Wild Rabbit Exposure to Leishmania infantum, Toxoplasma gondii, Anaplasma phagocytophilum and Babesia caballi Evidenced by Serum and Aqueous Humor Antibody Detection
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Sampling
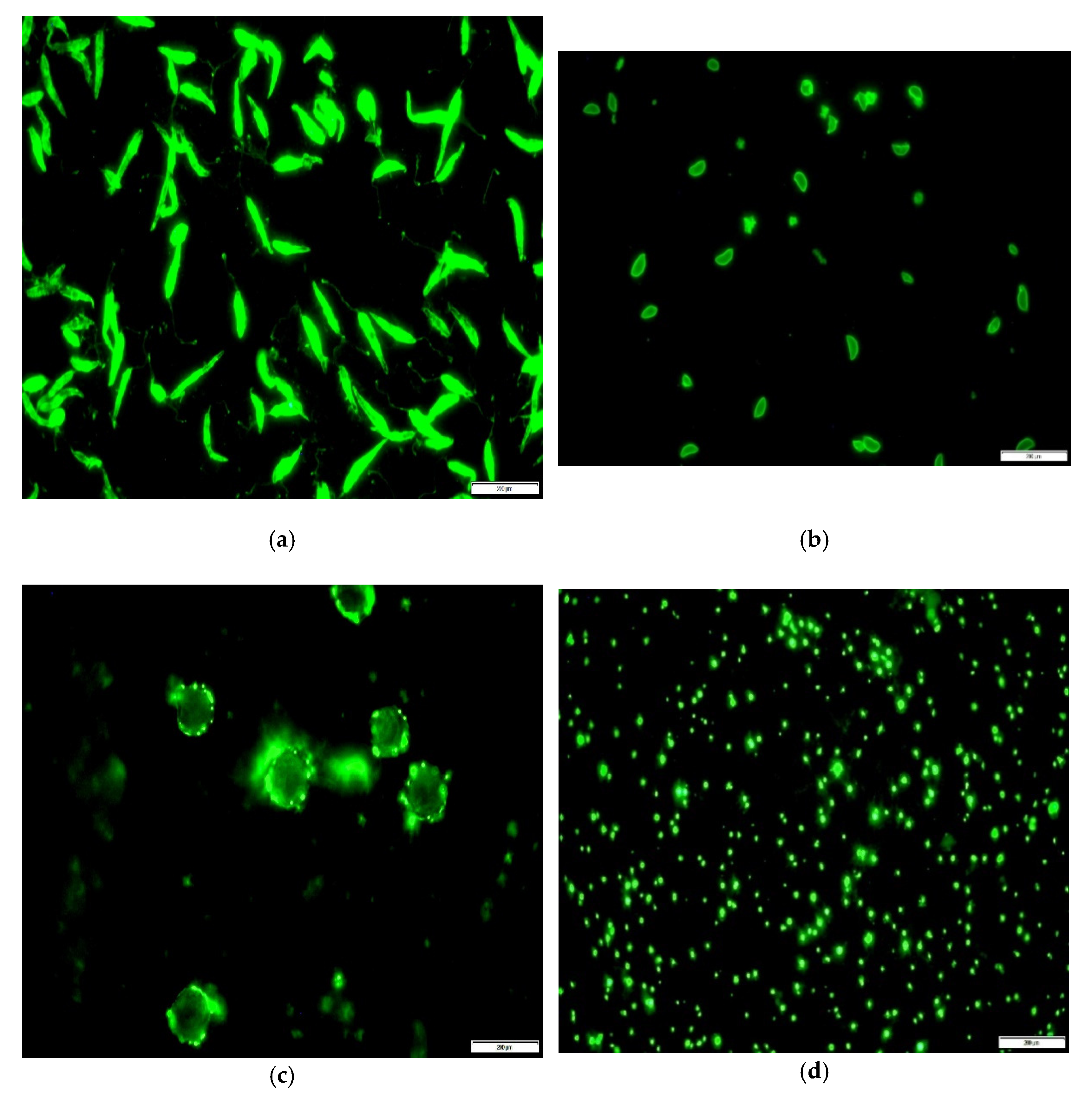
2.3. Indirect Immunofluorescence Antibody (IFA) Assay
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferrand, N. Inferring the Evolutionary History of the European Rabbit (Oryctolagus cuniculus) from Molecular Markers. In Lagomorph Biology; Alves, P.C., Ferrand, N.K.H., Eds.; Springer: Berlin/Heidelberg, Germany, 2008; pp. 47–63. [Google Scholar]
- Martín-Sánchez, J.; Torres-Medina, N.; Morillas-Márquez, F.; Corpas-López, V.; Díaz-Sáez, V. Role of wild rabbits as reservoirs of leishmaniasis in a non-epidemic Mediterranean hot spot in Spain. Acta Trop. 2021, 222, 106036. [Google Scholar] [CrossRef] [PubMed]
- McKenny, L.; O’Handley, R.; Kovaliski, J.; Mutze, G.; Peacock, D.; Lanyon, S. Evidence of infection with Toxoplasma gondii and Neospora caninum in South Australia: Using wild rabbits as a sentinel species. Aust. Vet. J. 2020, 98, 380–387. [Google Scholar] [CrossRef]
- Solano-Gallego, L.; Koutinas, A.; Miró, G.; Cardoso, L.; Pennisi, M.G.; Ferrer, L.; Bourdeau, P.; Oliva, G.; Baneth, G. Directions for the diagnosis, clinical staging, treatment and prevention of canine leishmaniosis. Vet. Parasitol. 2009, 165, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Quinnell, R.J.; Courtenay, O. Transmission, reservoir hosts and control of zoonotic visceral leishmaniasis. Parasitology 2009, 136, 1915–1934. [Google Scholar] [CrossRef]
- Millán, J.; Ferroglio, E.; Solano-Gallego, L.J.P.R. Role of wildlife in the epidemiology of Leishmania infantum infection in Europe. Parasitol. Res. 2014, 113, 2005–2014. [Google Scholar] [CrossRef]
- Molina, R.; Jiménez, M.I.; Cruz, I.; Iriso, A.; Martín-Martín, I.; Sevillano, O.; Melero, S.; Bernal, J. The hare (Lepus granatensis) as potential sylvatic reservoir of Leishmania infantum in Spain. Vet. Parasitol. 2012, 190, 268–271. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, M.; González, E.; Iriso, A.; Marco, E.; Alegret, A.; Fúster, F.; Molina, R. Detection of Leishmania infantum and identification of blood meals in Phlebotomus perniciosus from a focus of human leishmaniasis in Madrid, Spain. Parasitol. Res. 2013, 112, 2453–2459. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Fons, F.; Ferroglio, E.; Gortázar, C. Leishmania infantum in free-ranging hares, Spain, 2004–2010. Eurosurveillance 2013, 18, 20541. [Google Scholar] [CrossRef] [PubMed]
- Tsokana, C.N.; Sokos, C.K.; Giannakopoulos, A.; Mamuris, Z.; Birtsas, P.; Papaspyropoulos, K.; Valiakos, G.; Spyrou, V.; Lefkaditis, M.; Chatzopoulos, D.C.; et al. First evidence of Leishmania infection in European brown hare (Lepus europaeus) in Greece: GIS analysis and phylogenetic position within the Leishmania spp. Parasitol. Res. 2015, 115, 313–321. [Google Scholar] [CrossRef] [PubMed]
