Aquaporin 1 (AQP1) Expression in Healthy Dog Tears
Abstract
Simple Summary
Abstract
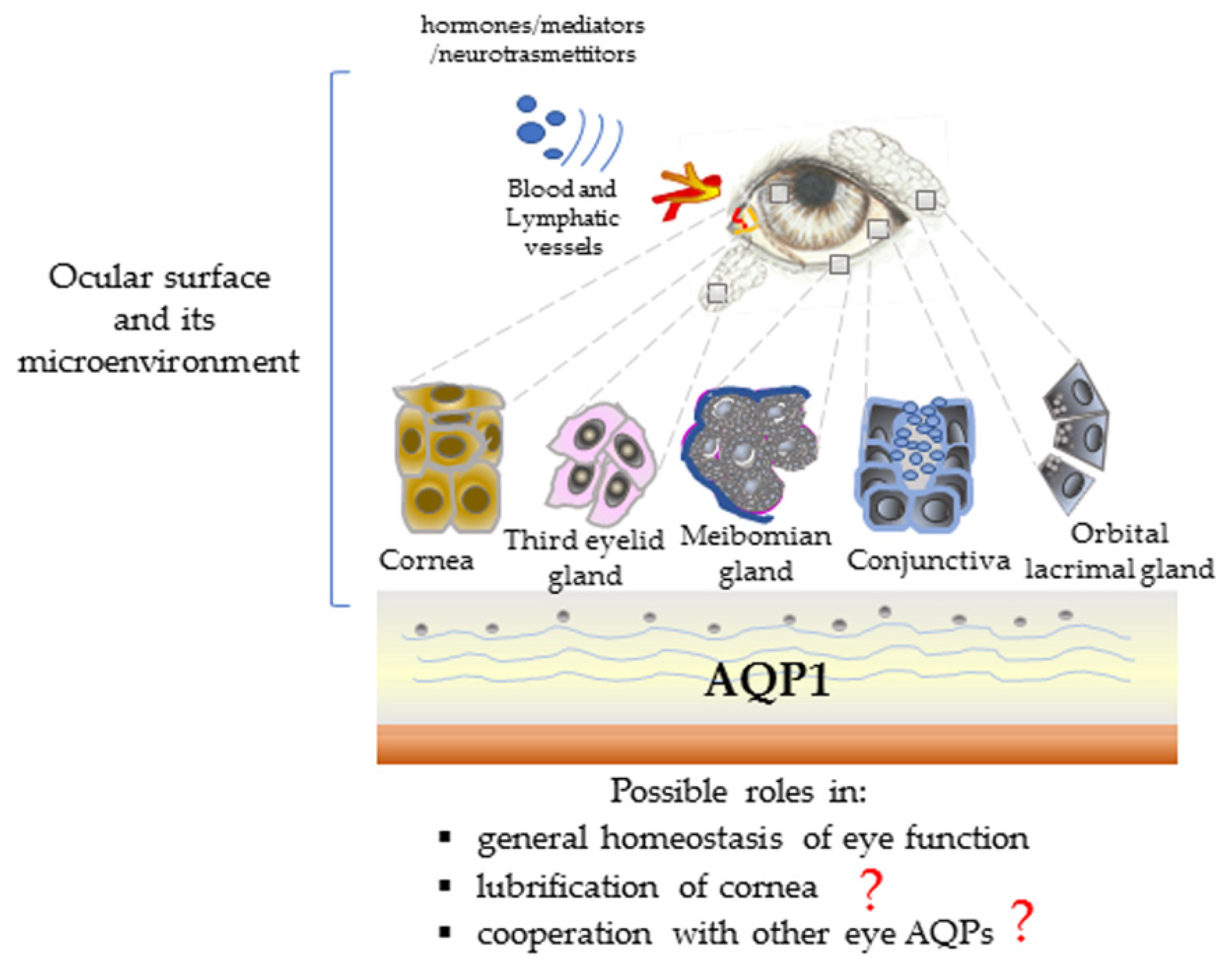
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Experimental Protocol
2.3. Complete Blood Count and Serum Biochemistry
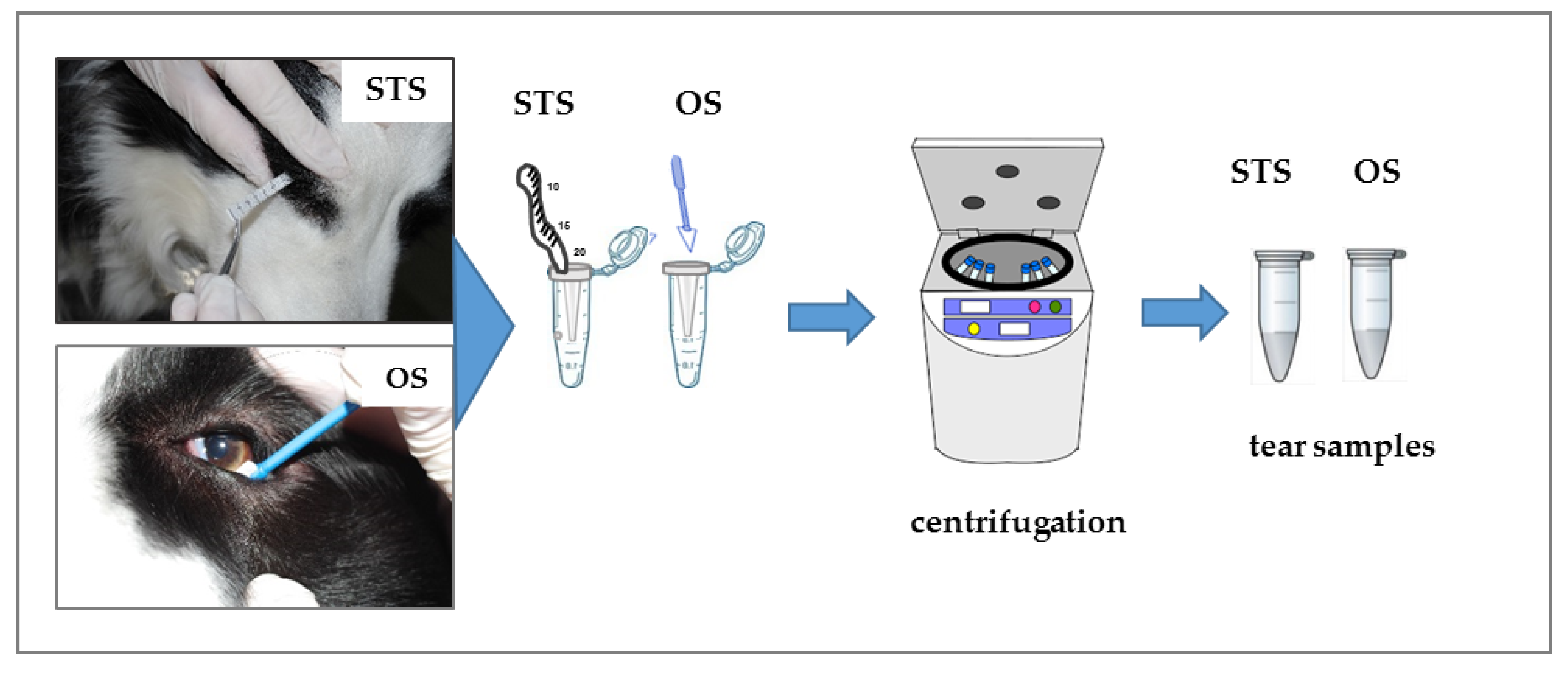
2.4. Tear Sample Collection
2.5. Tear Protein Analysis
2.6. AQP1 Expression in Tears by Western Blotting
2.7. Statistical Analysis
3. Results
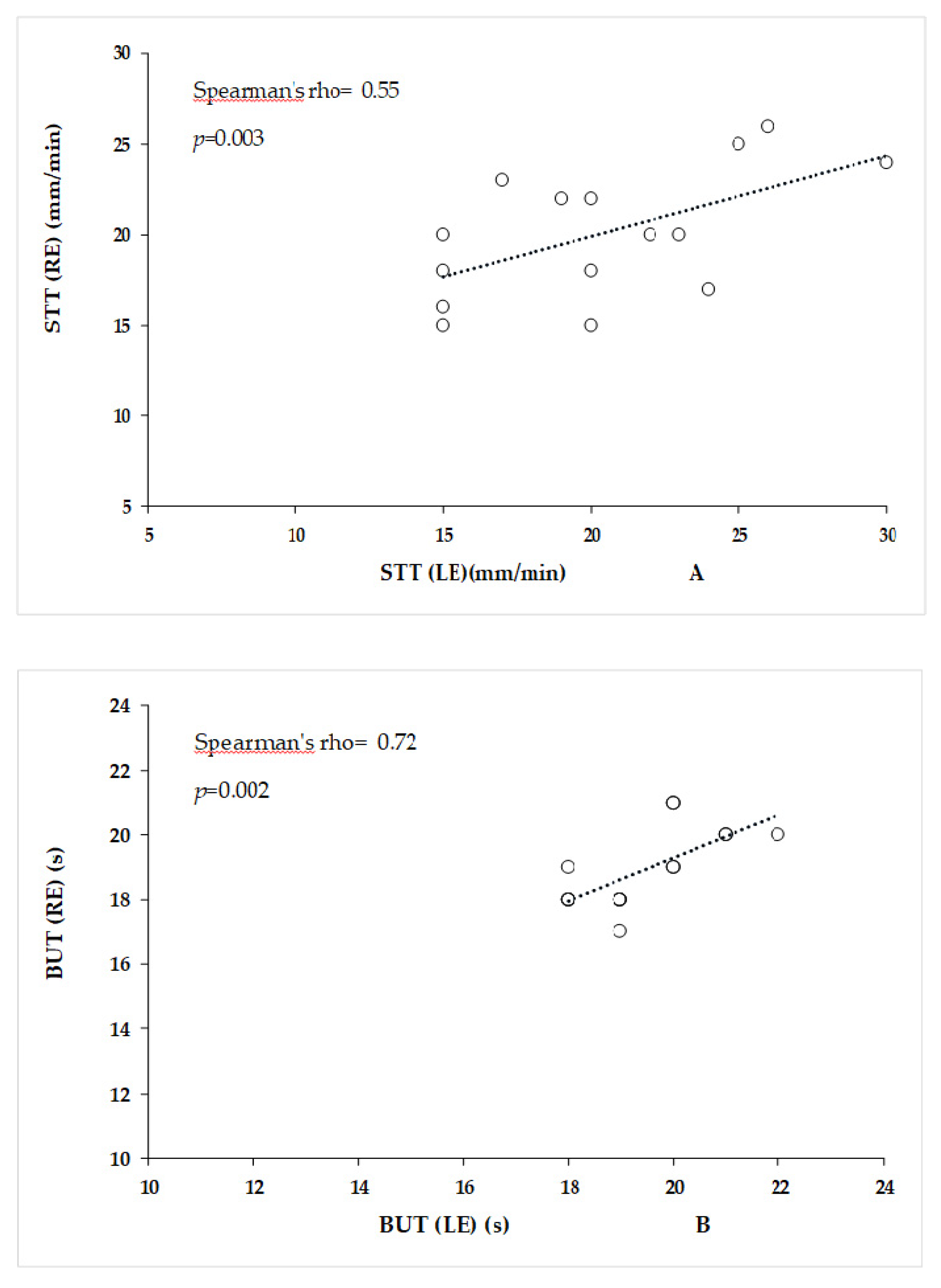
3.1. Ocular Parameters
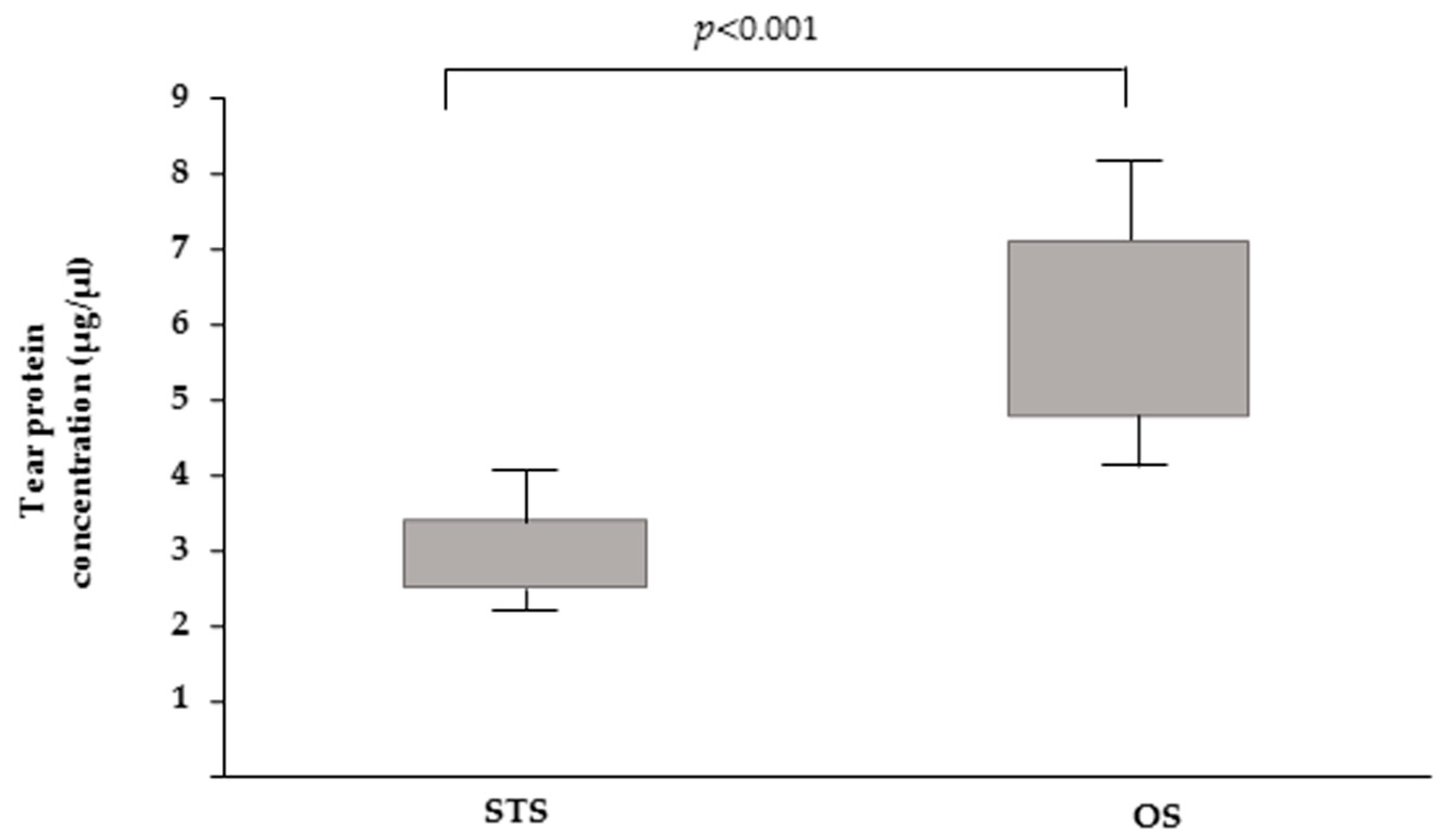
3.2. Analysis of Dog Tear Parameters (Volume and Total Protein Content)
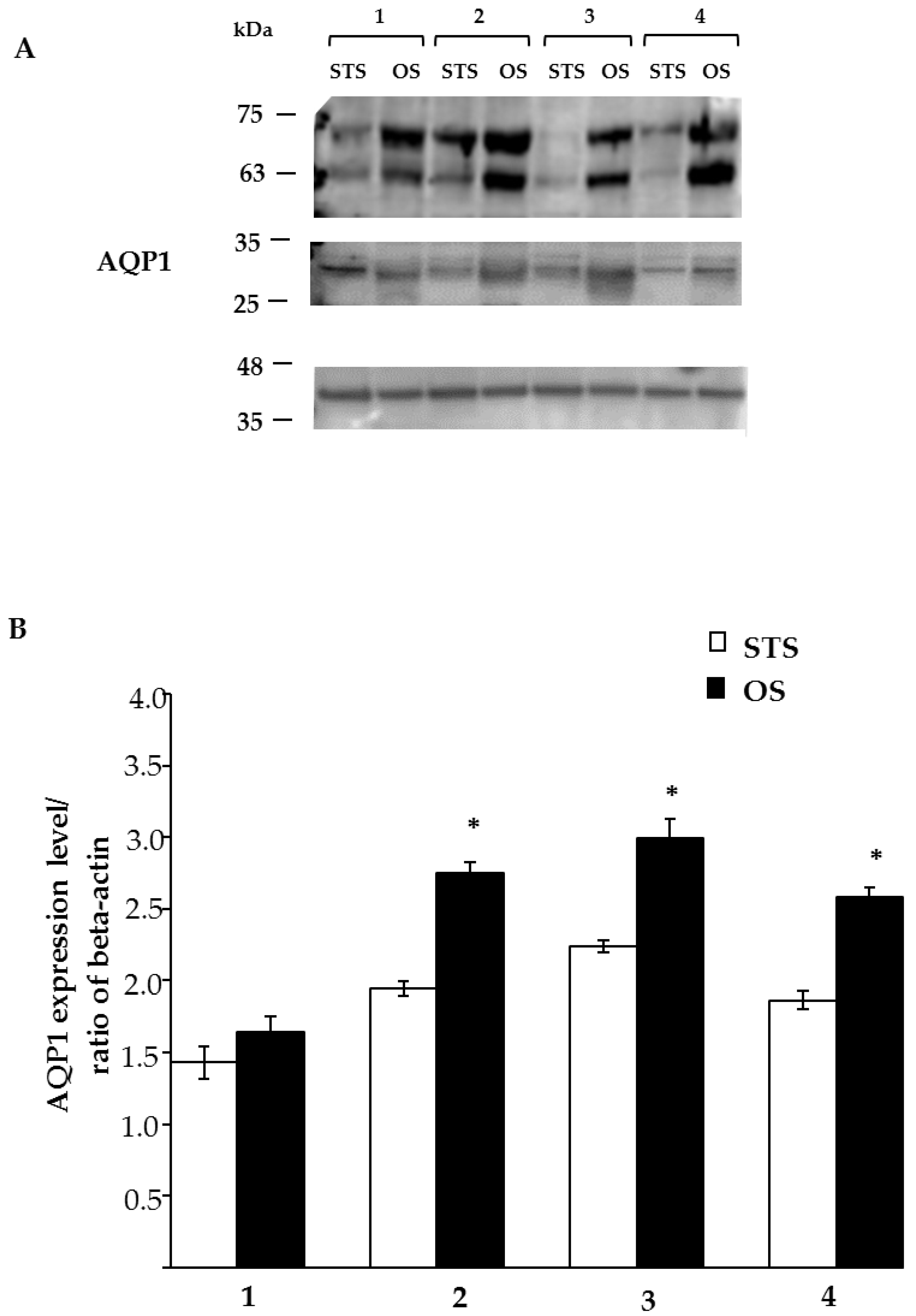
3.3. AQP1 Expression by Western Blotting
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Menaka, R.; Puri, G. Role of Lacrimal Gland in Tear Production in Different Animal Species: A Review. Livest. Res. Int. 2015, 3, 40–42. [Google Scholar]
- Walcott, B. The Lacrimal Gland and Its Veil of Tears. News Physiol. Sci. 1998, 13, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Conrady, C.D.; Joos, Z.P.; Patel, B.C.K. Lacrimal gland and its role in dry eye. J. Ophthalmol. 2016, 7542929. [Google Scholar] [CrossRef]
- Davidson, A.J.; Kuonen, V.J. The tear film and ocular mucins. Vet. Opthalmol. 2004, 7, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.; Ma, T.; Yang, B.; Verkman, A.S. Tear Secretion by Lacrimal Glands in Transgenic Mice Lacking Water Channels AQP1, AQP3, AQP4 and AQP5. Exp. Eye Res. 2000, 70, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Dartt, D.A. The Dry Eye; Lemp, M.A., Marquardt, R., Eds.; SpringerVerlag: Berlin, Germany, 1992; pp. 65–99. [Google Scholar]
