Detection of Pathogens by a Novel User-Developed Broad-Range BR 16S PCR rRNA Polymerase Chain Reaction/Gene Sequencing Assay: Multiyear Experience in a Large Canadian Healthcare Zone
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patient Population
2.3. Laboratory Setting and Clinical Specimens
2.4. Microbiology Methods
2.4.1. Culture
2.4.2. Molecular Methods
2.5. Data Analysis
3. Results
3.1. Patient Characteristics
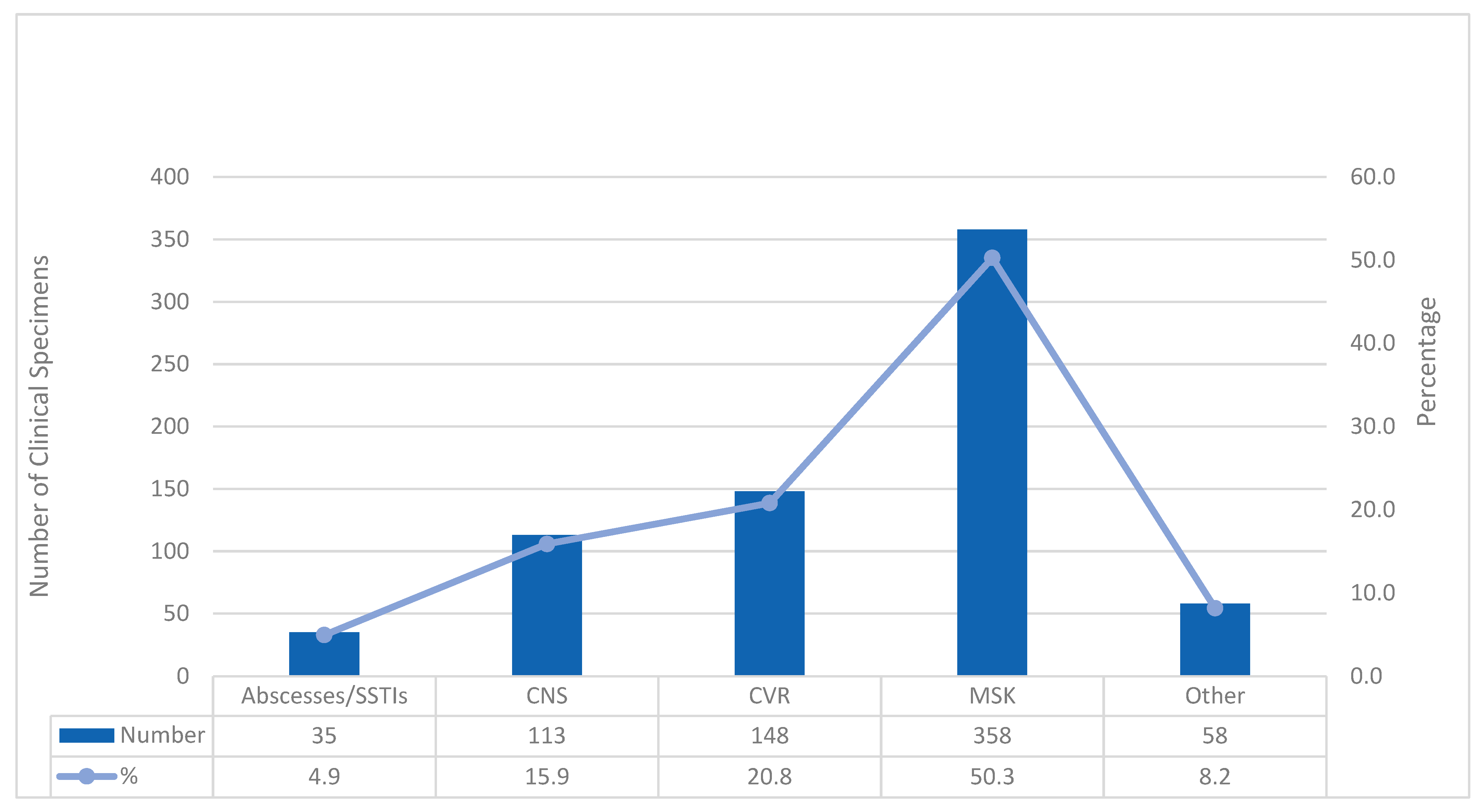
3.2. Distribution of the Clinical Specimens
3.3. Bacteria Detected by BR 16S PCR
3.4. The Performance of BR 16S PCR Compared to Culture
3.5. Prediction of Molecular Assay Results According to Clinical Specimen Microscopic Examination and Patient Biomarkers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BR 16S PCR | Broad range BR 16S PCR rDNA polymerase chain reaction and Sanger sequencing |
| BR 16S PCR rDNA gene | BR 16S PCR ribosomal ribonucleic acid gene |
| DNA | deoxyribonucleic acid |
| APL | Alberta precision laboratories |
| DSC | Diagnostic and Scientific Centre |
| BA | blood agar |
| BBA | Brucella blood agar |
| CHOC | chocolate agar |
| MAC | MacConkey agar |
| MALDI-TOF MS | matrix assisted laser desorption-time of flight mass spectrometry |
| MSK | musculoskeletal |
| PJI | prosthetic joint infection |
| CVR | cardiovascular |
| CNS | central nervous system |
| CSF | cerebrospinal fluid |
| SSTI | skin and soft tissue infection |
| CRP | C-reactive protein |
| WBC | white blood cell count |
| PMN | polymorphonuclear |
| PPV | positive predictive value |
| NPV | negative prediction value |
| OR | odds ratio |
| RR | relative risk |
| tMGS | targeted metagenomics |
| Ct | cycle threshold |
| Sterile fluids | pericardial, peritoneal, synovial, cerebrospinal fluid |
References
- Branda, J.A.; Rychert, J.; Burnham, C.A.; Bythrow, M.; Garner, O.B.; Ginocchio, C.C.; Jennemann, R.; Lewinski, M.A.; Manji, R.; Mochon, A.B.; et al. Multicenter validation of the VITEK MS v2.0 MALDI-TOF mass spectrometry system for the identification of fastidious gram-negative bacteria. Diagn. Microbiol. Infect. Dis. 2014, 78, 129–131. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Chung, H.S.; Moon, H.W.; Lee, S.H.; Lee, K. Comparative evaluation of two matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) systems, Vitek MS, and Microflex LT, for the identification of Gram-positive cocci routinely isolated in clinical microbiology laboratories. J. Microbiol. Methods 2015, 113, 13–15. [Google Scholar] [PubMed]
- Church, D.L.; Griener, T.; Gregson, D. Multi-year comparison of VITEK(R) MS and 16S rRNA gene sequencing performance for the identification of rarely encountered anaerobes causing invasive human infections in a large Canadian region: Can our laboratory abandon 16S rRNA gene sequencing? Anaerobe 2022, 78, 102640. [Google Scholar] [CrossRef] [PubMed]
