Mechanical Transmission of Lumpy Skin Disease Virus by Stomoxys spp. (Stomoxys calsitrans, Stomoxys sitiens, Stomoxys indica), Diptera: Muscidae
Abstract
Summary
Abstract
1. Introduction
2. Materials and methods
2.1. Animal Ethics
2.2. Experimental Animals
2.3. Experimental Design
2.4. Virus Strain
2.5. Virus Amplification Test
2.6. Serum Neutralization Test
2.7. Virus Isolation
3. Results
3.1. Demonstration of LSDV Transmission by Stomoxys calcitrans
3.2. Demonstration of LSDV Transmission by Stomoxys sitiens
3.3. Demonstration of LSDV Transmission by Stomoxys indica
3.4. Detection of LSDV in the Proboscis of Stable Flies Fed on LSDV-Infected Cattle
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Availability
References
- Davies, F.G. Lumpy skin disease, an African capripox virus disease of cattle. Br. Vet. J. 1991, 147, 489–503. [Google Scholar] [CrossRef]
- Tasioudi, K.E.; Antoniou, S.E.; Iliadou, P.; Sachpatzidis, A.; Plevraki, E.; Agianniotaki, E.I.; Agianniotaki, C.; Fouki, O.; Mangana-Vougiouka, E.; Chondrokouki, C.D. Emergence of Lumpy Skin Disease in Greece, 2015. Transbound. Emerg. Dis. 2016, 63, 260–265. [Google Scholar] [CrossRef]
- Zeynalova, S.; Asadov, K.; Guliyev, F.; Vatani, M.; Aliyev, V. Epizootology and Molecular Diagnosis of Lumpy Skin Disease among Livestock in Azerbaijan. Front. Microb. 2016, 7, 1022. [Google Scholar] [CrossRef] [PubMed]
- Sprygin, A.; Artyuchova, E.; Babin, Y.; Prutnikov, P.; Kostrova, E.; Byadovskaya, O.; Byadovskaya, A.K. Epidemiological characterization of lumpy skin disease outbreaks in Russia in 2016. Transbound. Emerg. Dis. 2018, 65, 1514–1521. [Google Scholar] [CrossRef] [PubMed]
- OIE. LUMPY SKIN DISEASE. Available online: https://www.oie.int/fileadmin/Home/eng/Animal_Health_in_the_World/docs/pdf/Disease_cards/LUMPY_SKIN_DISEASE_FINAL.pdf (accessed on 12 January 2020).
- Tuppurainen, E.S.M.; Oura, C.A.L. Review: Lumpy skin disease: An emerging threat to Europe, the Middle East and Asia. Transbound. Emerg. Dis. 2012, 59, 40–48. [Google Scholar] [CrossRef]
- Babiuk, S.; Bowden, T.R.; Boyle, D.B.; Wallace, D.B.; Kitching, R.P. Capripoxviruses: An emerging worldwide threat to sheep, goats and cattle. Transbound. Emerg. Dis. 2008, 55, 263–272. [Google Scholar] [CrossRef]
- Manual of Diagnostic Tests and Vaccines for Terrestrial Animals. Lumpy Skin Disease. Available online: http://web.oie.int/eng/normes/MMANUAL/A_Index.htm (accessed on 26 February 2016).
