Red Cell Distribution Width Has a Negative Prognostic Role in Dogs with Myxomatous Mitral Valve Disease
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Echocardiographic Examination
2.3. Blood Analysis
2.4. Statistical and Survival Analysis
3. Results
3.1. Animals
3.2. Laboratory and Echocardiographic Variables
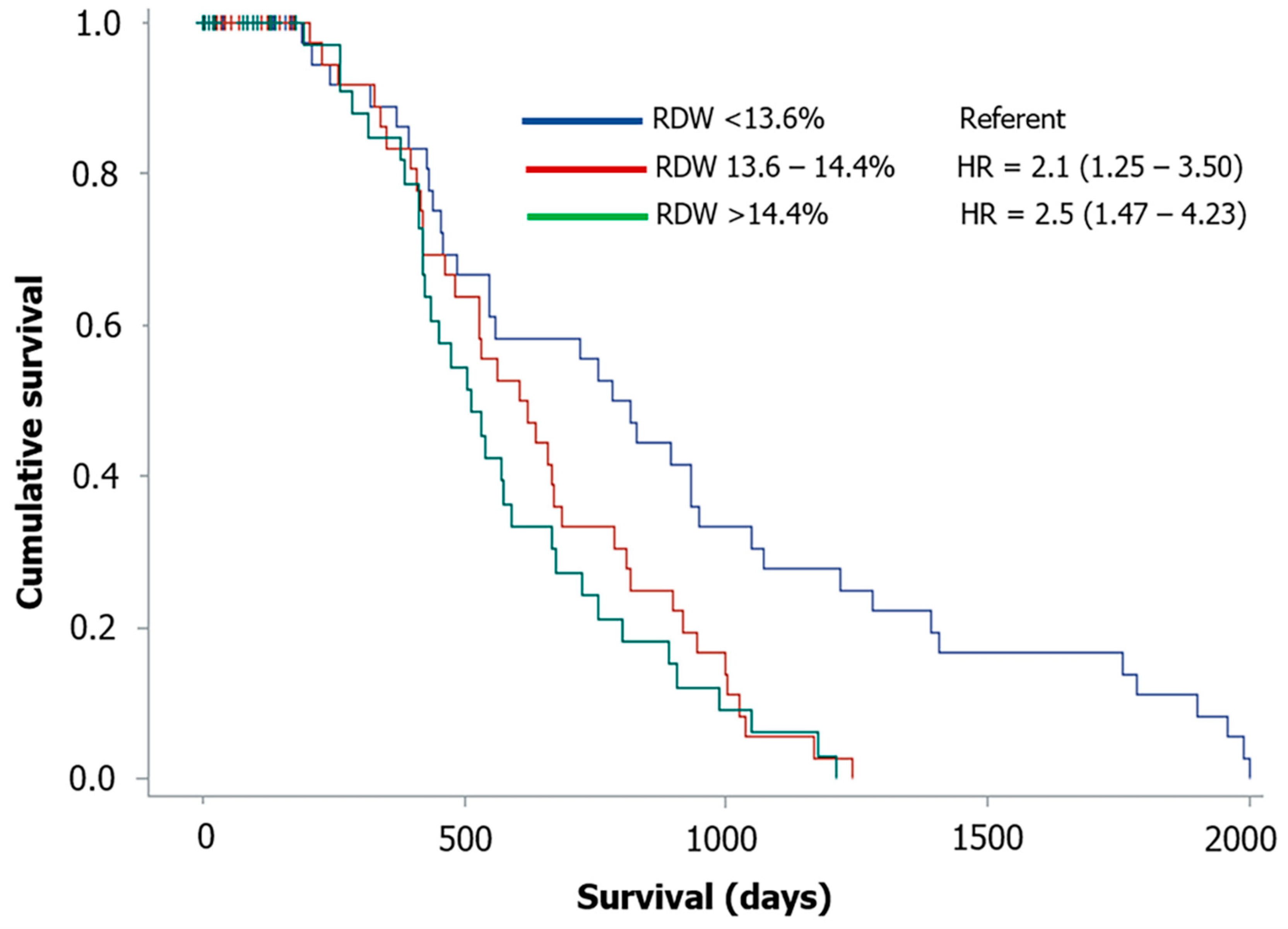
3.3. Correlation and Survival Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Therapy/Drugs | Number (%) |
|---|---|
| Cardiac treatment | 47 (32.2) |
| Loop diuretics | 36 (24.7) |
| ACE-Is | 32 (21.9) |
| Pimobendan | 26 (17.8) |
| Spironolactone | 7 (4.8) |
| Digoxin | 1 (0.7) |
| Mixed treatment | 13 (8.9) |
| ACE-Is | 10 (6.8) |
| Pimobendan | 6 (4.1) |
| Loop diuretics | 6 (4.1) |
| Steroids | 6 (4.1) |
| Antibiotics | 2 (1.4) |
| Anticonvulsants | 2 (1.4) |
| Hepatoprotective drugs | 2 (1.4) |
| NSAIDs | 1 (0.7) |
| Antacids-Antiemetics | 1 (0.7) |
| Vitamins-Other supplements | 1 (0.7) |
| Other treatments | 21 (14.4) |
| Antibiotics | 4 (2.7) |
| Anticonvulsants | 4 (2.7) |
| Steroids | 2 (1.4) |
| Antacids-Antiemetics | 2 (1.4) |
| Propentofylline | 2 (1.4) |
| Levothyroxine | 2 (1.4) |
| Hepatoprotective drugs | 2 (1.4) |
| NSAIDs | 1 (0.7) |
| Gabapentin | 1 (0.7) |
| Trilostane | 1 (0.7) |
| Vitamins-Other supplements | 1 (0.7) |
| Antiandrogen | 1 (0.7) |
| Phenylpropanolamine | 1 (0.7) |
| No therapy | 65 (44.5) |
References
- Lippi, G.; Plebani, M. Red blood cell distribution width (RDW) and human pathology. One size fits all. Clin. Chem. Lab. Med. 2014, 52, 1247–1249. [Google Scholar] [CrossRef] [PubMed]
- Salvagno, G.L.; Sanchis-Gomar, F.; Picanza, A.; Lippi, G. Red blood cell distribution width: A simple parameter with multiple clinical applications. Crit. Rev. Clin. Lab. Sci. 2015, 52, 86–105. [Google Scholar] [CrossRef]
- Neiger, R.; Hadley, J.; Pfeiffer, D.U. Differentiation of dogs with regenerative and non-regenerative anaemia on the basis of their red cell distribution width and mean corpuscular volume. Vet. Rec. 2002, 150, 431–434. [Google Scholar] [CrossRef] [PubMed]
- Hodges, J.; Christopher, M.M. Diagnostic accuracy of using erythrocyte indices and polychromasia to identify regenerative anemia in dogs. J. Am. Vet. Med. Assoc. 2011, 238, 1452–1458. [Google Scholar] [CrossRef]
- Felker, G.M.; Allen, L.A.; Pocock, S.J.; Shaw, L.K.; McMurray, J.J.; Pfeffer, M.A.; Swedberg, K.; Wang, D.; Yusuf, S.; Michelson, E.L.; et al. Red cell distribution width as a novel prognostic marker in heart failure: Data from the CHARM Program and the Duke Databank. J. Am. Coll. Cardiol. 