Targeted Combination Antibiotic Therapy Induces Remission in Treatment-Naïve Crohn’s Disease: A Case Series
Abstract
:1. Introduction
2. Materials and Methods
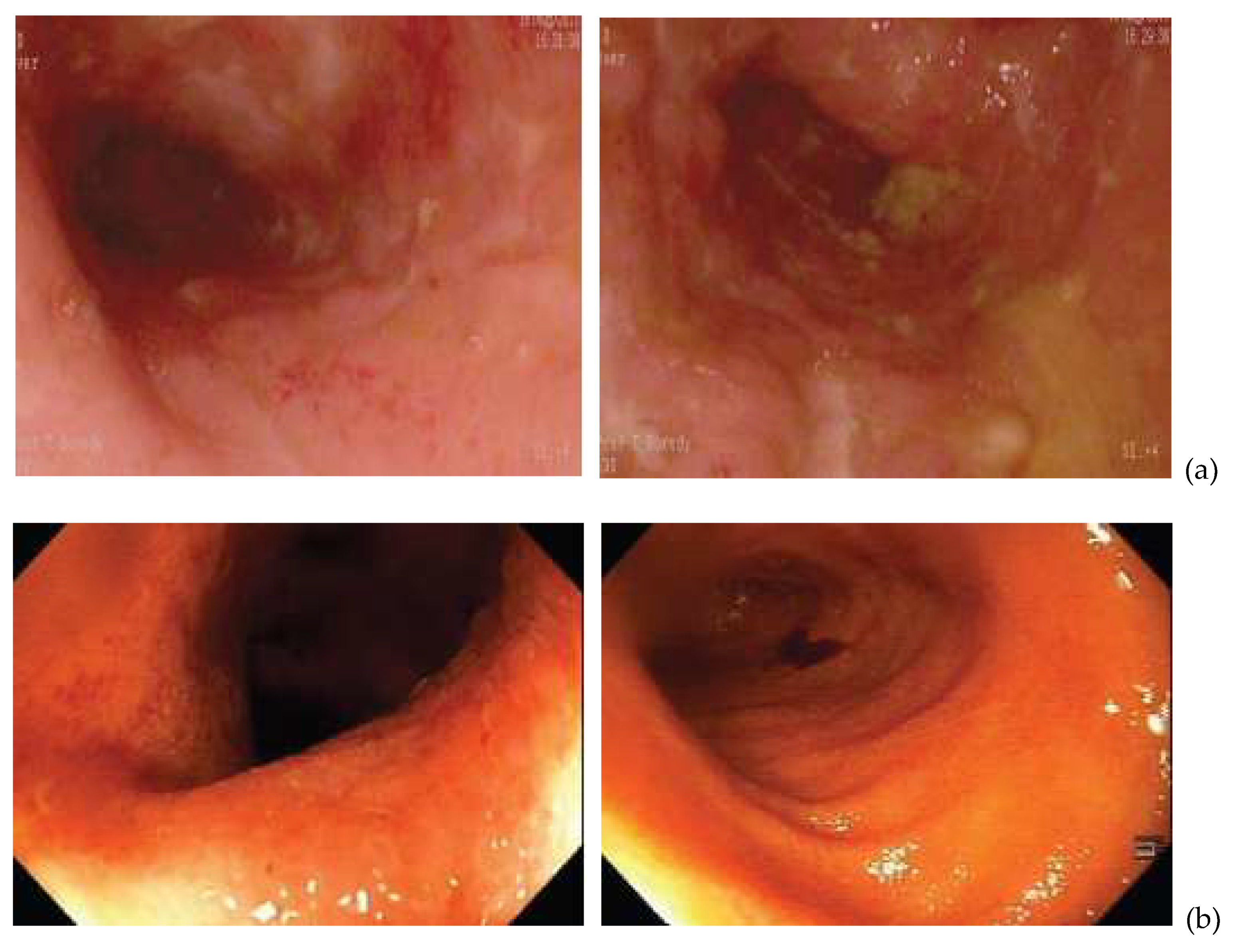
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lichtenstein, G.R.; Loftus, E.V.; Isaacs, K.L.; Regueiro, M.D.; Gerson, L.B.; Sands, B.E. ACG Clinical Guideline: Management of Crohn’s Disease in Adults. Am. J. Gastroenterol. 2018, 113, 481–517. [Google Scholar] [CrossRef]
- Feagan, B.G.; Sandborn, W.J.; Gasink, C.; Jacobstein, D.; Lang, Y.; Friedman, J.R.; Adedokun, O.J. Ustekinumab as Induction and Maintenance Therapy for Crohn’s Disease. N. Engl. J. Med. 2016, 375, 1946–1960. [Google Scholar] [CrossRef] [PubMed]
- Hanauer, S.B.; Sandborn, W.J.; Rutgeerts, P.; Fedorak, R.N.; Lukas, M.; MacIntosh, D.; Pollack, P. Human anti-tumor necrosis factor monoclonal antibody (adalimumab) in Crohn’s disease: The CLASSIC-I trial. Gastroenterology 2006, 130, 323–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roda, G.; Jharap, B.; Neeraj, N.; Colombel, J.F. Loss of Response to Anti-TNFs: Definition, Epidemiology, and Management. Clin. Transl. Gastroenterol. 2016, 7, e135-5. [Google Scholar] [CrossRef] [PubMed]
- Peyrin-Biroulet, L.; Lémann, M. Review article: Remission rates achievable by current therapies for inflammatory bowel disease. Aliment. Pharm. Ther. 2011, 33, 870–879. [Google Scholar] [CrossRef] [Green Version]
- Davis, W.C.; Kuenstner, J.T.; Singh, S.V. Resolution of Crohn’s (Johne’s) disease with antibiotics: What are the next steps? Expert Rev. Gastroenterol. Hepatol. 2017, 11, 393–396. [Google Scholar] [CrossRef] [Green Version]
- Joossens, M.; Huys, G.; Cnockaert, M.; De Preter, V.; Verbeke, K.; Rutgeerts, P.; Vermeire, S. Dysbiosis of the faecal microbiota in patients with Crohn’s disease and their unaffected relatives. Gut 2011, 60, 631–637. [Google Scholar] [CrossRef] [Green Version]
- Baldwin, S.L.; Larsenid, S.E.; Ordway, D.; Cassell, G.; Coler, R.N. The complexities and challenges of preventing and treating nontuberculous mycobacterial diseases. PLoS Negl. Trop. Dis. 2019, 13, 1–23. [Google Scholar] [CrossRef]
- Aitken, A.; Agrawal, G.; Markova, N.; Slavchev, G.; Chamberlin, W.; Borody, T.J. Demonstration of Intracellular Mycobacterium Species in Crohn’s Disease Using Novel Technologies. Am. J. Gastroenterol. 2015, 110, S843. [Google Scholar] [CrossRef]
- Naser, S.A.; Ghobrial, G.; Romero, C.; Valentine, J.F. Culture of Mycobacterium avium subspecies paratuberculosis from the blood of patients with Crohn’s disease. Lancet 2004, 364, 1039–1044. [Google Scholar] [CrossRef]
