Glucosamine and Chondroitin Sulfate: Is There Any Scientific Evidence for Their Effectiveness as Disease-Modifying Drugs in Knee Osteoarthritis Preclinical Studies?—A Systematic Review from 2000 to 2021
Abstract
Simple Summary
Abstract
1. Introduction
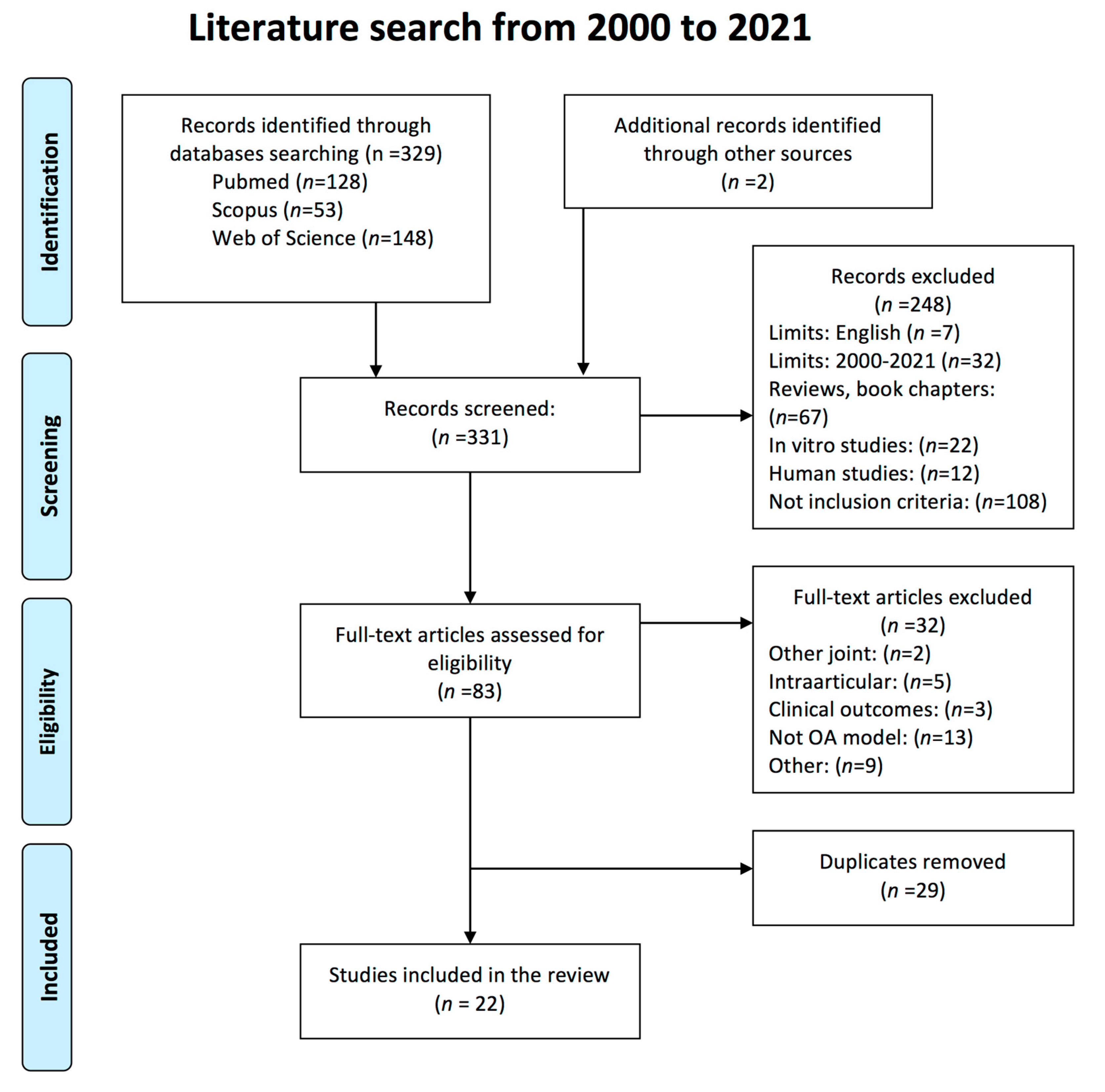
2. Materials and Methods
2.1. Protocol and Search Strategy
- Experimental preclinical studies in animal models of OA which focused on the structural effect of glucosamine and chondroitin sulfate on the knee synovial joint tissues and biochemical markers.
- Studies that included outcome measures by using gross, histologic, histomorphometric, biochemical and/or imaging techniques.
- Articles written in English language.
- Studies published in international peer-reviewed journals between 2000 and February 2021.
2.2. Study Selection and Data Extraction
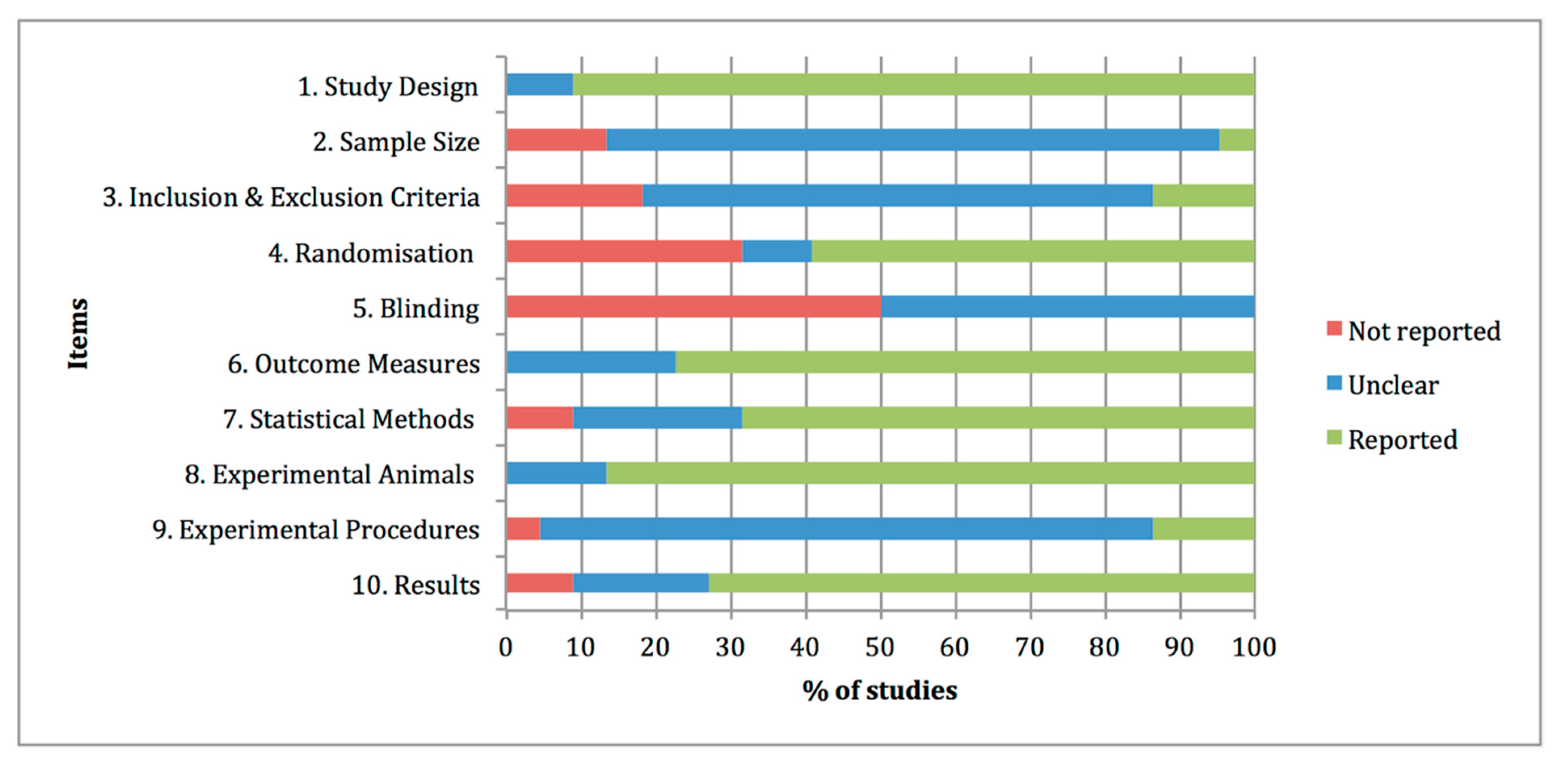
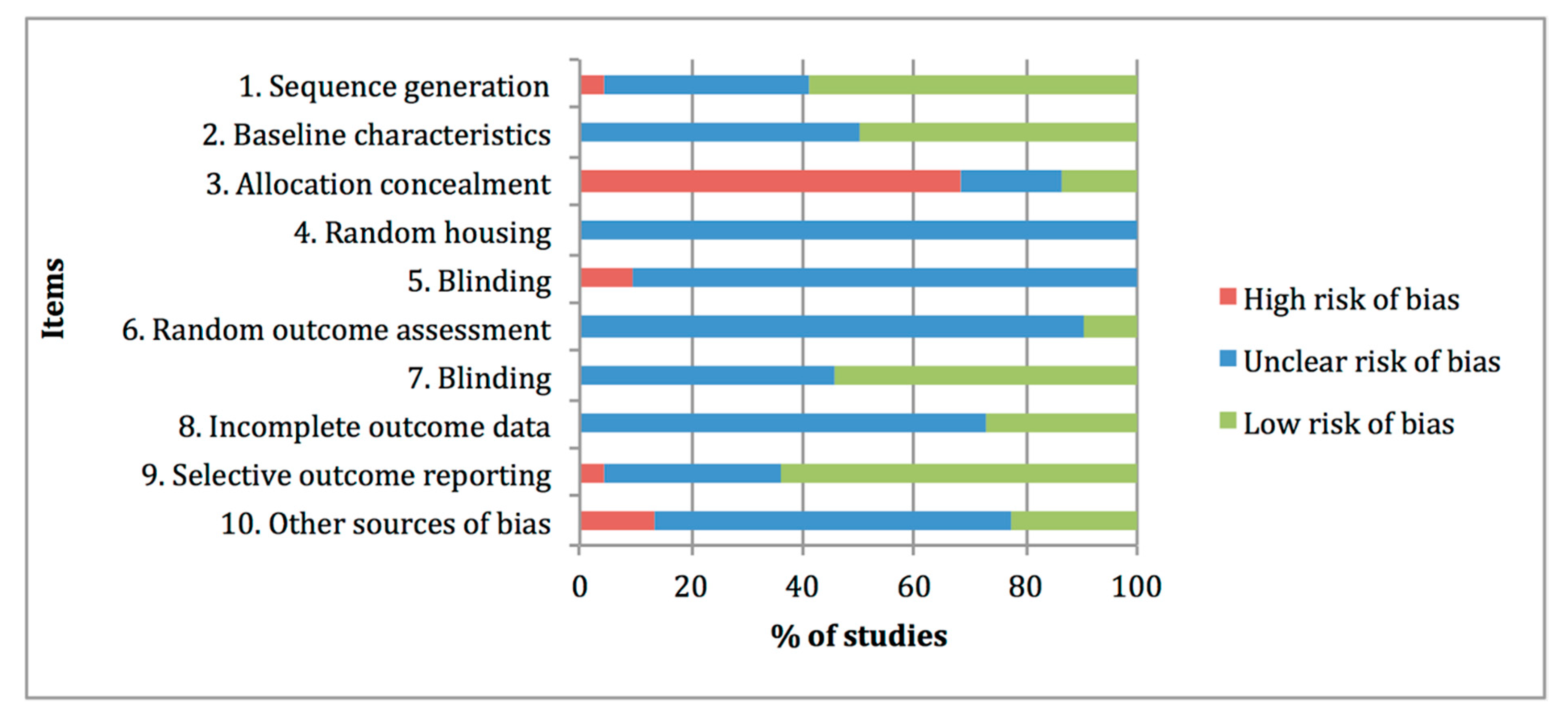
2.3. Quality Assessments and Risk of Bias
3. Results
3.1. Study Selection and Characteristics
3.2. Synthesis of the Main Outcomes of the Effect of Glucosamine and/or Chondroitin Sulfate
3.3. Therapy Duration and Initial Administration at Baseline
3.4. Quality and Risk-of-Bias Assessments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Felson, D.T.; Neogi, T. Osteoarthritis: Is It a Disease of Cartilage or of Bone? Arthritis Rheum. 2004, 50, 341–344. [Google Scholar] [CrossRef]
- Karsdal, M.A.; Leeming, D.J.; Dam, E.B.; Henriksen, K.; Alexandersen, P.; Pastoureau, P.; Altman, R.D.; Christiansen, C. Should subchondral bone turnover be targeted when treating osteoarthritis? Osteoarthr. Cartil. 2008, 16, 638–646. [Google Scholar] [CrossRef]
- Anderson, K.L.; O’Neill, D.G.; Brodbelt, D.C.; Church, D.B.; Meeson, R.L.; Sargan, D.; Summers, J.F.; Zulch, H.; Collins, L.M. Prevalence, duration and risk factors for appendicular osteoarthritis in a UK dog population under primary veterinary care. Sci. Rep. 2018, 8, 1–12. [Google Scholar] [CrossRef]
- Rychel, J.K. Diagnosis and Treatment of Osteoarthritis. Top. Companion Anim. Med. 2010, 25, 20–25. [Google Scholar] [CrossRef]
- Epstein, M.; Rodan, I.; Griffenhagen, G.; Kadrlik, J.; Petty, M.; Robertson, S.; Simpson, W. 2015 AAHA/AAFP pain management guidelines for dogs and cats. J. Am. Anim. Hosp. Assoc. 2015, 51, 67–84. [Google Scholar] [CrossRef]
- Henrotin, Y.; Sanchez, C.; Balligand, M. Pharmaceutical and nutraceutical management of canine osteoarthritis: Present and future perspectives. Vet. J. 2005, 170, 113–123. [Google Scholar] [CrossRef]
- Neundorf, R.H.; Lowerison, M.B.; Cruz, A.M.; Thomason, J.J.; McEwen, B.J.; Hurtig, M.B. Determination of the prevalence and severity of metacarpophalangeal joint osteoarthritis in Thoroughbred racehorses via quantitative macroscopic evaluation. Am. J. Vet. Res. 2010, 71, 1284–1293. [Google Scholar] [CrossRef]
- Espinosa-Mur, P.; Phillips, K.L.; Galuppo, L.D.; DeRouen, A.; Benoit, P.; Anderson, E.; Shaw, K.; Puchalski, S.; Peters, D.; Kass, P.H.; et al. Radiological prevalence of osteoarthritis of the cervical region in 104 performing Warmblood jumpers. Equine Vet. J. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Johnston, S.A. Osteoarthritis. Joint anatomy, physiology, and pathobiology. Vet. Clin. N. Am. Small Anim. Pract. 1997, 27, 699–723. [Google Scholar] [CrossRef]
- O′Neill, D.G.; Church, D.B.; McGreevy, P.D.; Thomson, P.C.; Brodbelt, D.C. Prevalence of Disorders Recorded in Dogs Attending Primary-Care Veterinary Practices in England. PLoS ONE 2014, 9, e90501. [Google Scholar] [CrossRef] [PubMed]
- Slingerland, L.I.; Hazewinkel, H.A.W.; Meij, B.P.; Picavet, P.; Voorhout, G. Cross-sectional study of the prevalence and clinical features of osteoarthritis in 100 cats. Vet. J. 2011, 187, 304–309. [Google Scholar] [CrossRef]
- Bennett, D.; bt Zainal Ariffin, S.M.; Johnston, P. Osteoarthritis in the cat: 1. how common is it and how easy to recognise? J. Feline Med. Surg. 2012, 14, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Bennett, D.; bt Zainal Ariffin, S.M.; Johnston, P. Osteoarthritis in the cat: 2. How should it be managed and treated? J. Feline Med. Surg. 2012, 14, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Apostu, D.; Lucaciu, O.; Mester, A.; Oltean-Dan, D.; Baciut, M.; Baciut, G.; Bran, S.; Onisor, F.; Piciu, A.; Pasca, R.D.; et al. Systemic drugs with impact on osteoarthritis. Drug Metab. Rev. 2019, 51, 498–523. [Google Scholar] [CrossRef] [PubMed]
