Simple Summary
Luteal deficiency is defined as reduced progesterone production by the corpus luteum, either in the amount or duration, or both. The clinical manifestations include primary infertility and pregnancy loss during the late embryonic/early fetal period (30–50 days post-AI). This work provides a clinical overview of the current understanding of luteal deficiency and its association with low fertility in dairy cows.
Abstract
Luteal deficiency is defined as reduced progesterone (P4) steroidogenesis by the corpus luteum (CL), either in the amount or duration, or both. This work provides a clinical overview of the current understanding of luteal deficiency and its association with low fertility in dairy cows. Low plasma P4 concentrations during the luteal phase post-artificial insemination (AI) are associated with lower conception rates. Treatments post-AI with P4, gonadotropin-releasing hormone (GnRH) or human chorionic gonadotropin (hCG) improve fertility in some conditions. Sub-luteal function during the late embryonic period (at pregnancy diagnosis, i.e., 28–34 days post-AI), is just one factor among other factors associated with pregnancy loss. Treatment with P4 in cows with one CL favors pregnancy maintenance, while GnRH treatment does the same in cows carrying twins. The diagnosis of sub-luteal function can be made clinically on the basis of plasma or milk P4 concentrations. Automated in-line milk P4 analysis systems to diagnose luteal activity emerge as a very interesting tool in dairy herds. Monitoring plasma or milk P4 concentrations with the help of Doppler ultrasonography to assess the CL function would allow individualizing the luteal phase support.
1. Introduction
Luteal phase deficiency was defined in 1949 as reduced progesterone (P4) steroidogenesis by the human corpus luteum (CL), either in the amount or duration, or both [1]. The clinical manifestations of the defect in women include primary infertility and repeated first trimester abortions [2,3]. As a consequence, luteal phase support during the first six weeks of gestation is regarded as an essential condition for the success of assisted human reproduction procedures [4,5]. In cattle, although the concept of luteal deficiency has been scarcely developed [6,7,8], the clinical manifestations of a poor luteal function are similar to those in humans. Indeed, therapies applied in the early luteal phase post-artificial insemination (AI) or during the late-embryonic period improve the fertility in some cow subpopulations. This work provides a clinical overview of the current understanding of luteal deficiency and its association with low fertility in dairy cattle.
2. The Early Luteal Phase of Pregnancy
Low plasma P4 concentrations during the luteal phase post-AI have been extensively associated with lower conception rates [9,10]. This demands treatments post-AI with P4, gonadotropin-releasing hormone (GnRH) or human chorionic gonadotropin (hCG) to improve fertility in some herds. In effect, the results of recent meta-analyses, including data from a total of 59,584 cows, indicate that P4, GnRH or hCG treatment in the early luteal phase of pregnancy improves fertility, particularly in cows of lower fertility [11,12,13]. Certainly, poor luteal activity following ovulation may turn a cow into a repeat breeder [14,15]. In high-producing dairy herds, the incidence of repeat breeding can greatly exceed 20% [16,17].
3. The Late Embryonic Period
The period of gestation is divided into embryonic, from conception to the end of differentiation (approximately 45 days), and fetal, from completion of differentiation to parturition [18]. In high-producing dairy herds, pregnancy diagnosis is commonly performed in the late embryonic period, and up to 20% of pregnancies are lost within 30–50 days of gestation [19,20,21]. Beyond this time interval, the risk of losses is much lower. In a similar way to the luteal period post-AI, reduced plasma P4 concentrations at pregnancy diagnosis have often been associated with pregnancy loss [21,22]. Two facts reinforce this perception. First, the presence of additional CL (more CL than the number of embryos) has been strongly linked to pregnancy maintenance [20]. Second, P4 treatment at pregnancy diagnosis may reduce the incidence of pregnancy loss in single pregnancies [23,24,25]. However, in contrast to the early luteal phase of pregnancy, treatment with GnRH or hCG at pregnancy diagnosis has not been found to reduce pregnancy loss in studies, including all pregnant cows [26,27], and P4 treatment may increase the likelihood of pregnancy loss up to three times in cows with two or more CL when compared to GnRH treatment [25]. Due to its immunosuppressive role, too high levels of P4 probably do not favor cases of spontaneous twin reduction in which conceptus remnants may determine pregnancy loss. In contrast, GnRH treatment favors pregnancy maintenance and is linked to an increased twin reduction rate in cows carrying twins [25,28].
