Long-Term Sinonasal Carriage of Staphylococcus aureus and Anti-Staphylococcal Humoral Immune Response in Patients with Chronic Rhinosinusitis
Abstract
1. Introduction
2. Materials and Methods
2.1. Collection of Serum and Bacterial Samples from Patients with CRS
2.2. Antibiotic Susceptibility Testing
2.3. DNA Sequencing and Single-Nucleotide Polymorphism (SNP) Analysis
2.4. Microarray-Based Immunoglobulin Analysis
2.5. Statistical Analysis
2.6. Ethical Approval
3. Results
3.1. Presence of S. aureus in CRS Patients and Antibiotic Susceptibility
3.2. SNP-Based Phylogenetic Analysis
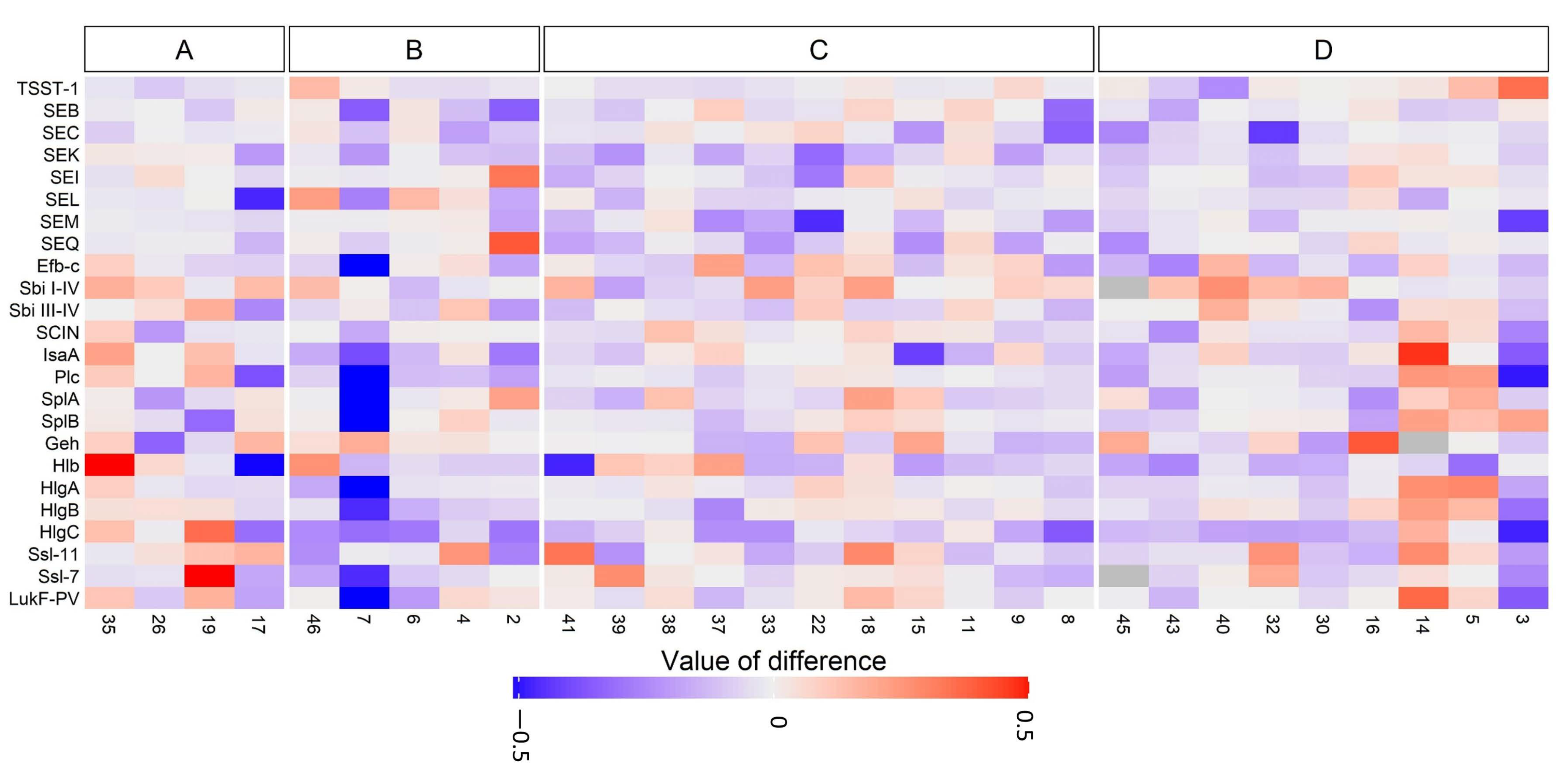
3.3. Anti-Staphylococcal Antibodies in CRS Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Derycke, L.; Perez-Novo, C.; Van Crombruggen, K.; Corriveau, M.N.; Bachert, C. Staphylococcus aureus and chronic airway disease. World Allergy Organ. J. 2010, 3, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Abou-Hamad, W.; Matar, N.; Elias, M.; Nasr, M.; Sarkis-Karam, D.; Hokayem, N.; Haddad, A. Bacterial flora in normal adult maxillary sinuses. Am. J. Rhinol. Allergy 2009, 23, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Thanasumpun, T.; Batra, P.S. Endoscopically-derived bacterial cultures in chronic rhinosinusitis: A systematic review. Am. J. Otolaryngol. 2015, 36, 686–691. [Google Scholar] [CrossRef]
- Thunberg, U.; Soderquist, B.; Hugosson, S. Bacterial findings in optimised sampling and characterisation of S. aureus in chronic rhinosinusitis. Eur. Arch. Otorhinolaryngol. 2017, 274, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Biel, M.A.; Brown, C.A.; Levinson, R.M.; Garvis, G.E.; Paisner, H.M.; Sigel, M.E.; Tedford, T.M. Evaluation of the microbiology of chronic maxillary sinusitis. Ann. Otol. Rhinol. Laryngol. 1998, 107 Pt 1, 942–945. [Google Scholar] [CrossRef]
- Kluytmans, J.; van Belkum, A.; Verbrugh, H. Nasal carriage of Staphylococcus aureus: Epidemiology, underlying mechanisms, and associated risks. Clin. Microbiol. Rev. 1997, 10, 505–520. [Google Scholar] [CrossRef]