- Church, D.L.; Griener, T.; Gregson, D. Multi-year comparison of VITEK MS performance for identification of rarely encountered pathogenic Gram-negative organisms (GNOs) in a large integrated Canadian healthcare region. Microbiol. Spectr. 2024, 12, e0227624. [Google Scholar] [CrossRef]
- Sharma, K.; Angrup, A.; Ghosh, A.; Singh, S.; Sood, A.; Arora, A.; Sharma, M.; Sethi, S.; Rudramurthy, S.M.; Kaur, H.; et al. Evaluation of VITEK MS Version 3.0 MALDI-TOF for the identification of anaerobes, mycobacteria, Nocardia, and moulds. Diagn. Microbiol. Infect. Dis. 2024, 110, 116477. [Google Scholar] [CrossRef]
- Church, D.; Griener, T.; Gregson, D. Multi-year comparison of VITEK MS performance for identification of rarely encountered pathogenic gram-positive organisms (GPOs) in a large integrated Canadian healthcare region. Microbiol. Spectr. 2025, 13, e0254524. [Google Scholar] [CrossRef]
- Stokes, W.; Campbell, L.; Pitout, J.; Conly, J.; Church, D.; Gregson, D. Comparison of Accelerate PhenoTest BC Kit and MALDI-TOF MS/VITEK 2 System for the rapid identification and antimicrobial susceptibility testing of gram-negative bacilli causing bloodstream infections. J. Assoc. Med. Microbiol. Infect. Dis. Can. 2020, 5, 145–157. [Google Scholar] [CrossRef]
- Perez, K.K.; Olsen, R.J.; Musick, W.L.; Cernoch, P.L.; Davis, J.R.; Peterson, L.E.; Musser, J.M. Integrating rapid diagnostics and antimicrobial stewardship improves outcomes in patients with antibiotic-resistant Gram-negative bacteremia. J. Infect. 2014, 69, 216–225. [Google Scholar] [CrossRef]
- Dalai, A.S.; Monti, E.B.; Mallesho, R.; Obeda, M.; Evans, G.A.; Perez-Patrigeon, S.; Wilson, E.; Martinez-Cajas, J.L.; Sheth, P.M.; Tomalty, L.; et al. Increasing evidence-based care practices for patients with Staphylococcus aureus bacteraemia through required infectious diseases consultation in a tertiary care hospital: A quality improvement initiative. BMJ Open Qual. 2025, 14, e003243. [Google Scholar] [CrossRef]
- Fournier, P.E.; Thuny, F.; Richet, H.; Lepidi, H.; Casalta, J.P.; Arzouni, J.P.; Maurin, M.; Celard, M.; Mainardi, J.L.; Caus, T.; et al. Comprehensive diagnostic strategy for blood culture-negative endocarditis: A prospective study of 819 new cases. Clin. Infect. Dis. 2010, 51, 131–140. [Google Scholar] [CrossRef]
- Miller, R.J.; Chow, B.; Pillai, D.; Church, D. Development and evaluation of a novel fast broad-range 16S ribosomal DNA PCR and sequencing assay for diagnosis of bacterial infective endocarditis: Multi-year experience in a large Canadian healthcare zone and a literature review. BMC Infect. Dis. 2016, 16, 146. [Google Scholar] [CrossRef] [PubMed]
- Muller Premru, M.; Lejko Zupanc, T.; Klokocovnik, T.; Ruzic Sabljic, E.; Cerar, T. Broad-Range 16S rDNA PCR on Heart Valves in Infective Endocarditis. J. Heart Valve Dis. 2016, 25, 221–226. [Google Scholar] [PubMed]
