Simple Summary
Endometritis is a common and important reproductive disease of domestic animals, leading to repeated infertility, abortion, and ovarian dysfunction, which affects the reproductive rate and production performance of female domestic animals, and causes serious financial loss to farmers. Infection with Gram-negative bacteria, the release of LPS and activation of the TLR4/NF-κB signaling pathway are the principal factors responsible for the disease. However, the mechanism of the interaction between endometrial immunity and bacterial infection is not entirely clear. Ubiquitin-like protein ISG15 can regulate the TLR4/NF-κB signaling pathway via the ISGylation modification system, which modulates the inflammatory response. In the present study, we found that ISG15 proteins were mainly located in the cytoplasm of goat endometrial epithelial cells (gEECs) and that the expression of key genes and proteins of ISGylation increased in LPS-induce gEECs. Overexpression and silencing of the ISG15 gene demonstrated that ISGylation inhibited an LPS-induced inflammatory response via the TLR4/NF-κB signaling pathway in gEECs. Here, we provide the experimental basis for further exploration of the role of the ISGylation modification system in the inflammatory response of endometrium and a potential method for the treatment of endometritis.
Abstract
Endometritis is a common and important reproductive disease of domestic animals. The principal factors responsible for the disease are infection with Gram-negative bacteria, the release of Lipopolysaccharides (LPS) and activation of the TLR4/NF-κB signaling pathway. However, we do not fully understand the interaction between endometrial immunity and bacterial infection in the disease etiology. The ubiquitin-like protein ISG15 can regulate the TLR4/NF-κB signaling pathway via the ISGylation modification system, modulating the inflammatory response. In the present study, we found that ISG15 protein was expressed mainly in the cytoplasm of goat endometrial epithelial cells (gEECs) and that the expression of key genes and proteins of ISGylation increased in LPS-induced gEECs. Overexpression and silencing of the ISG15 gene demonstrated that ISGylation inhibited an LPS-induced inflammatory response via the TLR4/NF-κB signaling pathway in gEECs. Here, we provide the experimental basis for further exploration of the role of the ISGylation modification system in the inflammatory response of endometrium and a potential method for the treatment of endometritis.
1. Introduction
Endometritis is a common reproductive disease in domestic animals. It may lead to repeated infertility, abortion, and ovarian dysfunction, affecting the reproductive rate and thus production in domestic animals, which can cause serious financial loss to farmers [1,2]. Pathogenic microorganisms infecting the uterus, either singly or in combination, release virulence factors and cause uterine tissue damage and inflammatory reactions. This is the principal cause of endometritis [3], which results mostly from infections from bacteria, such as Escherichia coli, Trueperella pyogenes, Clostridium, Streptococcus, or Staphylococcus [4,5,6]. Lipopolysaccharides (LPS), the main component of the cell wall of Gram-negative bacteria, is an important virulence factor that causes endometritis, provoking a robust inflammatory response in the uterus of female domestic animals. Although there have been many reports of LPS-induced uterine inflammation [7,8,9], the endometritis mechanism by which LPS-induced in ruminants is still not entirely clear.
The development of endometritis depends on the virulence of the pathogenic microorganisms and their ability to overcome uterine tolerance and resistance to infection. The endometrium is the first line of defense against pathogen invasion and initiates both an innate and adaptive immune response following infection. Type I interferon induces hundreds of interferon-stimulating genes (ISGs) to regulate the stress response [10], which play core roles in regulating the host’s immune response to pathogens. Of the ISGs, ISG15 produces the strongest and most rapid response [11]. ISG15 is a ubiquitin-like protein and binds covalently to cellular or pathogen-associated substrates, modifying them by ISGylation under the action of E1(activating enzyme, UBE1L)-E2(conjugating enzyme, UBE2L6)-E3(binding enzyme, HERC5/6 or TRIM25) reactions [12]. In addition to interferon, LPS, foreign DNA or RNA, retinoic acid, and DNA damaging agents also can induce the expression of ISG15 and the activation of the ISGylation modification system [13], thus playing a regulatory role in various biological processes such as immune regulation [14], anti-viral protection [15], and prevention of nerve injury [16] and cancer [17]. Studies have shown that LPS promotes the release of free ISG15 from monocytes and lymphocytes [18], inducing high expression levels of ISG15 and activation of ISGylation in macrophages [19], suggesting that ISGylation is closely associated with inflammation. The microarray results have shown that ISG15 in mixed bovine epithelial and stromal endometrial cells was significantly upregulated after being exposed to LPS [20]. However, the role of ISGylation in endometritis remains to be explored.
The TLR4/NF-κB signaling pathway operates in many types of eukaryotic cells and can be activated by LPS, bacterial glycoproteins, viral molecules, and inflammatory factors, leading to the regulation of cellular activity in the LPS-induced inflammatory response [21]. The TLR4/NF-κB signaling pathway is the principal pathway activated in the LPS-induced inflammatory response and forms an important element of the endometrial innate immune system [3]. Inhibition of TLR4/NF-κB signaling to reduce LPS-induced endometritis has recently been explored in the study of disease pathogenesis and the development of therapeutic drugs [22,23]. It also has been reported that ISG15 inhibits the NF-κB signaling pathway by downregulation of IKKβ and p65 expression, in addition to phosphorylation of p65 and IκBα [24], suggesting that the ISGylation system may play a regulatory role through this signaling pathway. However, to date, its role in goat endometritis has not been explored. Therefore, in the present study, goat endometrial epithelial cells (gEECs) were initially activated by the LPS to establish a goat endometritis cell model to explore the localization and expression of key components of the ISGylation modification system. We then silenced and overexpressed ISG15 in the cells to explore the role of the ISGylation modification system in LPS-induced endometritis by regulation of the TLR4/NF-κB signaling pathway. The purpose of the present study was to lay a foundation and provide data to support the investigation of ISGylation and similar ubiquitin-like modification systems in the pathogenesis of endometritis.