- Wertheim, H.F.; Melles, D.C.; Vos, M.C.; van Leeuwen, W.; van Belkum, A.; Verbrugh, H.A.; Nouwen, J.L. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 2005, 5, 751–762. [Google Scholar] [CrossRef]
- Liu, C.M.; Price, L.B.; Hungate, B.A.; Abraham, A.G.; Larsen, L.A.; Christensen, K.; Stegger, M.; Skov, R.; Andersen, P.S. Staphylococcus aureus and the ecology of the nasal microbiome. Sci. Adv. 2015, 1, e1400216. [Google Scholar] [CrossRef]
- Lowy, F.D. Staphylococcus aureus infections. N. Engl. J. Med. 1998, 339, 520–532. [Google Scholar] [CrossRef]
- Laudien, M.; Gadola, S.D.; Podschun, R.; Hedderich, J.; Paulsen, J.; Reinhold-Keller, E.; Csernok, E.; Ambrosch, P.; Hellmich, B.; Moosig, F.; et al. Nasal carriage of Staphylococcus aureus and endonasal activity in Wegener’s granulomatosis as compared to rheumatoid arthritis and chronic rhinosinusitis with nasal polyps. Clin. Exp. Rheumatol. 2010, 28 (Suppl. 57), 51–55. [Google Scholar]
- Seiti Yamada Yoshikawa, F.; Feitosa de Lima, J.; Notomi Sato, M.; Alefe Leuzzi Ramos, Y.; Aoki, V.; Leao Orfali, R. Exploring the role of Staphylococcus aureus toxins in atopic dermatitis. Toxins 2019, 11, 321. [Google Scholar] [CrossRef] [PubMed]
- Tabarya, D.; Hoffman, W.L. Staphylococcus aureus nasal carriage in rheumatoid arthritis: Antibody response to toxic shock syndrome toxin-1. Ann. Rheum. Dis. 1996, 55, 823–828. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Claeys, S.E.; Tomassen, P.; van Zele, T.; Zhang, N. Rhinosinusitis and asthma: A link for asthma severity. Curr. Allergy Asthma Rep. 2010, 10, 194–201. [Google Scholar] [CrossRef]
- Bachert, C.; Holtappels, G. Pathophysiology of chronic rhinosinusitis, pharmaceutical therapy options. GMS Curr. Top. Otorhinolaryngol. Head Neck Surg. 2015, 14, 1–40. [Google Scholar] [CrossRef]
