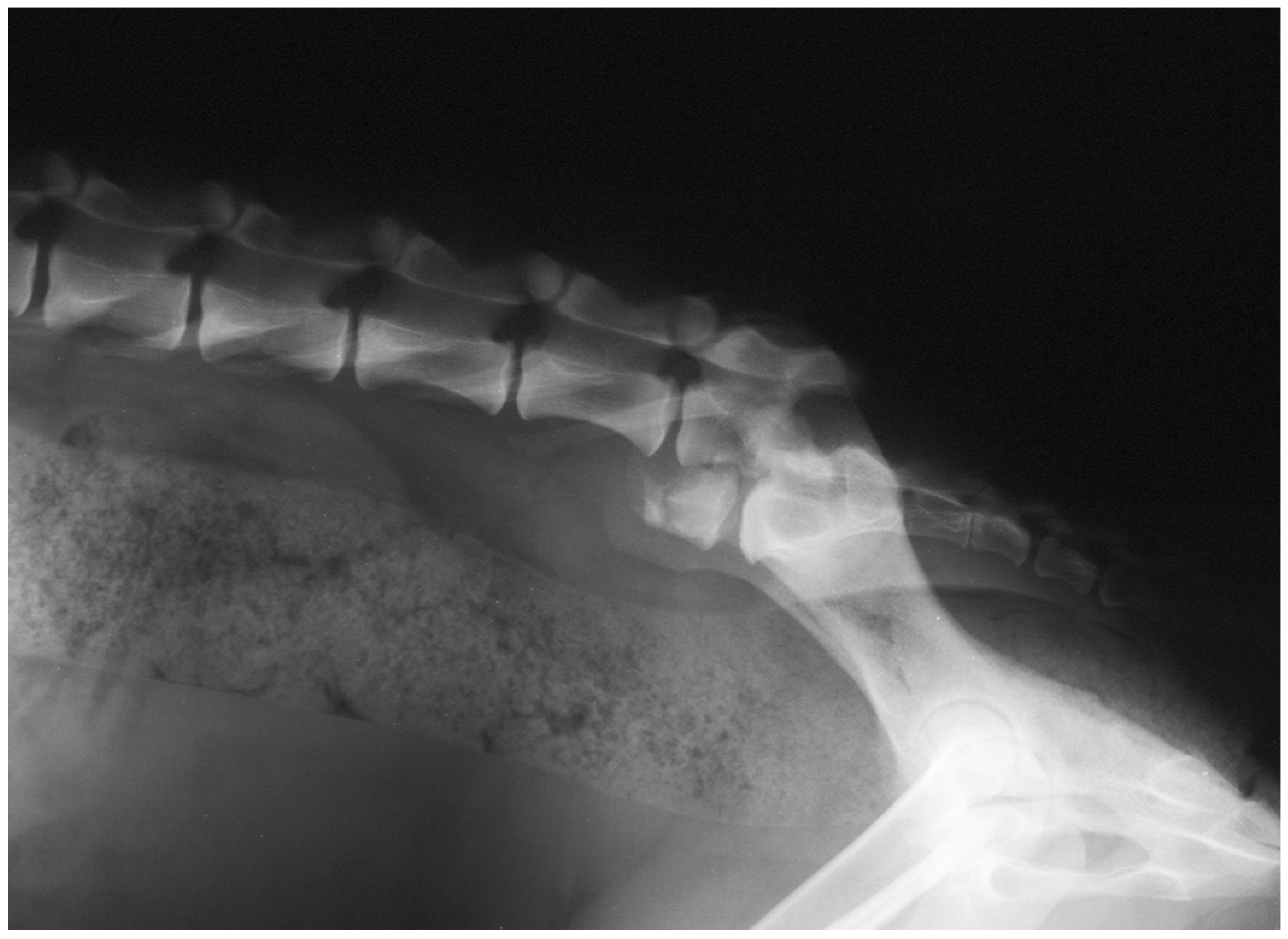
3.5. Treatment
3.6. Complications and Prognosis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Turner, W.D. Fractures and fracture-luxations of the lumbar spine: A retrospective study in the dog. J. Am. Anim. Hosp. Assoc. 1987, 23, 459–464. [Google Scholar]
- Selcer, R.R.; Bubb, W.J.; Walker, T.L. Management of vertebral column fractures in dogs and cats: 211 cases (1977–1985). J. Am. Vet. Med. Assoc. 1991, 198, 1965–1968. [Google Scholar] [PubMed]
- Jeffery, N.D. Vertebral fracture and luxation in small animals. Vet. Clin. N. Am. Small Anim. Pract. 2010, 40, 809–828. [Google Scholar] [CrossRef]
- Bali, M.S.; Lang, J.; Jaggy, A.; Spreng, D.; Doherr, M.G.; Forterre, F. Comparative study of vertebral fractures and luxations in dogs and cats. Vet. Comp. Orthop. Traumatol. 2009, 22, 47–53. [Google Scholar] [CrossRef] [Green Version]
- Di Dona, F.; Della Valle, G.; Lamagna, B.; Balestriere, C.; Murino, C.; Santangelo, B.; Lamagna, F.; Fatone, G. Percutaneous transilial pinning for treatment of seventh lumbar vertebral body fracture: A retrospective analysis of 17 cases. Vet. Comp. Orthop. Traumatol. 2016, 29, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Della Valle, G.; Di Dona, F.; Mennonna, G.; Lamagna, B.; Pasolini, M.P.; Caterino, C.; Lamagna, F.; Fatone, G. Traumatic lumbosacral joint dislocation in 3 dogs: Clinical presentation, diagnosis, treatment and short-term follow-up. Pak. Vet. J. 2021, 41, 97–101. [Google Scholar] [CrossRef]
- Slocum, B.; Rudy, R.L. Fractures of the seventh lumbar vertebra in the dog. J. Am. Anim. Hosp. Assoc. 1975, 11, 167–174. [Google Scholar]
- McAnulty, J.F.; Lenehan, T.M.; Maletz, L.M. Modified Segmental Spinal Instrumentation in Repair of Spinal Fractures and Luxations in Dogs. Vet. Surg. 1986, 15, 143–149. [Google Scholar] [CrossRef]
- Shores, A.; Nichols, C.; Rochat, M.; Fox, S.M.; Burt, G.J.; Fox, W.R. Combined Kirschner-Ehmer device and dorsal spinal plate fixation technique for caudal lumbar vertebral fractures in dogs. J. Am. Vet. Med. Assoc. 1989, 195, 335–339. [Google Scholar]
- Ullman, S.L.; Boudrieau, R.J. Internal Skeletal Fixation Using a Kirschner Apparatus for Stabilization of Fracture/Luxations of the Lumbosacral Joint in Six Dogs: A Modification of the Transilial Pin Technique. Vet. Surg. 1993, 22, 11–17. [Google Scholar] [CrossRef]
- Harrington, M.L.; Bagley, R.S. Realignment of a Seventh Lumbar Vertebral Fracture/Luxation Using a Senn Retractor in Two Puppies. J. Am. Anim. Hosp. Assoc. 1998, 34, 377–380. [Google Scholar] [CrossRef]