- Rocchigiani, G.; Ebani, V.V.; Nardoni, S.; Bertelloni, F.; Bascherini, A.; Leoni, A.; Mancianti, F.; Poli, A. Molecular survey on the occurrence of arthropod-borne pathogens in wild brown hares (Lepus europaeus) from Central Italy. Infect. Genet. Evol. J. Mol. Epidemiol. Evol. Genet. Infect. Dis. 2018, 59, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Hoverman, J.T.; Searle, C.L. Behavioural influences on disease risk: Implications for conservation and management. Anim. Behav. 2016, 120, 263–271. [Google Scholar] [CrossRef]
- Tomassone, L.; Berriatua, E.; De Sousa, R.; Duscher, G.G.; Mihalca, A.D.; Silaghi, C.; Sprong, H.; Zintl, A. Neglected vector-borne zoonoses in Europe: Into the wild. Vet. Parasitol. 2018, 251, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Dubey, J.P. Toxoplasmosis of Animals and Humans, 3rd ed.; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2021. [Google Scholar]
- Almeria, S.; Dubey, J.P. Foodborne transmission of Toxoplasma gondii infection in the last decade. An overview. Res. Vet. Sci. 2021, 135, 371–385. [Google Scholar] [CrossRef] [PubMed]
- Almeria, S.; Murata, F.H.A.; Cerqueira-Cézar, C.K.; Kwok, O.C.H.; Shipley, A.; Dubey, J.P. Epidemiological and Public Health Significance of Toxoplasma gondii Infection in Wild Rabbits and Hares: 2010–2020. Microorganisms 2021, 9, 597. [Google Scholar] [CrossRef]
- do Nascimento, L.C.; Pena, H.F.J.; Leite Filho, R.V.; Argenta, F.F.; Alves, B.F.; Oliveira, S.; Gennari, S.M.; Driemeier, D. Rare case of acute toxoplasmosis in a domestic rabbit (Oryctolagus cuniculus) in Brazil associated with the type BrIII Brazilian clonal lineage of Toxoplasma gondii. Parasitol. Res. 2017, 116, 2873–2876. [Google Scholar] [CrossRef]
- Ebani, V.V.; Poli, A.; Rocchigiani, G.; Bertelloni, F.; Nardoni, S.; Papini, R.A.; Mancianti, F. Serological survey on some pathogens in wild brown hares (Lepus europaeus) in Central Italy. Asian Pac. J. Trop. Med. 2016, 9, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Goethert, H.K.; Telford, S.R., 3rd. Enzootic transmission of Anaplasma bovis in Nantucket cottontail rabbits. J. Clin. Microbiol. 2003, 41, 3744–3747. [Google Scholar] [CrossRef]
- Yabsley, M.J.; Romines, J.; Nettles, V.F. Detection of Babesia and Anaplasma species in rabbits from Texas and Georgia, USA. Vector Borne Zoonotic Dis. 2006, 6, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Zhan, L.; Chu, C.Y.; Zuo, S.Q.; Wu, X.M.; Dumler, J.S.; Jia, N.; Jiang, B.G.; Yang, H.; Cao, W.C. Anaplasma phagocytophilum and Borrelia burgdorferi in rabbits from southeastern China. Vet. Parasitol. 2009, 162, 354–356. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, K.M.; Foley, J.E.; Kasten, R.W.; Chomel, B.B.; Larsen, R.S. Prevalence of Vector-borne Bacterial Pathogens in Riparian Brush Rabbits (Sylvilagus bachmani riparius) and their Ticks. J. Wildl. Dis. 2014, 50, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Homer, M.J.; Aguilar-Delfin, I.; Telford, S.R., 3rd; Krause, P.J.; Persing, D.H. Babesiosis. Clin. Microbiol. Rev. 2000, 13, 451–469. [Google Scholar] [CrossRef]