2007, 50, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Förhécz, Z.; Gombos, T.; Borgulya, G.; Pozsonyi, Z.; Prohàszka, Z.; Jànoskuti, L. Red cell distribution width in heart failure: Prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. Am. Heart J. 2009, 158, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.A.; Felker, G.M.; Mehra, M.R.; Chiong, J.R.; Dunlap, S.H.; Ghali, J.K.; Lenihan, D.J.; Oren, R.M.; Wagoner, L.E.; Schwartz, T.A.; et al. Validation and Potential Mechanisms of Red Cell Distribution Width as a Prognostic Marker in Heart Failure. J. Card. Fail. 2010, 16, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Al-Najjar, Y.; Goode, K.M.; Zhang, J.; Cleland, J.G.F.; Clark, A.L. Red cell distribution width: An inexpensive and powerful marker in heart failure. Eur. J. Heart Fail. 2009, 11, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Arbel, Y.; Weitzman, D.; Raz, R.; Steinvil, A.; Zeltser, D.; Berliner, S.; Chodick, G.; Shalev, V. Red blood cell distribution width and the risk of cardiovascular morbidity and all-cause mortality. A population-based study. Thromb. Haemost. 2014, 111, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Danese, E.; Lippi, G.; Montagnana, M. Red blood cell distribution width and cardiovascular diseases. J. Thorac. Dis. 2015, 7, E402–E411. [Google Scholar] [CrossRef] [PubMed]
- Guglielmini, C.; Poser, H.; Dalla Pria, A.; Drigo, M.; Mazzotta, E.; Berlanda, M.; Luciani, A. Red blood cell distribution width in dogs with chronic degenerative valvular disease. J. Am. Vet. Med. Assoc. 2013, 243, 858–862. [Google Scholar] [CrossRef] [PubMed]
- Swann, J.W.; Sudunagunta, S.; Covey, H.L.; English, K.; Hendricks, A.; Connolly, D.J. Evaluation of red cell distribution width in dogs with pulmonary hypertension. J. Vet. Cardiol. 2014, 16, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Mazzotta, E.; Guglielmini, C.; Menciotti, G.; Contiero, B.; BaronToaldo, M.; Berlanda, M.; Poser, H. Red blood cell distribution width, hematology, and serum biochemistry in dogs with echocardiographically estimated precapillary and postcapillary pulmonary arterial hypertension. J. Vet. Intern. Med. 2016, 30, 1806–1815. [Google Scholar] [CrossRef] [PubMed]
- Fish, E.J.; Hansen, S.C.; Spangler, E.A.; Gaillard, P.R.; Fan, S.; Bacek, L.M. Retrospective evaluation of serum/plasma iron, red blood cell distribution width, and nucleated red blood cells in dogs with acute trauma (2009–2015): 129 cases. J. Vet. Emerg. Crit. Care 2019, 29, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Martinez, C.; Mooney, C.T.; Shiel, R.E.; Tang, P.K.; Mooney, L.; O’Neill, E.J. Evaluation of red blood cell distribution width in dogs with various illnesses. Can. Vet. J. 2019, 60, 964–971. [Google Scholar] [PubMed]
- Su-Jung, K.; Sang, S., II; Changbaig, H. Evaluation of red blood cell profiles in dogs with heartworm disease. Can. J. Vet. Res. 2020, 84, 265–271. [Google Scholar]