- Marin, M.; Garcia-Lechuz, J.M.; Alonso, P.; Villanueva, M.; Alcala, L.; Gimeno, M.; Cercenado, E.; Sanchez-Somolinos, M.; Radice, C.; Bouza, E. Role of universal 16S rRNA gene PCR and sequencing in diagnosis of prosthetic joint infection. J. Clin. Microbiol. 2012, 50, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Qu, X.; Zhai, Z.; Wu, C.; Jin, F.; Li, H.; Wang, L.; Liu, G.; Liu, X.; Wang, W.; Li, H.; et al. Preoperative aspiration culture for preoperative diagnosis of infection in total hip or knee arthroplasty. J. Clin. Microbiol. 2013, 51, 3830–3834. [Google Scholar] [CrossRef]
- Godfrey, R.; Curtis, S.; Schilling, W.H.; James, P.R. Blood culture negative endocarditis in the modern era of 16S rRNA sequencing. Clin. Med. 2020, 20, 412–416. [Google Scholar] [CrossRef]
- Tan, J.; Liu, Y.; Ehnert, S.; Nussler, A.K.; Yu, Y.; Xu, J.; Chen, T. The Effectiveness of Metagenomic Next-Generation Sequencing in the Diagnosis of Prosthetic Joint Infection: A Systematic Review and Meta-Analysis. Front. Cell. Infect. Microbiol. 2022, 12, 875822. [Google Scholar] [CrossRef]
- Peeters, B.; Herijgers, P.; Beuselinck, K.; Verhaegen, J.; Peetermans, W.E.; Herregods, M.C.; Desmet, S.; Lagrou, K. Added diagnostic value and impact on antimicrobial therapy of 16S rRNA PCR and amplicon sequencing on resected heart valves in infective endocarditis: A prospective cohort study. Clin. Microbiol. Infect. 2017, 23, 888 e1–888 e5. [Google Scholar] [CrossRef]
- Borde, J.P.; Hacker, G.A.; Guschl, S.; Serr, A.; Danner, T.; Hubner, J.; Burrack-Lange, S.; Ludke, G.; Helwig, P.; Hauschild, O.; et al. Diagnosis of prosthetic joint infections using UMD-Universal Kit and the automated multiplex-PCR Unyvero i60 ITI((R)) cartridge system: A pilot study. Infection 2015, 43, 551–560. [Google Scholar] [CrossRef]
- Carter, K.; Doern, C.; Jo, C.H.; Copley, L.A. The Clinical Usefulness of Polymerase Chain Reaction as a Supplemental Diagnostic Tool in the Evaluation and the Treatment of Children with Septic Arthritis. J. Pediatr. Orthop. 2016, 36, 167–172. [Google Scholar] [CrossRef]
- Akram, A.; Maley, M.; Gosbell, I.; Nguyen, T.; Chavada, R. Utility of 16S rRNA PCR performed on clinical specimens in patient management. Int. J. Infect. Dis. 2017, 57, 144–149. [Google Scholar] [CrossRef]
- Kommedal, O.; Simmon, K.; Karaca, D.; Langeland, N.; Wiker, H.G. Dual priming oligonucleotides for broad-range amplification of the bacterial 16S rRNA gene directly from human clinical specimens. J. Clin. Microbiol. 2012, 50, 1289–1294. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Interpretive Criteria for Identification of Bacteria and Fungi by DNA Target Seqeuncing: Approved Guideline MM-18; CLSI: Wayne, PA, USA, 2018. [Google Scholar]