2. Materials and Methods
2.1. Ethics Statement and Consent to Participate
The present study experiments were conducted under the strict guidelines of the Committee for the Ethics on Animal Care and Experiments in Northwest A&F University.
2.2. Cell Culture and LPS Treatment
The gEECs were established by transfection with human telomerase reverse transcriptase (hTERT) and were well preserved in our laboratory [25]. gEECs were seeded in six-well plates and cultured with DMEM/F12 medium (HyClone, South Logan, UT, USA) containing 10% fetal bovine serum (FBS) (Corning, Manassas, VA, USA) at 37 °C in 5% CO2. After reaching 70%–80% confluence, the cells were treated with 5 μg/mL LPS from Escherichia coli 0111: B4 (3050; Sigma-Aldrich, Co., St. Louis, MO, USA) for 0, 3, 6 and 12 h. Three independent experiments were performed unless stated otherwise. At the end of the culture, the cells were collected for mRNA and protein experiments. The concentration of LPS was determined by previous studies in our laboratory and has been proved to cause an obvious inflammatory response of gEECs [26].
2.3. Overexpression Plasmid Transfection
Overexpression plasmids of ISG15 were constructed using pcDNA3.1(+) vectors, such as pcDNA3.1-ISG15. Empty plasmids were used as negative controls. The sequences of the primers used for the amplification of ISG15 complementary DNA (cDNA) fragments were as follows: forward primer 5′-cgggatcctgacaccagaacccacggcc-3′ and reverse primer 5′-ccctcgagtaaggccctcctggcccttccc-3′.
The gEECs were cultured at densities of 1 × 105 cells per mL in Dulbecco’s Modified Eagle Medium (DMEM)/F12 supplemented with 10% FBS in 6-well culture plates. After reaching 70–80% confluence, the gEECs were transfected with the appropriate overexpression plasmids using the TurboFect transfection reagent (Thermo Fisher Scientific, Waltham, MA, USA), in accordance with the manufacturer’s protocol. After transfection for 12 h, the culture media was exchanged for fresh medium, and incubation was continued for a further 12 h. The transfected cells were then treated with 5 μg/mL LPS for 12 h prior to analysis in the following experiments. Three independent experiments were performed unless stated otherwise.
2.4. ISG15 siRNA Interference Fragment Design and Transfection
ISG15 siRNA interference fragments were constructed by Shanghai Ji Ma Pharmacy Technology Co., Ltd. (Ji Ma, Shanghai, China). A si-NC sequence fragment, without any specific target, was also synthesized as a negative control. The ISG15 siRNA sequence is showed in Table 1. The detailed method of transfection is described in Section 2.3, except that the gEECs were transfected with the appropriate ISG15 siRNA fragment plasmids using the TurboFect transfection reagent.

Table 1.
The information of the siRNA sequence.
2.5. qRT-PCR Analysis
The total RNA was extracted from uterus samples using TRIzol reagent (Invitrogen, Inc., Carlsbad, CA, USA). After reverse transcription into cDNA by the 5X All-In-One RT MasterMix with AccuRT Genomic DNA Remove Kit (Applied Biological Materials Inc., Vancouver, BC, Canada), qRT-PCR was performed using an EvaGreen qPCR Mastermix Kit (AceQ®Universal SYBR®qPCR Master Mix. Vazyme Biotech Co., Ltd, Nanjing Jiangsu, China) according to the manufacturer’s instructions in the CFX96™ Real-Time PCR Detection System (Bio-Rad Laboratories, Inc., Hercules, CA, USA). The mRNA expression levels were normalized to the expression of GAPDH and quantified using the 2−ΔΔCt method. All reactions were conducted in biological triplicate. The information of primers is listed in Table 2.

Table 2.
Primer sequences for qRT-PCR.
2.6. Western Blot Analysis
The gEECs were lysed using a Total Protein Extraction Kit, and then the total protein was measured by the bicinchoninic acid (BCA) assay (Nanjing Keygen Biotech Co., Ltd., Nanjing, China). For each sample, 20 μg of total protein were separated using 15% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) followed by electro transfer to PVDF membrane (Millipore, Billerica, MA, USA). After blocking with 8% non-fat milk in TBST for 2 h, the membranes were incubated overnight at 4 °C with primary antibodies against ISG15 (CST, #15981-1AP; 1:1000 dilution), UBE1L (Proteinch, #YT4797; 1:1000 dilution), NF-κB p65 (GST, #8242; 1:1000 dilution), NF-κB p65(S536) (GST, #3033; 1:1000 dilution) or β-actin (1:2000; Beijing CWBIO Co., Ltd., Beijing, China). After the membranes were incubated with the secondary antibodies conjugated to HRP (1:5000 dilution; Zhong Shan Golden Bridge Biotechnology, Nanjing, China) for 1 h at room temperature, protein bands were detected using the SuperSignalWest Pico kit (Thermo, Rockford, IL, USA) in the Gel imaging system (Tanon-4100, Tanon Science & Technology Co., Ltd., Shanghai, China). The densitometric analyses were processed using ImageJ software (Bio-Rad).
2.7. Immunofluorescence
After treatment, the cells were fixed in 4% (wt/vol) paraformaldehyde for 30 min at room temperature, after which they were permeabilized using 0.1% Triton X-100 in phosphate-buffered salina (PBS) for 10 min. Cells were then blocked in 0.1% bovine serum albumin (BSA) in PBS for 1 h and then incubated overnight with primary antibodies at 4 °C, followed by three PBS washes for 5 min each time. The cells were incubated for 2 h with a red fluorescent-conjugated donkey anti-rabbit secondary antibody (1:200 dilution) at room temperature, followed by three PBS washes for 5 min each time. Coverslips were mounted over the cells on glass slides using ProLong Gold Antifade reagent (Thermo Fisher Scientific), with or without DAPI for visualization of cell nuclei. Images were acquired using a confocal microscope and post-processed in Adobe Photoshop for specific inset enlargement and RGB channel separation.