- Thomas, W.P.; Gaber, C.E.; Jacobs, G.J.; Kaplan, P.M.; Lombard, C.W.; Moise, N.S.; Moses, B.L. Recommendations for standards in transthoracic two-dimensional echocardiography in the dog and cat. Echocardiography Committee of the Specialty of Cardiology, American College of Veterinary Internal Medicine. J. Vet. Intern. Med. 1993, 7, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Keene, B.W.; Atkins, C.E.; Bonagura, J.D.; Fox, P.R.; Häggström, J.; Fuentes, V.L.; Oyama, M.A.; Rush, J.E.; Stepien, R.; Uechi, M. ACVIM consensus guidelines for the diagnosis and treatment of myxomatous mitral valve disease in dogs. J. Vet. Intern. Med. 2019, 33, 1127–1140. [Google Scholar] [CrossRef]
- Cornell, C.C.; Kittleson, M.D.; Della Torre, P.; Häggström, J.; Lombard, C.W.; Pedersen, H.D.; Vollmar, A.; Wey, A. Allometric scaling of M-mode cardiac measurements in normal adult dogs. J. Vet. Intern. Med. 2004, 18, 311–321. [Google Scholar] [CrossRef]
- Rishniw, M.; Erb, H.N. Evaluation of four 2-dimensional echocardiographic methods of assessing left atrial size in dogs. J. Vet. Intern. Med. 2000, 14, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Hansson, K.; Häggström, J.; Kvart, C.; Lord, P. Left atrial to aortic root indices using two-dimensional and M-mode echocardiography in Cavalier King Charles spaniels with and without left atrial enlargement. Vet. Radiol. Ultrasound. 2002, 43, 568–575. [Google Scholar] [CrossRef]
- Reinero, C.; Visser, L.C.; Kellihan, H.B.; Masseau, I.; Rozanski, E.; Clercx, C.; Williams, K.; Abbott, J.; Borgarelli, M.; Scansen, B.A. ACVIM consensus statement guidelines for the diagnosis, classification, treatment, and monitoring of pulmonary hypertension in dogs. J. Vet. Intern. Med. 2020, 34, 549–573. [Google Scholar] [CrossRef] [PubMed]
- Welles, E.G.; Hall, A.S.; Carpenter, D.M. Canine complete blood counts: A comparison of four in-office instruments with the ADVIA 120 and manual differential counts. Vet. Clin. Pathol. 2009, 38, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Pavesi, S.; Bardi, M.; Pipitone, S. Lack of harmonization of red blood cell distribution width (RDW). Evaluation of four hematological analyzers. Clin. Biochem. 2014, 47, 1100–1103. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.K.; Chan, J.; Cembrowski, G.S.; van Assendelft, O.W. Complete blood count reference interval diagrams derived from NHANES III: Stratification by age, sex, and race. Lab. Hematol. 2004, 10, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.V.; Ferrucci, L.; Ershler, W.B.; Longo, D.L.; Guralnik, J.M. Red blood cell distribution width and the risk of death in middle-aged and older adults. Arch. Intern. Med. 2009, 169, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Radakovich, L.B.; Pannone, S.C.; Truelove, M.P.; Olver, C.S.; Santangelo, K.S. Hematology and biochemistry of aging—evidence of “anemia of the elderly” in old dogs. Vet. Clin. Pathol. 2017, 46, 34–45. [Google Scholar] [CrossRef]
