Weekly and Daily Tooth Brushing by Care Staff Reduces Gingivitis and Calculus in Racing Greyhounds
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Subject Recruitment
2.2. Teeth Scoring
2.3. Group Allocation
2.4. Brushing Protocol
2.5. Follow Up Visits
2.6. Calculation of Dental Scores
2.7. Analysis
3. Results
3.1. Dental Scoring
3.2. Trainer Reports
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- EFRA—Environment, Food and Rural Affairs Committee. Greyhound Welfare; House of Commons: London, UK, 2016. [Google Scholar]
- Rooney, N.J. Welfare of racing greyhounds—Prioritisation of issues. In Proceedings of the UFAW International Animal Welfare Symposium, Portsmouth, UK, 28–29 June 2011. [Google Scholar]
- O′Neill, D.G.; Church, D.B.; McGreevy, P.; Thomson, P.C.; Brodbelt, D.C. Prevalence of Disorders Recorded in Dogs Attending Primary-Care Veterinary Practices in England. PLoS ONE 2014, 9, e90501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, T. Predisposing factors and gross examination findings in periodontal disease. Clin. Tech. Small Anim. Pr. 2000, 15, 189–196. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, D.; Rooney, N.J.; Brock, C.; Church, D.; Brodbelt, D.C.; Pelgram, C. Greyhounds under general veterinary care in the UK during 2016: Demography and common disorders Canine. Genet. Epidemiol. 2019, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Fries, W.C. The Perils of Gum Disease in Dogs. Available online: http://pets.webmd.com/dogs/features/perlis-gum-disease-dogs? (accessed on 15 May 2021).
- Debowes, L.J.; Mosier, D.; Logan, E.; Harvey, C.E.; Lowry, S.; Richardson, D.C. Association of Periodontal Disease and Histologic Lesions in Multiple Organs from 45 Dogs. J. Veter. Dent. 1996, 13, 57–60. [Google Scholar] [CrossRef]
- Glickman, L.T.; Glickman, N.W.; Moore, G.E.; Goldstein, G.S.; Lewis, H.B. Evaluation of the risk of endocarditis and other car-diovascular events on the basis of the severity of periodontal disease in dogs. J. Am. Vet. Med. Assoc. 2009, 234, 486–494. [Google Scholar] [CrossRef]