- Bernstein, J.M.; Kansal, R. Superantigen hypothesis for the early development of chronic hyperplastic sinusitis with massive nasal polyposis. Curr. Opin. Otolaryngol. Head Neck Surg. 2005, 13, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Gevaert, P.; van Cauwenberge, P. Staphylococcus aureus enterotoxins: A key in airway disease? Allergy 2002, 57, 480–487. [Google Scholar] [CrossRef] [PubMed]
- Balaban, N.; Rasooly, A. Staphylococcal enterotoxins. Int. J. Food Microbiol. 2000, 61, 1–10. [Google Scholar] [CrossRef]
- Foster, T.J.; McDevitt, D. Surface-associated proteins of Staphylococcus aureus: Their possible roles in virulence. FEMS Microbiol. Lett. 1994, 118, 199–205. [Google Scholar] [CrossRef]
- Oliveira, D.; Borges, A.; Simoes, M. Staphylococcus aureus toxins and their molecular activity in infectious diseases. Toxins 2018, 10, 252. [Google Scholar] [CrossRef]
- Bachert, C.; Gevaert, P.; Holtappels, G.; Johansson, S.G.; van Cauwenberge, P. Total and specific IgE in nasal polyps is related to local eosinophilic inflammation. J. Allergy Clin. Immunol. 2001, 107, 607–614. [Google Scholar] [CrossRef]
- Foreman, A.; Holtappels, G.; Psaltis, A.J.; Jervis-Bardy, J.; Field, J.; Wormald, P.J.; Bachert, C. Adaptive immune responses in Staphylococcus aureus biofilm-associated chronic rhinosinusitis. Allergy 2011, 66, 1449–1456. [Google Scholar] [CrossRef]
- Foreman, A.; Jervis-Bardy, J.; Wormald, P.J. Do biofilms contribute to the initiation and recalcitrance of chronic rhinosinusitis? Laryngoscope 2011, 121, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Thunberg, U.; Hugosson, S.; Fredlund, H.; Cao, Y.; Ehricht, R.; Monecke, S.; Muller, E.; Engelmann, S.; Söderquist, B. Anti-staphylococcal humoral immune response in patients with chronic rhinosinusitis. Rhinol. Online 2019, 2, 50–58. [Google Scholar] [CrossRef]
- Sahl, J.W.; Lemmer, D.; Travis, J.; Schupp, J.M.; Gillece, J.D.; Aziz, M.; Driebe, E.M.; Drees, K.P.; Hicks, N.D.; Williamson, C.H.D.; et al. NASP: An accurate, rapid method for the identification of SNPs in WGS datasets that supports flexible input and output formats. Microb. Genom. 2016, 2, e000074. [Google Scholar] [CrossRef] [PubMed]