- Donohue, M.J. Increasing nontuberculous mycobacteria reporting rates and species diversity identified in clinical laboratory reports. BMC Infect. Dis. 2018, 18, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gui, G.P.H.; Thomas, P.R.S.; Tizard, M.L.V.; Lake, J.; Sanderson, J.D.; Hermon-Taylor, J. Two-year-outcomes analysis of Crohn’s disease treated with rifabutin and macrolide antibiotics. J. Antimicrob. Chemother. 1997, 39, 393–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shafran, I.; Kugler, L.; El-Zaatari, F.; NAser, S.; Sandoval, J. Open clinical trial of rifabutin in Crohn’s disease and clarithromycin therapy. Dig. Liver Dis. 2002, 34, 22–28. [Google Scholar] [CrossRef]
- Borody, T.J.; Leis, S.M.; Warren, E.F.; Surace, R. Treatment of severe Crohns disease using antimycobacterial triple therapy—Approaching a cure. Dig. Liver Dis. 2002, 34, 29–38. [Google Scholar] [CrossRef]
- Behr, M.A.; Hanley, J. Reflection and Reaction Antimycobacterial therapy for Crohn’s disease: A reanalysis. Lancet Infect. Dis. 2008, 8, 2008. [Google Scholar] [CrossRef]
- WHO. Global Tuberculosis Report; World Health Organisation: Geneva, Switzerland, 2019; 261p. [Google Scholar]
- Feagan, B.G.; Mohammed, N.; Kant, P.; Abid, F.; Rivero-Sanchez, L.; Lopez-Ceron, M.; Graham, D.Y. Phase III randomised, double blind, placebo-controlled, multicenter, parallel group study to assess the efficacy and safety of add-on fixed-dose anti-mycobacterial therapy (RHB-104) in moderately to severely active Crohn’s disease. United Eur. Gastroenterol. 2018, 6, 1586–1597. [Google Scholar]
- Novosad, S.; Henkle, E.; Winthrop, K. The Challenge of Pulmonary Nontuberculous Mycobacterial Infection. Curr. Pulmonol. Rep. 2015, 176, 139–148. [Google Scholar] [CrossRef]
- Shulha, J.A.; Escalante, P.; Wilson, J.W. Pharmacotherapy Approaches in Nontuberculous Mycobacteria Infections. Mayo Clin. Proc. 2019, 94, 1567–1581. [Google Scholar] [CrossRef] [Green Version]
- Lacucci, M.; Ghosh, S. Looking beyond symptom relief: Evolution of mucosal healing in inflammatory bowel disease. Ther. Adv. Gastroenterol. 2011, 4, 129–143. [Google Scholar]
- Fernandes, S.; Rodrigues, R.; Bernardo, S. Transmural Healing Is Associated with Improved Long-term Outcomes of Patients with Crohn’s Disease. Inflamm. Bowel Dis. 2017, 23, 1403–1409. [Google Scholar] [CrossRef]
- Borody, T.J.; Leis, S.; Surace, R.G.J. Treatment of severe Crohn’s disease using rifabutin-macrolide-clofazimine combination: Results at 30–37 months. Gastroenterology 2000, 118, A1334. [Google Scholar] [CrossRef]