- Kjemtrup, A.M.; Thomford, J.; Robinson, T.; Conrad, P.A. Phylogenetic relationships of human and wildlife piroplasm isolates in the western United States inferred from the 18S nuclear small subunit RNA gene. Parasitology 2000, 120, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Florin-Christensen, M.; Schnittger, L. Piroplasmids and ticks: A long-lasting intimate relationship. Front. Biosci. 2009, 14, 3064–3073. [Google Scholar] [CrossRef] [PubMed]
- Gray, J.; Zintl, A.; Hildebrandt, A.; Hunfeld, K.-P.; Weiss, L. Zoonotic babesiosis Overview of the disease and novel aspects of pathogen identity. Ticks Tick-Borne Dis. 2010, 1, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Young, K.M.; Corrin, T.; Wilhelm, B.; Uhland, C.; Greig, J.; Mascarenhas, M.; Waddell, L.A. Zoonotic Babesia: A scoping review of the global evidence. PLoS ONE 2019, 14, e0226781. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, J.A.; Rojas, C.; Figueroa, J.V. Diagnostic Tools for the Identification of Babesia sp. in Persistently Infected Cattle. Pathogens 2019, 8, 143. [Google Scholar] [CrossRef]
- Baldani, C.; Machado, R.; Raso, T.; Pinto, A. Serodiagnosis of Babesia equi in horses submitted to exercise stress. Pesqui. Vet. Bras.-CBPA 2007, 27, 179–183. [Google Scholar] [CrossRef][Green Version]
- Curry, P.S.; Elkin, B.T.; Campbell, M.; Nielsen, K.; Hutchins, W.; Ribble, C.; Kutz, S.J. Filter-paper blood samples for ELISA detection of Brucella antibodies in caribou. J. Wildl. Dis. 2011, 47, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Woodford, M.H. Post-Mortem Procedures for Wildlife Veterinarians and Field Biologists; Office International des Epizooties: Paris, France, 1999. [Google Scholar]
- Sarran, D.; Greig, D.; Rios, C.; Zabka, T.; Gulland, F. Evaluation of Aqueous Humor as a Surrogate for Serum Biochemistry in California Sea Lions (Zalophus californianus). Aquat. Mamm. 2008, 34, 157. [Google Scholar] [CrossRef]
- Akiyama, T.; Ohta, N. Parasite-specific antibody profile in the aqueous humor of rabbits with ocular toxocariasis. Parasitol. Int. 2010, 59, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Aston, E.J.; Mayor, P.; Bowman, D.D.; Mohammed, H.O.; Liotta, J.L.; Kwok, O.; Dubey, J.P. Use of filter papers to determine seroprevalence of Toxoplasma gondii among hunted ungulates in remote Peruvian Amazon. Int. J. Parasitol. Parasites Wildl. 2014, 3, 15–19. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dubay, S.; Rosenstock, S.; Stallknecht, D.; Devos, J. Determining Prevalence of Bluetongue and Epizootic Hemorrhagic Disease Viruses in Mule Deer in Arizona (USA) Using Whole Blood Dried on Paper Strips Compared to Serum Analyses. J. Wildl. Dis. 2006, 42, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Elmore, S.A.; Huyvaert, K.P.; Bailey, L.L.; Milhous, J.; Alisauskas, R.T.; Gajadhar, A.A.; Jenkins, E.J. Toxoplasma gondii exposure in arctic-nesting geese: A multi-state occupancy framework and comparison of serological assays. Int. J. Parasitol. Parasites Wildl. 2014, 3, 147–153. [Google Scholar] [CrossRef]