- Stegger, M.; Driebe, E.M.; Roe, C.; Lemmer, D.; Bowers, J.R.; Engelthaler, D.M.; Keim, P.; Andersen, P.S. Genome sequence of Staphylococcus aureus strain CA-347, a USA600 methicillin-resistant isolate. Genome Announc. 2013, 1, e00517-13. [Google Scholar] [CrossRef]
- Nguyen, L.T.; Schmidt, H.A.; von Haeseler, A.; Minh, B.Q. IQ-TREE: A fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol. Biol. Evol. 2015, 32, 268–274. [Google Scholar] [CrossRef]
- Kloppot, P.; Selle, M.; Kohler, C.; Stentzel, S.; Fuchs, S.; Liebscher, V.; Müller, E.; Kale, D.; Ohlsen, K.; Bröker, B.M.; et al. Microarray-based identification of human antibodies against Staphylococcus aureus antigens. Proteom. Clin. Appl. 2015, 9, 1003–1011. [Google Scholar] [CrossRef]
- Selle, M.; Hertlein, T.; Oesterreich, B.; Klemm, T.; Kloppot, P.; Müller, E.; Ehricht, R.; Stentzel, S.; Bröker, B.M.; Engelmann, S.; et al. Global antibody response to Staphylococcus aureus live-cell vaccination. Sci. Rep. 2016, 6, 24754. [Google Scholar] [CrossRef]
- Holm, S. A simple sequentially rejective multiple test procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Duchêne, S.; Holt, K.E.; Weill, F.X.; Le Hello, S.; Hawkey, J.; Edwards, D.J.; Fourment, M.; Holmes, E.C. Genome-scale rates of evolutionary change in bacteria. Microb. Genom. 2016, 2, e000094. [Google Scholar] [CrossRef]
- Wertheim, H.F.; Verveer, J.; Boelens, H.A.; van Belkum, A.; Verbrugh, H.A.; Vos, M.C. Effect of mupirocin treatment on nasal, pharyngeal, and perineal carriage of Staphylococcus aureus in healthy adults. Antimicrob. Agents Chemother. 2005, 49, 1465–1467. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, N.H.; Espersen, F.; Rosdahl, V.T.; Jensen, K. Carriage of Staphylococcus aureus among 104 healthy persons during a 19-month period. Epidemiol. Infect. 1995, 115, 51–60. [Google Scholar] [CrossRef]