The CL regression causes embryonic death, or if vice versa, luteal regression is detected at least 3 days after the detection of the embryonic death [29]. Sub-luteal function is just one factor among other factors associated with pregnancy loss. This explains why post-AI treatment with P4, GnRH or hCG appears to have no effect on subsequent pregnancy loss [30]. Consequently, sub-luteal function in the luteal phase post-AI can be independent from luteal deficiency in the late embryonic period. If so, therapies should be established for each time point.
4. Diagnostic Tools for Luteal Deficiency
Numerous mechanisms are involved in the formation and regulation of luteal structures [31,32]. So, we can expect that the function of the CL is influenced by many factors. For example, poor luteal activity has been associated with the intense metabolism and steroid hormone clearance of high milk production [33,34]. Heat stress is also a main factor impairing the CL function [35,36,37]. Luteal deficiency, therefore, is not due to a single etiology, and an etiologic diagnosis may be difficult or impossible to establish in routine clinical practice. Irrespective of its origin, the diagnosis of sub-luteal function can be performed clinically on the basis of plasma or milk P4 concentrations. Post-ovulatory increase in plasma P4 concentrations is strongly correlated with pregnancy success [38], while advanced (<7 days) or delayed (>11 days) onset of luteal activity post-AI has been associated with a decreased pregnancy rate (9.3 and 12.1%, respectively) when compared to the 7–11 days interval [39]. Eventually, low plasma P4 concentration during the late embryonic period has been related to pregnancy loss [40,41,42]. However, it is difficult to establish a reliable cut-off value for predicting pregnancy loss. It seems that high plasma P4 concentrations are a more useful predictor of pregnancy maintenance than low P4 concentrations are for predicting pregnancy loss [21]. In this context, sequential ovarian brightness (B)-mode ultrasonography plus plasma P4 measurements from AI to pregnancy diagnosis (day 32 post-AI) have proven to be useful tools in diagnosing luteal deficiency [8]. Or better, color-flow Doppler ultrasonography could be used to monitor appropriate luteal vascularization at the time of pregnancy diagnosis (Figure 1). Luteal blood flow, a strong indicator of luteal function, may provide additional information on luteal physiology compared to plasma P4 measurements alone [43,44,45]. Doppler ultrasonography is already used at the time of embryo transfer for selection of recipients [46,47,48]. However, the relationship of CL blood flow with pregnancy maintenance or pregnancy loss has been scarcely studied during the late embryonic period. A positive correlation between CL blood flow and plasma P4 concentrations has been reported in pregnant cows up to day 40 of gestation [49]. Normal and low luteal vascular perfusions shown in Figure 1 are just one example to be confirmed in extensive studies. Doppler blood flow studies should provide significant information about luteal deficiency during the late embryonic period and pregnancy loss and its treatments.
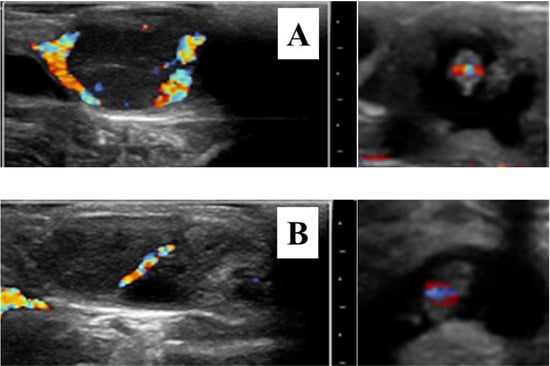
Figure 1.
Color-flow sonograms of corpora lutea and their corresponding 30-day embryos showing normal (A) and low luteal vascular perfusion (B). The apparent luteal vascular decrease in (B) compared to that of (A) was associated with pregnancy loss 14 days later. All images were selected on the basis of maximal vascular perfusion from real-time video clips. Bar spacing: 10 mm.
