Evaluating Impacts of a One Health Approach to Companion Animal Health and Management in a Remote Aboriginal Community in the Northern Territory, Australia
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Context
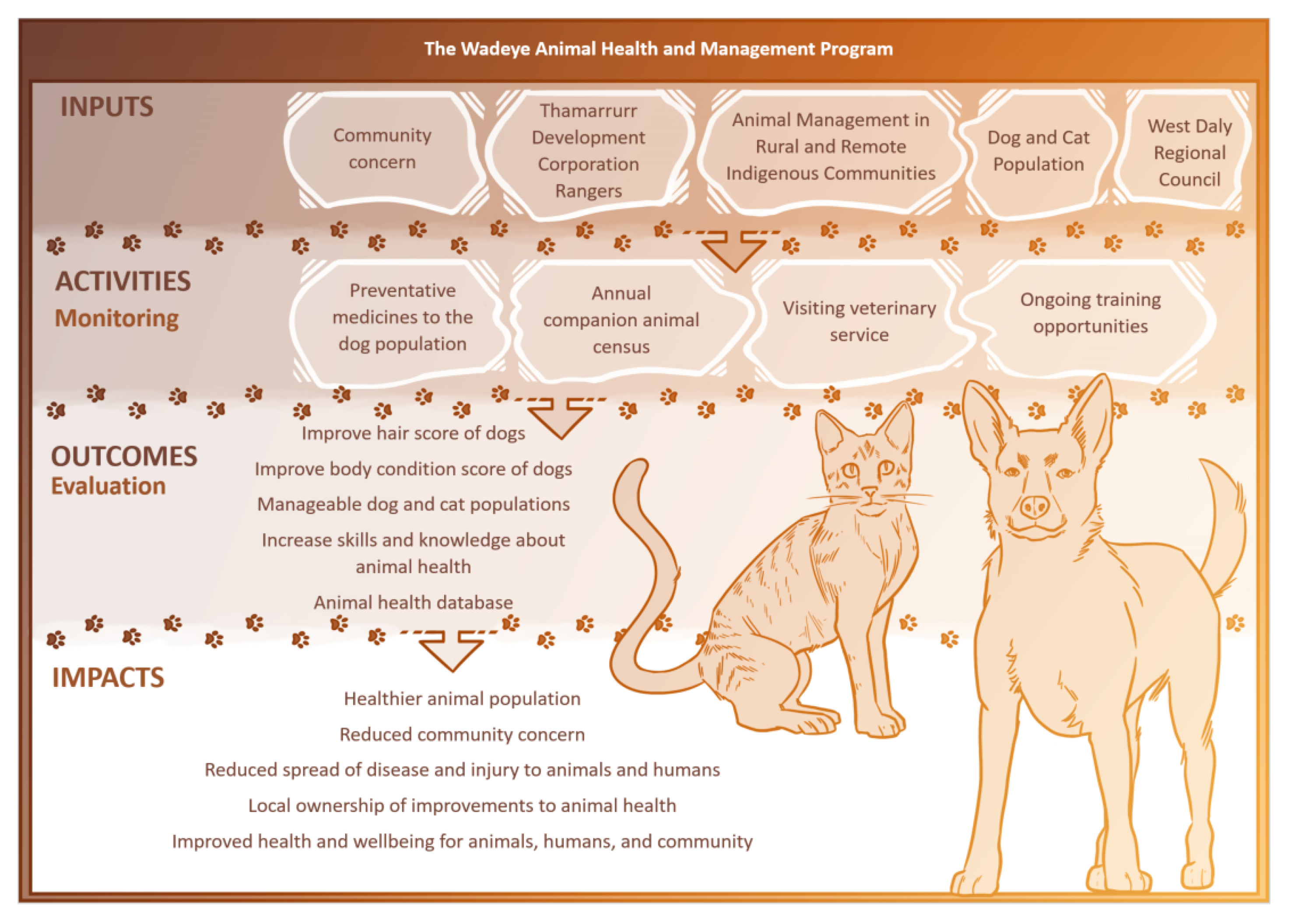
2.2. Program Components
- Co-developed animal health and management program
- ⚬
- The TDC Rangers and AMRRIC started initial discussions in September 2016, followed by an initial veterinary visit and companion animal census in June 2017. The animal health and management program then began in June 2018 and is ongoing.