- VandenBergh, M.F.; Yzerman, E.P.; van Belkum, A.; Boelens, H.A.; Sijmons, M.; Verbrugh, H.A. Follow-up of Staphylococcus aureus nasal carriage after 8 years: Redefining the persistent carrier state. J. Clin. Microbiol. 1999, 37, 3133–3140. [Google Scholar] [CrossRef]
- Harvey, R.J.; Snidvongs, K.; Kalish, L.H.; Oakley, G.M.; Sacks, R. Corticosteroid nasal irrigations are more effective than simple sprays in a randomized double-blinded placebo-controlled trial for chronic rhinosinusitis after sinus surgery. Int. Forum. Allergy Rhinol. 2018, 8, 461–470. [Google Scholar] [CrossRef]
- Lees, K.A.; Orlandi, R.R.; Oakley, G.; Alt, J.A. The role of macrolides and doxycycline in chronic rhinosinusitis. Immunol. Allergy Clin. N. Am. 2020, 40, 303–315. [Google Scholar] [CrossRef]
- Holtfreter, S.; Grumann, D.; Schmudde, M.; Nguyen, H.T.; Eichler, P.; Strommenger, B.; Kopron, K.; Kolata, J.; Giedrys-Kalemba, S.; Steinmetzet, I.; et al. Clonal distribution of superantigen genes in clinical Staphylococcus aureus isolates. J. Clin. Microbiol. 2007, 45, 2669–2680. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, G.; Monecke, S.; Ehricht, R.; Soderquist, B. Prevalence of clonal complexes and virulence genes among commensal and invasive Staphylococcus aureus isolates in Sweden. PLoS ONE 2013, 8, e77477. [Google Scholar] [CrossRef] [PubMed]
- Acton, D.S.; Plat-Sinnige, M.J.; van Wamel, W.; de Groot, N.; van Belkum, A. Intestinal carriage of Staphylococcus aureus: How does its frequency compare with that of nasal carriage and what is its clinical impact? Eur. J. Clin. Microbiol. Infect. Dis. 2009, 28, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Dancer, S.J.; Noble, W.C. Nasal, axillary, and perineal carriage of Staphylococcus aureus among women: Identification of strains producing epidermolytic toxin. J. Clin. Pathol. 1991, 44, 681–684. [Google Scholar] [CrossRef]