- Woods, J.A. Lumpy skin disease—a review. Trop. Anim. Health Prod. 1988, 20, 11–17. [Google Scholar] [CrossRef]
- Weiss, K.E. Lumpy Skin Disease Virus; Springer: Berlin/Heidelberg, Germany, 1968; pp. 111–131. [Google Scholar]
- Carn, V.M.; Kitching, R.P. An investigation of possible routes of transmission of lumpy skin disease virus (Neethling). Epidemiol. Infect. 1995, 114, 219–226. [Google Scholar] [CrossRef]
- Magori-Cohen, R.; Louzoun, Y.; Herziger, Y.; Oron, E.; Arazi, A.; Tuppurainen, E.; Shpigel, N.; Klement, E. Mathematical modelling and evaluation of the different routes of transmission of lumpy skin disease virus. Vet. Res. 2012, 43, 1. [Google Scholar] [CrossRef]
- Gubbins, S. Using the basic reproduction number to assess the risk of transmission of lumpy skin disease virus by biting insects. Transbound. Emerg. Dis. 2019, 66, 1873–1883. [Google Scholar] [CrossRef]
- Kitching, R.P.; Mellor, P.S. Insect transmission of capripoxvirus. Res. Vet. Sci. 1986, 40, 255–258. [Google Scholar] [CrossRef]
- Sohier, C.; Haegeman, A.; Mostin, L.; De Leeuw, I.; Van Campe, W.; De Vleeschauwer, A.; Tuppurainen, E.S.M.; Berg, T.V.D.; De Regge, N.; De Clercq, K. Experimental evidence of mechanical lumpy skin disease virus transmission by Stomoxys calcitrans biting flies and Haematopota spp. horseflies. Sci. Rep. 2019, 9, 20076. [Google Scholar] [CrossRef] [PubMed]
- Chihota, C.M.; Rennie, L.F.; Kitching, R.P.; Mellor, P.S. Mechanical transmission of lumpy skin disease virus by Aedes aegypti (Diptera: Culicidae). Epidemiol. Infect. 2001, 126, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Kahana-Sutin, E.; Klement, E.; Lensky, I.; Gottlieb, Y. High relative abundance of the stable fly Stomoxys calcitrans is associated with lumpy skin disease outbreaks in Israeli dairy farms. Med. Vet. Entomol. 2017, 31, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Ausems, E.J. The European Convention for the Protection of Vertebrate Animals Used for Experimental and Other Scientific Purposes. Z. Fur. Vers. 1986, 28, 219. [Google Scholar]
- Beard, P.; Sugar, S.; Bazarragchaa, E.; Gerelmaa, U.; Tserendorj, S.; Tuppurainen, E.; Sodnomdarjaa, R. A description of two outbreaks of capripoxvirus disease in Mongolia. Vet. Microbiol. 2010, 142, 427–431. [Google Scholar] [CrossRef]
- Zumpt, F. The Stomoxyine Biting Flies of the World. Diptera: Muscidae. Taxonomy, Biology, Economic Importance and Control Measures; Gustav Fischer Verlag: Stuttgart, Germany, 1973; 175p. [Google Scholar]
- Plowright, W.; Ferris, R.D. The growth and cytopathogenicity of sheep-pox virus in tissue cultures. Br. J. Exp. Pathol. 1958, 39, 424–435. [Google Scholar]
- Tuppurainen, E.S.; Venter, E.H.; Coetzer, J.A. The detection of lumpy skin disease virus in samples of experimentally infected cattle using different diagnostic techniques. Onderstepoort J. Vet. Res. 2005, 72, 153–164. [Google Scholar] [CrossRef]
- Ireland, D.C.; Binepal, Y.S. Improved detection of capripoxvirus in biopsy samples by PCR. J. Virol. Methods. 1998, 74, 1–7. [Google Scholar] [CrossRef]