- Preventative medicines administered to the dog population
- ⚬
- The TDC Rangers administered preventative medicines under veterinary direction, including ivermectin (a broad-spectrum anti-parasitic), to the dog population approximately every three months from February 2018 to June 2019. Afoxolaner (a broad-spectrum anti-parasitic) was administered to dogs that had an observed high burden of parasites. Additional preventative treatments (such as vaccination) were delivered by the visiting veterinary service when required.
- Annual companion animal census
- ⚬
- AMRRIC adapted the census for use in Wadeye. The TDC Rangers, with support from AMRRIC, conducted three annual companion animal censuses from June 2017 to June 2019. The Rangers assist with translating the census questions to community members, as the majority of people do not speak English as a first language.
- AMRRIC visiting veterinary service
- ⚬
- The visiting veterinary service, with assistance from the TDC Rangers, undertook weeklong visits to deliver desexing programs and undertake treatments and surgeries as needed. From June 2018 to June 2019, three veterinary visits occurred in Wadeye with 259 animals receiving treatment, 183 of which were surgically desexed.
- Ongoing training opportunities
- ⚬
- The TDC Rangers undertake training, provided by AMRRIC staff and TDC’s Trainer, on recognizing common animal health concerns, preparing and administering preventative medicines, and collecting data.
2.3. Ethics
2.4. Study Design
2.5. Variables
2.6. Statistical Analysis
3. Results
3.1. Animal Population and Health Outcomes
3.2. Dog Bites
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. The Control of Neglected Zoonotic Diseases: A Route to Poverty Alleviation: Report of a Joint WHO; World Health Organization: Geneva, Switzerland, 2006; p. 65, Report No.: 9241594306. [Google Scholar]
- Corning, S. World Organisation for Animal Health: Strengthening Veterinary Services for effective One Health collaboration. Rev. Sci. Tech. (Int. Off. Epizoot.) 2014, 33, 639–650. [Google Scholar] [CrossRef] [PubMed]
- Australian Government Department of Agriculture and Water Resources. Northern Australia Quarantine Strategy Canberra ACT: Australian Government Department of Agriculture and Water Resources. 2017. Available online: http://www.agriculture.gov.au/biosecurity/australia/naqs (accessed on 26 March 2020).
- Degeling, C.; Lea, T.; Brookes, V.J.; Ward, M. Rabies response, One Health and more-than-human considerations in Indigenous communities in northern Australia. Soc. Sci. Med. 2018, 212, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Australia’s Welfare 2017: In Brief; Australian Institute of Health and Welfare: Canberra, Australia, 2017.