2.8. Statistical Analysis
All experiments were replicated at least three times for each group. Data were expressed as means ± SEM. The data were analyzed with one-way ANOVA followed by Tukey’s post hoc test and the Independent-Samples T-test using the GraphPad Prism 6 Software. Differences were considered significant when p was < 0.05.
3. Results
3.1. Expression of ISGylation on LPS-Induced Inflammatory Response in gEECs
To analyze the potential function of ISGylation in LPS-mediated gEECs inflammatory response, the expression levels of ISG15 and the key enzymes were examined (Figure 1). ISG15 protein was mainly localized in the cytoplasm of gEECs, and the expression levels of ISG15 protein were significantly upregulated with increasing time of 5 μg/mL LPS treatment (Figure 1A). The free ISG15 protein levels were significantly increased after treatment with 5 μg/mL LPS for 3 h, although no significant difference was observed from 3 h to 12 h (Figure 1B,C). In contrast, the levels of conjugated ISG15 protein significantly increased with time after treatment with 5 μg/mL LPS (Figure 1B,C, p < 0.05; Supplementary Materials Figure S1). Meanwhile, the levels of UBE1L protein were significantly upregulated with increasing time of LPS treatment (Figure 1D,E, p < 0.05). The qRT-PCR results further revealed that the ISG15 and UBE1L mRNA levels were significantly upregulated with increasing time of LPS treatment (Figure 1F,G, p < 0.05). The expression levels of UBE2L6 mRNA were significantly upregulated after treatment with 5 μg/mL LPS for 3 h (Figure 1H, p < 0.05). The mRNA levels of HERC5 were significantly elevated after treatment with 5 μg/mL LPS, and the peaking levels were observed at 6 h (Figure 1I, p < 0.05). Significant differences in USP18 mRNA levels were observed after treatment with 5 μg/mL LPS for 6 h (Figure 1J, p < 0.05).
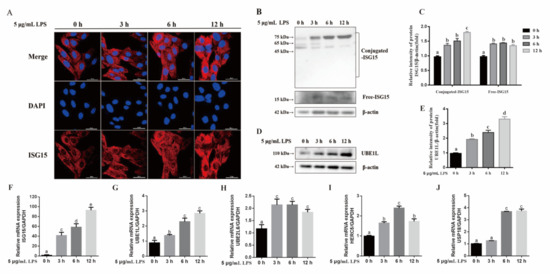
Figure 1.
The expression of ISGylation on LPS-induced inflammatory response in gEECs. (A) The immunofluorescence of ISG15 after gEECs treated with 5 μg/mL LPS for 0, 3, 6 or 12 h. (B) Western blot analysis for conjugated and free ISG15 after gEECs treated with 5 μg/mL LPS for 0, 3, 6 or 12 h. (C) The quantification of ISG15 band intensities from three independent results was determined by densitometric analysis. (D) Western blot analysis for UBEL1 protein after gEECs treated with 5 μg/mL LPS for 0, 3, 6 or 12 h. (E) The quantification of UBEL1 band intensities from three independent results was determined by densitometric analysis. (F–J) The mRNA levels of ISG15, UBE1L, UBE2L6, HERC5, and USP18 after gEECs treated with 5 μg/mL LPS for 0, 3, 6 or 12 h, respectively. The data are presented as the mean ± SEM from three independent experiments, and bars with different letters are significantly different (p < 0.05).
3.2. Effect of ISG15 on LPS-Induced Inflammatory Response in gEECs
To further reveal the role of ISGylation in LPS-induced inflammatory response, the gEECs were transfected with the siRNA or the overexpression vector pcDNA-ISG15 (Figure 2), and then the expression levels of IL-8, IL-6, and IL-1β were evaluated by qRT-PCR (Figure 3). As expected, both free and conjugated ISG15 protein expressions were significantly suppressed after transducing the si-ISG15, respectively (Figure 2A–C, p < 0.05; Supplementary Materials Figure S2). Meanwhile, transfection of the overexpression vector pcDNA-ISG15 in gEECs significantly upregulated the free and conjugated ISG15 protein expression, respectively (Figure 2D–F, p < 0.05; Supplementary Materials Figure S3). We found that overexpression ISG15 significantly inhibited IL-8, IL-6, and IL-1β expression in LPS-treated gEECs (Figure 3A–C, p < 0.05). Conversely, silencing of the ISG15 gene significantly upregulated IL-8, IL-6, and IL-1β expression in LPS-treated gEECs (Figure 3D–F, p < 0.05).
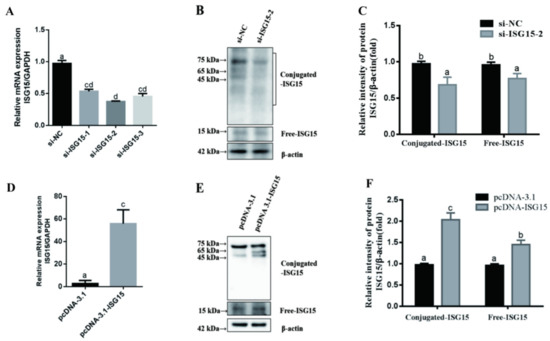
Figure 2.