- García-Alonso, M.; Blanco, A.; Reina, D.; Serrano, F.J.; Alonso, C.; Nieto, C.G. Immunopathology of the uveitis in canine leishmaniasis. Parasite Immunol. 1996, 18, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Garweg, J.G.; Boehnke, M. The antibody response in experimental ocular toxoplasmosis. Graefes Arch. Clin. Exp. Ophthalmol. 2006, 244, 1668–1679. [Google Scholar] [CrossRef][Green Version]
- Jakubek, E.B.; Mattsson, R.; Mörner, T.; Mattsson, J.G.; Gavier-Widén, D. Potential application of serological tests on fluids from carcasses: Detection of antibodies against Toxoplasma gondii and Sarcoptes scabiei in red foxes (Vulpes vulpes). Acta Vet. Scand. 2012, 54, 13. [Google Scholar] [CrossRef]
- Athanasiou, L.V.; Christodoulopoulos, G.; Polizopoulou, Z.S.; Kalaitzakis, E.; Papadakis, S.M.; Karatzia, M.A.; Katsogiannou, E.G.; Katsoulos, P.D. Post mortem aqueous humor analysis in sheep as index of ante mortem serum biochemistry profile. Small Rumin. Res. 2018, 159, 52–55. [Google Scholar] [CrossRef]
- Chen, K.; Li, X.; Wang, D.; Ma, Y.; Chen, B.; Wang, Q.; Ma, J.; Guan, M. The diagnostic value of IL-10 and IL-6 level in vitreous fluid and aqueous humor for vitreoretinal lymphoma. Clin. Chim. Acta Int. J. Clin. Chem. 2021, 515, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Kim, M.E.; Polski, A.; Prabakar, R.K.; Shen, L.; Peng, C.-C.; Reid, M.; Chevez-Barrios, P.; Kim, J.; Kuhn, P.; et al. Establishing Clinical Utility of ctDNA Analysis for Diagnosis, Prognosis, and Treatment Monitoring of Retinoblastoma: The Aqueous Humor Liquid Biopsy. Cancers 2021, 13, 1282. [Google Scholar] [CrossRef] [PubMed]
- Felten, S.; Matiasek, K.; Gruendl, S.; Sangl, L.; Hartmann, K. Utility of an immunocytochemical assay using aqueous humor in the diagnosis of feline infectious peritonitis. Vet. Ophthalmol. 2018, 21, 27–34. [Google Scholar] [CrossRef]
- Powell, C.C.; McInnis, C.L.; Fontenelle, J.P.; Lappin, M.R. Bartonella species, feline herpesvirus-1, and Toxoplasma gondii PCR assay results from blood and aqueous humor samples from 104 cats with naturally occurring endogenous uveitis. J. Feline Med. Surg. 2010, 12, 923–928. [Google Scholar] [CrossRef]
- Wiggans, K.T.; Vernau, W.; Lappin, M.R.; Thomasy, S.M.; Maggs, D.J. Diagnostic utility of aqueocentesis and aqueous humor analysis in dogs and cats with anterior uveitis. Vet. Ophthalmol. 2014, 17, 212–220. [Google Scholar] [CrossRef]
- Tsakmakidis, Ι.; Pavlou, C.; Tamvakis, A.; Papadopoulos, T.; Christodoulou, V.; Angelopoulou, K.; Dovas, C.I.; Antoniou, Μ.; Anastasakis, C.; Diakou, A. Leishmania infection in lagomorphs and minks in Greece. Vet. Parasitol. Reg. Stud. Rep. 2019, 16, 100279. [Google Scholar] [CrossRef] [PubMed]
- Vasios, G.K.; Antoniadis, I.; Zevgolis, Y.; Giaginis, G.; Troumbis, A.Y. Turning a Problem into an Opportunity Through Tourism and Marketing: The Case of Wild Rabbits in Lemnos Island, Greece. In Strategic Innovative Marketing and Tourism; Kavoura, A., Kefallonitis, E., Theodoridis, P., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 677–686. [Google Scholar]
- ELGA. Compensation Statistical Data for 2007. Available online: http://www.elga.gr/index.php?option=com_phocadownload&view=category&id=16&Itemid=103 (accessed on 10 November 2021).