- Quinn, E.; Massey, P.; Speare, R. Communicable diseases in rural and remote Australia: The need for improved understanding and action. Rural. Remote Heal. 2015, 15, 1–19. [Google Scholar]
- Caroll, T.; Khan, A.; Bell, G.; Standen, J. Evaluation of a Dog Health Program in an Aboriginal Community in Northern NSW. Aborig. Isl. Health Worker J. 2011, 35, 28–29. [Google Scholar]
- Schurer, J.M.; Phipps, K.; Okemow, C.; Beatch, H.; Jenkins, E. Stabilizing Dog Populations and Improving Animal and Public Health Through a Participatory Approach in Indigenous Communities. Zoonoses Public Health 2014, 62, 445–455. [Google Scholar] [CrossRef]
- Kennedy, B.; Brown, W.Y.; Vernes, K.; Körtner, G.; Butler, J.R. Dog and Cat Interactions in a Remote Aboriginal Community. Animals 2018, 8, 65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Companion Animal Management Coalition. Humane Dog Population Management Guidance; International Companion Animal Management Coalition: London, UK, 2019; p. 104. [Google Scholar]
- Constable, S.; Brown, G.; Dixon, R.M.; Dixon, R.J. Healing the Hand that Feeds You: Exploring Solutions for Dog and Community Health and Welfare in Australian Indigenous Cultures. Int. J. Interdiscip. Soc. Sci. Annu. Rev. 2008, 3, 219–230. [Google Scholar] [CrossRef]
- Ma, G.C.; Ford, J.; Lucas, L.; Norris, J.M.; Spencer, J.; Withers, A.-M.; Ward, M.P. “They Reckon They’re Man’s Best Friend and I Believe That.” Understanding Relationships with Dogs in Australian Aboriginal Communities to Inform Effective Dog Population Management. Animals 2020, 10, 810. [Google Scholar] [CrossRef]
- Constable, S.E.; Dixon, R.M.; Toribio, J.-A. Approaches to dog health education programs in Australian rural and remote Indigenous communities: Four case studies. Heal. Promot. Int. 2012, 28, 322–332. [Google Scholar] [CrossRef]
- Dhillon, J.; Favel, D.; Delorme, D.; Ratt, A.; Epp, T. Finding pathways for bite prevention and decreasing dog populations: The process of animal control for indigenous communities in Canada. J. Indig. Wellbeing 2016, 2, 82–92. [Google Scholar]
- Hudson, E.G.; Brookes, V.J.; Ward, M.P. Assessing the Risk of a Canine Rabies Incursion in Northern Australia. Front. Veter. Sci. 2017, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rusdi, B.; Laird, T.; Abraham, R.; Ash, A.; Robertson, I.D.; Mukerji, S.; Coombs, G.W.; Abraham, S.; O’Dea, M.A. Carriage of critically important antimicrobial resistant bacteria and zoonotic parasites amongst camp dogs in remote Western Australian indigenous communities. Sci. Rep. 2018, 8, 8725. [Google Scholar] [CrossRef] [PubMed]
- One Health Commission. What is One Health? Apex NC: One Health Commission. 2018. Available online: https://www.onehealthcommission.org/en/why_one_health/what_is_one_health/ (accessed on 26 March 2020).
- Molyneux, D.H.; Hallaj, Z.; Keusch, G.T.; McManus, D.P.; Ngowi, H.; Cleaveland, S.; Ramos-Jimenez, P.; Gotuzzo, E.; Kar, K.K.; Sanchez, A.; et al. Zoonoses and marginalised infectious diseases of poverty: Where do we stand? Parasites Vectors 2011, 4, 106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dhillon, J.M. Dog Population Management and Dog Bite Prevention in Rural and Remote Northern Saskatchewan Aboriginal Communities. Ph.D. Thesis, University of Saskatchewan, Saskatoon, SK, Canada, 2017. [Google Scholar]
- Constable, S.; Dixon, R.; Dixon, R. For the Love of Dog: The Human–Dog Bond in Rural and Remote Australian Indigenous Communities. Anthrozoös 2010, 23, 337–349. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. 2016 Census QuickStats: Wadeye, Canberra ACT: Australian Bureau of Statistics. 2016. Available online: http://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/SSC70275 (accessed on 26 March 2020).
- Purina. Body Condition System USA: University of Missouri. 2015. Available online: http://vhc.missouri.edu/wp-content/uploads/2015/07/BodyConditionScoreCharts.pdf (accessed on 17 August 2020).