- Wonham, K.L. Statistical Model-Based Approaches for Investigating the Welfare of the UK Racing Greyhound Population. Ph.D. Thesis, University of Bristol, Bristol, UK, 2017. [Google Scholar]
- Atkinson, M.; Young, K. Reservoir Dogs: Greyhound Racing, Mimesis and Sports-Related Violence. Int. Rev. Sociol. Sport 2005, 40, 335–356. [Google Scholar] [CrossRef]
- Lindhe, J.; Hamp, S.-E.; Loe, H. Experimental periodontitis in the Beagle dog. J. Periodontal Res. 1973, 8, 1–10. [Google Scholar] [CrossRef]
- White, D.J. Dental calculus: Recent insights into occurrence, formation, prevention, removal and oral health effects of su-pragingival and subgingival deposits. Eur. J. Oral Sci. 1997, 105, 508–522. [Google Scholar] [CrossRef]
- Kinane, D.F. Causation and pathogenesis of periodontal disease. Periodontol. 2000 2001, 25, 8–20. [Google Scholar] [CrossRef]
- Stookey, G.K. Soft Rawhide Reduces Calculus Formation in Dogs. J. Veter. Dent. 2009, 26, 82–85. [Google Scholar] [CrossRef]
- Tatakis, D.N.; Trombelli, L. Modulation of clinical expression of plaque-induced gingivitis. J. Clin. Periodontol. 2004, 31, 229–238. [Google Scholar] [CrossRef]
- Armitage, G.C. Periodontal diagnoses and classification of periodontal diseases. Periodontol. 2000 2004, 34, 9–21. [Google Scholar] [CrossRef]
- Wonham, K.; Browne, W.J.; Casey, R.A.; Blackwell, E.; Rooney, N.J. Development of a method to rapidly assess periodontal health in conscious dog. Unpublished work. 2021. [Google Scholar]
- Stella, J.L.; Bauer, A.E.; Croney, C.C. A cross-sectional study to estimate prevalence of periodontal disease in a population of dogs (Canis familiaris) in commercial breeding facilities in Indiana and Illinois. PLoS ONE 2018, 13, e0191395. [Google Scholar] [CrossRef]
- Wonham, K.; Browne, W.J.; Casey, R.A.; Blackwell, E.; Rooney, N.J. Risk Factors for periodontal disease in greyhounds. Unpublished work. 2021. [Google Scholar]