- Oh, J.; Kang, S.; Hong, N.; Choi, J.; Lee, S.; Park, S.; Shin, M.; Jang, Y.; Chung, N. Relation between red cell distribution width with echocardiographic parameters in patients with acute heart failure. J. Card. Fail. 2009, 15, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Tonelli, M.; Sacks, F.; Arnold, M.; Moye, L.; Davis, B.; Pfeffer, M. Relation Between Red Blood Cell Distribution Width and Cardiovascular Event Rate in People With Coronary Disease. Circulation 2008, 117, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Borgarelli, M.; Savarino, P.; Crosara, S.; Santilli, R.A.; Chiavegato, D.; Poggi, M.; Bellino, C.; La Rosa, G.; Zanatta, R.; Haggstron, J.; et al. Survival characteristics and prognostic variables of dogs with mitral regurgitation attributable to myxomatous valve disease. J. Vet. Intern. Med. 2008, 22, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Borgarelli, M.; Crosara, S.; Lamb, K.; Savarino, P.; La Rosa, G.; Tarducci, A.; Haggstrom, J. Survival characteristics and prognostic variables of dogs with preclinical chronic degenerative mitral valve disease attributable to myxomatous degeneration. J. Vet. Intern. Med. 2012, 26, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Moonmart, W.; Boswood, A.; Luis Fuentes, V.; Brodbelt, D.; Souttar, K.; Elliott, J. N-terminal pro B-type natriuretic peptide and left ventricular diameter independently predict mortality in dogs with mitral valve disease. J. Small Anim. Pract. 2010, 51, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Hezzell, M.J.; Boswood, A.; Chang, Y.M.; Moonarmart, W.; Souttar, K.; Elliott, J. The combined prognostic potential of serum high-sensitivity cardiac troponin I and N-terminal pro-B-type natriuretic peptide concentrations in dogs with degenerative mitral valve disease. J. Vet. Intern. Med. 2012, 26, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Hezzell, M.J.; Boswood, A.; Moonarmart, W.; Elliott, J. Selected echocardiographic variables change more rapidly in dogs that die from myxomatous mitral valve disease. J. Vet. Cardiol. 2012, 14, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Borgarelli, M.; Abbott, J.; Braz-Ruivo, L.; Chiavegato, D.; Crosara, S.; Lamb, K.; Ljungvall, I.; Poggi, M.; Santilli, R.A.; Haggstrom, J. Prevalence and prognostic importance of pulmonary hypertension in dogs with myxomatous mitral valve disease. J. Vet. Intern. Med. 2015, 29, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Sargent, J.; Muzzi, R.; Mukherjee, R.; Somarathne, S.; Schranz, K.; Stephenson, H.; Connolly, D.; Brodbelt, D.; Luis Fuentes, V. Echocardiographic predictors of survival in dogs with myxomatous mitral valve disease. J. Vet. Cardiol. 