- Verkaik, N.J.; de Vogel, C.P.; Boelens, H.A.; Grumann, D.; Hoogenboezem, T.; Vink, C.; Hooijkaas, H.; Foster, T.; Verbrugh, H.; Van Belkum, A.; et al. Anti-staphylococcal humoral immune response in persistent nasal carriers and noncarriers of Staphylococcus aureus. J. Infect. Dis. 2009, 199, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Soderquist, B.; Danielsson, D.; Holmberg, H.; Vikerfors, T. Granulocyte colony-stimulating factor (G-CSF) and interleukin (IL)-8 in sera from patients with Staphylococcus aureus septicemia. Clin. Microbiol. Infect. 1995, 1, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Dryla, A.; Prustomersky, S.; Gelbmann, D.; Hanner, M.; Bettinger, E.; Kocsis, B.; Kustos, T.; Henics, T.; Meinke, A.; Nagy, E. Comparison of antibody repertoires against Staphylococcus aureus in healthy individuals and in acutely infected patients. Clin. Diagn. Lab. Immunol. 2005, 12, 387–398. [Google Scholar] [CrossRef] [PubMed]
- Banks, M.C.; Kamel, N.S.; Zabriskie, J.B.; Larone, D.H.; Ursea, D.; Posnett, D.N. Staphylococcus aureus express unique superantigens depending on the tissue source. J. Infect. Dis. 2003, 187, 77–86. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Holtfreter, S.; Bauer, K.; Thomas, D.; Feig, C.; Lorenz, V.; Roschack, K.; Friebe, E.; Selleng, K.; Lövenich, S.; Greve, T.; et al. egc-encoded superantigens from Staphylococcus aureus are neutralized by human sera much less efficiently than are classical staphylococcal enterotoxins or toxic shock syndrome toxin. Infect. Immun. 2004, 72, 4061–4071. [Google Scholar] [CrossRef]
- Holtfreter, S.; Kolata, J.; Broker, B.M. Towards the immune proteome of Staphylococcus aureus—The anti-S. aureus antibody response. Int. J. Med. Microbiol. 2010, 300, 176–192. [Google Scholar] [CrossRef]
- Radke; E. E.; Brown, S.M.; Pelzek, A.J.; Fulmer, Y.; Hernandez, D.N.; Torres, V.J.; Thomsen, I.P.; Chiang, W.K.; Miller, A.O.; Shopsin, B.; et al. Hierarchy of human IgG recognition within the Staphylococcus aureus immunome. Sci. Rep. 2018, 8, 13296.