- Henrotin, Y.; Lambert, C.; Couchourel, D.; Ripoll, C.; Chiotelli, E. Nutraceuticals: Do they represent a new era in the management of osteoarthritis? A narrative review from the lessons taken with five products. Osteoarthr. Cartil. 2011, 19, 1–21. [Google Scholar] [CrossRef]
- McCarthy, G.; O’Donovan, J.; Jones, B.; McAllister, H.; Seed, M.; Mooney, C. Randomised double-blind, positive-controlled trial to assess the efficacy of glucosamine/chondroitin sulfate for the treatment of dogs with osteoarthritis. Vet. J. 2007, 174, 54–61. [Google Scholar] [CrossRef]
- Scott, R.M.; Evans, R.; Conzemius, M.G. Efficacy of an oral nutraceutical for the treatment of canine osteoarthritis: A doubled-blind, randomized, placebo-controlled prospective clinical trial. Vet. Comp. Orthop. Traumatol. 2017, 30, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Moreau, M.; Dupuis, J.; Bonneau, N.H.; Desnoyers, M. Clinical evaluation of a nutraceutical, carprofen and meloxicam for the treatment of dogs with osteoarthritis. Vet. Rec. 2003, 152, 323–329. [Google Scholar] [CrossRef]
- Comblain, F.; Serisier, S.; Barthelemy, N.; Balligand, M.H. Review of dietary supplements for the management of osteoarthritis indogs in studies from 2004 to 2014. J. Vet. Pharmacol. Ther. 2016, 39, 1–15. [Google Scholar] [CrossRef]
- Vandeweerd, J.M.; Coisnon, C.; Clegg, P.; Cambier, C.; Pierson, A.; Hontoir, F.; Saegerman, C.; Gustin, P.; Buczinski, S. Systematic Review of Efficacy of Nutraceuticals to Alleviate Clinical Signs of Osteoarthritis. J. Vet. Intern. Med. 2012, 26, 448–456. [Google Scholar] [CrossRef]
- Bhathal, A.; Spryszak, M.; Louizos, C.; Frankel, G. Glucosamine and chondroitin use in canines for osteoarthritis: A review. Open Vet. J. 2017, 7, 36–49. [Google Scholar] [CrossRef]
- Mével, E.; Monfoulet, L.E.; Merceron, C.; Coxam, V.; Wittrant, Y.; Beck, L.; Guicheux, J. Nutraceuticals in joint health: Animal models as instrumental tools. Drug Discov. Today 2014, 19, 1649–1658. [Google Scholar] [CrossRef]
- Kuyinu, E.L.; Narayanan, G.; Nair, L.S.; Laurencin, C.T. Animal models of osteoarthritis: Classification, update, and measurement of outcomes. J. Orthop. Surg. Res. 2016, 11, 1–27. [Google Scholar] [CrossRef] [PubMed]
- de Vries, R.B.M.; Hooijmans, C.R.; Langendam, M.W.; van Luijk, J.; Leenaars, M.; Ritskes-Hoitinga, M.; Wever, K.E. A protocol format for the preparation, registration and publication of systematic reviews of animal intervention studies. Evid. Based Preclin. Med. 2015, 2, e00007. [Google Scholar] [CrossRef]
- Percie du Sert, N.; Hurst, V.; Ahluwalia, A.; Alam, S.; Avey, M.T.; Baker, M.; Browne, W.J.; Clark, A.; Cuthill, I.C.; Dirnagl, U.; et al. The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. PLOS Biol. 2020, 18, e3000410. [Google Scholar] [CrossRef]
- Hooijmans, C.R.; Rovers, M.M.; De Vries, R.B.M.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef]
- Sun, Y.; Zhang, G.; Liu, Q.; Liu, X.; Wang, L.; Wang, J.; Liang, L. Chondroitin sulfate from sturgeon bone ameliorates pain of osteoarthritis induced by monosodium iodoacetate in rats. Int. J. Biol. Macromol. 2018, 117, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Park, Y.; Ahn, C.W.; Park, S.H.; Jung, E.Y.; Suh, H.J. Deer bone extract suppresses articular cartilage damage induced by monosodium iodoacetate in osteoarthritic rats: An in vivo micro-computed tomography study. J. Med. Food 2014, 17, 701–706. [Google Scholar] [CrossRef]
- Ivanovska, N.; Dimitrova, P. Bone resorption and remodeling in murine collagenase-induced osteoarthritis after administration of glucosamine. Arthritis Res. Ther. 2011, 13. [Google Scholar] [CrossRef] [PubMed]
- Torelli, S.R.; Rahal, S.C.; Volpi, R.S.; Sequeira, J.L.; Grassioto, I.Q. Histopathological evaluation of treatment with chondroitin sulphate for osteoarthritis induced by continuous immobilization in rabbits. J. Vet. Med. Ser. A Physiol. Pathol. Clin. Med. 2005, 52, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Salman, A.; Shabana, A.I.; El-ghazouly, D.E.S.; Maha, E. Protective effect of glucosamine and risedronate (alone or in combination) against osteoarthritic changes in rat experimental model of immobilized knee. Anat. Cell Biol. 2019, 52, 498–510. [Google Scholar] [CrossRef]