- Buckley, C.; Colyer, A.; Skrzywanek, M.; Jodkowska, K.; Kurski, G.; Gawor, J.; Ceregrzyn, M. The impact of home-prepared diets and home oral hygiene on oral health in cats and dogs. Br. J. Nutr. 2011, 106, S124–S127. [Google Scholar] [CrossRef] [Green Version]
- Milella, L.; Beckman, B.; Kane, J.S. Evaluation of an Anti-Plaque Gel for Daily Toothbrushing. J. Veter. Dent. 2014, 31, 160–167. [Google Scholar] [CrossRef]
- Tromp, J.A.H.; Jansen, J.; Pilot, T. Gingival health and frequency of tooth brushing in the beagle dog model. J. Clin. Periodontol. 1986, 13, 164–168. [Google Scholar] [CrossRef]
- Tromp, J.A.H.; Van Rijn, L.J.; Jansen, J. Experimental gingivitis and frequency of tooth brushing in the beagle dog model. Clinical findings. J. Clin. Periodontol. 1986, 13, 190–194. [Google Scholar] [CrossRef]
- Harvey, C.; Serfilippi, L.; Barnvos, D. Effect of Frequency of Brushing Teeth on Plaque and Calculus Accumulation, and Gingivitis in Dogs. J. Veter. Dent. 2015, 32, 16–21. [Google Scholar] [CrossRef]
- Ingham, K.E.; Gorrel, C. Assessing oral health and hygiene in dogs. Waltham Focus 1999, 9, 32–33. [Google Scholar]
- Gorrel, C.; Rawlings, J.M. The Role of Tooth-brushing and Diet in the Maintenance of Periodontal Health in Dogs. J. Veter. Dent. 1996, 13, 139–143. [Google Scholar] [CrossRef]
- Greene, J.G.; Vermillion, J.R. The Simplified Oral Hygiene Index. J. Am. Dent. Assoc. 1964, 68, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Kyllar, M.; Witter, K. Prevalence of dental disorders in pet dogs. Vet. Med. 2012, 50, 496–505. [Google Scholar] [CrossRef] [Green Version]
- Gad, T. Periodontal disease in dogs. J. Periodont. Res. 1968, 3, 268–272. [Google Scholar] [CrossRef]
- White, D.J. Processes contributing to the formation of dental calculus. Biofouling 1991, 4, 209–218. [Google Scholar] [CrossRef]
- Bauer, A.E.; Stella, J.; Lemmons, M.; Croney, C.C. Evaluating the validity and reliability of a visual dental scale for detection of periodontal disease (PD) in non-anesthetized dogs (Canis familiaris). PLoS ONE 2018, 13, e0203930. [Google Scholar] [CrossRef] [Green Version]