- Hadjigeorgiou, I.; Chatzigrorgiou, T.; Kosmas, C.; Kairis, O. Report on Lemnos Wild Rabbit Population; Agricultural University of Athens: Athens, Greece, 2018. [Google Scholar]
- Ministerial. Decision HMEE/DFM 71082/539/2019 (GG3137/B/6-8-2019): Hunting Arrangements for the Hunting Season 2019–2020. Available online: https://dasarxeio.com/wp-content/uploads/2019/08/71082_539_2019.pdf (accessed on 10 November 2021).
- García, N.; Moreno, I.; Alvarez, J.; de la Cruz, M.L.; Navarro, A.; Pérez-Sancho, M.; García-Seco, T.; Rodríguez-Bertos, A.; Conty, M.L.; Toraño, A.; et al. Evidence of Leishmania infantum infection in rabbits (Oryctolagus cuniculus) in a natural area in Madrid, Spain. BioMed Res. Int. 2014, 2014, 318254. [Google Scholar] [CrossRef]
- Almería, S.; Calvete, C.; Pagés, A.; Gauss, C.; Dubey, J.P. Factors affecting the seroprevalence of Toxoplasma gondii infection in wild rabbits (Oryctolagus cuniculus) from Spain. Vet. Parasitol. 2004, 123, 265–270. [Google Scholar] [CrossRef]
- Varloud, M.; Liebenberg, J.; Fourie, J. Early Babesia canis transmission in dogs within 24 h and 8 h of infestation with infected pre-activated male Dermacentor reticulatus ticks. Parasites Vectors 2018, 11, 41. [Google Scholar] [CrossRef]
- Gardner, I.A.; Greiner, M. Receiver-operating characteristic curves and likelihood ratios: Improvements over traditional methods for the evaluation and application of veterinary clinical pathology tests. Vet. Clin. Pathol. 2006, 35, 8–17. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Watson, P.F.; Petrie, A. Method agreement analysis: A review of correct methodology. Theriogenology 2010, 73, 1167–1179. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Martinez, N. The Lagomorph Fossil Record and the Origin of the European Rabbit. In Lagomorph Biology; Alves, P.C., Ferrand, N., Hackländer, K., Eds.; Springer: Berlin/Heidelberg, Germany, 2008; pp. 27–46. [Google Scholar]
- Athanasiou, L.V.; Kontos, V.I.; Saridomichelakis, M.N.; Rallis, T.S.; Diakou, A. A cross-sectional sero-epidemiological study of canine leishmaniasis in Greek mainland. Acta Trop. 2012, 122, 291–295. [Google Scholar] [CrossRef]
- Symeonidou, I.; Angelou, A.; Theodoridis, A.; Sioutas, G.; Papadopoulos, E. Canine Leishmaniosis in Greece: An Updated Countrywide Serological Study and Associated Risk Factors. Pathogens 2021, 10, 1129. [Google Scholar] [CrossRef] [PubMed]
- Chitimia, L.; Muñoz-García, C.I.; Sánchez-Velasco, D.; Lizana, V.; Del Río, L.; Murcia, L.; Fisa, R.; Riera, C.; Giménez-Font, P.; Jiménez-Montalbán, P.; et al. Cryptic Leishmaniosis by Leishmania infantum, a feature of canines only? A study of natural infection in wild rabbits, humans and dogs in southeastern Spain. Vet. Parasitol. 2011, 181, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Sáez, V.; Merino-Espinosa, G.; Morales-Yuste, M.; Corpas-López, V.; Pratlong, F.; Morillas-Márquez, F.; Martín-Sánchez, J. High rates of Leishmania infantum and Trypanosoma nabiasi infection in wild rabbits (Oryctolagus cuniculus) in sympatric and syntrophic conditions in an endemic canine leishmaniasis area: Epidemiological consequences. Vet. Parasitol. 2014, 202, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Moreno, I.; Álvarez, J.; García, N.; de la Fuente, S.; Martínez, I.; Marino, E.; Toraño, A.; Goyache, J.; Vilas, F.; Domínguez, L.; et al. Detection of anti-Leishmania infantum antibodies in sylvatic lagomorphs from an epidemic area of Madrid using the indirect immunofluorescence antibody test. Vet. Parasitol. 2014, 199, 264–267. [Google Scholar] [CrossRef]