- Taniguchi, S.; Ryu, J.; Seki, M.; Sumino, T.; Tokuhashi, Y.; Esumi, M. Long-term oral administration of glucosamine or chondroitin sulfate reduces destruction of cartilage and up-regulation of MMP-3 mRNA in a model of spontaneous osteoarthritis in Hartley guinea pigs. J. Orthop. Res. 2012, 30, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Abdul Kadir, A.; Abdul Kadir, A.; Abd Hamid, R.; Mat Jais, A.M.; Omar, J.; Sadagatullah, A.N.; Badrin, S.; Win, T.T.; Sirajudeen, K.N.S.; Salleh, A. Evaluation of Chondroprotective Activity of Channa striatus in Rabbit Osteoarthritis Model. Biomed. Res. Int. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Jeong, D.H.; Ullah, H.M.A.; Goo, M.J.; Ghim, S.G.; Hong, I.H.; Kim, A.Y.; Jeon, S.M.; Choi, M.S.; Elfadl, A.K.; Chung, M.J.; et al. Effects of oral glucosamine hydrochloride and mucopolysaccharide protein in a rabbit model of osteoarthritis. Int. J. Rheum. Dis. 2017, 21, 620–628. [Google Scholar] [CrossRef]
- Roman-Blas, J.A.; Mediero, A.; Tardío, L.; Portal-Nuñez, S.; Gratal, P.; Herrero-Beaumont, G.; Largo, R. The combined therapy with chondroitin sulfate plus glucosamine sulfate or chondroitin sulfate plus glucosamine hydrochloride does not improve joint damage in an experimental model of knee osteoarthritis in rabbits. Eur. J. Pharmacol. 2017, 794, 8–14. [Google Scholar] [CrossRef]
- Permuy, M.; Guede, D.; López-Peña, M.; Muñoz, F.; Caeiro, J.R.; González-Cantalapiedra, A. Comparison of various SYSADOA for the osteoarthritis treatment: An experimental study in rabbits Clinical rheumatology and osteoporosis. BMC Musculoskelet. Disord. 2015, 16, 1–12. [Google Scholar] [CrossRef]
- Ohnishi, A.; Osaki, T.; Matahira, Y.; Tsuka, T.; Imagawa, T.; Okamoto, Y.; Minami, S. Evaluation of the chondroprotective effects of glucosamine and fish collagen peptide on a rabbit ACLT model using serum biomarkers. J. Vet. Med. Sci. 2013, 75, 421–429. [Google Scholar] [CrossRef]
- Wang, S.X.; Laverty, S.; Dumitriu, M.; Plaas, A.; Grynpas, M.D. The effects of glucosamine hydrochloride on subchondral bone changes in an animal model of osteoarthritis. Arthritis Rheum. 2007, 56, 1537–1548. [Google Scholar] [CrossRef]
- Kobayashi, T.; Notoya, K.; Nakamura, A.; Akimoto, K. Fursultiamine, a vitamin B1 derivative, enhances chondroprotective effects of glucosamine hydrochloride and chondroitin sulfate in rabbit experimental osteoarthritis. Inflamm. Res. 2005, 54, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Tiraloche, G.; Girard, C.; Chouinard, L.; Sampalis, J.; Moquin, L.; Ionescu, M.; Reiner, A.; Poole, A.R.; Laverty, S. Effect of oral glucosamine on cartilage degradation in a rabbit model of osteoarthritis. Arthritis Rheum. 2005, 52, 1118–1128. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.X.; Cai, L. Expression level of proteoglycan, collagen and type II collagen in osteoarthritis rat model is promoted and degradation of cartilage is prevented by glucosamine methyl ester. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 3609–3616. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z.; Ji, Y.; Wang, Y.; Dong, L. Chondroitin sulfate from Scophthalmus maximus for treating osteoarthritis. Int. J. Biol. Macromol. 2017, 108, 1158–1164. [Google Scholar] [CrossRef] [PubMed]
- Sanches, M.; Assis, L.; Criniti, C.; Fernandes, D.; Tim, C.; Renno, A.C.M. Chondroitin sulfate and glucosamine sulfate associated to photobiomodulation prevents degenerative morphological changes in an experimental model of osteoarthritis in rats. Lasers Med. Sci. 2017, 33, 549–557. [Google Scholar] [CrossRef]
- Terencio, M.C.; Ferrándiz, M.L.; Carceller, M.C.; Ruhí, R.; Dalmau, P.; Vergés, J.; Montell, E.; Torrent, A.; Alcaraz, M.J. Chondroprotective effects of the combination chondroitin sulfate-glucosamine in a model of osteoarthritis induced by anterior cruciate ligament transection in ovariectomised rats. Biomed. Pharmacother. 2016, 79, 120–128. [Google Scholar] [CrossRef]
- Panahifar, A.; Jaremko, J.L.; Tessier, A.G.; Lambert, R.G.; Maksymowych, W.P.; Fallone, B.G.; Doschak, M.R. Development and reliability of a multi-modality scoring system for evaluation of disease progression in pre-clinical models of osteoarthritis: Celecoxib may possess disease-modifying properties. Osteoarthr. Cartil. 2014, 22, 1639–1650. [Google Scholar] [CrossRef] [PubMed]
