Clinical Detection of Chronic Rhinosinusitis through Next-Generation Sequencing of the Oral Microbiota
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Recruitment
2.2. Saliva and Nasal Swab of DNA Extraction
2.3. PCR Amplification and 16S Sequencing
2.4. Bioinformatics Analysis
3. Results
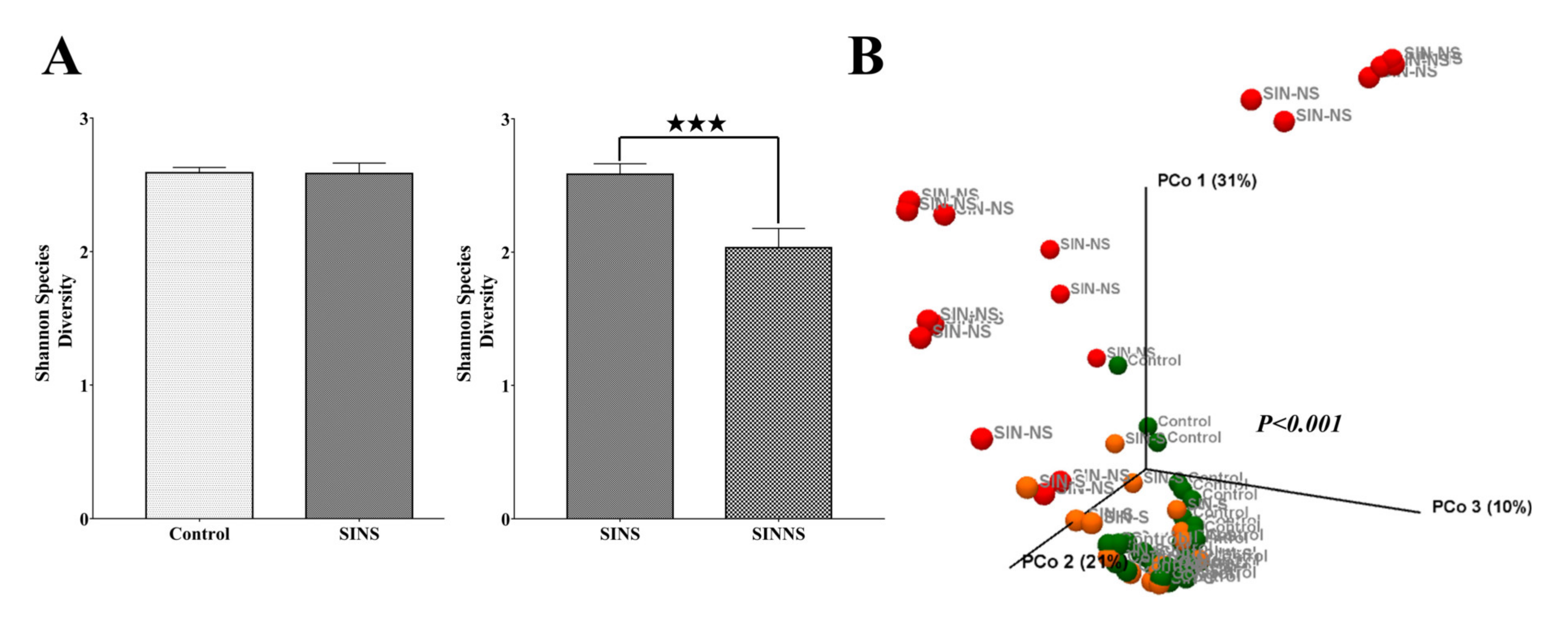
3.1. CRS Patients Had a Lower Diversity of the Nasal Microbiome
3.2. Operational Taxonomic Units (OTUs) of the Phylum and Species Level among Different Groups
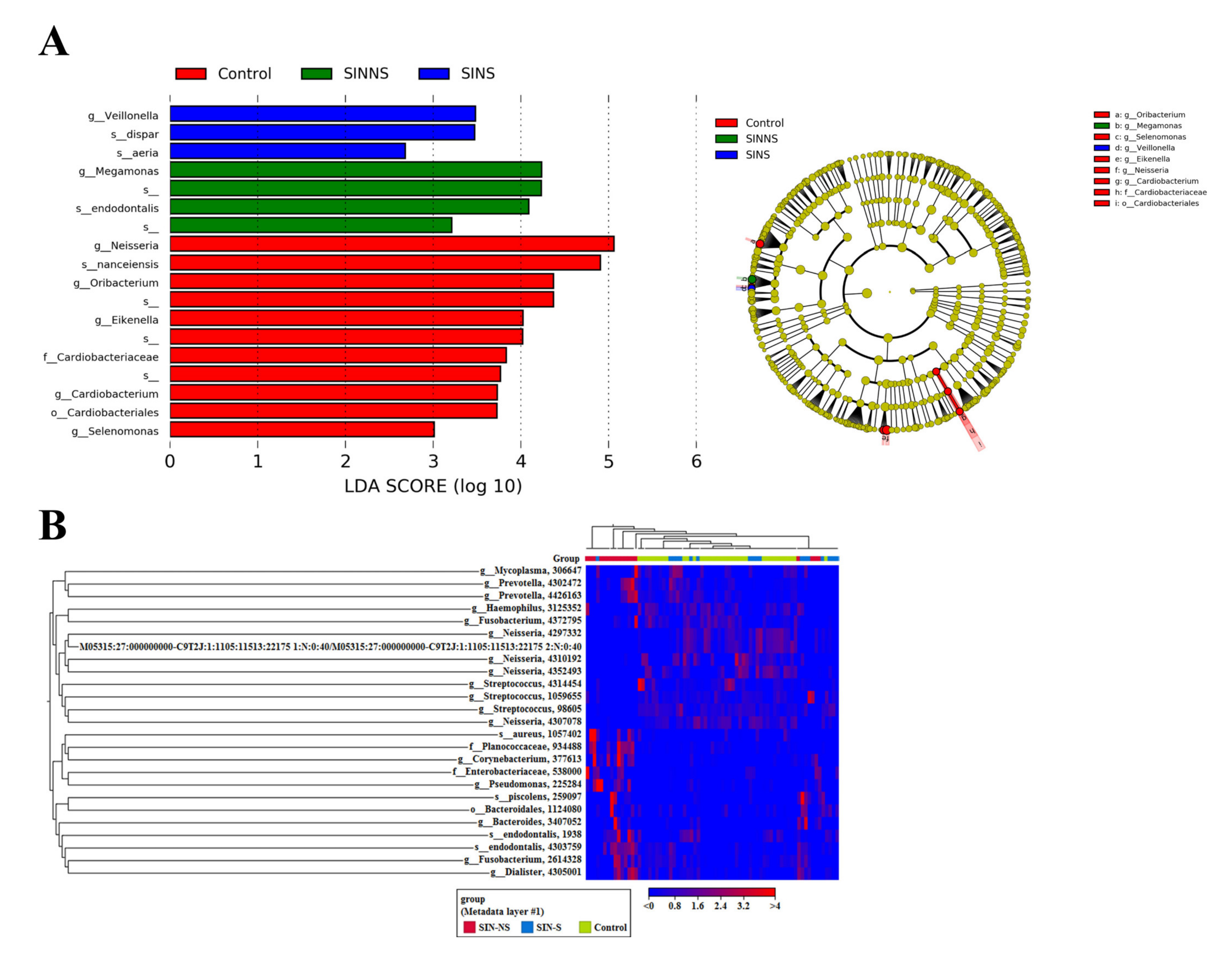
3.3. Specific Microbial Markers in CRS Patients
3.4. A Novel Microbial Ratio from Saliva to Distinguish CRS Patients from the Control Group
3.5. Microbiome-Related Functional Pathways in Chronic Rhinosinusitis
3.6. Comparison of Clinical Aerobic Culture and NGS Approaches
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- DeConde, A.S.; Soler, Z.M. Chronic rhinosinusitis: Epidemiology and burden of disease. Am. J. Rhinol. Allergy 2016, 30, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, N. Incremental health care utilization and expenditures for chronic rhinosinusitis in the United States. Ann. Otol. Rhinol. Laryngol. 2011, 120, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Sivasubramaniam, R.; Douglas, R. The microbiome and chronic rhinosinusitis. World J. Otorhinolaryngol. Head Neck Surg. 2018, 4, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Brook, I. Microbiology of sinusitis. Proc. Am. Thorac. Soc. 2011, 8, 90–100. [Google Scholar] [CrossRef]
- Hoggard, M.; Wagner Mackenzie, B.; Jain, R.; Taylor, M.W.; Biswas, K.; Douglas, R.G. Chronic Rhinosinusitis and the Evolving Understanding of Microbial Ecology in Chronic Inflammatory Mucosal Disease. Clin. Microbiol. Rev. 2017, 30, 321–348. [Google Scholar] [CrossRef]
- Aas, J.A.; Paster, B.J.; Stokes, L.N.; Olsen, I.; Dewhirst, F.E. Defining the normal bacterial flora of the oral cavity. J. Clin. Microbiol. 2005, 43, 5721–5732. [Google Scholar] [CrossRef]
- Lim, Y.; Totsika, M.; Morrison, M.; Punyadeera, C. Oral Microbiome: A New Biomarker Reservoir for Oral and Oropharyngeal Cancers. Theranostics 2017, 7, 4313–4321. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, X.; Li, H.; Ni, C.; Du, Z.; Yan, F. Human oral microbiota and its modulation for oral health. Biomed. Pharm. 2018, 99, 883–893. [Google Scholar] [CrossRef]
- Wade, W.G. The oral microbiome in health and disease. Pharm. Res. 2013, 69, 137–143. [Google Scholar] [CrossRef]
- He, J.; Li, Y.; Cao, Y.; Xue, J.; Zhou, X. The oral microbiome diversity and its relation to human diseases. Folia Microbiol. (Praha) 2015, 60, 69–80. [Google Scholar] [CrossRef]
- Shoemark, D.K.; Allen, S.J. The microbiome and disease: Reviewing the links between the oral microbiome, aging, and Alzheimer’s disease. J. Alzheimers Dis. 2015, 43, 725–738. [Google Scholar] [CrossRef] [PubMed]