- Li, C.; Wang, W. Molecular Biology of Aquaporins. Adv. Exp. Med. Biol. 2017, 969, 1–34. [Google Scholar] [CrossRef]
- Gorin, M.B.; Yancey, S.; Cline, J.; Revel, J.-P.; Horwitz, J. The major intrinsic protein (MIP) of the bovine lens fiber membrane: Characterization and structure based on cDNA cloning. Cell 1984, 39, 49–59. [Google Scholar] [CrossRef]
- Varadaraj, K.; Kumari, S.; Shiels, A.; Mathias, R.T. Regulation of Aquaporin Water Permeability in the Lens. Investig. Opthalmology Vis. Sci. 2005, 46, 1393–1402. [Google Scholar] [CrossRef]
- Kumari, S.S.; Varadaraj, K. Intact AQP0 performs cell-to-cell adhesion. Biochem. Biophys. Res. Commun. 2009, 390, 1034–1039. [Google Scholar] [CrossRef]
- Varadaraj, K.; Kumari, S.S.; Mathias, R.T. Transgenic expression of AQP1 in the fiber cells of AQP0 knockout mouse: Effects on lens transparency. Exp. Eye Res. 2010, 91, 393–404. [Google Scholar] [CrossRef]
- Schey, K.L.; Wang, Z.L.; Wenke, J.; Qi, Y. Aquaporins in the eye: Expression, function, and roles in ocular disease. Biochim. Biophys. Acta 2014, 1840, 1513–1523. [Google Scholar] [CrossRef] [PubMed]
- Patil, R.; Wang, H.; Sharif, N.A.; Mitra, A. Aquaporins: Novel Targets for Age-Related Ocular Disorders. J. Ocul. Pharmacol. Ther. 2018, 34, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Schey, K.L.; Petrova, R.; Gletten, R.B.; Donaldson, P.J. The Role of Aquaporins in Ocular Lens Homeostasis. Int. J. Mol. Sci. 2017, 18, 2693. [Google Scholar] [CrossRef] [PubMed]
- Ishida, N.; Hirai, S.-I.; Mita, S. Immunolocalization of Aquaporin Homologs in Mouse Lacrimal Glands. Biochem. Biophys. Res. Commun. 1997, 238, 891–895. [Google Scholar] [CrossRef] [PubMed]