- Wallis, C.; Patel, K.V.; Marshall, M.; Satunton, R.; Milella, L.; Harris, S.; Holcombe, L.J. A longitudinal assessment of periodontal health status in 53 Labrador retrievers. J. Small Anim. Pract. 2018, 59, 560–569. [Google Scholar] [CrossRef] [Green Version]
| Score | Definition |
|---|---|
| 0 | No observable calculus |
| 1 | Less than 25% coverage of calculus |
| 2 | Between 25–<75% coverage of calculus |
| 3 | 75–100% coverage of calculus |
| Score | Definition |
|---|---|
| 0 | No inflammation |
| 1 | Mild inflammation, slight change in colour, little change in texture of any portion of the gingival unit |
| 2 | Moderate inflammation (moderate glazing, redness, oedema and/or hypertrophy) of the gingival unit |
| 3 | Severe inflammation (marked by redness and oedema/hypertrophy, spontaneous bleeding or ulceration) of the gingival unit |
| Variable Name | Trainer 1 | Trainer 2 | Trainer 3 | Trainer 4 | Trainer 5 | Trainer 6 |
|---|---|---|---|---|---|---|
| Number of dogs completing the trial in each kennel | 27 | 26 | 37 | 18 | 25 | 27 |
| Perceived ease of brushing (1 very easy–5 very difficult) | 1 | 2 | 1 | 1–2 | 3 | 1 |
| Perceived change in the average dog in the kennels’ reaction to brushing over 2 months (+ slight improvement: 1 point on 5 point scale; ++ major improvement: 2 points on 5 point scale) | None | ++ | ++ | + | None | Failed to complete interview |
| Reported average change in gum health with weekly brushing (+ slight improvement: 1 point on 5 point scale; ++ major improvement: 2 points on 5 point scale) | + | + | + | None | None | NA |
| Perceived change in gum health with daily brushing (+ slight improvement: 1 point on 5 point scale; ++ major improvement: 2 points on 5 point scale) | ++ | ++ | ++ | None | None | NA |
| Perceived change in calculus with weekly brushing | ++ | + | + | ++ | + | NA |
| Perceived change in calculus with daily brushing on a five point scale (+ slight improvement: 1 point on 5 point scale; ++ major improvement: 2 points on 5 point scale) | ++ | ++ | ++ | + | + | NA |