- LUMPY SKIN DISEASE [Internet]. 2018. Available online: https://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.04.12_LSD.pdf (accessed on 12 January 2020).
- Karber, G. Article on the collective handling of pharmacological array effort. Naunyn-Schmiedebergs Arch. Exp. Pathol. Pharmakol. 1931, 162, 480–483. [Google Scholar]
- Coetzer, J.A.W. Lumpy skin disease. In Infectious Diseases of Livestock; Coetzer, J.A.W., Ed.; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- Foil, L.D.; Meek, C.L.; Adams, W.V.; Issel, C.J. Mechanical Transmission of Equine Infectious-Anemia Virus by Deer Flies (Chrysops-Flavidus) and Stable Flies (Stomoxys-Calcitrans). Am. J. Vet. Res. 1983, 44, 155–156. [Google Scholar]
- Mellor, P.S.; Kitching, R.P.; Wilkinson, P.J. Mechanical Transmission of Capripox Virus and African Swine Fever Virus by Stomoxys-Calcitrans. Res. Vet. Sci. 1987, 43, 109–112. [Google Scholar] [CrossRef]
- Turell, M.J.; Knudson, G.B. Mechanical transmission of Bacillus anthracis by stable flies (Stomoxys calcitrans) and mosquitoes (Aedes aegypti and Aedes taeniorhynchus). Infect. Immun. 1987, 55, 1859–1861. [Google Scholar] [CrossRef] [PubMed]
- Chihota, C.M.; Renniet, L.F.; Kitchingt, R.P.; Mellort, P.S. Attempted mechanical transmission of lumpy skin disease virus by biting insects. Med. Vet. Entomol. 2003, 17, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Carn, V.M.; Kitching, R.P. The clinical response of cattle experimentally infected with lumpy skin disease (Neethling) virus. Arch. Virol. 1995, 140, 503–513. [Google Scholar] [CrossRef]
- Prozesky, L.; Barnard, B.J.H. A Study of the Pathology of Lumpy Skin-Disease in Cattle. Onderstepoort J. Vet. Res. 1982, 49, 167–175. [Google Scholar]
- Webb, G. Studies on the Mechanical Transmission of Animal Viruses by Biting Flies. Ph.D. Thesis, Open University, London, UK, 1990. [Google Scholar]
- Schofield, S.; Torr, S.J. A comparison of the feeding behaviour of tsetse and stable flies. Med. Vet. Entomol. 2002, 16, 177–185. [Google Scholar] [CrossRef]
- Butler, J.F.; Kloft, W.J.; Dubose, L.A.; Kloft, E.S. Re-Contamination of Food after Feeding a P-32 Food Source to Biting Muscidae. J. Med. Entomol. 1977, 13, 567–571. [Google Scholar] [CrossRef]
- Tuppurainen, E.S.M.; Lubinga, J.C.; Stoltsz, W.H.; Troskie, M.; Carpenter, S.; Coetzer, J.A.W.; Venter, E.; Oura, C.A.L. Mechanical transmission of lumpy skin disease virus by Rhipicephalus appendiculatus male ticks. Epidemiol. Infect. 2013, 141, 425–430. [Google Scholar] [CrossRef]
- Lubinga, J.C.; Tuppurainen, E.S.M.; Mahlare, R.; Coetzer, J.A.W.; Stoltsz, W.H.; Venter, E.H. Evidence of Transstadial and Mechanical Transmission of Lumpy Skin Disease Virus by Amblyomma hebraeum Ticks. Transbound. Emerg. Dis. 2015, 62, 174–182. [Google Scholar] [CrossRef]