- Green, C.; Elliott, L.; Beaudoin, C.; Bernstein, C.N. A population-based ecologic study of inflammatory bowel disease: Searching for etiologic clues. Am. J. Epidemiol. 2006, 164, 615–623, discussion 624-8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pickup, R.W.; Rhodes, G.; Arnott, S.; Sidi-Boumedine, K.; Bull, T.J.; Weightman, A.; Hermon-Taylor, J. Mycobacterium avium subsp. paratuberculosis in the catchment area and water of the river Taff in South Wales, United Kingdom, and its potential relationship to clustering of Crohn’s Disease Cases in the City of Cradiff. Appl. Environ. Microbiol. 2005, 71, 2130–2139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gearry, R.B.; Richardson, A.; Frampton, C.M.; Collett, J.A.; Burt, M.J.; Chapman, B.A.; Barclay, M.L. High incidence of Crohn’s disease in Canterbury, New Zealand: Results of an epidemiologic study. Inflamm. Bowel Dis. 2006, 12, 936–943. [Google Scholar] [CrossRef] [Green Version]
- Jostins, L.; Ripke, S.; Weersma, R.K.; Duerr, R.H.; Dermot, P. Host-mictobe interactions have shaped the genetic architecture of Inflammatory Bowel Disease. Nature 2012, 491, 119–124. [Google Scholar] [CrossRef] [Green Version]
- Franke, A.; McGovern, D.P.; Barrett, J.C.; Wang, K.; Radford-Smith, G.L.; Ahmad, T.; Anderson, C.A. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn’s disease susceptibility loci. Nat. Genet. 2010, 42, 1118–1125. [Google Scholar] [CrossRef] [Green Version]
- Strober, W.; Asano, N.; Fuss, I.; Kitani, A.; Watanabe, T. Cellular and molecular mechanisms underlying NOD2 risk-associated polymorphisms in Crohn’s disease. Immunol. Rev. 2014, 260, 249–260. [Google Scholar] [CrossRef]
- Van Kruiningen, H.; Chiodini, R.; Thayer, W.; Coutu, J.; Merkal, R.; Runnels, P. Experimental disease in infant goats induced by a Mycobacterium isolated from a patient with Crohn’s disease. Dig. Dis. Sci. 1986, 31, 1351–1360. [Google Scholar] [CrossRef]
- Selby, W.; Pavli, P.; Crotty, B.; Florin, T.; Radford-Smith, G.; Gibson, P.; Ee, H. Two-Year Combination Antibiotic Therapy with Clarithromycin, Rifabutin, and Clofazimine for Crohn’s Disease. Gastroenterology 2007, 132, 2313–2319. [Google Scholar] [CrossRef]
- Abubakar, I.; Myhill, D.; Aliyu, S.; Hunter, P. Detection of MAP from patients with CD using nuclei acid-based techniques: A systematic review and meta-analysis. Inflamm. Bowel Dis. 2008, 14, 401–410. [Google Scholar] [CrossRef]
- Feller, M.; Huwiler, K.; Stephan, R.; Altpeter, E.; Shang, A.; Furrer, H.; Egger, M. Mycobacterium avium subspecies paratuberculosis and Crohn’s disease: A systematic review and meta-analysis. Lancet Infect. Dis. 2007, 7, 607–613. [Google Scholar] [CrossRef]
- Donaghy, J.A.; Totton, N.L.; Rowe, M.T. Persistence of Mycobacterium paratuberculosis during manufacture and ripening of cheddar cheese. Appl. Environ. Microbiol. 2004, 70, 4899–4905. [Google Scholar] [CrossRef] [Green Version]
- Bach, H.; Rosenfeld, H.; Bressler, B. Treatment of Crohn’s disease patients with infliximab is detrimental for the survival of Mycobacterium avium ssp. paratuberculosis within macrophages and shows remarkable decreas in the immunogenicity of mycobacterial proteins. J. Crohn’s Colitis 2012, 6, 628–629. [Google Scholar] [CrossRef] [Green Version]