- Beaver, D.P.; MacPhersont, G.C.; Muir, P.; Johnson, K.A. Methyl-methacrylate and bone screw repair of seventh lumbar vertebral fracture-luxations in dogs. J. Small Anim. Pract. 1996, 37, 381–386. [Google Scholar] [CrossRef]
- Weh, J.M.; Kraus, K.H. Use of a four pin and methylmethacrylate fixation in L7 and the iliac body to stabilize lumbosacral fracture-luxations: A clinical and anatomic study. Vet. Surg. 2007, 36, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Krauss, M.W.; Theyse, L.F.H.; Tryfonidou, M.A.; Hazewinkel, H.A.W.; Meij, B.P. Treatment of spinal fractures using Lubra plates: A retrospective clinical and radiological evaluation of 15 cases. Vet. Comp. Orthop. Traumatol. 2012, 25, 326–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Segal, U.; Bar, H.; Shani, J. Repair of lumbosacral fracture–luxation with bilateral twisted string-of-pearls locking plates. J. Small Anim. Pract. 2018, 59, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dulisch, M.L.; Nichols, J.B. A Surgical Technique for Management of Lower Lumbar Fractures: Case Report. Vet. Surg. 1981, 10, 90–93. [Google Scholar] [CrossRef]
- Wheeler, J.L.; Lewis, D.D.; Cross, A.R.; Sereda, C.W. Closed fluoroscopic-assisted spinal arch external skeletal fixation for the stabilization of vertebral column injuries in five dogs. Vet. Surg. 2007, 36, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Hermanson, J.W.; de Lahunta, A. Spinal Cord and Meninges. In Miller’s Anatomy of the Dog, 5th ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2018; pp. 589–610. [Google Scholar]
- Denis, F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin. Orthop. Relat. Res. 1984, 189, 65–76. [Google Scholar] [CrossRef]
- Barquet, A.; Menendez, J.; Dubra, A.; Masliah, R.; Pereyra, D. Anterolateral dislocation of the lumbosacral junction. Can. Assoc. Radiol. J. 1993, 44, 129–132. [Google Scholar] [PubMed]
- Sturges, B.K.; Kapatkin, A.S.; Garcia, T.C.; Anwer, C.; Fukuda, S.; Hitchens, P.L.; Wisner, T.; Hayashi, K.; Stover, S.M. Biomechanical Comparison of Locking Compression Plate versus Positive Profile Pins and Polymethylmethacrylate for Stabilization of the Canine Lumbar Vertebrae. Vet. Surg. 2016, 45, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Nel, J.J.; Kat, C.J.; Coetzee, G.L.; van Staden, P.J. Biomechanical comparison between pins and polymethylmethacrylate and the SOP locking plate system to stabilize canine lumbosacral fracture-luxation in flexion and extension. Vet. Surg. 2017, 46, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, J.L.; Cross, A.R.; Rapoff, A.J. A comparison of the accuracy and safety of vertebral body pin placement using a fluoroscopically guided versus an open surgical approach: An in vitro study. Vet. Surg. 2002, 31, 468–474. [Google Scholar] [CrossRef]