- Funaki, H.; Yamamoto, T.; Koyama, Y.; Kondo, D.; Yaoita, E.; Kawasaki, K.; Kobayashi, H.; Sawaguchi, S.; Abe, H.; Kihara, I. Localization and expression of AQP5 in cornea, serous salivary glands, and pulmonary epithelial cells. Am. J. Physiol. Content 1998, 275, C1151–C1157. [Google Scholar] [CrossRef]
- Hamann, S.; Zeuthen, T.; La Cour, M.; Nagelhus, E.A.; Ottersen, O.P.; Agre, P.; Nielsen, S. Aquaporins in complex tissues: Distribution of aquaporins 1–5 in human and rat eye. Am. J. Physiol. 1998, 274, C1332–C1345. [Google Scholar] [CrossRef]
- Yu, D.; Thelin, W.R.; Randell, S.H.; Boucher, R.C. Expression profiles of aquaporins in rat conjunctiva, cornea, lacrimal gland and Meibomian gland. Exp. Eye Res. 2012, 103, 22–32. [Google Scholar] [CrossRef]
- Thiagarajah, J.R.; Verkman, A.S. Aquaporin Deletion in Mice Reduces Corneal Water Permeability and Delays Restoration of Transparency after Swelling. J. Boil. Chem. 2002, 277, 19139–19144. [Google Scholar] [CrossRef]
- Wu, J.; Bell, O.H.; Copland, D.A.; Young, A.; Pooley, J.R.; Maswood, R.; Evans, R.S.; Khaw, P.T.; Ali, R.R.; Dick, A.D.; et al. Gene Therapy for Glaucoma by Ciliary Body Aquaporin 1 Disruption Using CRISPR-Cas9. Mol. Ther. 2020, 28, 820–829. [Google Scholar] [CrossRef]
- Li, Z.; Chen, W.; Zhang, H.; Cui, C. The Aquaporin-1 Depletion Downregulates the Sclera Biomechanical Strength. Curr. Eye Res. 2020, 20, 1–5. [Google Scholar] [CrossRef]
- Broadwater, J.J.; Colitz, C.; Carastro, S.; Saville, W. Tear production in normal juvenile dogs. Vet. Ophthalmol. 2010, 13, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Karasawa, K.; Tanaka, A.; Jung, K.; Matsuda, A.; Okamoto, N.; Oida, K.; Ohmori, K.; Matsuda, H. Patterns of aquaporin expression in the canine eye. Vet. J. 2011, 190, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Dodi, P.L. Immune-medited keratoconjunctivitis sicca in dogs: Current perspectives on management. Vet. Med. 2015, 6, 341–347. [Google Scholar] [CrossRef][Green Version]