- Wen, Z.H.; Tang, C.C.; Chang, Y.C.; Huang, S.Y.; Hsieh, S.P.; Lee, C.H.; Huang, G.S.; Ng, H.F.; Neoh, C.A.; Hsieh, C.S.; et al. Glucosamine sulfate reduces experimental osteoarthritis and nociception in rats: Association with changes of mitogen-activated protein kinase in chondrocytes. Osteoarthr. Cartil. 2010, 18, 1192–1202. [Google Scholar] [CrossRef]
- Naito, K.; Watari, T.; Furuhata, A.; Yomogida, S.; Sakamoto, K.; Kurosawa, H.; Kaneko, K.; Nagaoka, I. Evaluation of the effect of glucosamine on an experimental rat osteoarthritis model. Life Sci. 2010, 86, 538–543. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.S.; Yoshinari, N.H.; Castro, R.R.; Girão, V.C.C.; Pompeu, M.M.L.; Andrade Feitosa, J.P.; Rocha, F.A.C. Combined glucosamine and chondroitin sulfate provides functional and structural benefit in the anterior cruciate ligament transection model. Clin. Rheumatol. 2009, 28, 109–117. [Google Scholar] [CrossRef]
- Contartese, D.; Tschon, M.; De Mattei, M.; Fini, M. Molecular Sciences Sex Specific Determinants in Osteoarthritis: A Systematic Review of Preclinical Studies. Int. J. Mol. Sci. 2020, 21, 3696. [Google Scholar] [CrossRef] [PubMed]
- Shmagel, A.; Demmer, R.; Knights, D.; Butler, M.; Langsetmo, L.; Lane, N.E.; Ensrud, K. The effects of glucosamine and chondroitin sulfate on gut microbial composition: A systematic review of evidence from animal and human studies. Nutrients 2019, 11, 294. [Google Scholar] [CrossRef]
- Lampropoulou-Adamidou, K.; Lelovas, P.; Karadimas, E.V.; Liakou, C.; Triantafillopoulos, I.K.; Dontas, I.; Papaioannou, N.A. Useful animal models for the research of osteoarthritis. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 263–271. [Google Scholar] [CrossRef] [PubMed]
- McCoy, A.M. Animal Models of Osteoarthritis: Comparisons and Key Considerations. Vet. Pathol. 2015, 52, 803–818. [Google Scholar] [CrossRef]
- Fonsi, M.; El Amrani, A.I.; Gervais, F.; Vincent, P. Intra-Articular Hyaluronic Acid and Chondroitin Sulfate: Pharmacokinetic Investigation in Osteoarthritic Rat Models. Curr. Ther. Res. Clin. Exp. 2020, 92. [Google Scholar] [CrossRef]
- Frisbie, D.D.; McIlwraith, C.W.; Kawcak, C.E.; Werpy, N.M. Evaluation of intra-articular hyaluronan, sodium chondroitin sulfate and N-acetyl-d-glucosamine combination versus saline (0.9% NaCl) for osteoarthritis using an equine model. Vet. J. 2013, 197, 824–829. [Google Scholar] [CrossRef]
- Gibson, M.; Li, H.; Coburn, J.; Moroni, L.; Nahas, Z.; Bingham, C.; Yarema, K.; Elisseeff, J. Intra-articular delivery of glucosamine for treatment of experimental osteoarthritis created by a medial meniscectomy in a rat model. J. Orthop. Res. 2014, 32, 302–309. [Google Scholar] [CrossRef]
- Scotto D’Abusco, A.; Corsi, A.; Grillo, M.G.; Cicione, C.; Calamia, V.; Panzini, G.; Sansone, A.; Giordano, C.; Politi, L.; Scandurra, R. Effects of intra-articular administration of glucosamine and a peptidyl-glucosamine derivative in a rabbit model of experimental osteoarthritis: A pilot study. Rheumatol. Int. 2008, 28, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Shikhman, A.R.; Amiel, D.; D’Lima, D.; Hwang, S.B.; Hu, C.; Xu, A.; Hashimoto, S.; Kobayashi, K.; Sasho, T.; Lotz, M.K. Chondroprotective activity of N-acetylglucosamine in rabbits with experimental osteoarthritis. Ann. Rheum. Dis. 2005, 64, 89–94. [Google Scholar] [CrossRef]
- Henrotin, Y.; Mobasheri, A.; Marty, M. Is there any scientific evidence for the use of glucosamine in the management of human osteoarthritis? Arthritis Res. Ther. 2012. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Martín, S.; López-Peña, M.; Muñoz, F.; Permuy, M.; González-Cantalapiedra, A. Bisphosphonates as disease-modifying drugs in osteoarthritis preclinical studies: A systematic review from 2000 to 2020. Arthritis Res. Ther. 2021, 23, 60. [Google Scholar] [CrossRef]
- Leung, V.; Rousseau-Blass, F.; Beauchamp, G.; Pang, D.S.J. ARRIVE has not ARRIVEd: Support for the ARRIVE (Animal Research: Reporting of in vivo Experiments) guidelines does not improve the reporting quality of papers in animal welfare, analgesia or anesthesia. PLoS ONE 2018, 13, e0197882. [Google Scholar] [CrossRef]