- Tuppurainen, E.S.M.; Lubinga, J.C.; Stoltsz, W.H.; Troskie, M.; Carpenter, S.; Coetzer, J.A.; Venter, E.; Oura, C.A. Evidence of vertical transmission of lumpy skin disease virus in Rhipicephalus decoloratus ticks. Ticks Tick-Borne Dis. 2013, 4, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Lubinga, J.C.; Tuppurainen, E.S.M.; Coetzer, J.A.W.; Stoltsz, W.H.; Venter, E.H. Transovarial passage and transmission of LSDV by Amblyomma hebraeum, Rhipicephalus appendiculatus and Rhipicephalus decoloratus. Exp. Appl. Acarol. 2014, 62, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Vatsya, S.; Banerjee, P.S.; Yadav, C.L.; Kumar, R.R. Ivermectin pour-on against one-host cattle tick booohilus microplus. Indian Vet. J. 2006, 83, 22–24. [Google Scholar]
- Koshy, T.J.; Rajavelu, G.; Lalitha, C.M. Ecology and Bionomics of the Boophilids of Tamil-Nadu. Cheiron 1982, 11, 25–30. [Google Scholar]
- Cupp, E.W. Biology of Ticks. Vet. Clin. N. Am. Small Anim. Pract. 1991, 21, 1–26. [Google Scholar] [CrossRef]
- Bailey, D.L.; Whitfield, T.L.; Smittle, B.J. Flight and Dispersal of Stable Fly Diptera-Muscidae. J. Econ. Entomol. 1973, 66, 410–411. [Google Scholar] [CrossRef]
- Yeruham, I.; Nir, O.; Braverman, Y.; Davidson, M.; Grinstein, H.; Haymovitch, M.; Zamir, O. Spread of lumpy skin disease in Israeli dairy herds. Vet. Rec. 1995, 137, 91–93. [Google Scholar] [CrossRef]
- Gubbins, S.; Stegeman, A.; Klement, E.; Pite, L.; Broglia, A.; Cortinas Abrahantes, J. Inferences about the transmission of lumpy skin disease virus between herds from outbreaks in Albania in 2016. Prev. Vet. Med. 2018, in press. [Google Scholar] [CrossRef]
| Time/Day Post Feed | Stomoxys calcitrans | Stomoxys sitiens | Stomoxys indica | ||||||
|---|---|---|---|---|---|---|---|---|---|
| PCR (No Positive/No Tested) | Virus Isolation (No Positive/No Tested) | Virus Isolation (TCID50/mL), Mean | PCR (No Positive/No Tested) | Virus Isolation (No Positive/No Tested) | Virus Isolation (TCID50/mL), Mean | PCR (No Positive/No Tested) | Virus Isolation (No Positive/No Tested) | Virus Isolation (TCID50/mL), Mean | |
| 0 h | 12/15 | 9/15 | 3.5 | 13/15 | 12/15 | 3.1 | 11/15 | 10/15 | 3.3 |
| 6 h | 8/15 | 4/15 | 1.8 | 11/15 | 5/15 | 2.0 | 8/15 | 4/15 | 1.9 |
| 1 | 5/15 | 0/15 | - | 4/15 | 0/15 | - | 3/15 | 0/15 | - |
| 2 | 2/15 | 0/15 | - | 3/15 | 0/15 | - | 2/15 | 0/15 | - |
| 4 | 0/15 | 0/15 | - | 0/15 | 0/15 | - | 0/15 | 0/15 | - |
| 7 | 0/15 | 0/15 | - | 0/15 | 0/15 | - | 0/15 | 0/15 | - |
| 14 | 0/15 | 0/15 | - | 0/15 | 0/15 | - | 0/15 | 0/15 | - |
| Animal ID | Route of Transmission | Numbers and Species of Flies Fed | Body Temperature | Lesions | Enlargement of Lymph Nodes | Additional Clinical Signs |
|---|---|---|---|---|---|---|
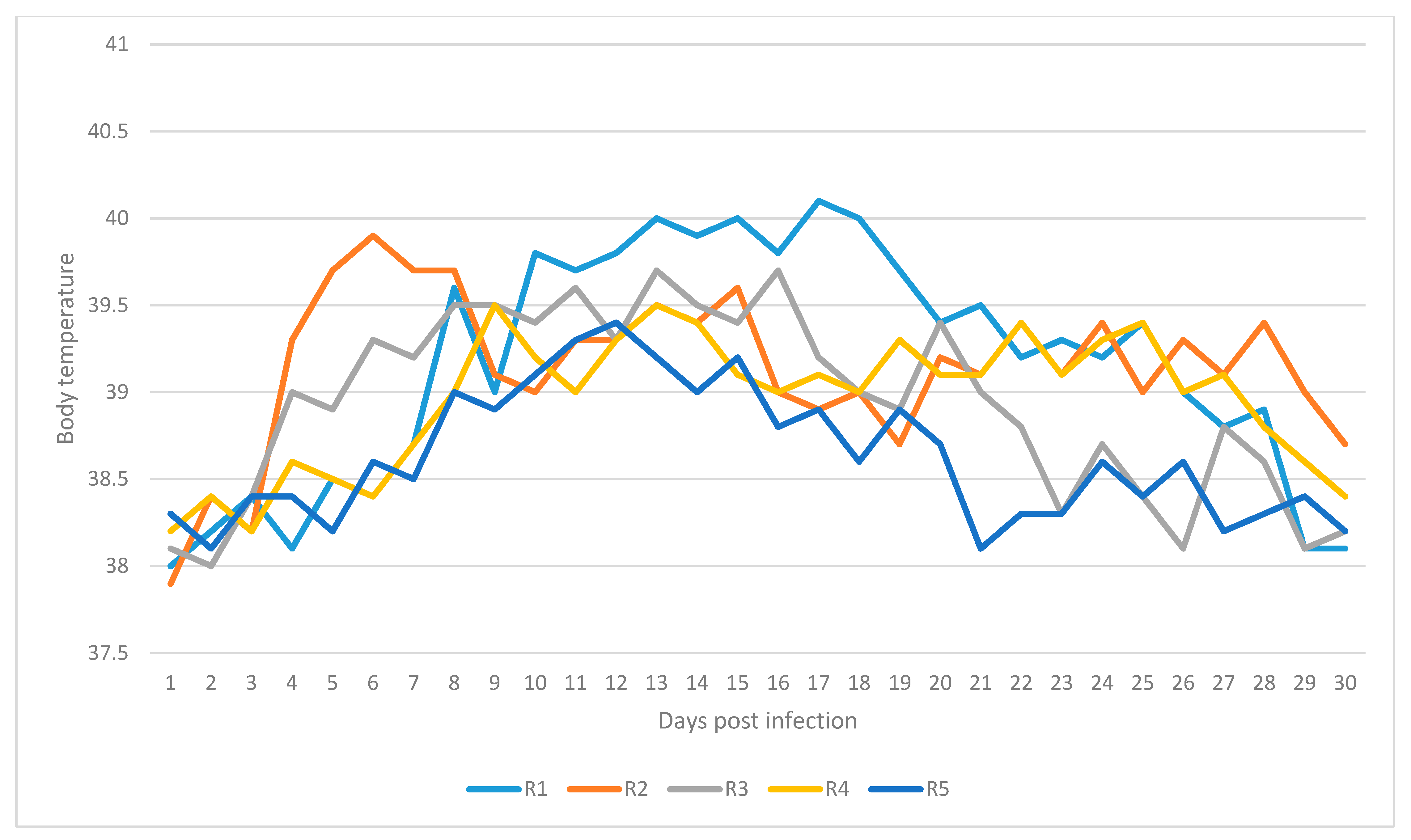
| R1 | Mechanical | 210 Stomoxys calcitrans | Up to 40.1 °C (on day 17 post exposure) | Small skin nodules developed on fly feeding sites (Day 10 post exposure) | Mild enlargement: prescapular and precrural lymph nodes (Day 11 post exposure) | Nasal and ocular discharges (Day 11 post exposure) |
| R2 | Mechanical | 210 Stomoxys calcitrans | Up to 39.9 °C (on day 6 post exposure) | Small swellings at feeding sites (Day 14 post exposure) | Mild enlargement: prescapular and precrural lymph nodes (Day 9 post exposure) | Nasal and ocular discharges (on day 6 post exposure) |