- Ollivier, F.J. The precorneal tear film in horses: Its importance and disorders. Vet. Clin. N. Am. Equine Pract. 2004, 20, 301–318. [Google Scholar] [CrossRef] [PubMed]
- Cullen, C.L.; Njaa, B.L.; Grahn, B.H. Ulcerative keratitis associated with qualitative tear film abnormalities in cats. Vet. Ophthalmol. 1999, 2, 197–204. [Google Scholar] [CrossRef]
- Higa, K.; Ochiai, H.; Fujise, H. Molecular cloning and expression of aquaporin 1 (AQP1) in dog kidney and erythroblasts. Biochim. Biophys. Acta (BBA) Biomembr. 2000, 1463, 374–382. [Google Scholar] [CrossRef]
- Ribeiro, A.P.; da Cunha Brito, F.L.; da Costa Martins, B.; Mamede, F.; Laus, J.L. Qualitative and quantitative tear film abnormalities in dogs. Cienc. Rural 2008, 38, 568–575. [Google Scholar] [CrossRef]
- Posa, A.; Bräuera, L.; Schichta, M.; Garreisa, F.; Beileke, S.; Paulsena, F. Schirmer strip vs. capillary tube method: Non-invasive methods of obtaining proteins from tear fluid. Ann. Anat. 2013, 195, 137–142. [Google Scholar] [CrossRef]
- Sebbag, L.; Harrington, D.; Mochel, J. Tear fluid collection in dogs and cats using ophthalmic sponges. Vet. Ophthalmol. 2018, 21, 249–254. [Google Scholar] [CrossRef]
- Bradford, M.M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 1976, 72, 248–254. [Google Scholar] [CrossRef]