- International Companion Animal Management Coalition. Are We Making a Difference? A Guide to Monitoring and Evaluating Dog Population Management Interventions 2015; International Companion Animal Management Coalition: London, UK, 2015; p. 132. [Google Scholar]
- Animal Medicines Australia. Pet Ownership in Australia 2016; Newgate Research: Canberra, Australia, 2016. [Google Scholar]
- D’Onise, K.; Hazel, S.; Caraguel, C.G. Mandatory desexing of dogs: One step in the right direction to reduce the risk of dog bite? A systematic review. Inj. Prev. 2017, 23, 212–218. [Google Scholar] [CrossRef]
- Lembo, T.; Attlan, M.; Bourhy, H.; Cleaveland, S.; Costa, P.; De Balogh, K.; Dodet, B.; Fooks, A.R.; Hiby, E.; Leanes, F.; et al. Renewed Global Partnerships and Redesigned Roadmaps for Rabies Prevention and Control. Veter. Med. Int. 2011, 2011, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Baker, T.; Kutz, S.; Toews, L.C.; Edwards, N.; Rock, M.J. Are we adequately evaluating subsidized veterinary services? A scoping review. Prev. Veter. Med. 2018, 157, 59–69. [Google Scholar] [CrossRef]
- Baker, T.; Rock, M.J.; Brook, R.; Van Der Meer, F.; Kutz, S. Indigenous community perspectives on dogs in Northern Canada after 10 years of veterinary services indicates improved animal and human welfare. Prev. Veter. Med. 2020, 181, 105061. [Google Scholar] [CrossRef]
- Australian Veterinary Association. Uniform Companion Animal Legislation in the Northern Territory; Discussion paper consultation; Australian Veterinary Association: Sydney, NSW, Australia, 2020; pp. 1–10. [Google Scholar]
- Smout, F.A.; Schrieber, L.; Speare, R.; Skerratt, L.F. More bark than bite: Comparative studies are needed to determine the importance of canine zoonoses in Aboriginal communities. A critical review of published research. Zoonoses Public Health 2017, 64, 495–504. [Google Scholar] [CrossRef] [Green Version]
- Johnson, I.; Hansen, A.; Bi, P. The challenges of implementing an integrated One Health surveillance system in Australia. Zoonoses Public Health 2017, 65, e229–e236. [Google Scholar] [CrossRef]
- Ma, G.C.; Withers, A.-M.; Spencer, J.; Norris, J.M.; Ward, M.P. Evaluation of a Dog Population Management Intervention: Measuring Indicators of Impact. Animals 2020, 10, 1061. [Google Scholar] [CrossRef] [PubMed]
| Research Questions | Intended Outcome of the Program | Indicator Measure of the Intended Outcome | Specific Evaluation Question |
|---|---|---|---|
| What is the state of animal health in Wadeye pre program implementation (2017)? How does the state of animal health change over the period of the program (2018 to 2019)? | Reduce or stabilise the animal population | Animals per 100 people Age group structure Breeding females Animals per household | To what extent were there changes in the companion animal population size and age distribution? To what extent were there changes to desexing status in the dog and cat population? |
| Improve animal health | Body condition score of dogs Hair score of dogs | To what extent were there changes to animal health outcomes including dog body condition and hair score? | |
| How many veterinary treatments are delivered over the program (2018 to 2019)? | Improve animal health care | Preventative and curative veterinary care Owner engagement | To what extent were veterinary care and animal medicines delivered? To what extent were households engaged in the program? |
| What is the rate of dog bite presentations to the health clinic pre program implementation (2016 to 2018)? How does the rate of dog bite presentations change over the program (2018 to 2019)? | Reduce risks to public health | Total number and rate of presentations to the clinic for dog bites | To what extent were there changes to the rate of presentations to the health clinic for a dog bite? |