| R3 | Mechanical | 200 Stomoxys sitiens | Up to 39.7 ℃ (on day 13 post exposure) | Large swellings at feeding sites (Day 7 post exposure) | Mild enlargement: prescapular lymph node (Day 13 post exposure) | Oedema of the hind limbs (Day 13 post exposure) |
| R4 | Mechanical | 200 Stomoxys sitiens | Up to 39.5 ℃ (on day 9 post exposure) | Skin lesions at feeding sites (Day 14 post exposure) | Mild enlargement: prescapular and precrural lymph nodes (Day 14 post exposure) | Nasal and oral discharges, rhinitis (Day 11 post exposure) |
| R5 | Mechanical | 230 Stomoxys indica | Up to 39.8 ℃ (on day 12 post exposure) | Small skin lesions at feeding sites (Day 10 post exposure) | Mild enlargement: prescapular lymph node (Day 11 post exposure) | - |
| R6 | Mechanical | 230 Stomoxys indica | - | Small-sized swellings on the feeding site (Day 2 post exposure) | - | - |
| Animal ID | Transmission | Gel-Based PCR | SNT | Virus Isolation/Titre | Results |
|---|---|---|---|---|---|
| R1 | Mechanical | Positive (days 7, 13, 17, 21 pe) | Positive (days 14, 21, 28 pe) | Positive (day 15 pe)/103 TCID50 | Infected |
| R2 | Mechanical | Positive (days 11, 13, 15 pe) | Positive (days 14, 21, 28 pe) | Positive (days 9, 11 pe)/102.5 TCID50 | Infected |
| R3 | Mechanical | Positive (days 7, 9, 13, 17 pe) | Positive (days 14, 21 pe) | Positive, 2nd passage (day 13 pe)/ 103.5 TCID50 | Infected |
| R4 | Mechanical | Positive (days 11, 15 pe) | Positive (days 14, 21 pe) | Positive, 2nd passage (day 13 pe)103 TCID50 | Infected |
| R5 | Mechanical | Positive (day 9, 11 pe) | Positive (days 14, 21 pe) | - | Infected |
| R6 | Mechanical | - | - | - | Not Infected |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Issimov, A.; Kutumbetov, L.; Orynbayev, M.B.; Khairullin, B.; Myrzakhmetova, B.; Sultankulova, K.; White, P.J. Mechanical Transmission of Lumpy Skin Disease Virus by Stomoxys spp. (Stomoxys calsitrans, Stomoxys sitiens, Stomoxys indica), Diptera: Muscidae. Animals 2020, 10, 477. https://doi.org/10.3390/ani10030477
Issimov A, Kutumbetov L, Orynbayev MB, Khairullin B, Myrzakhmetova B, Sultankulova K, White PJ. Mechanical Transmission of Lumpy Skin Disease Virus by Stomoxys spp. (Stomoxys calsitrans, Stomoxys sitiens, Stomoxys indica), Diptera: Muscidae. Animals. 2020; 10(3):477. https://doi.org/10.3390/ani10030477
Chicago/Turabian StyleIssimov, Arman, Lespek Kutumbetov, Mukhit B. Orynbayev, Berik Khairullin, Balzhan Myrzakhmetova, Kulyaisan Sultankulova, and Peter J. White. 2020. "Mechanical Transmission of Lumpy Skin Disease Virus by Stomoxys spp. (Stomoxys calsitrans, Stomoxys sitiens, Stomoxys indica), Diptera: Muscidae" Animals 10, no. 3: 477. https://doi.org/10.3390/ani10030477
APA StyleIssimov, A., Kutumbetov, L., Orynbayev, M. B., Khairullin, B., Myrzakhmetova, B., Sultankulova, K., & White, P. J. (2020). Mechanical Transmission of Lumpy Skin Disease Virus by Stomoxys spp. (Stomoxys calsitrans, Stomoxys sitiens, Stomoxys indica), Diptera: Muscidae. Animals, 10(3), 477. https://doi.org/10.3390/ani10030477