- Yaginuma, S.; Akune, Y.; Shigeyasu, C.; Takano, Y.; Yamada, M. Tear protein analysis in presumed congenital alacrima. Clin. Ophthalmol. 2018, 12, 2591–2595. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.M. The Protein Protocols Handbook, 2nd ed.; Humana Press Inc.: Totowa, NJ, USA, 2002. [Google Scholar]
- De Luca, A.; Vassalotti, G.; Pelagalli, A.; Pero, M.E.; Squillacioti, C.; Mirabella, N.; Lombardi, P.; Avallone, L. Expression and localization of aquaporin-1 along the intestine of colostrum suckling buffalo calves. Anat. Histol. Embryol. 2015, 44, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Pelagalli, A.; Squillacioti, C.; De Luca, A.; Pero, M.; Vassalotti, G.; Lombardi, P.; Avallone, L.; Mirabella, N. Expression and Localization of Aquaporin 4 and Aquaporin 5 along the Large Intestine of Colostrum-Suckling Buffalo Calves. Anat. Histol. Embryol. 2015, 45, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Keech, A.; Senchyna, M.; Jones, L. Impact of Time Between Collection and Collection Method on Human Tear Fluid Osmolarity. Curr. Eye Res. 2013, 38, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Verkman, A.S. Role of aquaporin water channels in eye function. Exp. Eye Res. 2003, 76, 137–143. [Google Scholar] [CrossRef]
- Bhattacharya, D.; Ning, Y.; Zhao, F.; Stevenson, W.; Chen, R.; Zhang, J.; Wang, M. Tear Production after Bilateral Main Lacrimal Gland Resection in Rabbits. Invest. Ophthalmol. Vis. Sci. 2015, 56, 7774–7783. [Google Scholar] [CrossRef]
- Kenney, M.C.; Atilano, S.R.; Zorapapel, N.; Holguin, B.; Gaster, R.N.; Ljubimov, A.V. Altered expression of aquaporins in bullous keratopathy and Fuchs’ dystrophy corneas. J. Histochem. Cytochem. 2004, 52, 1341–1350. [Google Scholar] [CrossRef]