| Opinion of what most contributed to improvement, product (P) or brushing (B) | P | P and B | P | Neither | P and B | NA |
| Reported time spent brushing each dog’s teeth | 3–4 min | 1 min | 2 min | 1–2 min | 1.5 min | NA |
| Initial % of dogs with bleeding gums | 30 | 25 | 50 | 5 | 25 | NA |
| Ultimate % of dosg with bleeding gums | 0 | 5 | 0 | 0 | 0 | NA |
| Food soaked in water | Unknown | Cold water 60 min | Hot water 5–10 min | Warm water 3 h | Hot water 60 min | NA |
| Bone feeding regime | Reported roasted whenever in magnetic therapy box | Reported roasted whenever in magnetic therapy box | Roasted every 3–4 weeks | Roasted monthly | Roasted every 1–2 weeks | NA |
| Variable | Dog’s Baseline | Treatment | Kennel Establishment | Comparisons | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable Name | F | p | F | p | F | p | Control-Weekly | p | Control-Daily | p | Weekly-Daily | p |
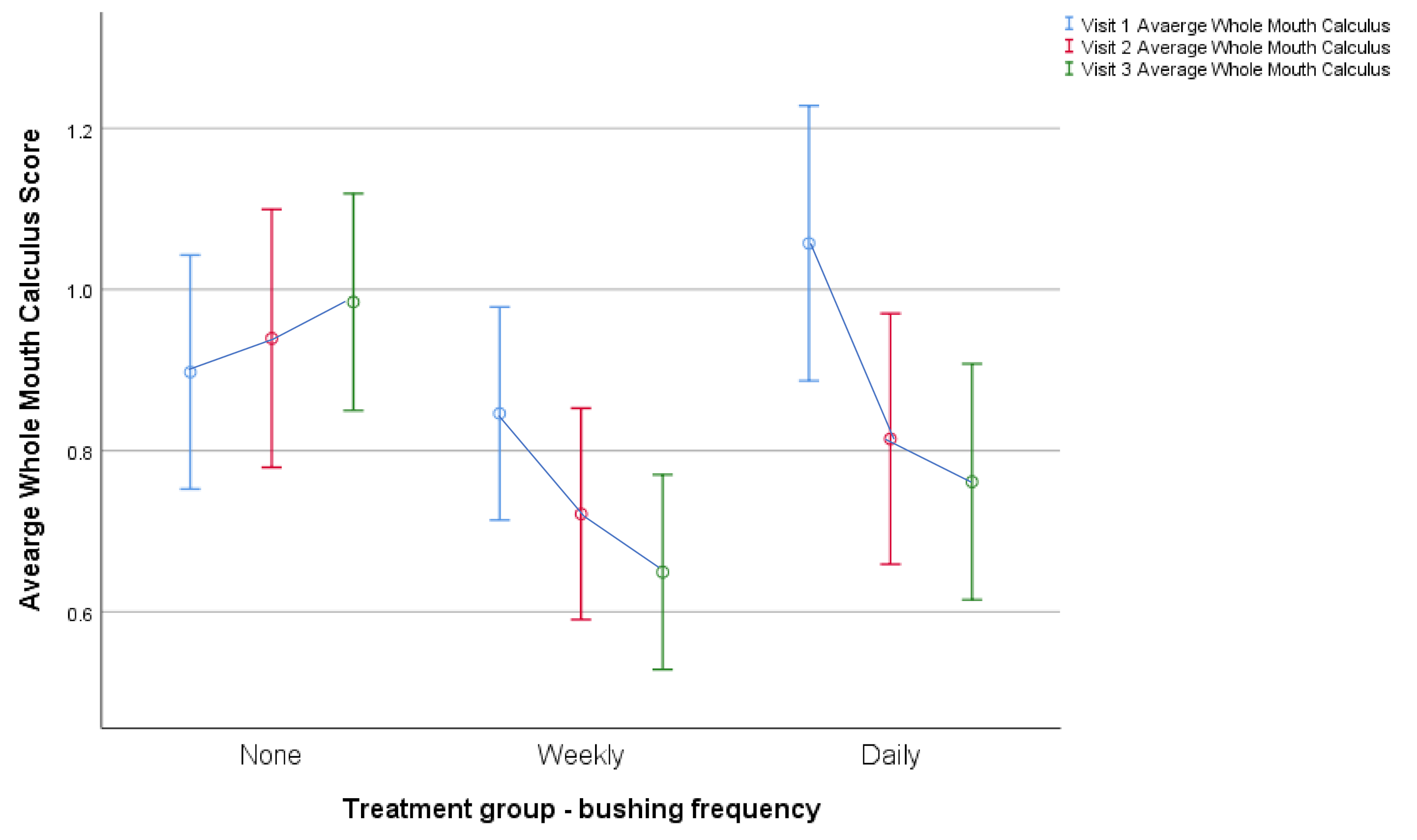
| Average whole mouth calculus | 27.13 | <0.001 | 10.76 | <0.001 | 8.64 | <0.001 | C > W | <0.001 | C > D | <0.001 | W > D | NS |
| Incisor calculus | 33.60 | <0.001 | 1.18 | NS | 0.62 | NS | - | - | - | - | - | - |
| Canine calculus | 11.04 | 0.001 | 5.36 | 0.006 | 6.18 | <0.001 | C > W | 0.003 | C > D | 0.018 | W > D | NS |
| Pre-molar calculus | 15.21 | <0.001 | 8.87 | <0.001 | 9.99 | <0.001 | C > W | <0.001 | C > D | 0.001 | W > D | NS |
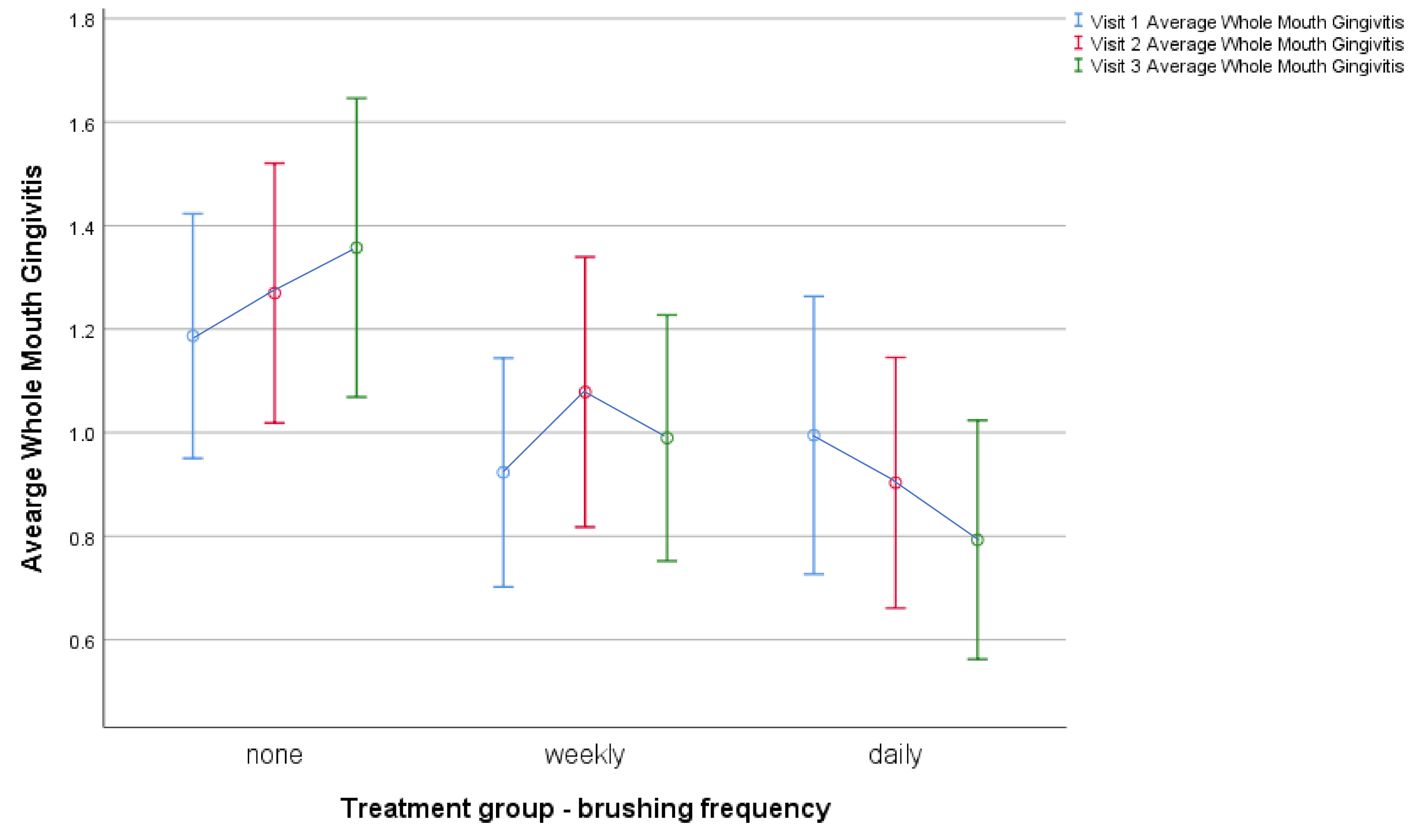
| Average whole mouth gingivitis | 25.21 | <0.001 | 4.57 | 0.012 | 3.51 | 0.005 | C > W | NS | C>D | 0.003 | W > D | NS |
| Incisor gingivitis | 21.31 | <0.001 | 2.56 | NS | 1.22 | NS | - | - | - | - | - | - |
| Canine gingivitis | 14.44 | <0.001 | 3.92 | 0.022 | 3.79 | 0.003 | C > W | NS | C > D | 0.006 | W > D | NS |
| Pre-molar gingivitis | 14.84 | <0.001 | 5.46 | 0.005 | 3.54 | 0.005 | C > W | NS | C > D | 0.002 | W > D | NS |
| Variable | Control | Weekly | Daily | |||
|---|---|---|---|---|---|---|
| Variable Name | Pre (Visit 1) | Post (Visit 3) | Pre (Visit 1) | Post (Visit 3) | Pre (Visit 1) | Post (Visit 3) |