5. Clinical Perspectives
Pregnancy rate and pregnancy loss are two main reproductive parameters associated with luteal deficiency. Treatments during the early phase of pregnancy usually involve all inseminated cows [11,12,13]. Monitoring daily plasma or milk P4 concentrations during at least two or more cycles should allow individualizing luteal phase support. Cut-off values of P4 concentrations in different conditions are needed to confirm the effectiveness of adjusting treatments in cows with low P4 levels. For on-site assay of progesterone in milk, several validated enzyme immunoassay test kits have been developed, and some of them are commercially available [50,51,52], but they are too expensive to be included in daily screening programs. Even so, following a lengthy and laborious process [53], automated monitoring of P4 in the milking parlor is already possible with a new technology (in-line milk analysis system) [39,54,55,56]. Such systems may be an important tool for reproductive management in dairy herds [57].
6. The Situation in Other Mammalian Species
Luteal deficiency has been focused on in some studies on equine, porcine and dog, which may serve to illustrate major findings or divergences from the dairy cow model. Low levels of circulating P4 have been associated with pregnancy loss in the mare [58] and the bitch [59], and with pregnancy maintenance in the gilt [60]. Therefore, P4 therapy is recommended to reduce the incidence of pregnancy failure in mares and bitches of suspected sub-luteal function [59,60]. In contrast to the cow, controversial results are shown using Doppler ultrasonography to assess the CL function in the selection of equine embryo transfer recipients [61,62]. Turning the point to women, and as has been noted above, luteal deficiency has long been considered a main factor associated with low fertility [1,2,3,4,5]. It should be highlighted that, although the clinical manifestations of a poor luteal activity are similar for women and cows, the intensive protocols used in assisted human reproduction may have had a negative influence on subsequent CL function. This makes P4-based therapies particularly indispensable in women [63,64].
7. Concluding Remarks
In this age in which we are living of transition from clinics to reproductive genomics [65], the establishment of pregnancy following insemination remains the primary goal in most dairy systems [66]. At this juncture, clinical procedures to improve fertility in high-producing dairy herds leave much scope for improvement. In light of the information on sub-luteal function and its influence on dairy cow fertility, three important points stand out. First, luteal deficiency should not be considered in the follow-up work of low fertility alone. Second, treatment with P4, GnRH or hCG in the early luteal phase of pregnancy works well in sub-fertile cows. During the late embryonic period, treatment with P4 favors pregnancy in cows with one CL, while GnRH treatment increases the rate of pregnancy survival in twin pregnancies. Third, monitoring plasma or milk P4 concentrations with the help of Doppler ultrasonography to assess the CL function would allow individualizing the luteal phase support. Large controlled trials will be necessary to improve the efficiency of individualized treatments of luteal deficiency.
Author Contributions