- Van Belkum, A.; Verkaik, N.; De Vogel, C.P.; Boelens, H.A.; Verveer, J.; Nouwen, J.L.; Verbrugh, H.A.; Wertheim, H.F.L. Reclassification of Staphylococcus aureus nasal carriage types. J. Infect. Dis. 2009, 199, 1820–1826. [Google Scholar] [CrossRef]
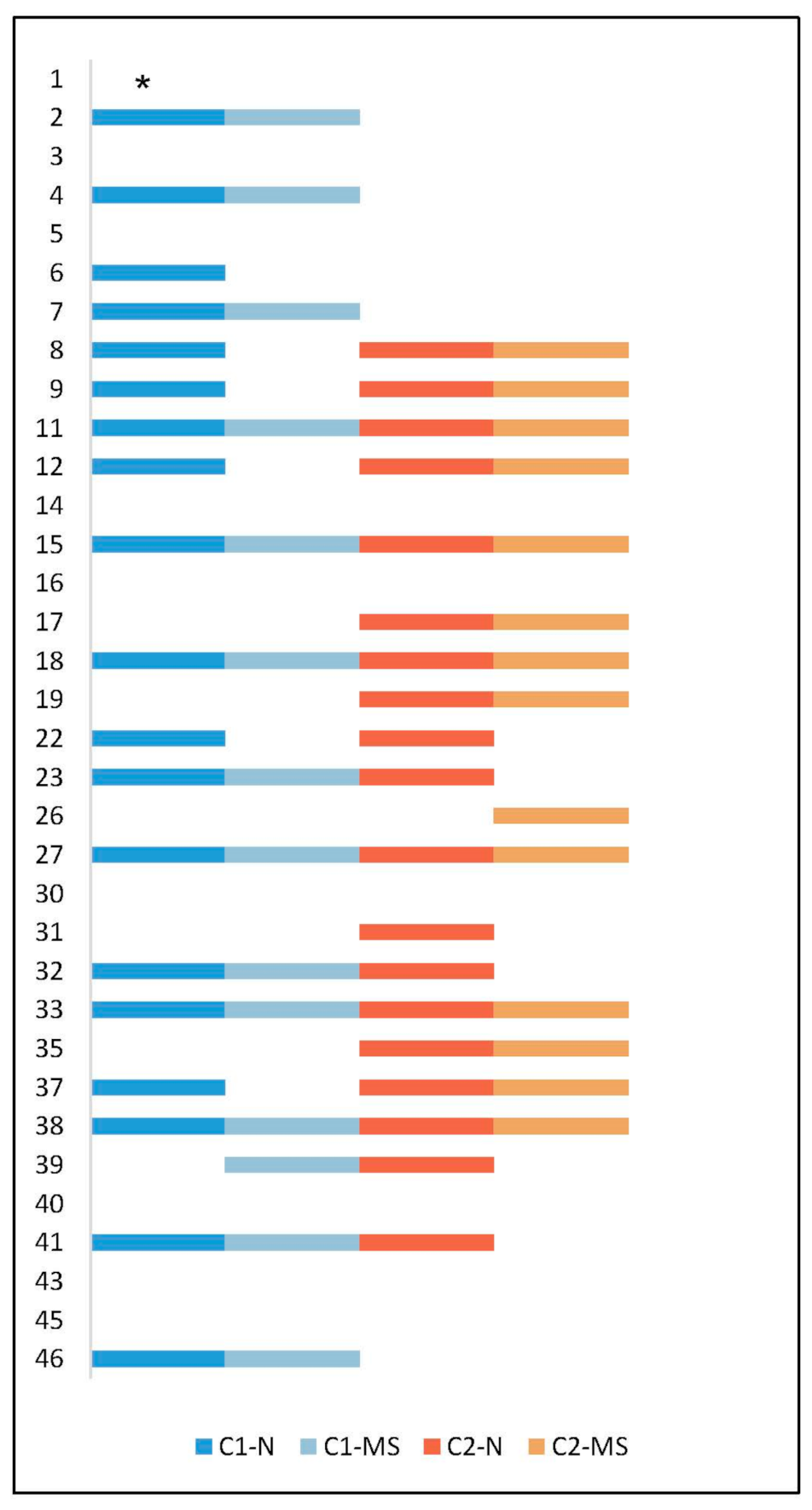
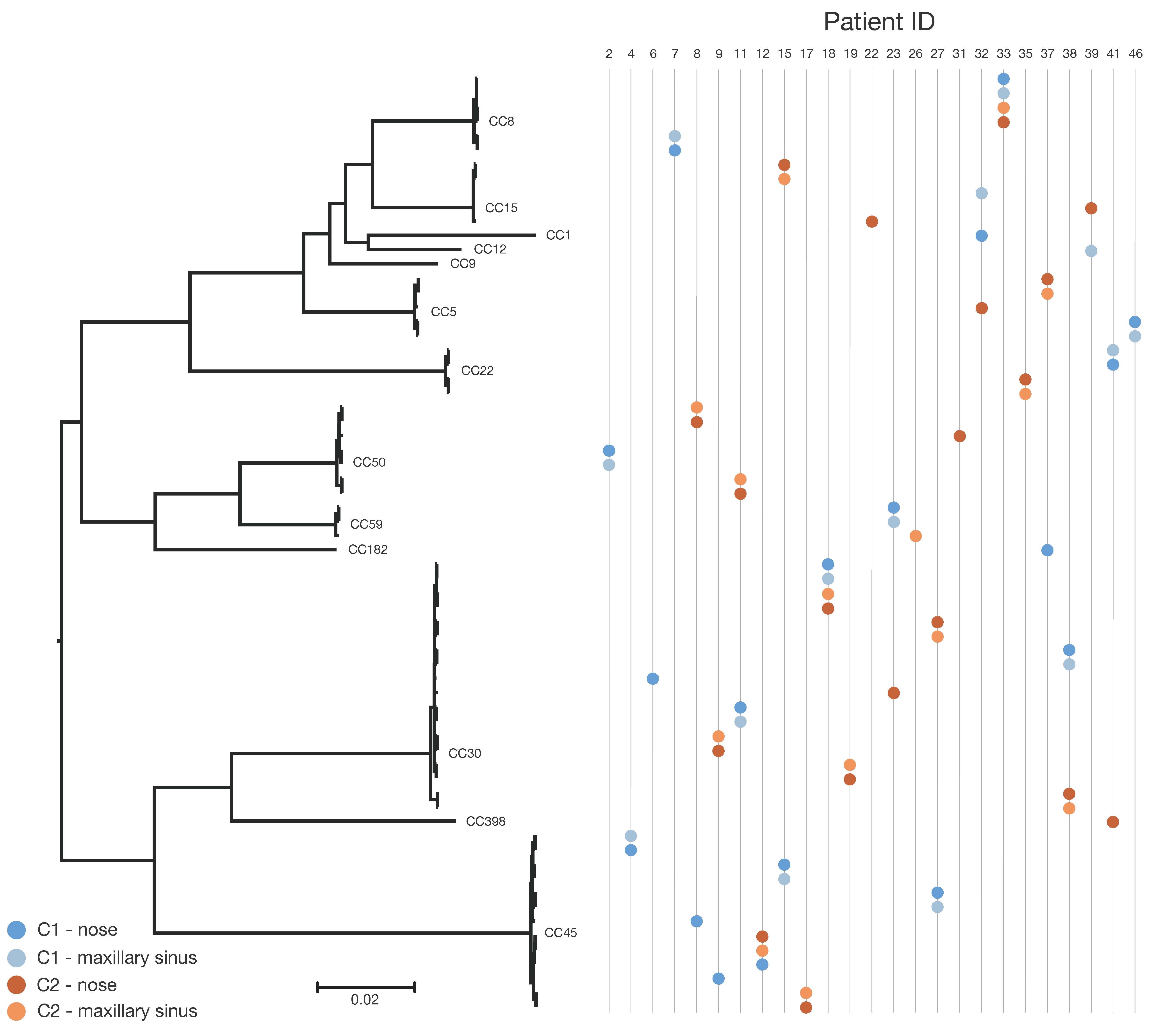
| Patient ID | Clonal Complex | Time Point | Sample Site | SNP Differences between C1 and C2 | SNP Differences Comparing C1 to C1 or C2 to C2 |
|---|---|---|---|---|---|
| 2 c | CC50 | C1 | N | Not applicable | 0 |
| 2 | CC50 | C1 | MS | ||
| 4 c | CC45 | C1 | N | Not applicable | 1 |
| 4 | CC45 | C1 | MS | ||
| 6 | CC30 | C1 | N | Not applicable | Not applicable |
| 7 c | CC8 | C1 | N | Not applicable | 2 |
| 7 | CC8 | C1 | MS | ||
| 8 | CC45 | C1 | N | 37,758–37,761 | 3 |
| 8 | CC50 | C2 | N | ||
| 8 | CC50 | C2 | MS | ||
| 9 | CC45 | C1 | N | 33,462–33,463 | 1 |
| 9 | CC30 | C2 | N | ||
| 9 | CC30 | C2 | MS | ||
| 11 | CC30 | C1 | N | 32,890–32,892 | 1 |
| 11 | CC30 | C1 | MS | ||
| 11 | CC50 | C2 | N | 3 | |
| 11 | CC50 | C2 | MS | ||
| 12 | CC45 | C1 | N | 29–30 a | 1 |
| 12 | CC45 | C2 | MS | ||
| 12 | CC45 | C2 | N | ||
| 15 | CC45 | C1 | N | 41,088–41,089 | 1 |
| 15 | CC45 | C1 | MS | ||
| 15 | CC15 | C2 | N | 2 | |
| 15 | CC15 | C2 | MS | ||
| 17 b | CC45 | C2 | N | Not applicable | 0 |
| 17 | CC45 | C2 | MS | ||
| 18 | CC30 | C1 | N | 65–67 a | 2 |
| 18 | CC30 | C1 | MS | ||
| 18 | CC30 | C2 | N | 0 | |
| 18 | CC30 | C2 | MS | ||
| 19 b | CC30 | C2 | N | Not applicable | 2 |
| 19 | CC30 | C2 | MS | ||
| 22 | CC9 | C1 | N | 18,896 | Not applicable |
| 22 | CC15 | C2 | N | ||
| 23 | CC59 | C1 | N | 32,884–32,885 | 3 |
| 23 | CC59 | C1 | MS | ||
| 23 | CC30 | C2 | N | ||
| 26 | CC59 | C2 | MS | Not applicable | Not applicable |
| 27 | CC45 | C1 | N | 33,500–33,505 | 1 |
| 27 | CC45 | C1 | MS | ||
| 27 | CC30 | C2 | N | 4 | |
| 27 | CC30 | C2 | MS | ||
| 31 | CC50 | C2 | N | Not applicable | Not applicable |
| 32 | CC1 | C1 | N | 13,939–17,065 | 15,884 |
| 32 | CC15 | C1 | MS | ||
| 32 | CC5 | C2 | N | ||
| 33 | CC8 | C1 | N | 48–51 a | 2 |