Efficiency verification of siRNA and overexpression ISG15 in gEECs. The gEECs were transduced with si-NC, si-ISG15, pcDNA-3.1, and pcDNA-ISG15 for 24 h, and then treated with 5 μg/mL LPS for 12 h, respectively. The efficiency of ISG15 silencing and overexpression were determined using qRT-PCR (A,D) and Western blot (B,C,E,F), respectively. The data are presented as the mean ± SEM from three independent experiments, and bars with different letters are significantly different (p < 0.05).
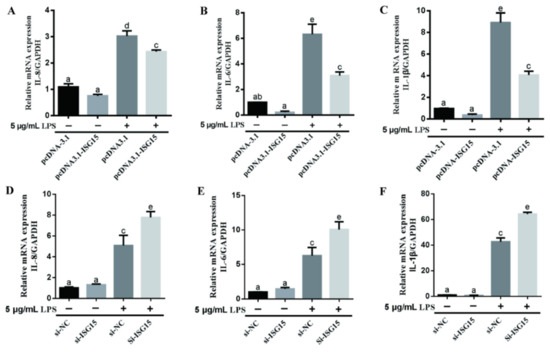
Figure 3.
The effect of ISG15 on LPS-induced changes of inflammatory factors in gEECs. (A–C) qRT-PCR analysis of the mRNA levels of IL-8, IL-6, and IL-1β in 5 μg/mL LPS-treated gEECs for 12 h after transducing the overexpression vector pcDNA-ISG15, respectively. (D–F) qRT-PCR analysis of the mRNA levels of IL-8, IL-6, and IL-1β in 5 μg/mL LPS-treated gEECs for 12 h after transducing the si-ISG15, respectively. The data are presented as the mean ± SEM from three independent experiments, and bars with different letters are significantly different (p < 0.05).
3.3. Effects of ISG15 on LPS-Induced TLR4/NF-κB Pathway in gEECs
To detect the anti-inflammatory mechanism of ISGylation, the expression of phospho-p65, TLR4 and NF-κB were measured. As shown in Figure 4A,B, the phosphorylation levels of p65 were significantly elevated after 5 μg/mL LPS treatment, with a peak at 6 h (p < 0.05). However, overexpression of ISG15 significantly suppressed the phosphorylation levels of p65 induced by LPS (Figure 4C,D, p < 0.05). Conversely, the phosphorylation levels of p65 induced by LPS were significantly upregulated after silencing of ISG15 in gEECs (Figure 4E,F, p < 0.05). Meanwhile, the immunofluorescence result demonstrated that the level of p65 in the nucleus induced by LPS was significantly downregulated and upregulated after knockdown or overexpression of the ISG15 gene, respectively (Figure 4G). The expression levels of TLR4 and NF-κB-p65 mRNAs induced by LPS were significantly repressed after ISG15 overexpression (Figure 5A,C, p < 0.05), and knockdown of ISG15 significantly promoted the mRNA levels of TLR4 and NF-κB-p65 (Figure 5B,D, p < 0.05).
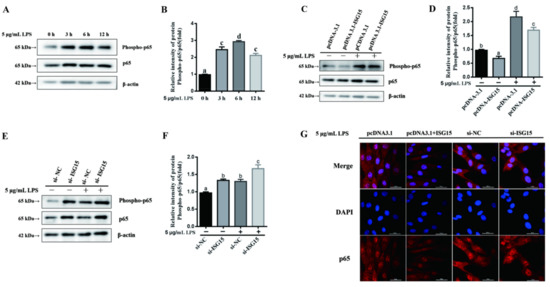
Figure 4.
The effects of ISG15 on LPS-induced phospho-p65 in gEECs. (A,B) Western blot analysis of the phosphorylation levels of p65 after 5 μg/mL LPS-treated gEECs for 0, 3, 6 and 12 h, respectively. (C,D) Western blot analysis of the phosphorylation levels of p65 in 5 μg/mL LPS-treated gEECs for 12 h after transducing the overexpression vector pcDNA-ISG15. (E,F) Western blot analysis of the phosphorylation levels of p65 in 5 μg/mL LPS-treated gEECs for 12 h after transducing the si-ISG15. (G) The immunofluorescence of p65 in 5 μg/mL LPS-treated gEECs for 12 h after transducing the overexpression vector pcDNA-ISG15 or the si-ISG15, respectively. The data are presented as the mean ± SEM from three independent experiments, and bars with different letters are significantly different (p < 0.05).
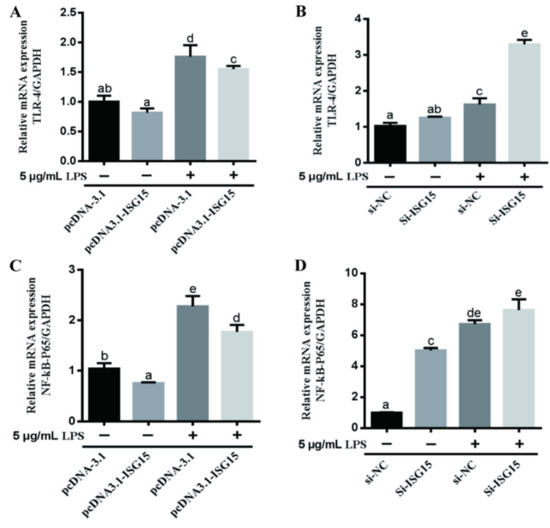
Figure 5.
The effects of ISG15 on LPS-induced TLR4 and NF-κB-p65 in gEECs. qRT-PCR analysis of the mRNA levels of TLR4 (A,C) and NF-κB-p65 (B,D) with or without 5 μg/mL LPS-treated gEECs for 12 h after overexpression or silencing of ISG15, respectively. The data are presented as the mean ± SEM from three independent experiments, and bars with different letters are significantly different (p < 0.05).