Conceptualization and writing—original draft preparation, F.L.-G. Investigation, writing—review and editing, I.G.-I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All the data provided were extracted from the cited references.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Jones, G.S. The luteal phase defect. Fertil. Steril. 1976, 27, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Csapo, A.I.; Pulkkinen, M. Indispensability of the human corpus luteum in the maintenance of early pregnancy. Luteectomy evidence. Obstet. Gynecol. Surv. 1978, 33, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Practice Committees of the American Society for Reproductive Medicine and the Society for Reproductive Endocrinology and Infertility. Diagnosis and treatment of luteal phase deficiency: A committee opinion. Fertil. Steril. 2021, 115, 1416–1423. [Google Scholar] [CrossRef] [PubMed]
- Van der Linden, M.; Buckingham, K.; Farquhar, C.; Kremer, J.A.M.; Metwally, M. Luteal phase support for assisted reproduction cycles. Hum. Reprod. Update 2012, 18, 473. [Google Scholar] [CrossRef][Green Version]
- Mizrachi, Y.; Horowitz, E.; Ganer Herman, H.; Farhi, J.; Raziel, A.; Weissman, A. Should women receive luteal support following natural cycle frozen embryo transfer? A systematic review and meta-analysis. Hum. Reprod. Update 2021, 27, 643–650. [Google Scholar] [CrossRef]
- Kimura, M.; Nakao, T.; Moriyoshi, M.; Kawata, K. Luteal phase deficiency as a possible cause of repeat breeding in dairy cows. Br. Vet. J. 1987, 143, 560–566. [Google Scholar] [CrossRef]
- Starbuck, G.R.; Gutierrez, C.G.; Peters, A.R.; Mann, G.E. Timing of follicular phase events and the postovulatory progesterone rise following synchronisation of oestrus in cows. Vet. J. 2006, 172, 103–108. [Google Scholar] [CrossRef]
- Pérez-Marín, C.C.; España, F. Oestrus expression and ovarian function in repeat breeder cows, monitored by ultrasonography and progesterone assay. Reprod. Domest. Anim. 2007, 42, 449–456. [Google Scholar] [CrossRef]
- Lukaszewska, J.; Hansel, W. Corpus luteum maintenance during early pregnancy in the cow. J. Reprod. Fertil. 1980, 59, 485–493. [Google Scholar] [CrossRef]
- Mann, G.E.; Lamming, G.E. The influence of progesterone during early pregnancy in cattle. Reprod. Domest. Anim. 1999, 34, 269–274. [Google Scholar] [CrossRef]
- Nascimento, A.B.; Bender, R.W.; Souza, A.H.; Ayres, H.; Araujo, R.R.; Guenther, J.N.; Sartori, R.; Wiltbank, M.C. Effect of treatment with human chorionic gonadotropin on day 5 after timed artificial insemination on fertility of lactating dairy cows. J. Dairy Sci. 2013, 96, 2873–2882. [Google Scholar] [CrossRef]
- Yan, L.; Robinson, R.; Shi, Z.; Mann, G. Efficacy of progesterone supplementation during early pregnancy in cows: A meta-analysis. Theriogenology 2016, 85, 1390–1398. [Google Scholar] [CrossRef]
- Besbaci, M.; Abdelli, A.; Minviel, J.J.; Belabdi, I.; Kaidi, R.; Raboisson, D. Association of pregnancy per artificial insemination with gonadotropin-releasing hormone and human chorionic gonadotropin administered during the luteal phase after artificial insemination in dairy cows: A meta-analysis. J. Dairy Sci. 2020, 103, 2006–2018. [Google Scholar] [CrossRef]
- Gustafsson, H. Studies on follicular dynamics and hormonal asynchrony around ovulation as a potential cause of repeat breeding. Reprod. Domest. Anim. 1988, 33, 139–140. [Google Scholar] [CrossRef]
- Gustafsson, H.; Emanuelson, U. Characterisation of the repeat breeding syndrome in Swedish dairy cattle. Acta Vet. Scand. 2002, 43, 115–125. [Google Scholar] [CrossRef]
- Yusuf, M.; Nakao, T.; Ranasinghe, R.B.; Gautam, G.; Long, S.T.; Yoshida, C.; Koike, K.; Hayashi, A. Reproductive performance of repeat breeders in dairy herds. Theriogenology 2010, 73, 1220–1229. [Google Scholar] [CrossRef]
- López-Gatius, F.; Garcia-Ispierto, I. Treatment with an elevated dose of the GnRH analogue dephereline in the early luteal phase improves pregnancy rates in repeat-breeder dairy cows. Theriogenology 2020, 155, 12–16. [Google Scholar] [CrossRef]