- Ortega-García, M.V.; Salguero, F.J.; Rodríguez-Bertos, A.; Moreno, I.; García, N.; García-Seco, T.; Luz Torre, G.; Domínguez, L.; Domínguez, M. A pathological study of Leishmania infantum natural infection in European rabbits (Oryctolagus cuniculus) and Iberian hares (Lepus granatensis). Transbound. Emerg. Dis. 2019, 66, 2474–2481. [Google Scholar] [CrossRef]
- Abbate, J.M.; Arfuso, F.; Napoli, E.; Gaglio, G.; Giannetto, S.; Latrofa, M.S.; Otranto, D.; Brianti, E. Leishmania infantum in wild animals in endemic areas of southern Italy. Comp. Immunol. Microbiol. Infect. Dis. 2019, 67, 101374. [Google Scholar] [CrossRef] [PubMed]
- Ortega, M.V.; Moreno, I.; Domínguez, M.; de la Cruz, M.L.; Martín, A.B.; Rodríguez-Bertos, A.; López, R.; Navarro, A.; González, S.; Mazariegos, M.; et al. Application of a specific quantitative real-time PCR (qPCR) to identify Leishmania infantum DNA in spleen, skin and hair samples of wild Leporidae. Vet. Parasitol. 2017, 243, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Risueño, J.; Ortuño, M.; Pérez-Cutillas, P.; Goyena, E.; Maia, C.; Cortes, S.; Campino, L.; Bernal, L.J.; Muñoz, C.; Arcenillas, I.; et al. Epidemiological and genetic studies suggest a common Leishmania infantum transmission cycle in wildlife, dogs and humans associated to vector abundance in Southeast Spain. Vet. Parasitol. 2018, 259, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Dubey, J.P. Toxoplasmosis of Animals and Humans, 2nd ed.; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2010. [Google Scholar]
- Salman, D.; Oohashi, E.; Mohamed, A.E.A.; Abd El-Mottelib, A.E.-R.; Okada, T.; Igarashi, M. Seroprevalences of Toxoplasma gondii and Neospora caninum in pet rabbits in Japan. J. Vet. Med. Sci. 2014, 76, 855–862. [Google Scholar] [CrossRef]
- Harfoush, M.; Tahoon Ael, N. Seroprevalence of Toxoplasma gondii antibodies in domestic ducks, free-range chickens, turkeys and rabbits in Kafr El-Sheikh Governorate Egypt. J. Egypt. Soc. Parasitol. 2010, 40, 295–302. [Google Scholar]
- Mason, S.; Dubey, J.P.; Smith, J.E.; Boag, B. Toxoplasma gondii coinfection with diseases and parasites in wild rabbits in Scotland. Parasitology 2015, 142, 1415–1421. [Google Scholar] [CrossRef] [PubMed]
- Waap, H.; Nunes, T.; Vaz, Y.; Leitão, A. Serological survey of Toxoplasma gondii and Besnoitia besnoiti in a wildlife conservation area in southern Portugal. Vet. Parasitol. Reg. Stud. Rep. 2016, 3–4, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Coelho, C.; Vieira-Pinto, M.; Vilares, A.; Gargaté, M.J.; Rodrigues, M.; Cardoso, L.; Lopes, A.P. PCR Detection of Toxoplasma gondii in European Wild Rabbit (Oryctolagus cuniculus) from Portugal. Microorganisms 2020, 8, 1926. [Google Scholar] [CrossRef]
- Hughes, J.M.; Thomasson, D.; Craig, P.S.; Georgin, S.; Pickles, A.; Hide, G. Neospora caninum: Detection in wild rabbits and investigation of co-infection with Toxoplasma gondii by PCR analysis. Exp. Parasitol. 2008, 120, 255–260. [Google Scholar] [CrossRef]