4. Discussion
ISG15 represents the first ubiquitin-like modifier gene to be identified [27] and is widely found in mammalian immune and non-immune cells [27,28], constituting a modification system termed ISGylation, that uses a three-step enzymatic reaction similar to that of ubiquitination [29], while the deubiquitination enzyme USP18 removes ISG15 from target protein, thus reversing ISGylation [30]. ISG15 regulates cytokine secretion and immune cell activation through ubiquitination or in its free form [31]. In domestic animals, ISG15 has been shown to be expressed in epithelial and stromal cells of the endometrium in cattle, horses, and sheep [32,33,34] and is located in the nucleus, nuclear stroma, cytoplasm, and organelles of bovine subcellular structures [32]. In the present study, LPS was used to induce an inflammatory response in gEECs to successfully construct an in vitro model of goat endometritis, as has been previously reported in earlier studies [26]. Here, we found that ISG15 was mostly localized in the cytoplasm, with low levels of expression in the nucleus, essentially consistent with previous studies. The ISG15 expression was significantly increased in a non-type І interferon-dependent manner after LPS induction. As the time after LPS treatment increased, there was an upward trend in the level of conjugated ISG15, while the levels of free ISG15 did not change significantly, suggesting that ISG15 may preferentially react via ISGylation. In certain cells, ISG15 and ISGylation related enzymes are mainly expressed in the nucleus [35]; therefore, to further explore ISGylation activation, we investigated the mRNA levels of ISG15, UBE1L, UBE2L6, HERC5 and USP18, observing that they were significantly upregulated after 6 h of LPS treatment, with changes in the UBE1L protein levels consistent with the mRNA expression. These results are consistent with those of Piotr Przanowski [36], suggesting that ISGylation plays a regulatory role in the process of LPS-induced goat endometritis.
Although ISG15 and ISGylation play important roles in both immunity and inflammation [37], the majority of studies have focused on the induction of type І interferon, with few reports exploring the LPS-induced inflammatory response. ISG15 was found to be upregulated in the endometrium after perfusion of LPS into bovine mammary glands [38], while endometrial and stromal cells infected with bovine viral diarrhea virus (BVDV) reduced the response of ISG15 to LPS [39], suggesting the involvement of ISG15 in the regulation of inflammation and the immune response in endometritis; ISGylation increases the stability of numerous proteins including signal transducer and activator of transcription 1 (STAT1), preventing the premature termination of the immune response in LPS-stimulated microglia, and playing a protective role in inflammation [36]. In the present study, the overexpression of ISG15 significantly reduced the mRNA expression levels of IL-1β, IL-6 and IL-8 in gEECs following LPS treatment, while the silencing of ISG15 had the opposite effect, indicating that ISG15 plays a protective role in goat endometritis. These results are contrary to Jun-Bao’s findings that type I interferon induces the expression of cytokines involved in ISGylation and intensifies colon inflammation in mice [40]; the discrepancy may be related to factors, such as cell type, inflammation type, induction method, and time.
Innate immunity is closely associated with the mechanisms of recovery after delivery in ruminants [41], and the TLR4/NF-κB signaling pathway is known to activate in E. coli-induced endometritis. Studies have reported the use of hormones [23,42], natural product extracts [22,43], functional proteins [44,45], trace elements [46] and microRNA [47,48] that regulate the TLR4/NF-κB signaling pathway to alleviate endometrial inflammation. ISG15 induces cancer cell death through inhibition of NF-κB signaling [24] and is positively correlated with IκBα or phosphorylated IκBα in ovarian high-grade serous carcinoma. In the present study, the addition of LPS to gEECs upregulated the mRNA expression levels of TLP4 and NF-κB and significantly increased the phosphorylation of p65, indicating activation of the TLR4/NF-κB signaling pathway. Overexpression and interference with ISG15 significantly downregulated and upregulated the mRNA expression levels of TLP4 and NF-κB, respectively. Furthermore, overexpression of ISG15 decreased p65 phosphorylation and nucleation, while interference with ISG15 expression had the opposite effect, suggesting that ISG15 may play a role in alleviating inflammation by inhibition of the TLR4/NF-κB signaling pathway in LPS-induced endometritis. A number of studies have reported that IFN-τ alleviates endometritis by inhibiting NF-κB [44,49,50], possibly by inducing the overexpression of multiple ISGs, including ISG15.
In ruminants, IFN-τ is an important maternal gestation-recognition signaling factor secreted by embryonic trophoblast cells [51], that is highly expressed during embryo implantation and stimulates significant upregulation of ISG15 [52]. The establishment of pregnancy requires transient regulation of innate and adaptive maternal immunity [53]. The results of the present study demonstrated that ISG15 inhibited the TLR4/NF-κB signaling pathway, and such temporary immune tolerance may lead to weakened identification of pathogenic microorganisms in the body during this period, thus increasing the risk of infection. However, type I interferon mainly mediates the upregulation of ISG through the JAK/STAT signaling pathway [54], and so the interaction between the multiple signaling pathways still requires additional exploration.
5. Conclusions
We found that ISG15 protein expression was mainly located in the cytoplasm of gEECs, and ISGylation was increased in a time-dependent manner after LPS induction. ISGylation inhibited LPS-induced inflammatory responses via the TLR4/NF-κB signaling pathway in gEECs. The results provide an experimental basis for further exploring the role of the ISGylation modification system in the inflammatory response of the endometrium.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ani11092593/s1, Figure S1: Full blots of WB analysis of the conjugated ISG15 after gEECs treated with 5 μg/mL LPS for 0, 3, 6 or 12 h were shown, Figure S2: Full blots of WB analysis of the conjugated ISG15 in LPS-treated gEECs after transducing the si-NC and si-ISG15 were shown. Figure S3: Full blots of WB analysis of the conjugated ISG15 in LPS-treated gEECs after transducing the pcDNA-3.1 and pcDNA-ISG15 were shown.