- Pastoureau, P.C.; Hunziker, E.B.; Pelletier, J.P. Cartilage, bone and synovial histomorphometry in animal models of osteoarthritis. Osteoarthr. Cartil. 2010, 18, S106–S112. [Google Scholar] [CrossRef] [PubMed]
- Malek, S.; Sample, S.J.; Schwartz, Z.; Nemke, B.; Jacobson, P.B.; Cozzi, E.M.; Schaefer, S.L.; Bleedorn, J.A.; Holzman, G.; Muir, P. Effect of analgesic therapy on clinical outcome measures in a randomized controlled trial using client-owned dogs with hip osteoarthritis. BMC Vet. Res. 2012, 8, 185. [Google Scholar] [CrossRef] [PubMed]
| References | Animal Model (n) | OA Model | Therapy: Dosage, Frequency and Administration Route (Duration Treatment) | Start Point (1) | Follow-Up (2) Outcome Measures | Main Results |
|---|---|---|---|---|---|---|
| Abdul-Kadir et al. 2019 [33] | New Zealand Rabbit Male 7–8 months old (33) | Surgically induced OA: ACLT | GS (77.5 mg/kg/day) orally Channa (51.4 mg/kg/day) orally (8 weeks) | 3 weeks | 8 weeks Macroscopic evaluation. Histology of cartilage (modified OARSI score). Histomorphometry (cartilage roughness and Cg.Th). Serum biomarkers (COMP, COX-2 and PGE2) | Both treatment groups showed lower histopathology changes compared to the untreated group. However, Channa showed less cartilage roughness compared to GS treated-animals. Channa and GS significantly ↓COMP levels |
| Jeong et al. 2017 [34] | New Zealand Rabbit 9 month old (24) | Surgically induced OA: ACLT | GH (100 mg/kg/day), orally Celecoxib (10 mg/kg/day), orally MucoP (100 mg/kg/day), orally (8 weeks) | 3 days | 8 weeks X-ray. Macroscopic evaluation. Histology of cartilage. GAG quantification. TUNEL assay (Apoptosis of chondrocytes). | Macroscopically GH and MucoP groups had significantly milder cartilage damage and fibrillation. All the treatments investigated showed significantly reduced histology degenerative changes and prevented the apoptosis od chondrocytes. |
| Roman-Blas et al. 2017 [35] | New Zealand Rabbit Male (20) | Surgically induced OA: ACLT and partial MMT | CS (1200 mg/day) + GS (1500 mg/day), orally CS (1200 mg/day) + GH (1500 mg/day), orally (14 weeks) | −14 days | 12 weeks Histology of cartilage (Mankin score) and synovial membrane (Krenn scale); X-ray densitometer scanner (Subchondral BMD) and Western blot studies (COX-2, IL-1β, iNOS, MMP-1, MMP-3, MMP-13) | Treatments did not significantly modify the cartilage damage or the synovial inflammation and failed to conserve the subchondral BMD. In addition, were unable to decrease the biochemical OA markers expression. |
| Permuy et al. 2015 [36] | New Zealand Rabbit Female Adult (56) | Surgically induced OA: ACLT and partial MMT | GS (21.5 mg/kg/day) orally CS (11.5 mg/kg/day) i.p. HA (0.3 mg/kg/week) i.a. DC (1.5 mg/kg/day) orally RIS (0.07 mg/kg/day) orally GS + RIS daily orally (8 weeks) | 3 weeks | 11 weeks Histology of cartilage and synovial membrane (OARSI score). Histomorphometric evaluation (Tb.A, Tb.Sp, SB.Th, FI, Cg.Th) and μ-CT (vBMD, BV/TV, Tb.Th, Tb.Sp, Tb.N, Tb.Pf, SMI, nCgTh) | GS and CS prevented cartilage swelling but did not reduce the cartilage damage or the superficial fibrillation. In addition, they did not have any effect on synovial and subchondral bone. |
| Ohnishi et al. 2013 [37] | Japanese Rabbit Female 12 weeks old (12) | Surgically induced OA: ACLT | FCP (1000 mg/day), orally GH (1000 mg/day), orally FCP + GS daily orally (4 weeks) | 0 days | 4 weeks Macroscopic evaluation. Histology of cartilage (modified Mankin score). IHQ (CTX-II). Serum biomarkers (CS-846, HA, KS) | Administration of FCP and/or GH showed chondroprotective effects. However, there were no significant differences in the biomarker concentrations comparing with untreated animals (↑CS846 and HA) |
| Wang et al. 2007 [38] | New Zealand Rabbit Male 9 month old (26) | Surgically induced OA: ACLT | GH (100 mg/day) orally (8 weeks) | 1 day | 8 weeks Macroscopic evaluation. X-ray absorptiometry scanner (BMD). Histomorphomethry (osteoid volumen, osteoid thicknes, BV/TV, Tb.Th, Tb.Sp, Tb.N, SB.Th) | GH tended to have lower severity of cartilage lesions but this difference was not significant. Additionally, GH prevented the subchondral bone changes and prevented the trabecular bone loss. |