- Velasquez-Mejia, E.P.; de la Cuesta-Zuluaga, J.; Escobar, J.S. Impact of DNA extraction, sample dilution, and reagent contamination on 16S rRNA gene sequencing of human feces. Appl. Microbiol. Biotechnol. 2018, 102, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, D.; Rajan, D.; Bellis, K.L.; Betteridge, E.; Brennan, J.; de Sousa, C.; Carriage Study, T.; Parkhill, J.; Peacock, S.J.; de Goffau, M.C.; et al. Optimization of high throughput 16S rRNA gene amplicon sequencing: An assessment of PCR pooling, mastermix use and contamination. Microb. Genom. 2023, 9, 001115. [Google Scholar] [CrossRef] [PubMed]
- Dyrhovden, R.; Rippin, M.; Ovrebo, K.K.; Nygaard, R.M.; Ulvestad, E.; Kommedal, O. Managing Contamination and Diverse Bacterial Loads in 16S rRNA Deep Sequencing of Clinical Samples: Implications of the Law of Small Numbers. mBio 2021, 12, e0059821. [Google Scholar] [CrossRef] [PubMed]
- Fida, M.; Wolf, M.J.; Hamdi, A.; Vijayvargiya, P.; Esquer Garrigos, Z.; Khalil, S.; Greenwood-Quaintance, K.E.; Thoendel, M.J.; Patel, R. Detection of Pathogenic Bacteria from Septic Patients Using 16S Ribosomal RNA Gene-Targeted Metagenomic Sequencing. Clin. Infect. Dis. 2021, 73, 1165–1172. [Google Scholar] [CrossRef]
- Kim, M.S.; Chang, J.; Kim, M.N.; Choi, S.H.; Jung, S.H.; Lee, J.W.; Sung, H. Utility of a Direct 16S rDNA PCR and Sequencing for Etiological Diagnosis of Infective Endocarditis. Ann. Lab. Med. 2017, 37, 505–510. [Google Scholar] [CrossRef][Green Version]
- Marin, M.; Munoz, P.; Sanchez, M.; del Rosal, M.; Alcala, L.; Rodriguez-Creixems, M.; Bouza, E. Molecular diagnosis of infective endocarditis by real-time broad-range polymerase chain reaction (PCR) and sequencing directly from heart valve tissue. Medicine 2007, 86, 195–202. [Google Scholar] [CrossRef]
- Sebastian, S.; Malhotra, R.; Sreenivas, V.; Kapil, A.; Chaudhry, R.; Dhawan, B. Utility of 16S rRNA PCR in the Synovial Fluid for the Diagnosis of Prosthetic Joint Infection. Ann. Lab. Med. 2018, 38, 610–612. [Google Scholar] [CrossRef]
- Reuwer, A.Q.; van den Bijllaardt, W.; Murk, J.L.; Buiting, A.G.M.; Verweij, J.J. Added diagnostic value of broad range 16S PCR on periprosthetic tissue and clinical specimens from other normally sterile body sites. J. Appl. Microbiol. 2019, 126, 661–666. [Google Scholar]
- Rodriguez-Garcia, R.; Rodriguez-Esteban, M.A.; Fernandez-Suarez, J.; Morilla, A.; Garcia-Carus, E.; Telenti, M.; Morales, C.; Albaiceta, G.M.; Fernandez, J. Evaluation of 16S rDNA Heart Tissue PCR as a Complement to Blood Cultures for the Routine Etiological Diagnosis of Infective Endocarditis. Diagnostics 2021, 11, 1372. [Google Scholar] [CrossRef]
- Anton-Vazquez, V.; Dworakowski, R.; Cannata, A.; Amin-Youssef, G.; Gunning, M.; Papachristidis, A.; MacCarthy, P.; Baghai, M.; Deshpande, R.; Khan, H.; et al. 16S rDNA PCR for the aetiological diagnosis of culture-negative infective endocarditis. Infection 2022, 50, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Lane, M.A.; Ganeshraj, N.; Gu, A.; Warren, D.K.; Burnham, C.D. Lack of Additional Diagnostic Yield of 16s rRNA Gene PCR for Prosthetic Joint Infections. J. Appl. Lab. Med. 2019, 4, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Tkadlec, J.; Peckova, M.; Sramkova, L.; Rohn, V.; Jahoda, D.; Raszka, D.; Berousek, J.; Mosna, F.; Vymazal, T.; Kvapil, M.; et al. The use of broad-range bacterial PCR in the diagnosis of infectious diseases: A prospective cohort study. Clin. Microbiol. Infect. 2019, 25, 747–752. [Google Scholar] [CrossRef] [PubMed]