2015, 17, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.W.; Sun, W.; Griffiths, L.G.; Kittleson, M.D. Atrial fibrillation as a prognostic indicator in medium to large- sized dogs with myxomatous mitral valvular degeneration and congestive heart failure. J. Vet. Intern. Med. 2016, 30, 51–57. [Google Scholar] [CrossRef]
- Kim, H.T.; Han, S.M.; Song, W.J.; Kim, B.; Choi, M.; Yoon, J.; Youn, H.Y. Retrospective study of degenerative mitral valve disease in small-breed dogs: Survival and prognostic variables. J. Vet. Sci. 2017, 18, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Baron Toaldo, M.; Romito, G.; Guglielmini, C.; Diana, A.; Pelle, N.G.; Contiero, B.; Cipone, M. Prognostic value of echocardiographic indices of left atrial morphology and function in dogs with myxomatous mitral valve disease. J. Vet. Intern. Med. 2018, 32, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Guglielmini, C.; Baron Toaldo, M.; Chiesa, A.; Contiero, B.; Berlanda, M.; Poser, H. Effect of temperature variation on hospital admissions and outcomes in dogs with myxomatous mitral valve disease and new onset pulmonary edema. PLoS ONE 2020, 15, e0227807. [Google Scholar] [CrossRef] [PubMed]
- Guglielmini, C.; Sousa, M.G.; Baron Toaldo, M.; Valente, C.; Bentivoglio, V.; Mazzoldi, C.; Bergamin, I.; Drigo, M.; Poser, H. Prevalence and risk factors for atrial fibrillation in dogs with myxomatous mitral valve disease. J. Vet. Intern. Med. 2020, 34, 2223–2231. [Google Scholar] [CrossRef] [PubMed]
- Petric, A.D.; Lukman, T.; Verk, B.; Svete, A.N. Systemic inflammation in dogs with advanced-stage heart failure. Acta. Vet. Scand. 2018, 60, 20. [Google Scholar] [CrossRef] [PubMed]
- Farabaugh, A.E.; Freeman, L.M.; Rush, J.E.; George, K.L. Lymphocyte subpopulations and hematologic variables in dogs with congestive heart failure. J. Vet. Intern. Med. 2004, 18, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Hamilton-Elliot, J.; Ambrose, E.; Christley, E.; Dukes-McEwan, J. White blood cell differentials in dogs with congestive heart failure (CHF) in comparison to those in dogs without cardiac disease. J. Small Anim. Pract. 2018, 59, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Nicolle, A.P.; Chetoboul, V.; Allerheiligen, T.; Pouchelon, J.; Gouni, V.; Tessier-Vetzel, D.; Sampedrano, C.C.; Lefebvre, H.P. Azotemia and glomerular filtration rate in dogs with chronic valvular disease. J. Vet. Intern. Med. 2007, 21, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Valente, C.; Guglielmini, C.; Domenech, O.; Contiero, B.; Zini, E.; Poser, H. Symmetric dimethylarginine in dogs with myxomatous mitral valve disease at various stages of disease severity. PLoS ONE 2020, 15, e0238440. [Google Scholar] [CrossRef]