- Feazel, L.M.; Robertson, C.E.; Ramakrishnan, V.R.; Frank, D.N. Microbiome complexity and Staphylococcus aureus in chronic rhinosinusitis. Laryngoscope 2012, 122, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, M.F.; Mfuna, L.; Dowd, S.E.; Wolcott, R.D.; Barbeau, J.; Poisson, M.; James, G.; Desrosiers, M. Molecular characterization of the polymicrobial flora in chronic rhinosinusitis. J. Otolaryngol. Head Neck Surg. 2010, 39, 182–187. [Google Scholar]
- Vaughn, A.; Shaver, C.; Clark, D. Association Between Culture and Culture-Independent Microtyping in Recalcitrant Chronic Rhinosinusitis. Ear Nose Throat J. 2019, 98, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Jervis Bardy, J.; Psaltis, A.J. Next Generation Sequencing and the Microbiome of Chronic Rhinosinusitis: A Primer for Clinicians and Review of Current Research, Its Limitations, and Future Directions. Ann. Otol Rhinol. Laryngol. 2016, 125, 613–621. [Google Scholar] [CrossRef]
- Mosca, A.; Leclerc, M.; Hugot, J.P. Gut Microbiota Diversity and Human Diseases: Should We Reintroduce Key Predators in Our Ecosystem? Front. Microbiol. 2016, 7, 455. [Google Scholar] [CrossRef]
- Kriss, M.; Hazleton, K.Z.; Nusbacher, N.M.; Martin, C.G.; Lozupone, C.A. Low diversity gut microbiota dysbiosis: Drivers, functional implications and recovery. Curr. Opin. Microbiol. 2018, 44, 34–40. [Google Scholar] [CrossRef]
- Mombelli, A. Microbial colonization of the periodontal pocket and its significance for periodontal therapy. Periodontol. 2000 2018, 76, 85–96. [Google Scholar] [CrossRef]
- Costalonga, M.; Herzberg, M.C. The oral microbiome and the immunobiology of periodontal disease and caries. Immunol. Lett. 2014, 162, 22–38. [Google Scholar] [CrossRef]
- Hoggard, M.; Biswas, K.; Zoing, M.; Wagner Mackenzie, B.; Taylor, M.W.; Douglas, R.G. Evidence of microbiota dysbiosis in chronic rhinosinusitis. Int. Forum Allergy Rhinol. 2017, 7, 230–239. [Google Scholar] [CrossRef]
- Wagner Mackenzie, B.; Waite, D.W.; Hoggard, M.; Douglas, R.G.; Taylor, M.W.; Biswas, K. Bacterial community collapse: A meta-analysis of the sinonasal microbiota in chronic rhinosinusitis. Environ. Microbiol. 2017, 19, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Dewhirst, F.E.; Chen, T.; Izard, J.; Paster, B.J.; Tanner, A.C.; Yu, W.H.; Lakshmanan, A.; Wade, W.G. The human oral microbiome. J. Bacteriol. 2010, 192, 5002–5017. [Google Scholar] [CrossRef] [PubMed]
- Mager, D.L.; Haffajee, A.D.; Devlin, P.M.; Norris, C.M.; Posner, M.R.; Goodson, J.M. The salivary microbiota as a diagnostic indicator of oral cancer: A descriptive, non-randomized study of cancer-free and oral squamous cell carcinoma subjects. J. Transl. Med. 2005, 3, 27. [Google Scholar] [CrossRef] [PubMed]