- Tsiodras, S.; Spanakis, N.; Spanakos, G.; Pervanidou, D.; Georgakopoulou, T.; Campos, E.; Petra, T.; Kanellopoulos, P.; Georgiadis, G.; Antalis, E.; et al. Fatal human anaplasmosis associated with macrophage activation syndrome in Greece and the Public Health response. J. Infect. Public Health 2017, 10, 819–823. [Google Scholar] [CrossRef] [PubMed]
- Diakou, A.; Di Cesare, A.; Morelli, S.; Colombo, M.; Halos, L.; Simonato, G.; Tamvakis, A.; Beugnet, F.; Paoletti, B.; Traversa, D. Endoparasites and vector-borne pathogens in dogs from Greek islands: Pathogen distribution and zoonotic implications. PLoS Negl. Trop. Dis. 2019, 13, e0007003. [Google Scholar] [CrossRef] [PubMed]
- Katsogiannou, E.G.; Katsoulos, P.D.; Christodoulopoulos, G.; Polizopoulou, Z.S.; Papadakis, S.M.; Kokkinaki, K.C.; Billinis, C.; Boutsini, S.; Stougiou, D.; Athanasiou, L.V. Quantitative and Morphological Blood Cell Findings Associated with the Presence of Antigen and/or Antibodies Against Anaplasma phagocytophilum in Sheep. Vector Borne Zoonotic Dis. 2021, 21, 321–329. [Google Scholar] [CrossRef]
- Snellgrove, A.N.; Krapiunaya, I.; Ford, S.L.; Stanley, H.M.; Wickson, A.G.; Hartzer, K.L.; Levin, M.L. Vector competence of Rhipicephalus sanguineus sensu stricto for Anaplasma platys. Ticks Tick-Borne Dis. 2020, 11, 101517. [Google Scholar] [CrossRef]
- Goethert, H.K.; Telford, S.R., 3rd. Enzootic transmission of the agent of human granulocytic ehrlichiosis among cottontail rabbits. Am. J. Trop. Med. Hyg. 2003, 68, 633–637. [Google Scholar] [CrossRef] [PubMed]
- Goethert, H.K.; Telford, S.R., 3rd. Enzootic transmission of Babesia divergens among cottontail rabbits on Nantucket Island, Massachusetts. Am. J. Trop. Med. Hyg. 2003, 69, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Fritzen, C.; Mosites, E.; Applegate, R.D.; Telford, S.R., 3rd; Huang, J.; Yabsley, M.J.; Carpenter, L.R.; Dunn, J.R.; Moncayo, A.C. Environmental investigation following the first human case of babesiosis in Tennessee. J. Parasitol. 2014, 100, 106–109. [Google Scholar] [CrossRef]
- Kouam, M.K.; Kantzoura, V.; Gajadhar, A.A.; Theis, J.H.; Papadopoulos, E.; Theodoropoulos, G. Seroprevalence of equine piroplasms and host-related factors associated with infection in Greece. Vet. Parasitol. 2010, 169, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, B.; Brossard, M.; Perié, N.M. Piroplasms of domestic animals in the Macedonia region of Greece 3. Piroplasms of small ruminants. Vet. Parasitol. 1996, 63, 67–74. [Google Scholar] [CrossRef]
- Papadopoulos, B.; Brossard, M.; Perié, N.M. Piroplasms of domestic animals in the Macedonia region of Greece 2. Piroplasms of cattle. Vet. Parasitol. 1996, 63, 57–66. [Google Scholar] [CrossRef]
- Turunen, H.J.; Leinikki, P.O.; Saari, K.M. Demonstration of intraocular synthesis of immunoglobulin G toxoplasma antibodies for specific diagnosis of toxoplasmic chorioretinitis by enzyme immunoassay. J. Clin. Microbiol. 1983, 17, 988–992. [Google Scholar] [CrossRef] [PubMed]
- Meunier, V.; Jourda, S.; Deville, M.; Guillot, J. Prevalence of anti-Toxoplasma gondii antibodies in serum and aqueous humor samples from cats with uveitis or systemic diseases in France. Vet. Parasitol. 2006, 138, 362–365. [Google Scholar] [CrossRef]
- Ragg, S.; Key, M.; Rankin, F.; WuDunn, D. The Effect of Molecular Weight on Passage of Proteins Through the Blood-Aqueous Barrier. Investig. Ophthalmol. Vis. Sci. 2019, 60, 1461–1469. [Google Scholar] [CrossRef]