- Jäger, K.; Reh, D.; Gebhardt, M.; Schaudig, U.; Sel, S.; Bräuer, L.; Paulsen, F. Expression Profile of Aquaporins in Human Nasolacrimal Duct Epithelium. Curr. Eye Res. 2010, 35, 267–273. [Google Scholar] [CrossRef]
- Verkman, A.S. Aquaporin water channels and endothelial cell function. J. Anat. 2002, 200, 617–627. [Google Scholar] [CrossRef]
- Kuang, K.; Yiming, M.; Wen, Q.; Li, Y.; Ma, L.; Iserovich, P.; Verkman, A.S.; Fischbarg, J. Fluid transport across cultured layers of corneal endothelium from aquaporin-1 null mice. Exp. Eye Res. 2004, 78, 791–798. [Google Scholar] [CrossRef]
- Bogner, B.; Schroedl, F.; Trost, A.; Kaser-Eichberger, A.; Runge, C.; Strohmaier, C.; Motloch, K.A.; Brückner, D.; Hauser-Kronberger, C.; Bauer, H.C.; et al. Aquaporin expression and localization in the rabbit eye. Exp. Eye Res. 2016, 147, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Ederra, J.; Verkman, A.S. Aquaporin-1-facilitated keratocyte migration in cell culture and in vivo corneal wound healing models. Exp. Eye Res. 2009, 89, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Yeo, A.; Kim, T.I.; Seo, K.Y.; Kim, E.K.; Lee, H.K. Comparison of the Effectiveness between Sampling Methods for Protein Analysis of Tear Fluids. J. Korean Opthalmol. Soc. 2015, 56, 1677–1683. [Google Scholar] [CrossRef][Green Version]
- Inic-Kanada, A.; Nussbaumer, A.; Montanaro, J.; Belij, S.; Schlacher, S.; Stein, E.; Bintner, N.; Merio, M.; Zlabinger, G.J.; Barisani-Asenbauer, T. Comparison of ophthalmic sponges and extraction buffers for quantifying cytokine profiles in tears using Luminex technology. Mol. Vis. 2012, 18, 2717–2725. [Google Scholar] [PubMed]
- van Agtmaal, E.J.; van Haeringen, N.J.; Bloem, M.W.; Schreurs, W.H.; Saowakontha, S. Recovery of protein from tear fluid stored in cellulose sponges. Curr. Eye Res. 1987, 6, 585–588. [Google Scholar] [CrossRef]