- Crielaard, W.; Zaura, E.; Schuller, A.A.; Huse, S.M.; Montijn, R.C.; Keijser, B.J. Exploring the oral microbiota of children at various developmental stages of their dentition in the relation to their oral health. BMC Med. Genom. 2011, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- Mancl, K.A.; Kirsner, R.S.; Ajdic, D. Wound biofilms: Lessons learned from oral biofilms. Wound Repair Regen. 2013, 21, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Keijser, B.J.; Zaura, E.; Huse, S.M.; van der Vossen, J.M.; Schuren, F.H.; Montijn, R.C.; ten Cate, J.M.; Crielaard, W. Pyrosequencing analysis of the oral microflora of healthy adults. J. Dent. Res. 2008, 87, 1016–1020. [Google Scholar] [CrossRef]
- Heller, D.; Silva-Boghossian, C.M.; do Souto, R.M.; Colombo, A.P. Subgingival microbial profiles of generalized aggressive and chronic periodontal diseases. Arch. Oral Biol. 2012, 57, 973–980. [Google Scholar] [CrossRef]
- Mashima, I.; Fujita, M.; Nakatsuka, Y.; Kado, T.; Furuichi, Y.; Sulistyani, H.; Nakazawa, F. Original Research Article The Distribution and Frequency of Oral Veillonella spp. Assoc. Chronic Periodontitis 2015, 4, 150–160. [Google Scholar]
- Matera, G.; Muto, V.; Vinci, M.; Zicca, E.; Abdollahi-Roodsaz, S.; van de Veerdonk, F.L.; Kullberg, B.J.; Liberto, M.C.; van der Meer, J.W.; Foca, A.; et al. Receptor recognition of and immune intracellular pathways for Veillonella parvula lipopolysaccharide. Clin. Vaccine Immunol. 2009, 16, 1804–1809. [Google Scholar] [CrossRef]
- Ready, D.; Pratten, J.; Roberts, A.P.; Bedi, R.; Mullany, P.; Wilson, M. Potential role of Veillonella spp. as a reservoir of transferable tetracycline resistance in the oral cavity. Antimicrob. Agents Chemother. 2006, 50, 2866–2868. [Google Scholar] [CrossRef]
- Ready, D.; Bedi, R.; Mullany, P.; Wilson, M. Penicillin and amoxicillin resistance in oral Veillonella spp. Int. J. Antimicrob. Agents 2012, 40, 188–189. [Google Scholar] [CrossRef] [PubMed]
- Houston, S.; Taylor, D.; Rennie, R. Prosthetic valve endocarditis due to Veillonella dispar: Successful medical treatment following penicillin desensitization. Clin. Infect. Dis. 1997, 24, 1013–1014. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Loughrey, A.C.; Chew, E.W. Endocarditis caused by Veillonella dispar. J. Infect. 1990, 21, 319–321. [Google Scholar] [CrossRef]
- Marchandin, H.; Jean-Pierre, H.; Carriere, C.; Canovas, F.; Darbas, H.; Jumas-Bilak, E. Prosthetic joint infection due to Veillonella dispar. Eur. J. Clin. Microbiol. Infect. Dis. 2001, 20, 340–342. [Google Scholar] [CrossRef] [PubMed]
- Ramanan, P.; Barreto, J.N.; Osmon, D.R.; Tosh, P.K. Rothia bacteremia: A 10-year experience at Mayo Clinic, Rochester, Minnesota. J. Clin. Microbiol. 2014, 52, 3184–3189. [Google Scholar] [CrossRef]