- Watine, S.; Cabassu, J.P.; Catheland, S.; Brochier, L.; Ivanoff, S. Computed tomography study of implantation corridors in canine vertebrae. J. Small Anim. Pract. 2006, 47, 651–657. [Google Scholar] [CrossRef]
- Oberli, H.; Frigg, R.; Schenk, R. [External fixator: Surgical technique, pinless fixator, change in procedure]. Helv. Chir. Acta 1994, 60, 1073–1080. [Google Scholar]
- Clary, E.M.; Roe, S.C. In Vitro Biomechanical and Histological Assessment of Pilot Hole Diameter for Positive-Profile External Skeletal Fixation Pins in Canine Tibiae. Vet. Surg. 1996, 25, 453–462. [Google Scholar] [CrossRef]
- Lanz, O.I. Lumbosacral and pelvic injuries. Vet. Clin. N. Am. Small Anim. Pract. 2002, 32, 949–962. [Google Scholar] [CrossRef]
| Authors | Study Design | N. Cases | Paresis Ambulatory | Paresis/Plegia | Sciatic Nerve Sensitivity | Urinary/Faecal Incontinence | Post-Operative Recovery | Technique | Year |
|---|---|---|---|---|---|---|---|---|---|
| Dulish et al. | Case report | 1 | 0 | 1 | 1 | 1 | 100% | Transilial pins and plastic plates | 1981 |
| McAnulty et al. | Case series | 1 | 0 | 1 | 0 | 1 | 100% | Transilial pins | 1986 |
| Ullman et al. | Case series | 6 | 6 | 0 | 0 | 6 | 100% | Double crossed pins | 1993 |
| Beaver et al. | Case series | 2 | 0 | 2 | 2 | 2 | 100% | Screws and PMMA | 1996 |
| Harrington et al. | Case series | 2 | 1 | 1 | 0 | 1 | 100% | Pins and PMMA | 1998 |
| Wheeler et al. | Case series | 1 | 0 | 1 | 1 | 1 | 100% | Trans-sacral and transilial pins | 2007 |
| Weh et al. | Case series | 5 | 1 | 4 | 1 | 0 | 100% | Pins and PMMA | 2007 |
| Di Dona et al. | Case series | 17 | 5 | 12 | 3 | 6 | 100% | double transilial pins | 2016 |
| Segal et al. | Case series | 6 | 2 | 4 | 3 | 2 | 100% | SOP plates | 2018 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caterino, C.; Aragosa, F.; Della Valle, G.; Fatone, G. Canine Seventh Lumbar Vertebra Fracture: A Systematic Review. Animals 2022, 12, 193. https://doi.org/10.3390/ani12020193
Caterino C, Aragosa F, Della Valle G, Fatone G. Canine Seventh Lumbar Vertebra Fracture: A Systematic Review. Animals. 2022; 12(2):193. https://doi.org/10.3390/ani12020193
Chicago/Turabian StyleCaterino, Chiara, Federica Aragosa, Giovanni Della Valle, and Gerardo Fatone. 2022. "Canine Seventh Lumbar Vertebra Fracture: A Systematic Review" Animals 12, no. 2: 193. https://doi.org/10.3390/ani12020193
APA StyleCaterino, C., Aragosa, F., Della Valle, G., & Fatone, G. (2022). Canine Seventh Lumbar Vertebra Fracture: A Systematic Review. Animals, 12(2), 193. https://doi.org/10.3390/ani12020193