- Brito, F.L.C.; Alves, L.C.; Maia, F.C.L.; Santos, E.S.C.; Laus, J.L.; Meunier, I. Ocular alterations in dogs naturally infected by Leishmania (Leishmania) chagasi. Arq. Bras. Med. Vet. Zootec. 2006, 58, 768–775. [Google Scholar] [CrossRef][Green Version]
| Serum | Aqueous Humor | |||||
|---|---|---|---|---|---|---|
| Cut Off Value | Positive | Cut Off Value | Positive | |||
| N | % | N | % | |||
| L. infantum | 1:25 | 3 | 4.2 | 1:25 | 1 | 1.3 |
| 1:10 | 1 | 1.3 | ||||
| T. gondii | 1:25 | 4 | 5.5 | 1:25 | 1 | 1.3 |
| 1:10 | 1 | 1.3 | ||||
| A. phagocytophilum | 1:25 | 13 | 18 | 1:25 | 4 | 5.5 |
| 1:10 | 6 | 8.3 | ||||
| B. caballi | 1:50 | 7 | 9.7 | 1:50 | 2 | 2.7 |
| 1:10 | 3 | 4.2 | ||||
| S-AH1 | S-AH2 | |
|---|---|---|
| L. infantum | 0.489 | 0.489 |
| T. gondii | 0.386 | 0.386 |
| A. phagocytophilum | 0.421 | 0.584 |
| B. caballi | 0.419 | 0.575 |
| L. infantum | T. gondii | A. phagocytophilum | B. caballi | |
|---|---|---|---|---|
| Sensitivity (%) | 33.33 | 25.00 | 30.77 | 28.57 |
| 95% CI | 0.84–90.57 | 0.63–80.59 | 9.09–61.43 | 3.67–70.96 |
| Specificity (%) | 100.00 | 100.00 | 100.00 | 100.00 |
| 95% CI | 94.79–100.00 | 94.72–100.00 | 93.94–100.00 | 94.48–100.00 |
| PLR | - | - | - | - |
| 95% CI | - | - | - | - |
| NLR | 0.67 | 0.75 | 0.69 | 0.71 |
| 95% CI | 0.30–1.48 | 0.43–1.32 | 0.48–0.99 | 0.45–1.14 |
| L. infantum | T. gondii | A. phagocytophilum | B. caballi | |
|---|---|---|---|---|
| Sensitivity (%) | 60.00 | 25.00 | 38.46 | 28.57 |
| 95% CI | 14.66–94.73 | 0.63–80.59 | 13.86–68.42 | 3.67–70.96 |
| Specificity (%) | 100.00 | 100.00 | 98.31 | 98.46 |
| 95% CI | 94.79–100.00 | 94.72–100.00 | 90.91–99.96 | 91.72–99.96 |
| PLR | - | - | 22.69 | 18.57 |
| 95% CI | - | - | 2.89–178.29 | 1.92–179.82 |
| NLR | 0.40 | 0.75 | 0.63 | 0.73 |
| 95% CI | 0.14–1.17 | 0.43–1.32 | 0.41–0.96 | 0.45–1.16 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Athanasiou, L.V.; Katsogiannou, E.G.; Tsokana, C.N.; Boutsini, S.G.; Bisia, M.G.; Papatsiros, V.G. Wild Rabbit Exposure to Leishmania infantum, Toxoplasma gondii, Anaplasma phagocytophilum and Babesia caballi Evidenced by Serum and Aqueous Humor Antibody Detection. Microorganisms 2021, 9, 2616. https://doi.org/10.3390/microorganisms9122616
Athanasiou LV, Katsogiannou EG, Tsokana CN, Boutsini SG, Bisia MG, Papatsiros VG. Wild Rabbit Exposure to Leishmania infantum, Toxoplasma gondii, Anaplasma phagocytophilum and Babesia caballi Evidenced by Serum and Aqueous Humor Antibody Detection. Microorganisms. 2021; 9(12):2616. https://doi.org/10.3390/microorganisms9122616
Chicago/Turabian StyleAthanasiou, Labrini V., Eleni G. Katsogiannou, Constantina N. Tsokana, Sofia G. Boutsini, Marina G. Bisia, and Vasileios G. Papatsiros. 2021. "Wild Rabbit Exposure to Leishmania infantum, Toxoplasma gondii, Anaplasma phagocytophilum and Babesia caballi Evidenced by Serum and Aqueous Humor Antibody Detection" Microorganisms 9, no. 12: 2616. https://doi.org/10.3390/microorganisms9122616
APA StyleAthanasiou, L. V., Katsogiannou, E. G., Tsokana, C. N., Boutsini, S. G., Bisia, M. G., & Papatsiros, V. G. (2021). Wild Rabbit Exposure to Leishmania infantum, Toxoplasma gondii, Anaplasma phagocytophilum and Babesia caballi Evidenced by Serum and Aqueous Humor Antibody Detection. Microorganisms, 9(12), 2616. https://doi.org/10.3390/microorganisms9122616