- Lee, A.B.; Harker-Murray, P.; Ferrieri, P.; Schleiss, M.R.; Tolar, J. Bacterial meningitis from Rothia mucilaginosa in patients with malignancy or undergoing hematopoietic stem cell transplantation. Pediatric Blood Cancer 2008, 50, 673–676. [Google Scholar] [CrossRef]
- Morgan, E.A.; Henrich, T.J.; Jarell, A.D.; Shieh, W.J.; Zaki, S.R.; Marty, F.M.; Thorner, A.R.; Milner, D.A.; Velazquez, E.F. Infectious granulomatous dermatitis associated with Rothia mucilaginosa bacteremia: A case report. Am. J. Derm. 2010, 32, 175–179. [Google Scholar] [CrossRef]
- Trivedi, M.N.; Malhotra, P. Rothia prosthetic knee joint infection. J. Microbiol. Immunol. Infect. 2015, 48, 453–455. [Google Scholar] [CrossRef]
- Nambu, T.; Tsuzukibashi, O.; Uchibori, S.; Mashimo, C. Complete Genome Sequence of Rothia mucilaginosa Strain NUM-Rm6536, Isolated from a Human Oral Cavity. Genome Announc. 2015, 3. [Google Scholar] [CrossRef]
- Lombardo Bedran, T.B.; Marcantonio, R.A.; Spin Neto, R.; Alves Mayer, M.P.; Grenier, D.; Spolidorio, L.C.; Spolidorio, D.P. Porphyromonas endodontalis in chronic periodontitis: A clinical and microbiological cross-sectional study. J. Oral Microbiol. 2012, 4, 1–7. [Google Scholar] [CrossRef]
- Cao, H.; Qi, Z.; Jiang, H.; Zhao, J.; Liu, Z.; Tang, Z. Detection of Porphyromonas endodontalis, Porphyromonas gingivalis and Prevotella intermedia in primary endodontic infections in a Chinese population. Int. Endod. J. 2012, 45, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.P.; Pinheiro, E.T.; Jacinto, R.C.; Zaia, A.A.; Ferraz, C.C.; Souza-Filho, F.J. Microbial analysis of canals of root-filled teeth with periapical lesions using polymerase chain reaction. J. Endod. 2008, 34, 537–540. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, J.; Ha, J.; Choi, Y.; Kim, S.; Lee, H.; Yoon, Y.; Choi, K.H. Clinical relevance of infections with zoonotic and human oral species of Campylobacter. J. Microbiol. 2016, 54, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Ma, R.; Wang, Y.; Zhang, L. The Clinical Importance of Campylobacter concisus and Other Human Hosted Campylobacter Species. Front. Cell. Infect. Microbiol. 2018, 8, 243. [Google Scholar] [CrossRef]
- Ambrosioni, J.; Martinez-Garcia, C.; Llopis, J.; Garcia-de-la-Maria, C.; Hernandez-Meneses, M.; Tellez, A.; Falces, C.; Almela, M.; Vidal, B.; Sandoval, E.; et al. HACEK infective endocarditis: Epidemiology, clinical features, and outcome: A case-control study. Int. J. Infect. Dis. 2018, 76, 120–125. [Google Scholar] [CrossRef]
- Bonavent, T.B.; Nielsen, X.C.; Kristensen, K.S.; Ihlemann, N.; Moser, C.; Christensen, J.J. Cardiobacterium hominis and Cardiobacterium valvarum: Two Case Stories with Infective Episodes in Pacemaker Treated Patients. Open Microbiol. J. 2016, 10, 183–187. [Google Scholar] [CrossRef]
- Han, X.Y.; Falsen, E. Characterization of oral strains of Cardiobacterium valvarum and emended description of the organism. J. Clin. Microbiol. 2005, 43, 2370–2374. [Google Scholar] [CrossRef]