| Kobayashi et al. 2005 [39] | Japanese Rabbit Male 13 weeks old (30) | Surgically induced OA: Partial MMT | GH (1000 mg/kg/day) + CS (800 mg/kg/day), orally GH + CS + Fursultiamine (100 mg/kg/day), orally (8 weeks) | 3 days | 8 weeks Macroscopic evaluation. Histology of cartilage (modified Mankin score). IHQ (MMP-1) | The GH + CS treatment slightly reduce the severity of cartilage lesions but no significantly. Only the group with received the combined treatment with fursultiamine showed a significant chondroprotective effects and ↓MMP-1. |
| Tiraloche et al. 2005 [40] | New Zealand Rabbit Male 9 month old (39) | Surgically induced OA: ACLT | GH (100 mg/day) orally (8 weeks) | 3 weeks | 11 weeks Macroscopic evaluation. Histology of cartilage (modified Mankin score). GAG quantification and total type II collagen. | GH administration tended to have lower macroscopic severity grades compared with placebo group, but it was not significant. Regarding histology parameters, GH did not prevent the cartilage erosion nor superficial fibrillation. |
| Torelli et al. 2005 [30] | Norflok Rabbit Female 2.5–3 monts old (40) | Physically induced OA: Immobilization (12 weeks) | CS (120 mg/week) s.c. (12 weeks) | 0 days | 12 weeks Histology of cartilage (hematoxylin-eosin, Masson trichrome and picrosirius red) and proteoglycan content. | CS did not reduce the histological changes such as cartilage fibrillation, chondrocyte disorganization and ↓proteoglycan, compared to untreated animals. |
| Salman et al. 2019 [31] | Abino Rat Male Adult (25) | Physically induced OA: Immobilization (6 weeks) | GS (40 mg/kg/day), orally RIS (0.2 mg/kg/day), orally GS + RIS daily orally (6 weeks) | 0 days | 6 weeks Histology of cartilage (modified Mankin score). Histomorphometry (Cg.Th, chondrocytes number). IHQ (type II collagen) | Both treatments improved the articular cartilage damage with the least degenerative changes in the group treated with a combination of both drugs. GS and RIS alone did not prevent the chondrocytes number decrease. ↑type II collagen. |
| Sun et al. 2018 [27] | Sprague Dawley Rat Male 5–6 weeks old (48) | Chemically induced OA: MIA | CSSB (50 mg/kg/day), orally CSSB (100 mg/kg/day), orally CSSB (200 mg/kg/day), orally CS (200 mg/kg/day), orally (1 month) | 0 days | In-vivo paint and bearing test, daily 1 month Histology of cartilage (OARSI score). Synovial markers (IL-1β, TNF-alpha, PGE2 and NO). Western-blot (MMP-1, MMP-3 and TIMP-1) | Treated groups exhibited significant reduced histopathological cartilage changes, relieved joint pain and showed ↓IL1β, TNF-alpha, PGE2 and NO. Additionally, regulated the protein expression (↓MMP-1 and MMP-3 and ↑TIMP-1). Dose-dependent manner. |
| Wang et al. 2018 [41] | Sprague Dawley Rat (40) | Surgically induced OA: ACLT and MMT | GS (2, 5 or 10 mg/kg/day), intraperitonally (1 month) | 0 days | 1 month Histology of cartilage. IHQ (type II collagen). Synovial fluid inflammatory mediators (NO and IL1β). Western-blot (MMP-1, MMP-13). qPCR (TIMP-1) | Glucosamine treatment prevented cartilage degradation, up-regulated the levels of type II collagen and ↓MMP-1 and MMP-13 and ↑TIMP-1, in a dose-dependent manner. |
| Ren et al. 2017 [42] | Rat Male (24) | Surgically induced OA: ACLT | CSSM (25 mg/twice daily), orally CS (shark) (25 mg/twice daily), orally (6 weeks) | 4 weeks | 10 weeks Macroscopic evaluation. Histology of cartilage (Mankin score). Synovial fluid inflammatory mediators (IL-1β, TNF-alpha, PGE2). TUNNEL assay (Apoptosis of chondrocytes). Western-blot (MMP-1 and TIMP-1). | Treated groups showed chondroprotective effects by inhibiting the cartilage degradation and the apoptosis of chondrocytes. ↓IL-1β, TNF-alpha, PGE2, ↓MMP-1 and ↑TIMP-1. |
| Sanches et al. 2017 [43] | Wistar Rat Male 8 weeks old (40) | Surgically induced OA: ACLT | CS (400 mg/kg) + GS (500 mg/kg) 3 days/week, orally CS + GS + photobiomodulation (29 days) | 2 days | 30 days Histology of cartilage (OARSI score). Histomorphometry (chondrocytes density and CgTh). IHQ (IL-1β, IL-10, type II collagen) | All treated groups showed lower degenerative histological changes and chondrocytes density. Animals treated with CS + GS + PBM showed significant ↓IL-1β and ↑IL-10 and type II collagen compared to untreated group. |