- Martinelli, E.; Locatelli, C.; Bassis, S.; Crosara, S.; Paltrinieri, S.; Scarpa, P.; Spalla, I.; Zanaboni, A.M.; Quintavalla, C.; Brambilla, P. Preliminary Investigation of Cardiovascular-Renal Disorders in Dogs with Chronic Mitral Valve Disease. J. Vet. Intern. Med. 2016, 30, 1612–1618. [Google Scholar] [CrossRef] [PubMed]
- Ineson, D.L.; Freeman, L.M.; Rush, J.E. Clinical and laboratory findings and survival time associated with cardiac cachexia in dogs with congestive heart failure. J. Vet. Intern. Med. 2019, 33, 1902–1908. [Google Scholar] [CrossRef] [PubMed]
- Freeman, L.M.; Rush, J.E.; Milbury, P.E.; Blumberg, J.B. Antioxidant status and biomarkers of oxidative stress in dogs with congestive heart failure. J. Vet. Intern. Med. 2005, 19, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Reimann, M.J.; Häggström, J.; Møller, J.E.; Lykkesfeldt, J.; Falk, T.; Olsen, L.H. Markers of oxidative stress in dogs with myxomatous mitral valve disease are influenced by sex, neuter status, and serum cholesterol concentration. J. Vet. Intern. Med. 2017, 31, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Rubio, C.P.; Saril, A.; Kocaturk, M.; Tanaka, R.; Koch, J.; Ceron, J.J.; Yilmaz, Z. Changes of inflammatory and oxidative stress biomarkers in dogs with different stages of heart failure. BMC Vet. Res. 2020, 16, 433. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total Cohort (n = 146) | Dead by 6 Months (n = 41) | Alive at 6 Months (n = 105) | p-Value |
|---|---|---|---|---|
| Age (month) | 143 ± 35 | 152 ± 32 | 140 ± 36 | 0.057 |
| Weight (kg) | 9 (2–38) | 8 (2–38) | 9 (2–3) | 0.979 |
| Sex (F/M) | 58/88 | 19/22 | 39/66 | 0.410 |
| Pure breed (n [%]) | 62 (42.5) | 22 (53.7) | 40 (38.1) | 0.128 |
| No treatment (n [%]) | 56 (38.4) | 8 (19.5) | 48 (45.7) | 0.002 |
| Cardiac treatment (n [%]) | 44 (30.1) | 16 (39.0) | 28 (26.7) | 0.223 |
| Mixed treatment/disease (n [%]) | 16 (11.0) | 7 (17.1) | 9 (8.6) | 0.294 |
| Other treatment/disease (n [%]) | 30 (20.5) | 10 (24.4) | 20 (19.0) | 0.637 |
| ACVIM stage C + D (n [%]) | 51 (34.9) | 20 (48.8) | 31 (29.5) | 0.051 |
| AF (n [%]) | 5 (3.4) | 2 (4.9) | 3 (2.9) | 0.458 |
| PH (n [%]) | 18 (12.3) | 6 (14.6) | 12 (11.4) | 0.812 |
| Urea (mg/dL) | 43 (16–202) | 60 (21–202) | 40 (16–138) | 0.001 |
| Total protein (g/L) | 71.4 ± 7.8 | 70.3 ± 9.8 | 71.9 ± 6.9 | 0.266 |
| Albumin (g/L) | 29.7 ± 4.8 | 29.1 ± 5.8 | 30.3 ± 3.6 | 0.137 |