- Willis, J.R.; Gabaldon, T. The Human Oral Microbiome in Health and Disease: From Sequences to Ecosystems. Microorganisms 2020, 8, 308. [Google Scholar] [CrossRef]
- Socransky, S.S.; Haffajee, A.D.; Cugini, M.A.; Smith, C.; Kent, R.L., Jr. Microbial complexes in subgingival plaque. J. Clin. Periodontol. 1998, 25, 134–144. [Google Scholar] [CrossRef]
- De Lima, C.O.; Devito, K.L.; Baraky Vasconcelos, L.R.; Prado, M.D.; Campos, C.N. Correlation between Endodontic Infection and Periodontal Disease and Their Association with Chronic Sinusitis: A Clinical-tomographic Study. J. Endod. 2017, 43, 1978–1983. [Google Scholar] [CrossRef]
- Melen, I.; Lindahl, L.; Andreasson, L.; Rundcrantz, H. Chronic maxillary sinusitis. Definition, diagnosis and relation to dental infections and nasal polyposis. Acta Otolaryngol. 1986, 101, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Puglisi, S.; Privitera, S.; Maiolino, L.; Serra, A.; Garotta, M.; Blandino, G.; Speciale, A. Bacteriological findings and antimicrobial resistance in odontogenic and non-odontogenic chronic maxillary sinusitis. J. Med. Microbiol. 2011, 60, 1353–1359. [Google Scholar] [CrossRef] [PubMed]
- Cervin, A.U. The Potential for Topical Probiotic Treatment of Chronic Rhinosinusitis, a Personal Perspective. Front. Cell. Infect. Microbiol. 2017, 7, 530. [Google Scholar] [CrossRef] [PubMed]
- Abreu, N.A.; Nagalingam, N.A.; Song, Y.; Roediger, F.C.; Pletcher, S.D.; Goldberg, A.N.; Lynch, S.V. Sinus microbiome diversity depletion and Corynebacterium tuberculostearicum enrichment mediates rhinosinusitis. Sci. Transl. Med. 2012, 4, 151ra124. [Google Scholar] [CrossRef] [PubMed]
- Habermann, W.; Zimmermann, K.; Skarabis, H.; Kunze, R.; Rusch, V. Reduction of acute recurrence in patients with chronic recurrent hypertrophic sinusitis by treatment with a bacterial immunostimulant (Enterococcus faecalis Bacteriae of human origin. Arzneimittelforschung 2002, 52, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Gluck, U.; Gebbers, J.O. Ingested probiotics reduce nasal colonization with pathogenic bacteria (Staphylococcus aureus, Streptococcus pneumoniae, and beta-hemolytic streptococci). Am. J. Clin. Nutr. 2003, 77, 517–520. [Google Scholar] [CrossRef] [PubMed]
- Hao, Q.; Lu, Z.; Dong, B.R.; Huang, C.Q.; Wu, T. Probiotics for preventing acute upper respiratory tract infections. Cochrane Database Syst. Rev. 2011, 7, 1–9. [Google Scholar] [CrossRef]
- Yang, F.; Zeng, X.; Ning, K.; Liu, K.L.; Lo, C.C.; Wang, W.; Chen, J.; Wang, D.; Huang, R.; Chang, X.; et al. Saliva microbiomes distinguish caries-active from healthy human populations. ISME J. 2012, 6, 1–10. [Google Scholar] [CrossRef]