- Committee on Bovine Reproductive Nomenclature. Recommendations for standardizing bovine reproductive terms. Cornell Vet. 1972, 62, 216–237. [Google Scholar]
- Grimard, B.; Freret, S.; Chevallier, A.; Pinto, A.; Ponsart, C.; Humblot, P. Genetic and environmental factors influencing first service conception rate and late embryonic/foetal mortality in low fertility dairy herds. Anim. Reprod. Sci. 2006, 91, 31–44. [Google Scholar] [CrossRef]
- López-Gatius, F. Factors of a noninfectious nature affecting fertility after artificial insemination in lactating dairy cows. A review. Theriogenology 2012, 77, 1029–1041. [Google Scholar] [CrossRef]
- Ealy, A.D.; Seekford, Z.K. Predicting pregnancy loss in dairy cattle. J. Dairy Sci. 2019, 102, 11798–11804. [Google Scholar] [CrossRef]
- Szenci, O. Recent Possibilities for the diagnosis of early pregnancy and embryonic mortality in dairy cows. Animals 2021, 11, 1666. [Google Scholar] [CrossRef]
- López-Gatius, F.; Santolaria, P.; Yániz, J.L.; Hunter, R.H.F. Progesterone supplementation during the early fetal period reduces pregnancy loss in high-yielding dairy cattle. Theriogenology 2004, 62, 1529–1535. [Google Scholar] [CrossRef]
- Alnimer, M.A.; Lubbadeh, W.F. Effect of progesterone (P(4)) intravaginal device (CIDR) to reduce embryonic loss and to synchronize return to oestrus of previously timed inseminated lactating dairy cows. Anim. Reprod. Sci. 2008, 107, 36–47. [Google Scholar] [CrossRef]
- Bech-Sàbat, G.; López-Gatius, F.; García-Ispierto, I.; Santolaria, P.; Serrano, B.; Nogareda, C.; de Sousa, N.M.; Beckers, J.F.; Yániz, J. Pregnancy patterns during the early fetal period in high producing dairy cows treated with GnRH or progesterone. Theriogenology 2009, 71, 920–929. [Google Scholar] [CrossRef]
- Bartolome, J.A.; Kamimura, S.; Silvestre, F.; Arteche, A.C.; Trigg, T.; Thatcher, W.W. The use of a deslorelin implant (GnRH agonist) during the late embryonic period to reduce pregnancy loss. Theriogenology 2006, 65, 1443–1453. [Google Scholar] [CrossRef]
- Stevenson, J.S.; Tiffany, S.M.; Inskeep, E.K. Maintenance of pregnancy in dairy cattle after treatment with human chorionic gonadotropin or gonadotropin-releasing hormone. J. Dairy Sci. 2008, 91, 3092–3101. [Google Scholar] [CrossRef]
- Garcia-Ispierto, I.; López-Gatius, F. The effects of a single or double GnRH dose on pregnancy survival in high producing dairy cows carrying singletons or twins. J. Reprod. Dev. 2018, 64, 523–527. [Google Scholar] [CrossRef]
- Kastelic, J.P.; Northey, D.L.; Ginther, O.J. Spontaneous embryonic death on Days 20 to 40 in heifers. Theriogenology 1991, 35, 351–363. [Google Scholar] [CrossRef]
- Bech-Sàbat, G.; García-Ispierto, I.; Yániz, J.; López-Gatius, F. Therapeutic approaches to pregnancy loss of non-infectious cause during the late embryonic/early foetal period in dairy cattle. A review. Reprod. Domest. Anim. 2010, 45, e469–e475. [Google Scholar] [CrossRef]
- Niswender, G.D.; Juengel, J.L.; Silva, P.J.; Rollyson, M.K.; McIntush, E.W. Mechanisms controlling the function and life span of the corpus luteum. Physiol. Rev. 2000, 80, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Sakumoto, R. Pregnancy-associated changes in uterine-luteal relationships in cows: A mini-review. Reprod. Biol. 2016, 16, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Sangsritavong, S.; Combs, D.K.; Sartori, R.; Armentano, L.-E.; Wiltbank, M.C. High feed intake increases liver blood flow and metabolism of progesterone and estradiol-17beta in dairy cattle. J. Dairy Sci. 2002, 85, 2831–2842. [Google Scholar] [CrossRef]
- Wiltbank, M.; Lopez, H.; Sartori, R.; Sangsritavong, S.; Gümen, A. Changes in reproductive physiology of lactating dairy cows due to elevated steroid metabolism. Theriogenology 2006, 65, 17–29. [Google Scholar] [CrossRef]