| Creatinine (mg/dL) | 1.05 (0.57–3.02) | 1.09 (0.57–2.39) | 1.05 (0.60–3.02) | 0.318 |
| WBC (103/μL) | 11.42 (4.85–48.54) | 14.02 (6.05–48.54) | 9.92 (4.85–39.31) | <0.001 |
| RBC (106/μL) | 6.92 ± 1.01 | 6.96 ± 1.26 | 6.9 ± 0.9 | 0.737 |
| Hemoglobin (g/dL) | 16.2 ± 2.4 | 16.3 ± 2.9 | 16.1 ± 2.1 | 0.667 |
| Hematocrit (%) | 46.2 ± 6.8 | 46.7 ± 8.5 | 46.0 ± 6.1 | 0.606 |
| RDW (%) | 14.0 (12.1–21.8) | 14.0 (12.2–18.9) | 13.9 (12.1–21.8) | 0.708 |
| MCV (fL) | 67.0 ± 4.3 | 67.4 ± 4.8 | 66.8 ± 4.2 | 0.499 |
| Platelet (103/μL) | 361.2 ± 135.6 | 344.7 ± 149.2 | 367.6 ± 130.0 | 0.361 |
| LA/Ao | 2.07 ± 0.68 | 2.33 ± 0.67 | 1.97 ± 0.66 | 0.004 |
| LVDDn | 1.76 ± 0.37 | 1.83 ± 0.4 | 1.74 ± 0.36 | 0.219 |
| LVSDn | 0.98 ± 0.22 | 0.99 ± 0.24 | 0.97 ± 0.21 | 0.651 |
| FS (%) | 41.9 ± 9.6 | 42.1 ± 11.9 | 41.8 ± 8.6 | 0.875 |
| E-max (cm/s) | 104.0 ± 40.0 | 115.6 ± 37.9 | 99.3 ± 40.1 | 0.027 |
| TR Vmax (m/s) | 2.72 ± 0.73 | 2.89 ± 0.8 | 2.66 ± 0.69 | 0.115 |
| Variable | RDW | p-Value | Survival (d) | p-Value |
|---|---|---|---|---|
| Age (month) | 0.206 | 0.013 | −0.261 | 0.002 |
| Weight (kg) | 0.091 | 0.275 | −0.092 | 0.268 |
| Sex—Male | −0.047 | 0.575 | 0.039 | 0.638 |
| Breed—Pure breed | 0.059 | 0.480 | −0.041 | 0.623 |
| Cardiac treatment Vs. No Treatment | 0.159 | 0.113 | −0.359 | <0.001 |
| Mixed treatment/disease Vs. No Treatment | 0.087 | 0.468 | −0.301 | 0.010 |
| Other treatment/disease Vs. No treatment | 0.075 | 0.494 | −0.151 | 0.164 |
| ACVIM stage C + D | −0.211 | 0.011 | −0.265 | 0.001 |
| AF | 0.031 | 0.707 | −0.123 | 0.139 |
| PH | 0.101 | 0.226 | −0.122 | 0.142 |
| Urea (mg/dL) | 0.109 | 0.191 | −0.342 | < 0.001 |
| Total protein (g/L) | 0.188 | 0.024 | 0.082 | 0.326 |
| Albumin (g/L) | 0.007 | 0.936 | 0.142 | 0.087 |
| Creatinine (mg/dL) | 0.031 | 0.712 | −0.135 | 0.105 |
| WBC (103/μL) | −0.056 | 0.499 | −0.388 | <0.001 |
| RBC (106/μL) | −0.193 | 0.020 | 0.054 | 0.516 |
| Hemoglobin (g/dL) | −0.329 | < 0.001 | 0.051 | 0.540 |
| Hematocrit (%) | −0.322 | < 0.001 | 0.061 | 0.462 |
| RDW (%) | NA | NA | −0.171 | 0.040 |
| MCV (fL) | −0.277 | 0.001 | 0.030 | 0.718 |
| Platelet (103/μL) | 0.119 | 0.152 | −0.035 | 0.677 |
| LA/Ao | −0.123 | 0.138 | −0.352 | < 0.001 |
| LVDDn | −0.246 | 0.003 | −0.175 | 0.034 |
| LVSDn | −0.163 | 0.050 | −0.144 | 0.082 |
| FS (%) | −0.024 | 0.778 | −0.015 | 0.861 |
| E-max (cm/s) | −0.087 | 0.300 | −0.282 | 0.001 |
| TR Vmax (m/s) | 0.094 | 0.306 | −0.249 | 0.006 |
| Survival (d) | −0.171 | 0.040 | NA | NA |
| Predictors | Hazard Ratio | 95% CI | Chi Square | p-Value |
|---|---|---|---|---|
| Age (months) | 1.008 | 1.002–1.013 | 7.960 | 0.005 |
| Weight (kg) | 1.028 | 0.999.0–1.057 | 3.514 | 0.061 |
| Sex—Male | 1.152 | 0.770–1.724 | 0.474 | 0.491 |