- Sakamoto, M.; Umeda, M.; Ishikawa, I.; Benno, Y. Comparison of the oral bacterial flora in saliva from a healthy subject and two periodontitis patients by sequence analysis of 16S rDNA libraries. Microbiol. Immunol. 2000, 44, 643–652. [Google Scholar] [CrossRef]
- Pushalkar, S.; Mane, S.P.; Ji, X.; Li, Y.; Evans, C.; Crasta, O.R.; Morse, D.; Meagher, R.; Singh, A.; Saxena, D. Microbial diversity in saliva of oral squamous cell carcinoma. FEMS Immunol. Med. Microbiol. 2011, 61, 269–277. [Google Scholar] [CrossRef]
- Do, T.; Sheehy, E.C.; Mulli, T.; Hughes, F.; Beighton, D. Transcriptomic analysis of three Veillonella spp. present in carious dentine and in the saliva of caries-free individuals. Front. Cell. Infect. Microbiol. 2015, 5, 25. [Google Scholar] [CrossRef] [PubMed]
- Yamane, K.; Nambu, T.; Yamanaka, T.; Mashimo, C.; Sugimori, C.; Leung, K.-P.; Fukushima, H. Complete Genome Sequence of Rothia mucilaginosa DY-18: A Clinical Isolate with Dense Meshwork-Like Structures from a Persistent Apical Periodontitis Lesion. Sequencing 2010, 6. [Google Scholar] [CrossRef][Green Version]
- Abby, S.S.; Cury, J.; Guglielmini, J.; Neron, B.; Touchon, M.; Rocha, E.P. Identification of protein secretion systems in bacterial genomes. Sci. Rep. 2016, 6, 23080. [Google Scholar] [CrossRef] [PubMed]
- Rajagopala, S.V.; Titz, B.; Goll, J.; Parrish, J.R.; Wohlbold, K.; McKevitt, M.T.; Palzkill, T.; Mori, H.; Finley, R.L., Jr.; Uetz, P. The protein network of bacterial motility. Mol. Syst. Biol. 2007, 3, 128. [Google Scholar] [CrossRef] [PubMed]
- Lasserre, J.F.; Brecx, M.C.; Toma, S. Oral Microbes, Biofilms and Their Role in Periodontal and Peri-Implant Diseases. Materials 2018, 11, 1802. [Google Scholar] [CrossRef]
- Peters, B.A.; Wu, J.; Pei, Z.; Yang, L.; Purdue, M.P.; Freedman, N.D.; Jacobs, E.J.; Gapstur, S.M.; Hayes, R.B.; Ahn, J. Oral Microbiome Composition Reflects Prospective Risk for Esophageal Cancers. Cancer Res. 2017, 77, 6777–6787. [Google Scholar] [CrossRef]
- Zhou, P.; Li, X.; Qi, F. Identification and characterization of a haem biosynthesis locus in Veillonella. Microbiology 2016, 162, 1735–1743. [Google Scholar] [CrossRef]
- Shah, H.N.; Gharbia, S.E. Biochemical and chemical studies on strains designated Prevotella intermedia and proposal of a new pigmented species, Prevotella nigrescens sp. nov. Int. J. Syst. Bacteriol. 1992, 42, 542–546. [Google Scholar] [CrossRef]
- Gomes, B.P.; Jacinto, R.C.; Pinheiro, E.T.; Sousa, E.L.; Zaia, A.A.; Ferraz, C.C.; Souza-Filho, F.J. Porphyromonas gingivalis, Porphyromonas endodontalis, Prevotella intermedia and Prevotella nigrescens in endodontic lesions detected by culture and by PCR. Oral Microbiol. Immunol. 2005, 20, 211–215. [Google Scholar] [CrossRef]
- Joss, T.V.; Burke, C.M.; Hudson, B.J.; Darling, A.E.; Forer, M.; Alber, D.G.; Charles, I.G.; Stow, N.W. Bacterial Communities Vary between Sinuses in Chronic Rhinosinusitis Patients. Front. Microbiol. 2015, 6, 1532. [Google Scholar] [CrossRef]