- Tuft, S.J.; Dart, J.K. The measurement of IgE in tear fluid: A comparison of collection by sponge or capillary. Acta Ophthalmol. 1989, 67, 301–305. [Google Scholar] [CrossRef]
- Small, D.; Hevy, J.; Tang-Liu, D. Comparison of Tear Sampling Techniques for Pharmacokinetic Analysis: Ofloxacin Concentrations in Rabbit Tears after Sampling with Schirmer Tear Strips, Capillary Tubes, or Surgical Sponges. J. Ocul. Pharmacol. Ther. 2000, 16, 439–446. [Google Scholar] [CrossRef]


| ID | Breed | BW (kg) | Sex | Age (years) |
|---|---|---|---|---|
| 1 | Labrador | 32 | F | 2 |
| 2 | Golden Retriever | 34 | M | 5 |
| 3 | Kurzhaar | 28 | M | 3 |
| 4 | Mix breed | 10 | F | 2 |
| 5 | Whippet | 17 | M | 6 |
| 6 | Whippet | 19 | M | 7 |
| 7 | Mix breed | 30 | M | 3 |
| 8 | Mix breed | 31 | M | 4 |
| 9 | Mix breed | 25 | F | 5 |
| 10 | Jack Russel | 13 | M | 3 |
| 11 | Beagle | 17 | M | 6 |
| 12 | Mix breed | 19 | M | 1 |
| 13 | Mix breed | 14 | F | 3 |
| 14 | Border Collie | 15 | F | 2 |
| 15 | Pointer | 23 | M | 1 |
| Order of Testing | Study Procedure |
|---|---|
| Day 0 | |
| 1 | Visual examination |
| 2 | Slit lamp examination of eyelids, cornea, tear meniscus and conjunctiva |
| 3 | Shirmer tear test (STT-1) and intraocular pressure (IOP) (both eyes) |
| Day 1 | |
| 1 | Tear sample collection: by randomly using Schirmer tear strips (STS) in one eye and ophthalmic sponges (OS) in the other |
| 2 | Analysis of parameters (volume and total protein content) |
| 3 | Evaluation of aquaporin 1 (AQP1) expression by Western blotting |
| Day 2 | |
| 1 | Assessment of tear film break up time (BUT) |