Author Contributions
Conceptualization, Y.J. and P.L.; Data curation, J.X. and S.L.; Investigation, Z.W. and R.Z.; Methodology, Y.J. and P.L.; Software, X.Z.; Supervision, Y.J. and P.L.; Writing—original draft, J.X. and S.L.; Writing—review and editing, J.X., S.L., Z.W., R.Z., X.Z., A.W., Y.J. and P.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China (Grant No. 32172934; 31772817).
Institutional Review Board Statement
The study did not involve humans or animals.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Beena, V.; Pawaiya, R.; Gururaj, K.; Singh, D.D.; Mishra, A.K.; Gangwar, N.K.; Gupta, V.K.; Singh, R.; Sharma, A.K.; Karikalan, M. Molecular etiopathology of naturally occurring reproductive diseases in female goats. Vet. World 2017, 10, 964–972. [Google Scholar] [CrossRef][Green Version]
- Gilbert, R.O. The effects of endometritis on the establishment of pregnancy in cattle. Reprod. Fertil. Dev. 2011, 24, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Sheldon, I.M.; Cronin, J.G.; Bromfield, J.J. Tolerance and innate immunity shape the development of postpartum uterine disease and the impact of endometritis in dairy cattle. Annu. Rev. Anim. Biosci. 2019, 7, 361–384. [Google Scholar] [CrossRef] [PubMed]
- Wagener, K.; Gabler, C.; Drillich, M. A review of the ongoing discussion about definition, diagnosis and pathomechanism of subclinical endometritis in dairy cows. Theriogenology 2017, 94, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Sheldon, I.M.; Noakes, D.E.; Rycroft, A.N.; Pfeiffer, D.U.; Dobson, H. Influence of uterine bacterial contamination after parturition on ovarian dominant follicle selection and follicle growth and function in cattle. Reproduction 2002, 123, 837–845. [Google Scholar] [CrossRef]
- Huszenicza, G.; Fodor, M.; Gacs, M.; Kulcsar, M.; Dohmen, M.; Vamos, M.; Porkolab, L.; Kegl, T.; Bartyik, J.; Lohuis, J. Uterine bacteriology, resumption of cyclic ovarian activity and fertility in postpartum cows kept in large-scale dairy herds. Reprod. Domest. Anim. 2010, 34, 3–4. [Google Scholar] [CrossRef]
- Yang, C.; Yang, C.; Zhang, J.; Guo, Y.; Chen, N.; Yin, B.; Zhou, Q.; Zhang, T.; Guo, S.; Deng, G. Microrna-211 regulates the expression of tab1 and inhibits the nf-kappab signaling pathway in lipopolysaccharide-induced endometritis. Int. Immunopharmacol. 2021, 96, 107668. [Google Scholar] [CrossRef]
- Deng, Y.; Liu, B.; Fu, C.; Gao, L.; Shen, Y.; Liu, K.; Li, Q.; Cao, J.; Mao, W. Lipopolysaccharide stimulates bovine endometrium explants through tolllike receptor 4 signaling and pge2 synthesis. Prostaglandins Leukot. Essent. Fatty Acids 2021, 168, 102272. [Google Scholar] [CrossRef]
- Yan, C.; Lv, H.; Peng, Z.; Yang, D.; Shen, P.; Yu, J.; Tong, C.; Wang, X. Analysis of mirna expression changes in bovine endometrial stromal cells treated with lipopolysaccharide. Theriogenology 2021, 167, 85–93. [Google Scholar] [CrossRef]
- Jeon, Y.J.; Yoo, H.M.; Chung, C.H. Isg15 and immune diseases. Biochim. Biophys. Acta 2010, 1802, 485–496. [Google Scholar] [CrossRef]
- Skaug, B.; Chen, Z.J. Emerging role of isg15 in antiviral immunity. Cell 2010, 143, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.B.; Arimoto, K.; Motamedchaboki, K.; Yan, M.; Wolf, D.A.; Zhang, D.E. Identification and characterization of a novel isg15-ubiquitin mixed chain and its role in regulating protein homeostasis. Sci. Rep. 2015, 5, 12704. [Google Scholar] [CrossRef] [PubMed]
- Sung, P.S.; Cheon, H.; Cho, C.H.; Hong, S.H.; Park, D.Y.; Seo, H.I.; Park, S.H.; Yoon, S.K.; Stark, G.R.; Shin, E.C. Roles of unphosphorylated isgf3 in hcv infection and interferon responsiveness. Proc. Natl. Acad. Sci. USA 2015, 112, 10443–10448. [Google Scholar] [CrossRef] [PubMed]
- Kimmey, J.M.; Campbell, J.A.; Weiss, L.A.; Monte, K.J.; Lenschow, D.J.; Stallings, C.L. The impact of isgylation during mycobacterium tuberculosis infection in mice. Microbes Infect. 2017, 19, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Villarroya-Beltri, C.; Guerra, S.; Sanchez-Madrid, F. Isgylation—A key to lock the cell gates for preventing the spread of threats. J. Cell Sci. 2017, 130, 2961–2969. [Google Scholar] [CrossRef]
- Nakka, V.P.; Mohammed, A.Q. A critical role for isgylation, ubiquitination and, sumoylation in brain damage, implications for neuroprotection. Neurochem. Res. 2020, 45, 1975–1985. [Google Scholar] [CrossRef]
- Alcala, S.; Sancho, P.; Martinelli, P.; Navarro, D.; Pedrero, C.; Martin-Hijano, L.; Valle, S.; Earl, J.; Rodriguez-Serrano, M.; Ruiz-Canas, L. Isg15 and isgylation is required for pancreatic cancer stem cell mitophagy and metabolic plasticity. Nat. Commun. 2020, 11, 2682. [Google Scholar] [CrossRef]