- Koeller, K.; Herlemann, D.P.R.; Schuldt, T.; Ovari, A.; Guder, E.; Podbielski, A.; Kreikemeyer, B.; Olzowy, B. Microbiome and Culture Based Analysis of Chronic Rhinosinusitis Compared to Healthy Sinus Mucosa. Front. Microbiol. 2018, 9, 643. [Google Scholar] [CrossRef] [PubMed]



| SINNS1 | SINNS2 | SINNS3 | SINNS4 | SINNS5 | SINNS6 | SINNS7 | SINNS8 | SINNS9 | SINNS10 | SINNS11 | SINNS12 | SINNS13 | SINNS14 | SINNS15 | SINNS16 | SINNS17 | SINNS18 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Common aerobic culture (Nasopharynx) | Staphylococcus aureus | No beta Streptococcus group A | No beta Streptococcus group A | No beta Streptococcus group A | Pseudomonas aeruginosa | No beta Streptococcus group A | No beta Streptococcus group A | No beta Streptococcus group A | No beta Streptococcus group A | No beta Streptococcus group A | Staphylococcus pneumoniae | No beta Streptococcus group A | No beta Streptococcus group A | Haemophilus influenzae | No beta Streptococcus group A | No beta Streptococcus group A | No beta Streptococcus group A | No beta Streptococcus group A |
| NGS | 62.43% | 48.81% | 0.268% | 2.59% | ||||||||||||||
| NGS: Aerobes | ||||||||||||||||||
| Staphylococcus aureus | 62.43% | 0% | 0.006% | 0% | 0% | 0% | 0% | 0.006% | 0% | 0.341% | 0% | 0.005% | 0% | 0% | 0.003% | 0.105% | 0% | 40.028% |
| Streptococcus pyogenes | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% |
| Streptococcus pneumoniae | 0% | 0% | 0% | 0% | 0% | 0.011% | 0% | 0% | 0% | 0% | 0.268% | 0% | 0.001% | 0% | 0% | 0% | 0% | 0% |
| Haemophilus influenza | 0% | 0% | 0% | 0% | 0% | 21.003% | 0% | 0% | 0% | 0.057% | 0% | 0.001% | 0.01% | 2.59% | 0% | 0% | 0% | 0% |
| Moraxella catarrhalis | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0.001% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% |
| Pseudomonas aeruginosa | 0% | 0% | 0% | 0.001% | 48.81% | 0% | 0.003% | 0.003% | 0% | 0.118% | 0% | 0% | 0% | 0% | 0% | 0.012% | 0.002% | 0.117% |
| NGS: Anaerobes- periodontopathogens | ||||||||||||||||||
| Porphyromonas gingivalis | 0% | 0% | 0% | 0% | 0.001% (Saliva: 2.246%) | 0% | 0% | 0.228% (Saliva: 0.598%) | 0% | 0.042% (Saliva: 0.322%) | 0% | 0% | 0% | 0.023% (Saliva: 0.246%) | 0.001% (Saliva: 0.472%) | 0.001% (Saliva: 0%) | 0.2% (Saliva: 0.097%) | 0% |
| Porphyromonas endodontalis | 0% | 3.352% (Saliva: 0.069%) | 43.814% (Saliva: 0.039%) | 0.008% (Saliva: 0.012%) | 0% | 0.001% (Saliva: 0.14%) | 0.002% (Saliva: 0.03%) | 2.33% (Saliva: 10.161%) | 21.005% (Saliva:0.254 %) | 44.197% (Saliva:0.355 %) | 0.003% (Saliva: 0.245%) | 11.3% (Saliva: 1.223%) | 19.587% (Saliva:0.002 %) | 15.89% (Saliva:0.834 %) | 0.286% (Saliva:0.468%) | 11.323% (Saliva: 0.856%) | 31.165% (Saliva: 1.186%) | 0.007% (Saliva: 0.015%) |