| 2 | Fluorescein test corneal staining |
| 3 | Lyssamine green corneal staining |
| ID | STT-1 (RE) (mm/min) | STT-1(LE) (mm/min) | IOP (RE) (mm/Hg) | IOP (LE) (mm/Hg) | BUT (RE) (s) | BUT (LE) (s) |
|---|---|---|---|---|---|---|
| 1 | 15 | 18 | 15 | 20 | 18 | 19 |
| 2 | 20 | 22 | 16 | 22 | 19 | 17 |
| 3 | 22 | 20 | 21 | 14 | 18 | 18 |
| 4 | 15 | 15 | 14 | 17 | 21 | 20 |
| 5 | 30 | 24 | 22 | 19 | 20 | 21 |
| 6 | 13 | 16 | 14 | 20 | 19 | 18 |
| 7 | 17 | 24 | 16 | 22 | 18 | 19 |
| 8 | 18 | 20 | 23 | 21 | 20 | 22 |
| 9 | 25 | 25 | 22 | 23 | 18 | 18 |
| 10 | 23 | 17 | 20 | 22 | 18 | 19 |
| 11 | 23 | 20 | 17 | 17 | 20 | 19 |
| 12 | 26 | 26 | 19 | 21 | 21 | 20 |
| 13 | 20 | 15 | 23 | 19 | 20 | 19 |
| 14 | 15 | 20 | 14 | 18 | 20 | 21 |
| 15 | 19 | 22 | 14 | 17 | 18 | 18 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lamagna, B.; Ciaramella, P.; Lamagna, F.; Di Loria, A.; Brunetti, A.; Pelagalli, A. Aquaporin 1 (AQP1) Expression in Healthy Dog Tears. Animals 2020, 10, 820. https://doi.org/10.3390/ani10050820
Lamagna B, Ciaramella P, Lamagna F, Di Loria A, Brunetti A, Pelagalli A. Aquaporin 1 (AQP1) Expression in Healthy Dog Tears. Animals. 2020; 10(5):820. https://doi.org/10.3390/ani10050820
Chicago/Turabian StyleLamagna, Barbara, Paolo Ciaramella, Francesco Lamagna, Antonio Di Loria, Arturo Brunetti, and Alessandra Pelagalli. 2020. "Aquaporin 1 (AQP1) Expression in Healthy Dog Tears" Animals 10, no. 5: 820. https://doi.org/10.3390/ani10050820
APA StyleLamagna, B., Ciaramella, P., Lamagna, F., Di Loria, A., Brunetti, A., & Pelagalli, A. (2020). Aquaporin 1 (AQP1) Expression in Healthy Dog Tears. Animals, 10(5), 820. https://doi.org/10.3390/ani10050820