- Stavnsbjerg, C.; Frimodt-Moller, N.; Moser, C.; Bjarnsholt, T. Comparison of two commercial broad-range PCR and sequencing assays for identification of bacteria in culture-negative clinical samples. BMC Infect. Dis. 2017, 17, 233. [Google Scholar] [CrossRef]
- Parvizi, J.; Tan, T.L.; Goswami, K.; Higuera, C.; Della Valle, C.; Chen, A.F.; Shohat, N. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J. Arthroplast. 2018, 33, 1309–1314.e2. [Google Scholar] [CrossRef]
- Boers, S.A.; Jansen, R.; Hays, J.P. Understanding and overcoming the pitfalls and biases of next-generation sequencing (NGS) methods for use in the routine clinical microbiological diagnostic laboratory. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 1059–1070. [Google Scholar] [CrossRef]
- Wang, C.X.; Huang, Z.; Fang, X.; Li, W.; Yang, B.; Zhang, W. Comparison of broad-range polymerase chain reaction and metagenomic next-generation sequencing for the diagnosis of prosthetic joint infection. Int. J. Infect. Dis. 2020, 95, 8–12. [Google Scholar] [CrossRef]
- Mishra, D.; Satpathy, G.; Chawla, R.; Paliwal, D.; Panda, S.K. Targeted metagenomics using next generation sequencing in laboratory diagnosis of culture negative endophthalmitis. Heliyon 2021, 7, e06780. [Google Scholar] [CrossRef]
- Flurin, L.; Wolf, M.J.; Mutchler, M.M.; Daniels, M.L.; Wengenack, N.L.; Patel, R. Targeted Metagenomic Sequencing-based Approach Applied to 2146 Tissue and Body Fluid Samples in Routine Clinical Practice. Clin. Infect. Dis. 2022, 75, 1800–1808. [Google Scholar] [CrossRef]
- Flurin, L.; Fisher, C.R.; Wolf, M.J.; Pritt, B.S.; DeSimone, D.C.; Patel, R. Comparison of Blood-Based Shotgun and Targeted Metagenomic Sequencing for Microbiological Diagnosis of Infective Endocarditis. Open Forum Infect. Dis. 2023, 10, ofad546. [Google Scholar] [CrossRef]
- Olearo, F.; Zein, S.E.; Portillo, M.E.; Zapf, A.; Rohde, H.; Berbari, E.F.; Wouthuyzen-Bakker, M. ESCMID Study Group on Implant-Associated Infections (ESGIAI); The Molecular Working Group for the Unified PJI Definition Task Force. Diagnostic accuracy of 16S rDNA PCR, multiplex PCR and metagenomic next-generation sequencing in periprosthetic joint infections: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2025, 31, 1115–1125. [Google Scholar]
| Parameter | Characteristic | N (%) ± SD |
|---|---|---|
| Number of subjects | 662 | |
| Age, years (mean ± SD) | 41.8 ± 7.7 | |
| Adults (≥14 yrs) | 532 (80.4); 56.95 ± 10.8 | |