| Breed—Pure breed | 0.815 | 0.547–1.213 | 1.016 | 0.313 |
| Cardiac treatment Vs. No Treatment | 2.001 | 1.235–3.241 | 7.946 | 0.005 |
| Mixed treatment/disease Vs. No Treatment | 1.828 | 0.886–3.770 | 2.667 | 0.1024 |
| Other treatment/disease Vs. No Treatment | 0.989 | 0.583–1.678 | 0.002 | 0.966 |
| ACVIM stage C + D | 1.870 | 1.212–2.886 | 7.999 | 0.005 |
| AF | 3.896 | 1.213–12.514 | 5.218 | 0.022 |
| PH | 1.876 | 0.998–3.526 | 3.813 | 0.051 |
| Urea (mg/dL) | 1.017 | 1.007–1.026 | 11.893 | <0.001 |
| Total protein (g/L) | 1.016 | 0.988–1.046 | 1.246 | 0.264 |
| Albumin (g/L) | 1.044 | 0.986–1.105 | 2.209 | 0.137 |
| Creatinine (mg/dL) | 1.600 | 0.989–2.589 | 3.666 | 0.055 |
| WBC (103/μL) | 1.043 | 1.007–1.080 | 5.527 | 0.019 |
| RBC (106/μL) | 0.927 | 0.744–1.155 | 0.458 | 0.498 |
| Hemoglobin (g/dL) | 0.960 | 0.873–1.055 | 0.733 | 0.392 |
| Hematocrit (%) | 0.980 | 0.948–1.012 | 1.529 | 0.216 |
| RDW (%) | 1.245 | 1.103–1.405 | 12.609 | <0.001 |
| MCV (fL) | 0.971 | 0.925–1.019 | 1.419 | 0.234 |
| Platelet (103/μL) | 1.001 | 1.000–1.002 | 1.913 | 0.167 |
| LA/Ao | 2.108 | 1.488–2.987 | 17.582 | <0.001 |
| LVDDn | 2.053 | 1.115–3.779 | 5.330 | 0.021 |
| LVSDn | 2.949 | 1.182–7.353 | 5.380 | 0.020 |
| FS (%) | 0.998 | 0.977–1.021 | 0.022 | 0.883 |
| E-max (cm/s) | 1.008 | 1.003–1.014 | 8.802 | 0.003 |
| TR Vmax (m/s) | 1.559 | 1.117–2.177 | 6.797 | 0.009 |
| Predictors | Hazard Ratio | 95% CI | Chi Square | p-Value |
|---|---|---|---|---|
| Urea (mg/dL) | 1.016 | 1.005–1.026 | 9.000 | 0.003 |
| WBC (103/μL) | 1.043 | 1.004–1.083 | 4.734 | 0.030 |
| RDW (%) | 1.203 | 1.045–1.384 | 6.624 | 0.010 |
| LA/Ao | 1.892 | 1.232–2.905 | 8.478 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guglielmini, C.; Valentini, C.M.; Contiero, B.; Valente, C.; Poser, H. Red Cell Distribution Width Has a Negative Prognostic Role in Dogs with Myxomatous Mitral Valve Disease. Animals 2021, 11, 778. https://doi.org/10.3390/ani11030778
Guglielmini C, Valentini CM, Contiero B, Valente C, Poser H. Red Cell Distribution Width Has a Negative Prognostic Role in Dogs with Myxomatous Mitral Valve Disease. Animals. 2021; 11(3):778. https://doi.org/10.3390/ani11030778
Chicago/Turabian StyleGuglielmini, Carlo, Chiara Martina Valentini, Barbara Contiero, Carlotta Valente, and Helen Poser. 2021. "Red Cell Distribution Width Has a Negative Prognostic Role in Dogs with Myxomatous Mitral Valve Disease" Animals 11, no. 3: 778. https://doi.org/10.3390/ani11030778
APA StyleGuglielmini, C., Valentini, C. M., Contiero, B., Valente, C., & Poser, H. (2021). Red Cell Distribution Width Has a Negative Prognostic Role in Dogs with Myxomatous Mitral Valve Disease. Animals, 11(3), 778. https://doi.org/10.3390/ani11030778