| 33 | CC8 | C1 | MS | ||
| 33 | CC8 | C2 | N | 5 | |
| 33 | CC8 | C2 | MS | ||
| 35 b | CC22 | C2 | N | Not applicable | 25 |
| 35 | CC22 | C2 | MS | ||
| 37 | CC182 | C1 | N | 29,807 | 0 |
| 37 | CC5 | C2 | N | ||
| 37 | CC5 | C2 | MS | ||
| 38 | CC30 | C1 | N | 817–818 | 2 |
| 38 | CC30 | C1 | MS | ||
| 38 | CC30 | C2 | N | 1 | |
| 38 | CC30 | C2 | MS | ||
| 39 | CC12 | C1 | MS | 12,182 | Not applicable |
| 39 | CC15 | C2 | N | ||
| 41 | CC22 | C1 | N | 33,882–33,883 | 1 |
| 41 | CC22 | C1 | MS | ||
| 41 | CC398 | C2 | N | ||
| 46 c | CC5 | C1 | N | Not applicable | 1 |
| 46 | CC5 | C1 | MS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thunberg, U.; Hugosson, S.; Ehricht, R.; Monecke, S.; Müller, E.; Cao, Y.; Stegger, M.; Söderquist, B. Long-Term Sinonasal Carriage of Staphylococcus aureus and Anti-Staphylococcal Humoral Immune Response in Patients with Chronic Rhinosinusitis. Microorganisms 2021, 9, 256. https://doi.org/10.3390/microorganisms9020256
Thunberg U, Hugosson S, Ehricht R, Monecke S, Müller E, Cao Y, Stegger M, Söderquist B. Long-Term Sinonasal Carriage of Staphylococcus aureus and Anti-Staphylococcal Humoral Immune Response in Patients with Chronic Rhinosinusitis. Microorganisms. 2021; 9(2):256. https://doi.org/10.3390/microorganisms9020256
Chicago/Turabian StyleThunberg, Ulrica, Svante Hugosson, Ralf Ehricht, Stefan Monecke, Elke Müller, Yang Cao, Marc Stegger, and Bo Söderquist. 2021. "Long-Term Sinonasal Carriage of Staphylococcus aureus and Anti-Staphylococcal Humoral Immune Response in Patients with Chronic Rhinosinusitis" Microorganisms 9, no. 2: 256. https://doi.org/10.3390/microorganisms9020256
APA StyleThunberg, U., Hugosson, S., Ehricht, R., Monecke, S., Müller, E., Cao, Y., Stegger, M., & Söderquist, B. (2021). Long-Term Sinonasal Carriage of Staphylococcus aureus and Anti-Staphylococcal Humoral Immune Response in Patients with Chronic Rhinosinusitis. Microorganisms, 9(2), 256. https://doi.org/10.3390/microorganisms9020256