- Malakhova, O.; Malakhov, M.; Hetherington, C.; Zhang, D.E. Lipopolysaccharide activates the expression of isg15-specific protease ubp43 via interferon regulatory factor 3. J. Biol. Chem. 2002, 277, 14703–14711. [Google Scholar] [CrossRef]
- Li, C.; Wang, Y.; Zheng, H.; Dong, W.; Lv, H.; Lin, J.; Guo, K.; Zhang, Y. Antiviral activity of isg15 against classical swine fever virus replication in porcine alveolar macrophages via inhibition of autophagy by isgylating becn1. Vet. Res. 2020, 51, 22. [Google Scholar] [CrossRef]
- Oguejiofor, C.F.; Cheng, Z.; Abudureyimu, A.; Fouladi-Nashta, A.A.; Wathes, D.C. Global transcriptomic profiling of bovine endometrial immune response in vitro. I. Effect of lipopolysaccharide on innate immunity. Biol. Reprod. 2015, 93, 100. [Google Scholar]
- Tilborghs, S.; Corthouts, J.; Verhoeven, Y.; Arias, D.; Rolfo, C.; Trinh, X.B.; Van Dam, P.A. The role of nuclear factor-kappa b signaling in human cervical cancer. Crit. Rev. Oncol. Hematol. 2017, 120, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Yi, Y.; Hong, L. Oridonin ameliorates lipopolysaccharide-induced endometritis in mice via inhibition of the tlr-4/nf-kappabpathway. Inflammation 2019, 42, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Liu, B.; Mao, W.; Gao, R.; Feng, S.; Qian, Y.; Wu, J.; Zhang, S.; Gao, L.; Fu, C. Pge2 downregulates lps-induced inflammatory responses via the tlr4-nf-kappab signaling pathway in bovine endometrial epithelial cells. Prostaglandins Leukot. Essent. Fatty Acids 2018, 129, 25–31. [Google Scholar] [CrossRef]
- Mao, H.; Wang, M.; Cao, B.; Zhou, H.; Zhang, Z.; Mao, X. Interferon-stimulated gene 15 induces cancer cell death by suppressing the nf-kappab signaling pathway. Oncotarget 2016, 7, 70143–70151. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.Y.; Wang, A.H.; Wu, Q.X.; Sheng, H.X.; Jin, Y.P. Establishment and characteristics of immortal goat endometrial epithelial cells and stromal cells with htert. J. Anim. Vet. Adv. 2010, 9, 2738–2747. [Google Scholar] [CrossRef]
- Xiao, J.; Liu, S.; Yu, T.; Zhang, R.; Guo, X.; Jia, Y.; Shang, C.; Wang, A.; Jin, Y.; Lin, P. Ufmylation is associated with lps-induced inflammatory response in goat endometrial epithelial cells. Reprod. Domest. Anim. 2020, 55, 1725–1734. [Google Scholar] [CrossRef] [PubMed]
- Haas, A.L.; Ahrens, P.; Bright, P.M.; Ankel, H. Interferon induces a 15-kilodalton protein exhibiting marked homology to ubiquitin. J. Biol. Chem. 1987, 262, 11315–11323. [Google Scholar] [CrossRef]
- Loeb, K.R.; Haas, A.L. Conjugates of ubiquitin cross-reactive protein distribute in a cytoskeletal pattern. Mol. Cell Biol. 1994, 14, 8408–8419. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Zhang, D.E. Interferon-stimulated gene 15 and the protein isgylation system. J. Interferon. Cytokine Res. 2011, 31, 119–130. [Google Scholar] [CrossRef]
- Malakhov, M.P.; Malakhova, O.A.; Kim, K.I.; Ritchie, K.J.; Zhang, D.E. Ubp43 (usp18) specifically removes isg15 from conjugated proteins. J. Biol. Chem. 2002, 277, 9976–9981. [Google Scholar] [CrossRef]
- Dos, S.P.; Mansur, D.S. Beyond isglylation, functions of free intracellular and extracellular isg15. J. Interferon Cytokine Res. 2017, 37, 246–253. [Google Scholar]
- Austin, K.J.; Carr, A.L.; Pru, J.K.; Hearne, C.E.; George, E.L.; Lee, B.E.; Hansen, T.R. Localization of isg15 and conjugated proteins in bovine endometrium using immunohistochemistry and electron microscopy. Endocrinology 2004, 145, 967–975. [Google Scholar] [CrossRef]
- Klein, C.; Scoggin, K.E.; Troedsson, M.H. The expression of interferon-stimulated gene 15 in equine endometrium. Reprod. Domest. Anim. 2011, 46, 692–698. [Google Scholar] [CrossRef]
- Alak, I.; Hitit, M.; Kose, M.; Kaya, M.S.; Ucar, E.H.; Atli, Z.; Atli, M.O. Relative abundance and localization of interferon-stimulated gene 15 mrna transcript in intra- and extra-uterine tissues during the early stages of pregnancy in sheep. Anim. Reprod. Sci. 2020, 216, 106347. [Google Scholar] [CrossRef]
- Tecalco, C.A.; Mejia-Barreto, K. Cell type-dependent regulation of free isg15 levels and isgylation. J. Cell Commun. Signal. 2017, 11, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Przanowski, P.; Loska, S.; Cysewski, D.; Dabrowski, M.; Kaminska, B. Isg’ylation increases stability of numerous proteins including stat1, which prevents premature termination of immune response in lps-stimulated microglia. Neurochem. Int. 2018, 112, 227–233. [Google Scholar] [CrossRef]
- Hermann, M.; Bogunovic, D. Isg15, in sickness and in health. Trends Immunol. 2017, 38, 79–93. [Google Scholar] [CrossRef] [PubMed]