| Terencio et al. 2016 [44] | Wistar Rat Female 10 weeks old (45) | OVX + Surgically induced OA: ACLT (2 weeks post-OVX) | CS (140 mg/kg/day) + GH (175 mg/kg/day), orally (12 weeks) | −2 weeks | 10 weeks Histology of cartilage and synovial membrane (OARSI score). Synovial fluid inflammatory mediators by ELISA (IL-1β, TNF-alpha) and radioimmunoassay (PGE2). Serum biomarkers (CTX-II, MMP-3, OPG, RANKL and osteocalcin). μ-CT (BV/TV, Tb.Th, Tb.N and vBMD) | OARSI scores of cartilage degradation were decreased in the treated group. CS and GH showed reduced levels of inflammatory mediators (↓IL-1β and TNF-alpha, CTX-II, MMP-3, OPG, RANKL) and a tendency to prevent the bone microstructural changes (↑vBMD) although, without statistical significance. |
| Panahafir et al. 2014 [45] | Sprague Dawley Rat 9 month old (27) | Surgically induced OA: KTI | Celecoxib (2.86 mg/kg/day), orally GH (192 mg/kg/day), orally (4, 8 or 12 weeks) | 0 days | 4, 8 or 12 weeks μ-CT and MRI. Histology of cartilage and synovial membrane (RAKSS score) | None of the treatments prevented cartilage loss, synovial inflammation or subchondral sclerosis. Additionally, GH failed to prevent the osteophyte formation |
| Lee et al. 2014 [28] | Wistar Rat Male 6 weeks old (50) | Chemically induced OA: MIA | GS (125 mg/kg) + CS (125 mg/kg), daily orally Deer bone extract (250 or 500 mg/kg/day), orally (50 days) | 0 days | 50 days μ-CT (BV/TV, Tb.Th, Tb.N and Tb.Sp) | Both treatments relieved the morphological bone changes. ↑BV/TV and Tb.Th, ↓Tb.Sp. |
| Wen et al. 2010 [46] | Wistar Rat Male 2 moth old (36) | Surgically induced OA: ACLT | GS (250 mg/kg/day/, orally (10 weeks) | 5 weeks | 3, 6, 9, 12, 15 and 18 weeks Allodynia and weight-bearing Macroscopic evaluation. Histology of cartilage and synovial membrane (Mankin score). IHQ (p38, JNK, ERK and MAPKs) | GS treated animals showed significantly lower cartilage damage and suppressed the synovial inflammation. Additionally, reduced the allodynia and weight bearing. ↓p38 and JNK, ↑ERK. |
| Naito et al. 2010 [47] | Sprague Dawley Rat Male 10 week old (18) | Surgically induced OA: ACLT | GH (1000 mg/kg/day), orally (8 weeks) | 0 days | 56 days Macroscopic evaluation. Histology of cartilage (Mankin score). Serum biomarkers (CTX-I, CTX-II, CPII) | GH administration suppressed the macroscopic changes and reduced the Mankin scores, but not significantly. ↓CTX-II, ↑CPII |
| Silva et al. 2009 [48] | Wistar Rat Male (?) | Surgically induced OA: ACLT | GS (500 mg/kg/day), orally GS (500 mg/kg/day) + CS (400 mg/kg/day), orally (70 days) | −7 days | In-vivo joint pain 70 days Histology of cartilage (OARSI score). Densitometry (CS content of cartilage) | GS + CS significantly prevented the cartilage histology alterations. Additionally, significantly reversed the increase in the CS cartilage quantification and reduced the joint pain. |
| Ivanovska et al. 2011 [29] | Outbred ICR (CD-2) Mice Male 10–12 weeks old (50) | Chemically induced OA: CIOA | GS (20 mg/kg/day), orally GH (20 mg/kg/day), orally (20 days) | 0 or 7 days | 30 days Histology of cartilage. Osteophyte area. Synovial fluid inflammatory mediators (RANKL, TNF-alpha, IL-6, IL-4 and IL-10). IHQ (RANKL, BMP-2) | GH significantly reduces the cartilage damage and osteophyte area. Additionally, ameliorates the OA progression by regulating the degree of bone resorption and bone remodeling. ↓RANKL, BMP-2 and IL-6, ↑IL-10. |
| Taniguchi et al. 2011 [32] | Hartley Guinea-pig Female 3 weeks old (50) | Spontaneusly model: Naturally occurring | GH (200 mg/kg/day), orally CS (200 mg/kg/day), orally (8, 12 or 18 months) | — | 8, 12 or 18 months Histology of cartilage (modified Mankin score). TUNEL assay (Apoptosis of chondrocytes). mRNA levels for cartilage tissue (MMP-3, MMP-8, MMP-13, collagen type II and aggrecan) | Long-term GH or CS administration reduced the cartilage degeneration. Additionally, inhibited the loss of cartilage total RNA and the increase of MMP-3 mRNA |
| Nutraceutical | Reference | Initial Adminst Ration | C | SB | SM | OST | BM |
|---|---|---|---|---|---|---|---|
| Glucosamine sulfate (GS) | Abdul-Kadir et al. [33] | Delayed | + | x | x | x | + |
| n = 6 | Permuy et al. [36] | Delayed | − | − | − | x | x |
| Salman et al. [31] | Early | + | x | x | x | + | |