- Wolfenson, D.; Flamenbaum, I.; Berman, A. Hyperthermia and body energy store effects on estrous behavior, conception rate, and corpus luteum function in dairy cows. J. Dairy Sci. 1988, 71, 3497–3504. [Google Scholar] [CrossRef]
- Kornmatitsuk, B.; Chantaraprateep, P.; Kornmatitsuk, S.; Kindahl, H. Different types of postpartum luteal activity affected by the exposure of heat stress and subsequent reproductive performance in Holstein lactating cows. Reprod. Domest. Anim. 2008, 43, 515–519. [Google Scholar] [CrossRef]
- Nanas, I.; Chouzouris, T.M.; Dovolou, E.; Dadouli, K.; Stamperna, K.; Kateri, I.; Barbagianni, M.; Amiridis, G.S. Early embryo losses, progesterone and pregnancy associated glycoproteins levels during summer heat stress in dairy cows. J. Thermal Biol. 2021, 98, 102951. [Google Scholar] [CrossRef]
- Spencer, T.E.; Forde, N.; Lonergan, P. The role of progesterone and conceptus-derived factors in uterine biology during early pregnancy in ruminants. J. Dairy Sci. 2016, 99, 5941–5950. [Google Scholar] [CrossRef]
- Bruinjé, T.C.; Colazo, M.G.; Ribeiro, E.S.; Gobikrushanth, M.; Ambrose, D.J. Using in-line milk progesterone data to characterize parameters of luteal activity and their association with fertility in Holstein cows. J. Dairy Sci. 2019, 102, 780–798. [Google Scholar] [CrossRef]
- Bech-Sàbat, G.; López-Gatius, F.; Yániz, J.L.; García-Ispierto, I.; Santolaria, P.; Serrano, B.; Sulon, J.; de Sousa, N.M.; Beckers, J.F. Factors affecting plasma progesterone in the early fetal period in high producing dairy cows. Theriogenology 2008, 69, 426–432. [Google Scholar] [CrossRef]
- Katagiri, S.; Moriyoshi, M. Alteration of the endometrial EGF profile as a potential mechanism connecting the alterations in the ovarian steroid hormone profile to embryonic loss in repeat breeders and high-producing cows. J. Reprod. Dev. 2013, 59, 415–420. [Google Scholar] [CrossRef]
- Nyman, S.; Gustafsson, H.; Berglund, B. Extent and pattern of pregnancy losses and progesterone levels during gestation in Swedish Red and Swedish Holstein dairy cows. Acta Vet. Scand. 2018, 60, 68. [Google Scholar] [CrossRef]
- Herzog, K.; Bollwein, H. Application of Doppler ultrasonography in cattle reproduction. Reprod. Domest. Anim. 2007, 42 (Suppl. 2), 51–58. [Google Scholar] [CrossRef]
- Matsui, M.; Miyamoto, A. Evaluation of ovarian blood flow by colour Doppler ultrasound: Practical use for reproductive management in the cow. Vet. J. 2009, 181, 232–240. [Google Scholar] [CrossRef]
- Lüttgenau, J.; Bollwein, H. Evaluation of bovine luteal blood flow by using color Doppler ultrasonography. Reprod. Biol. 2014, 14, 103–109. [Google Scholar] [CrossRef]
- Kanazawa, T.; Seki, M.; Ishiyama, K.; Kubo, T.; Kaneda, Y.; Sakaguchi, M.; Izaike, Y.; Takahashi, T. Pregnancy prediction on the day of embryo transfer (Day 7) and Day 14 by measuring luteal blood flow in dairy cows. Theriogenology 2016, 86, 1436–1444. [Google Scholar] [CrossRef]
- Pugliesi, G.; de Melo, G.D.; Ataíde, G.A., Jr.; Pellegrino, C.; Silva, J.B.; Rocha, C.C.; Motta, I.G.; Vasconcelos, J.; Binelli, M. Use of Doppler ultrasonography in embryo transfer programs: Feasibility and field results. Anim. Reprod. 2018, 15, 239–246. [Google Scholar] [CrossRef]
- Pugliesi, G.; Dalmaso de Melo, G.; Silva, J.B.; Carvalhêdo, A.S.; Lopes, E.; de Siqueira Filho, E.; Silva, L.A.; Binelli, M. Use of color-Doppler ultrasonography for selection of recipients in timed-embryo transfer programs in beef cattle. Theriogenology 2019, 135, 73–79. [Google Scholar] [CrossRef]