- Campos, C.C.; Hartling, I.; Kaur, M.; Fernandes, A.; Santos, R.M.; Cerri, R. Intramammary infusion of lipopolysaccharide promotes inflammation and alters endometrial gene expression in lactating holstein cows. J. Dairy Sci. 2018, 101, 10440–10455. [Google Scholar] [CrossRef]
- Oguejiofor, C.F.; Cheng, Z.; Abudureyimu, A.; Anstaett, O.L.; Brownlie, J.; Fouladi-Nashta, A.A.; Wathes, D.C. Global transcriptomic profiling of bovine endometrial immune response in vitro. Ii. Effect of bovine viral diarrhea virus on the endometrial response to lipopolysaccharide. Biol. Reprod. 2015, 93, 101. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.B.; Miyauchi-Ishida, S.; Arimoto, K.; Liu, D.; Yan, M.; Liu, C.W.; Gyorffy, B.; Zhang, D.E. Type i ifn induces protein isgylation to enhance cytokine expression and augments colonic inflammation. Proc. Natl. Acad. Sci. USA 2015, 112, 14313–14318. [Google Scholar] [CrossRef]
- Horst, E.A.; Kvidera, S.K.; Baumgard, L.H. Invited review, the influence of immune activation on transition cow health and performance-a critical evaluation of traditional dogmas. J. Dairy Sci. 2021, 104, 8380–8410. [Google Scholar] [CrossRef]
- Dong, J.; Qu, Y.; Li, J.; Cui, L.; Wang, Y.; Lin, J.; Wang, H. Cortisol inhibits nf-kappab and mapk pathways in lps activated bovine endometrial epithelial cells. Int. Immunopharmacol. 2018, 56, 71–77. [Google Scholar] [CrossRef]
- Miao, Y.; Ishfaq, M.; Liu, Y.; Wu, Z.; Wang, J.; Li, R.; Qian, F.; Ding, L.; Li, J. Baicalin attenuates endometritis in a rabbit model induced by infection with escherichia coli and staphylococcus aureus via nf-kappab and jnk signaling pathways. Domest. Anim. Endocrinol. 2021, 74, 106508. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Guo, Y.; Liu, Y.; Li, C.; Guo, M.; Deng, G. Ifn-tau displays anti-inflammatory effects on staphylococcus aureus endometritis via inhibiting the activation of the nf-kappab and mapk pathways in mice. Biomed. Res. Int. 2017, 2017, 2350482. [Google Scholar] [PubMed]
- Li, W.; Fu, K.; Lv, X.; Wang, Y.; Wang, J.; Li, H.; Tian, W.; Cao, R. Lactoferrin suppresses lipopolysaccharide-induced endometritis in mice via down-regulation of the nf-kappab pathway. Int. Immunopharmacol. 2015, 28, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Gao, X.; Cao, Y.; Jiang, H.; Wang, T.; Song, X.; Guo, M.; Zhang, N. Selenium deficiency facilitates inflammation through the regulation of tlr4 and tlr4-related signaling pathways in the mice uterus. Inflammation 2015, 38, 1347–1356. [Google Scholar] [CrossRef]
- Zhao, G.; Zhang, T.; Wu, H.; Jiang, K.; Qiu, C.; Deng, G. Microrna let-7c improves lps-induced outcomes of endometritis by suppressing nf-kappab signaling. Inflammation 2019, 42, 650–657. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Guo, S.; Zhang, T.; Ma. X.; Wu, Z.; Jiang, K.; Zhang, X.; Guo, X.; Deng, G. Mir-505 as an anti-inflammatory regulator suppresses hmgb1/nf-kappab pathway in lipopolysaccharide-mediated endometritis by targeting hmgb1. Int. Immunopharmacol. 2020, 88, 106912. [Google Scholar] [CrossRef] [PubMed]
- Jiang, K.; Chen, X.; Zhao, G.; Wu, H.; Mi, J.; Qiu, C.; Peng, X.; Deng, G. Ifn-tau plays an anti-inflammatory role in staphylococcus aureus-induced endometritis in mice through the suppression of nf-kappab pathway and mmp9 expression. J. Interferon Cytokine Res. 2017, 37, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Wu, Z.; Guo, S.; Zhang, T.; Ma, X.; Jiang, K.; Guo, X.; Deng, G. Ifn-tau attenuates lps-induced endometritis by restraining hmgb1/nf-kappab activation in beecs. Inflammation 2021, 44, 1478–1489. [Google Scholar] [CrossRef]
- Talukder, A.K.; Rashid, M.B.; Takedomi, T.; Moriyasu, S.; Imakawa, K.; Miyamoto, A. Day-7 embryos generate an anti-inflammatory immune response in peripheral blood immune cells in superovulated cows. Am. J. Reprod. Immunol. 2019, 81, e13069. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, A.A.; Hooda, O.K.; Kalyan, A.; Kamboj, A.; Mohammed, S.; Alhussien, M.; Reddi, S.; Shimray, P.G.; Rautela, A.; Pandita, S.; et al. Interferon-tau stimulated gene expression, a proxy to predict embryonic mortality in dairy cows. Theriogenology 2018, 120, 61–67. [Google Scholar] [CrossRef]
- Makhseed, M.; Raghupathy, R.; Azizieh, F.; Al-Azemi, M.M.; Hassan, N.A.; Bandar, A. Mitogen-induced cytokine responses of maternal peripheral blood lymphocytes indicate a differential th-type bias in normal pregnancy and pregnancy failure. Am. J. Reprod Immunol. 1999, 42, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Ivashkiv, L.B.; Donlin, L.T. Regulation of type i interferon responses. Nat. Rev. Immunol. 2014, 14, 36–49. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).