| Companion Animal Population in Wadeye by Year | |||
|---|---|---|---|
| 2017 | 2018 | 2019 | |
| Animal population | |||
| Species: % (n) | |||
| Cat | 18 (134) | 19 (123) | 16 (101) |
| Dog | 82 (598) | 81 (530) | 84 (532) |
| Total | 100 (732) | 100 (653) | 100 (633) |
| Animals per 100 people | |||
| Cats per 100 people | 5.9 | 5.4 | 4.4 |
| Dogs per 100 people | 26.2 | 23.3 | 23.3 |
| Total animals per 100 people | 32.1 | 28.6 | 27.8 |
| Average animals per household | |||
| Animals per household | 3.6 | 3.9 | 3.7 |
| Animal health outcomes | |||
| Dogs desexed: % | |||
| Desexed | 28.6 | 18.5 | 37.0 |
| Not desexed | 57.4 | 54.9 | 46.1 |
| Missing | 14.1 | 26.6 | 16.9 |
| Cats desexed: % | |||
| Desexed | 14.9 | 22.0 | 30.7 |
| Not desexed | 75.4 | 52.0 | 39.6 |
| Missing | 9.7 | 26.0 | 29.7 |
| Dogs body condition score: % | |||
| Overweight | 1.2 | 0.8 | 3.8 |
| Normal | 62.2 | 48.7 | 76.7 |
| Underweight | 26.3 | 25.9 | 13.9 |
| Missing | 10.4 | 24.7 | 5.6 |
| Dogs hair score: % | |||
| Normal | 69.4 | 29.1 | 80.3 |
| Any hair loss | 19.2 | 1.5 | 13.5 |
| Missing | 11.4 | 69.4 | 6.2 |
| Animal Health Outcomes in 2019 (Post Program Implementation) Compared to 2017/2018 (Pre Program Implementation), Unadjusted and Adjusted for Age Group and Sex | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | PR | 95% CI | p Value | PR | 95% CI | p Value | |
| Desexing status of dogs and cats pre and post program implementation (desexed versus not desexed) | ||||||||||
| Dogs | Desexed | Not desexed | Unadjusted | Adjusted for age group and sex | ||||||
| 2018 | 22 | 17.6 | 103 | 82.4 | 1 | 1 | ||||
| 2019 | 192 | 44.3 | 241 | 55.7 | 2.52 | 1.70–3.74 | <0.001 | 2.50 | 1.70–3.70 | <0.001 |
| Cats | Desexed | Not desexed | Unadjusted | Adjusted for age group and sex | ||||||
| 2018 | 7 | 24.1 | 22 | 75.9 | 1 | 1 | ||||
| 2019 | 31 | 44.3 | 39 | 55.7 | 1.84 | 0.91–3.68 | 0.088 | 2.25 | 1.14–4.47 | 0.020 |
| Dogs body condition pre and post program implementation (normal weight/overweight versus underweight) | ||||||||||
| Dogs | Good body condition | Underweight | Unadjusted | Adjusted for age group and sex | ||||||
| 2018 | 53 | 48.2 | 57 | 51.8 | 1 | 1 | ||||
| 2019 | 419 | 85.0 | 74 | 15.0 | 1.76 | 1.45–2.15 | <0.001 | 1.77 | 1.45–2.15 | <0.001 |
| Dogs hair score pre and post program implementation (good hair versus any hair loss) | ||||||||||
| Dogs | Good hair score | Any hair loss | Unadjusted | Adjusted for age group and sex | ||||||
| 2017 | 408 | 78.6 | 111 | 21.4 | 1 | 1 | ||||
| 2019 | 422 | 85.6 | 71 | 14.4 | 1.09 | 1.03–1.15 | 0.004 | 1.09 | 1.03–1.16 | 0.003 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riley, T.; Lovett, R.; Thandrayen, J.; Cumming, B.; Thurber, K.A. Evaluating Impacts of a One Health Approach to Companion Animal Health and Management in a Remote Aboriginal Community in the Northern Territory, Australia. Animals 2020, 10, 1790. https://doi.org/10.3390/ani10101790
Riley T, Lovett R, Thandrayen J, Cumming B, Thurber KA. Evaluating Impacts of a One Health Approach to Companion Animal Health and Management in a Remote Aboriginal Community in the Northern Territory, Australia. Animals. 2020; 10(10):1790. https://doi.org/10.3390/ani10101790
Chicago/Turabian StyleRiley, Tamara, Raymond Lovett, Joanne Thandrayen, Bonny Cumming, and Katherine A. Thurber. 2020. "Evaluating Impacts of a One Health Approach to Companion Animal Health and Management in a Remote Aboriginal Community in the Northern Territory, Australia" Animals 10, no. 10: 1790. https://doi.org/10.3390/ani10101790