- Greenstein, R.J.; Su, L.; Shahidi, A.; Brown, S.T. On the Action of 5-Amino-Salicylic Acid and Sulfapyridine on M. avium including Subspecies paratuberculosis. PLoS ONE 2007, 2, e516. [Google Scholar] [CrossRef] [Green Version]
- Greenstein, R.J.; Su, L.; Haroutunian, V.; Shahidi, A.; Brown, S.T. On the action of methotrexate and 6-mercaptopurine on M. avium subspecies paratuberculosis. PLoS ONE 2007, 2, e161. [Google Scholar]
- Greenstein, R.J.; Su, L.; Juste, R.A.; Brown, S.T. On the action of cyclosporine A, rapamycin and tacrolimus on M. avium including subspecies paratuberculosis. PLoS ONE 2008, 3, e2496. [Google Scholar] [CrossRef] [Green Version]
- Greenstein, R.J.; Su, L.; Brown, S.T. The thioamides methimazole and thiourea inhibit growth of M. avium subspecies paratuberculosis in culture. PLoS ONE 2010, 5, e11099. [Google Scholar] [CrossRef]
- Arrazuria, R.; Elguezabal, N.; Juste, R.A.; Derakhshani, H.; Khafipour, E. Mycobacterium avium subspecies paratuberculosis infection modifies gut microbiota under different dietary conditions in a rabbit model. Front. Microbiol. 2016, 7, 1–14. [Google Scholar] [CrossRef]
- Hermon-Taylor, J. Mycobacterium avium subspecies paratuberculosis is a cause of Crohn’s disease. Gut 2001, 49, 755–756. [Google Scholar] [CrossRef] [Green Version]
- Walters, T.D.; Griffiths, A.M. Mechanisms of growth impairment in pediatric Crohn’s disease. Nat. Rev. Gastroenterol. Hepatol. 2009, 6, 513–523. [Google Scholar] [CrossRef]
- Gupta, N.; Cohen, S.A.; Bostrom, A.G.; Kirschner, B.S.; Baldassano, R.N.; Winter, H.S.; Heyman, M.B. Risk Factors for Initial Surgery in Pediatric Patients with Crohn’s Disease. Gastroenterology 2006, 130, 1069–1077. [Google Scholar] [CrossRef]
- De Ridder, L.; Rings, E.H.; Damen, G.M.; Kneepkens, F.C.; Schweizer, J.J.; Kokke, F.T.; Escher, J.C. Infliximab dependency in pediatric Crohn’s disease: Long-term follow-up of an unselected cohort. Inflamm. Bowel Dis. 2008, 14, 353–358. [Google Scholar] [CrossRef]
- Dupont-Lucas, C.; Sternszus, R.; Ezri, J.; Leibovitch, S.; Gervais, F.; Amre, D.; Deslandres, C. Identifying patients at high risk of loss of response to infliximab maintenance therapy in paediatric crohn’s disease. J. Crohn’s Colitis 2016, 10, 795–804. [Google Scholar] [CrossRef] [Green Version]
- Khan, S.S.; Patil, S.S. Bone density in pediatric Crohn’s disease: A cross-sectional observation from South India. Indian J. Gastroenterol. 2017, 36, 184–188. [Google Scholar] [CrossRef]
- Riello, L.; Talbotec, C.; Garnier-Lengline, H.; Pigneur, B.; Svahn, J.; Canioni, D.; Ruemmele, F.M. Tolerance and efficacy of azathioprine in pediatric Crohn’s disease. Inflamm. Bowel Dis. 2011, 17, 2138–2143. [Google Scholar] [CrossRef]