| Fusobacterium nucleatum | 0% | 1.57% (Saliva: 0.133%) | 0.487% (Saliva: 0.089%) | 0% | 0% | 0% | 0% | 0.183% (Saliva: 0.789%) | 0.942% (Saliva: 0.031%) | 1.151% (Saliva: 0.214%) | 0.005% (Saliva: 0.125%) | 9.509% (Saliva: 1.027%) | 0.219% (Saliva: 0.026%) | 7.014% (Saliva: 0.383%) | 0.001% (Saliva: 0.284%) | 11.012% (Saliva: 0.154%) | 20.261% (Saliva: 2.068%) | 0% |
| Prevotella oris | 0% | 27.092% (Saliva: 1.31%) | 28.478% (Saliva: 0.15%) | 0.014% (Saliva: 0.02%) | 0% | 0% | 0.001% (Saliva: 0.03%) | 0.986% (Saliva: 8.238%) | 0.004% (Saliva: 0.001%) | 11.349% (Saliva: 0.427%) | 0.003% (Saliva: 0.036%) | 6.93% (Saliva: 1.219%) | 0.004% (Saliva: 0.032%) | 0.003% (Saliva: 0.019%) | 0.256% (Saliva: 0.03%) | 0.001% (Saliva: 0.025%) | 0.001% (Saliva: 0.111%) | 0.002% (Saliva: 0.262%) |
| Prevotella intermedia | 0% | 0.159% (Saliva: 0.024%) | 0.076% (Saliva: 0.022%) | 0.014% (Saliva: 0.02%) | 0% | 0% | 0.001% (Saliva: 0.288%) | 0% | 0% | 0% | 0% | 0.001% (Saliva: 0.223%) | 0.584% (Saliva: 0.001%) | 0.061% (Saliva: 0.17%) | 0.001% (Saliva: 0.753%) | 0.002% (Saliva: 0.002%) | 0% | 0% |
| Treponema Denticola | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0.146% (Saliva: 0.469%) | 2.507% (Saliva: 0.012%) | 0.001% (Saliva: 0.07%) | 0% | 0% | 0% | 0.001% (Saliva: 0.073%) | 0% | 0.001% (Saliva: 0.002%) | 0.713% (Saliva: 0.42%) | 0% |
| Tannerella Forsythia | 0% | (Saliva: 0.066%) | 0.001% (Saliva: 0.092%) | 0.001% (Saliva: 0.003%) | 0% | 0% | 0.001% (Saliva: 0.017%) | 0.038% (Saliva: 0.17%) | 0.007% (Saliva: 0.011%) | 0.015% (Saliva: 0.046%) | 0% | 0.247% (Saliva: 0.056%) | 0% | 0.016% (Saliva: 0.022%) | 0% | 0.002% (Saliva: 0.002%) | 0.733% (Saliva: 0.264%) | 0% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuan, B.-C.; Yeh, Y.-T.; Lin, C.-C.; Huang, C.-H.; Liu, H.-C.; Chiang, C.-P. Clinical Detection of Chronic Rhinosinusitis through Next-Generation Sequencing of the Oral Microbiota. Microorganisms 2020, 8, 959. https://doi.org/10.3390/microorganisms8060959
Yuan B-C, Yeh Y-T, Lin C-C, Huang C-H, Liu H-C, Chiang C-P. Clinical Detection of Chronic Rhinosinusitis through Next-Generation Sequencing of the Oral Microbiota. Microorganisms. 2020; 8(6):959. https://doi.org/10.3390/microorganisms8060959
Chicago/Turabian StyleYuan, Ben-Chih, Yao-Tsung Yeh, Ching-Chiang Lin, Cheng-Hsieh Huang, Hsueh-Chiao Liu, and Chih-Po Chiang. 2020. "Clinical Detection of Chronic Rhinosinusitis through Next-Generation Sequencing of the Oral Microbiota" Microorganisms 8, no. 6: 959. https://doi.org/10.3390/microorganisms8060959
APA StyleYuan, B.-C., Yeh, Y.-T., Lin, C.-C., Huang, C.-H., Liu, H.-C., & Chiang, C.-P. (2020). Clinical Detection of Chronic Rhinosinusitis through Next-Generation Sequencing of the Oral Microbiota. Microorganisms, 8(6), 959. https://doi.org/10.3390/microorganisms8060959