| Wang et al. [41] | Early | + | x | x | x | + | |
| Wen et al. [46] | Delayed | + | x | + | x | + | |
| Ivanovska et al. [29] | Early | - | x | x | - | - | |
| Glucosamine hydrochloride (GH) | Jeong et al. [34] | Early | + | x | x | x | + |
| n = 8 | Ohnishi et al. [37] | Early | + | x | x | x | − |
| Wang et al. [38] | Early | ? | + | x | x | x | |
| Tiraloche et al. [40] | Delayed | ? | x | x | x | − | |
| Panahafir et al. [45] | Early | - | - | - | - | x | |
| Naito et al. [47] | Early | ? | x | x | x | + | |
| Ivanovska et al. [29] | Early | + | x | x | + | + | |
| Taniguchi et al. [32] | Pre-emptive | + | x | x | x | + | |
| Chondroitin sulfate | Permuy et al. [36] | Delayed | − | − | − | x | x |
| n = 5 | Torelli et al. [30] | Early | − | x | x | x | x |
| Sun et al. [27] | Early | + | x | x | x | + | |
| Ren et al. [42] | Delayed | + | x | x | x | + | |
| Taniguchi et al. [32] | Pre-emptive | + | x | x | x | + | |
| Chondroitin sulfate + GH | Roman-Blas et al. [35] | Pre-emptive | − | − | − | x | − |
| n = 3 | Kobayashi et al. [39] | Early | ? | x | x | x | ? |
| Terencio et al. [44] | Pre-emptive | + | ? | ? | x | + | |
| Chondroitin sulfate + GS | Roman-Blas et al. [35] | Pre-emptive | − | − | − | x | − |
| n = 4 | Sanches et al. [43] | Early | + | x | x | x | ? |
| Lee et al. [28] | Early | x | + | x | x | x | |
| Silva et al. [48] | Pre-emptive | + | x | x | x x | + |
| Animal Model | Short-term (≤8 Weeks) | Intermediate-Term (>8 to <24 Weeks) | Long-Term (≥24 Weeks) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Reference | Therapy | Duration | Reference | Therapy | Duration | Reference | Therapy | Duration | |
| Rabbit | Abdul-Kadir et al. [33] | GS | 8 weeks | Roman-Blas et al. [35] | GH/GS + CS | 14 weeks | |||
| Jeong et al. [34] | GH | 8 weeks | Torelli et al. [30] | CS | 12 weeks | ||||
| Permuy et al. [36] | GS/CS | 8 weeks | |||||||
| Ohnishi et al. [37] | GH | 4 weeks | |||||||
| Wang et al. [38] | GH | 8 weeks | |||||||
| Kobayashi et al. [39] | GH + CS | 8 weeks | |||||||
| Tiraloche et al. [40] | GH | 8 weeks | |||||||
| Rat | Salman et al. [31] | GS | 6 weeks | Terencio et al. [44] | GH + CS | 12 weeks | |||
| Sun et al. [27] | CS | 4 weeks | Panahafir et al. [45] | GH | 12 weeks | ||||
| Wang et al. [41] | GS | 4 weeks | Wen et al. [46] | GS | 10 weeks | ||||
| Ren et al. [42] | CS | 6 weeks | Silva et al. [48] | GS + CS | 10 weeks | ||||
| Sanches et al. [43] | GH + CS | 4 weeks | |||||||
| Lee et al. [28] | GS + CS | 7 weeks | |||||||
| Naito et al. [47] | GH | 8 weeks | |||||||
| Mice | Ivanovska et al. [29] | GH /GS | 3 weeks | ||||||
| Guinea-Pig | Taniguchi et al. [32] | GH/CS | 18 months | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Martín, S.; González-Cantalapiedra, A.; Muñoz, F.; García-González, M.; Permuy, M.; López-Peña, M. Glucosamine and Chondroitin Sulfate: Is There Any Scientific Evidence for Their Effectiveness as Disease-Modifying Drugs in Knee Osteoarthritis Preclinical Studies?—A Systematic Review from 2000 to 2021. Animals 2021, 11, 1608. https://doi.org/10.3390/ani11061608
Fernández-Martín S, González-Cantalapiedra A, Muñoz F, García-González M, Permuy M, López-Peña M. Glucosamine and Chondroitin Sulfate: Is There Any Scientific Evidence for Their Effectiveness as Disease-Modifying Drugs in Knee Osteoarthritis Preclinical Studies?—A Systematic Review from 2000 to 2021. Animals. 2021; 11(6):1608. https://doi.org/10.3390/ani11061608
Chicago/Turabian StyleFernández-Martín, Silvia, Antonio González-Cantalapiedra, Fernando Muñoz, Mario García-González, María Permuy, and Mónica López-Peña. 2021. "Glucosamine and Chondroitin Sulfate: Is There Any Scientific Evidence for Their Effectiveness as Disease-Modifying Drugs in Knee Osteoarthritis Preclinical Studies?—A Systematic Review from 2000 to 2021" Animals 11, no. 6: 1608. https://doi.org/10.3390/ani11061608
APA StyleFernández-Martín, S., González-Cantalapiedra, A., Muñoz, F., García-González, M., Permuy, M., & López-Peña, M. (2021). Glucosamine and Chondroitin Sulfate: Is There Any Scientific Evidence for Their Effectiveness as Disease-Modifying Drugs in Knee Osteoarthritis Preclinical Studies?—A Systematic Review from 2000 to 2021. Animals, 11(6), 1608. https://doi.org/10.3390/ani11061608