| Pt. | Demographics (Gender, Age) | Baseline | Treatment | 6 Weeks | 12 Months | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | CDAI | CRP | Symptoms | CRP (mg/L) | Symptoms | CDAI | CRP (mg/L) | |||
| 1 | F, 30 | BM 10/day, abdominal pain | 367 | 11.3 | Rifabutin, clarithromycin, clofazimine, ciprofloxacin | BM 2–3/day | 10.5 | BM 2–3/day, no abdominal pain | 85 | 5.9 |
| 2 | M, 29 | Abdominal pain, weight loss | 230 | 142.9 | Rifabutin, clarithromycin, clofazimine, metronidazole | BM 2–3/day | 8.1 | BM 2–3/day | 31 | 2.1 |
| 3 | F, 35 | BM 5–6/day, abdominal pain, weight loss | 346 | 32 | Rifabutin, clarithromycin, clofazimine, metronidazole | BM 1–2/day | 3.8 | BM 1/day | 16 | 1.0 |
| 4 | M, 27 | Abdominal pain, weight loss | 298 | 68 | Rifabutin, clarithromycin, clofazimine, ciprofloxacin | BM 1–3/day, no abdominal pain | 2.8 | BM 2/day | 78 | 0.5 |
| 5 | M, 46 | BM 2–6/day, weight loss | 269 | 5.7 | Rifabutin, clarithromycin, clofazimine, metronidazole | BM 2–3/day | 9.6 | BM 2–3/day | 87 | 1.7 |
| 6 | M, 13 | BM 5/day, abdominal pain, weight loss | 468 | 42.6 | Rifabutin, clarithromycin, clofazimine | BM 1–2/day, reduced abdominal pain, weight gain 2 kg | 12.1 | BM 2–4/day | 88 | 3.5 |
| 7 | F, 14 | BM 3–4/day | 273 | 5.7 | Rifabutin, clarithromycin, clofazimine, ciprofloxacin | BM 2–3/day | 1.7 | BM 3/day | 45 | 0.4 |
| 8 | F, 19 | BM 20/day, abdominal pain | 280 | 10 | Rifabutin, clarithromycin, clofazimine, metronidazole | BM 2/day, no pain | 3.9 | BM 2/day | 46 | 4.0 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agrawal, G.; Clancy, A.; Sharma, R.; Huynh, R.; Ramrakha, S.; Borody, T. Targeted Combination Antibiotic Therapy Induces Remission in Treatment-Naïve Crohn’s Disease: A Case Series. Microorganisms 2020, 8, 371. https://doi.org/10.3390/microorganisms8030371
Agrawal G, Clancy A, Sharma R, Huynh R, Ramrakha S, Borody T. Targeted Combination Antibiotic Therapy Induces Remission in Treatment-Naïve Crohn’s Disease: A Case Series. Microorganisms. 2020; 8(3):371. https://doi.org/10.3390/microorganisms8030371
Chicago/Turabian StyleAgrawal, Gaurav, Annabel Clancy, Rijata Sharma, Roy Huynh, Sanjay Ramrakha, and Thomas Borody. 2020. "Targeted Combination Antibiotic Therapy Induces Remission in Treatment-Naïve Crohn’s Disease: A Case Series" Microorganisms 8, no. 3: 371. https://doi.org/10.3390/microorganisms8030371
APA StyleAgrawal, G., Clancy, A., Sharma, R., Huynh, R., Ramrakha, S., & Borody, T. (2020). Targeted Combination Antibiotic Therapy Induces Remission in Treatment-Naïve Crohn’s Disease: A Case Series. Microorganisms, 8(3), 371. https://doi.org/10.3390/microorganisms8030371