- Beindorff, N.; Nagai, K.; Shirasuna, K.; Herzog, K.; Hoeffmann, K.; Sasaki, M.; Bollwein, M.; Miyamoto, K. Vascular changes in the corpus luteum during early pregnancy in the cow. J. Reprod. Dev. 2010, 56, 263–270. [Google Scholar] [CrossRef]
- Nebel, R.L. On-farm milk progesterone tests. J. Dairy Sci. 1988, 71, 1682–1690. [Google Scholar] [CrossRef]
- Claycomb, R.W.; Delwiche, M.J.; Munro, C.J.; BonDurant, R.H. Rapid enzyme immunoassay for measurement of bovine progesterone. Biosens. Bioelectron. 1998, 13, 1165–1171. [Google Scholar] [CrossRef]
- Samsonova, J.V.; Safronova, V.A.; Osipov, A.P. Rapid flow-through enzyme immunoassay of progesterone in whole cows’ milk. Anal. Biochem. 2018, 545, 43–48. [Google Scholar] [CrossRef]
- Posthuma-Trumpie, G.A.; van Amerongen, A.; Korf, J.; van Berkel, W.J. Perspectives for on-site monitoring of progesterone. Trends Biotechnol. 2009, 27, 652–660. [Google Scholar] [CrossRef]
- Bruinjé, T.C.; Gobikrushanth, M.; Colazo, M.G.; Ambrose, D.J. Dynamics of pre- and post-insemination progesterone profiles and insemination outcomes determined by an in-line milk analysis system in primiparous and multiparous Canadian Holstein cows. Theriogenology 2017, 102, 147–153. [Google Scholar] [CrossRef]
- Bruinjé, T.C.; Ambrose, D.J. Technical note: Validation of an automated in-line milk progesterone analysis system to diagnose pregnancy in dairy cattle. J. Dairy Sci. 2019, 102, 3615–3621. [Google Scholar] [CrossRef]
- Gavelis, A.; Juozaitis, A.; Japertienė, R.; Palubinskas, G.; Juozaitienė, V.; Žilaitis, V. Relationship between in-line milk progesterone before and after artificial insemination and fertility outcomes in dairy cows. Pol. J. Vet. Sci. 2021, 24, 183–190. [Google Scholar] [CrossRef]
- Saint-Dizier, M.; Chastant-Maillard, S. Potential of connected devices to optimize cattle reproduction. Theriogenology 2018, 112, 53–62. [Google Scholar] [CrossRef]
- Allen, W.R. Luteal deficiency and embryo mortality in the mare. Reprod. Domesst. Anim. 2001, 36, 121–131. [Google Scholar] [CrossRef]
- Günzel-Apel, A.; Urhausen, C.; Wolf, K.; Einspanier, A.; Oei, C.; Piechotta, M. Serum progesterone in pregnant bitches supplemented with progestin because of expected or suspected luteal insufficiency. Reprod. Domest. Anim. 2012, 47 (Suppl. 6), 55–60. [Google Scholar] [CrossRef]
- Moon, J.; Choi, J.Y.; Kang, J.T.; Park, S.J.; Kim, S.J.; Jang, G.; Lee, B.C. Relationship between pregnancy rate and serum progesterone concentration in cases of porcine embryo transfer. J. Vet. Sci. 2014, 15, 167–171. [Google Scholar] [CrossRef]
- Brogan, P.T.; Henning, H.; Stout, T.A.; de Ruijter-Villani, M. Relationship between colour flow Doppler sonographic assessment of corpus luteum activity and progesterone concentrations in mares after embryo transfer. Anim. Reprod. Sci. 2016, 166, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, C.; Morais, R.; de Andrade, A.; Balaro, M.; Ribas, J.; Gomes, G.M.; Pinna, A.E. Spectral Doppler ultrasound in selecting an equine embryo receiver. Reprod. Domest. Anim. 2020, 55, 747–752. [Google Scholar] [CrossRef] [PubMed]
- Labarta, E.; Rodríguez, C. Progesterone use in assisted reproductive technology. Best Pract. Res. Clin. Obstet. Gynaecol. 2020, 69, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Su, S.; Zeng, M.; Duan, J. Luteal phase support for natural cycle frozen embryo transfer: A meta-analysis. Gynecol. Endocrinol. 2022, 38, 116–123. [Google Scholar] [CrossRef]
- Humblot, P. From clinics to (cow)mics: A reproductive journey. Anim. Reprod. 2018, 15, 278–291. [Google Scholar] [CrossRef]
- Lucy, M.C. Symposium review: Selection for fertility in the modern dairy cow-Current status and future direction for genetic selection. J. Dairy Sci. 2019, 102, 3706–3721. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).