| Whole Mouth Calculus | 0.90 ± 0.496 | 0.99 ± 0.460 | 0.91 ± 0.478 | 0.70 ± 0.471 | 1.06 ± 0.534 | 0.79 ± 0.463 |
| Incisor Calculus | 0.04 ± 0.153 | 0.09 ± 0.211 | 0.10 ± 0.281 | 0.09 ± 0.314 | 0.13 ± 0.347 | 0.09 ± 0.259 |
| Canine Calculus | 1.11 ± 0.637 | 1.09 ± 0.641 | 1.20 ± 0.634 | 0.82 ± 0.654 | 1.26 ± 0.671 | 0.87 ± 0.513 |
| Pre-molar calculus | 1.57 ± 1.061 | 1.80 ± 0.876 | 1.42 ± 0.948 | 1.19 ± 0.852 | 1.81 ± 0.954 | 1.42 ± 0.931 |
| Whole Mouth Gingivitis | 1.19 ± 0.804 | 1.37 ± 0.990 | 1.03 ± 0.839 | 1.01 ± 0.802 | 1.01 ± 0.846 | 0.87 ± 0.771 |
| Incisor Gingivitis | 0.73 ± 0.904 | 0.98 ± 1.198 | 0.56 ± 0.899 | 0.62 ± 0.885 | 0.57 ± 1.000 | 0.54 ± 0.884 |
| Canine Gingivitis | 1.56 ± 0.826 | 1.65 ± 0.900 | 1.41 ± 0.909 | 1.36 ± 0.865 | 1.36 ± 0.802 | 1.16 ± 0.813 |
| Pre-molar Gingivitis | 1.33 ± 0.931 | 1.47 ± 1.005 | 1.13 ± 0.956 | 1.06 ± 0.858 | 1.10 ± 0.954 | 0.90 ± 0.843 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rooney, N.J.; Wonham, K.L.; McIndoe, K.S.; Casey, R.A.; Blackwell, E.J.; Browne, W.J. Weekly and Daily Tooth Brushing by Care Staff Reduces Gingivitis and Calculus in Racing Greyhounds. Animals 2021, 11, 1869. https://doi.org/10.3390/ani11071869
Rooney NJ, Wonham KL, McIndoe KS, Casey RA, Blackwell EJ, Browne WJ. Weekly and Daily Tooth Brushing by Care Staff Reduces Gingivitis and Calculus in Racing Greyhounds. Animals. 2021; 11(7):1869. https://doi.org/10.3390/ani11071869
Chicago/Turabian StyleRooney, Nicola J., Katharine L. Wonham, Katherine S. McIndoe, Rachel A. Casey, Emily J. Blackwell, and William J. Browne. 2021. "Weekly and Daily Tooth Brushing by Care Staff Reduces Gingivitis and Calculus in Racing Greyhounds" Animals 11, no. 7: 1869. https://doi.org/10.3390/ani11071869
APA StyleRooney, N. J., Wonham, K. L., McIndoe, K. S., Casey, R. A., Blackwell, E. J., & Browne, W. J. (2021). Weekly and Daily Tooth Brushing by Care Staff Reduces Gingivitis and Calculus in Racing Greyhounds. Animals, 11(7), 1869. https://doi.org/10.3390/ani11071869