| Male; Age, years (mean ± 2 SD) | 300 (56.4); 56.5 ± 6.6 | |
| Female; Age, years (mean ± 2 SD) | 232 (43.6); 57.6 ± 4.5 | |
| Pediatrics (≤14 yrs) | 130 (19.6); 6.3 ± 9.6 | |
| Male; Age, years (mean ± 2 SD) | 78 (60.0); 6.7 ± 7.4 | |
| Female; Age, years (mean ± 2 SD) | 52 (40.0); 6.6 ± 9.9 | |
| Location | Hospitalized or ED | 589 (89) |
| Ambulatory | 33 (11) | |
| Prior antibiotic therapy | 652 (98.6) | |
| Therapy prior to specimen collection | 9 d ± 6.4 d |
| (A) | |||
| Culture Compared to BR 16S PCR a | |||
| BR 16S PCR Result | |||
| Culture Results | Positive | Negative | Total |
| Positive | 35 | 10 | 45 |
| Negative | 251 | 448 | 709 |
| Total | 286 | 468 | |
| BR 16S PCR Compared to Culture b | |||
| Culture Result | |||
| BR 16S Results | Positive | Negative | Total |
| Positive | 283 | 1 | 284 |
| Negative | 5 | 467 | 472 |
| Total | 288 | 468 | |
| (B) | |||
| Culture Compared to BR 16S PCR a | |||
| BR 16S PCR Result | |||
| Culture Results | Positive | Negative | Total |
| Positive | 45 | 15 | 60 |
| Negative | 240 | 404 | 664 |
| Total | 265 | 419 | |
| BR 16S PCR Compared to Culture b | |||
| Culture Result | |||
| BR 16S Results | Positive | Negative | Total |
| Positive | 283 | 1 | 284 |
| Negative | 5 | 467 | 472 |
| Total | 288 | 468 | |
| All Specimens (N = 685) | Gram PMN (N = 685, 37.5%) | Gram Organism (N = 684, 37.6%) | WBC > 9.0 × 109/L (N = 611, 37.8%) | Neutrophils HIGH (N = 351, 37.0%) | CRP > 50 mg/L (N = 420, 35.5%) |
|---|---|---|---|---|---|
| TRUE POSITIVE (Parameter predicts positive/16S positive) | 175 | 62 | 198 | 73 | 107 |
| FALSE POSITIVE (Parameter predicts positive/16S negative) | 200 | 17 | 264 | 87 | 133 |
| FALSE NEGATIVE (Parameter predicts negative/16S positive) | 77 | 190 | 32 | 57 | 42 |
| TRUE NEGATIVE (Parameter predicts negative/16S negative) | 233 | 415 | 117 | 134 | 138 |
| BR 16S PCR Assay Performance | |||||
| Sensitivity (correct prediction of positive) | 69.4% (95% CI: 63.5–75.1%) | 24.6% (95% CI: 19.4–30.4%) | 86.1% (95% CI: 80.9–90.3%) | 56.15% (95% CI: 47.18–64.84%) | 71.8% (956% CI: 63.9–78.9%) |
| Specificity (correct prediction of negative) | 53.8% (95% CI: 49.0–58.6%) | 96.1% (95% CI: 93.8–97.7%) | 30.7% (95% CI: 26.1–35.6%) | 6.63% (95% CI: 53.86–67.12%) | 50.9% (95% CI: 44.8–57.0%) |
| Positive Predictive Value | 46.7% (95% CI: 43.4–49.9%) | 78.5% (95% CI: 68.6–85.9%) | 42.9%% (95% CI: 40.8–44.9%) | 45.62% (95% CI: 40.16–51.20%) | 44.6% (95% CI: 40.7–48.5%) |
| Negative Predictive Value | 75.2% (95% CI: 71.1–78.8%) | 68.6% (95% CI: 67.0–70.2%) | 78.5% (95% CI: 71.9–83.9%) | 70.16% (95% CI: 65.32–74.58%) | 76.7% (95% CI: 71.3–81.3%) |
| Accuracy | 59.6% (95% CI: 77.8–63.3%) | 69.7% (95% CI: 66.1–73.2% | 51.6% (95% CI: 47.5–55.6%) | 59.0% (95% CI: 53.6–64.2%) | 58.3% (95% CI: 53.5–63.1%) |
| Odds Ratio | 2.65 | 7.97 | 2.74 | 1.97 | 2.64 |
| Relative Risk | 1.88 | 2.50 | 2.00 | 1.53 | 1.91 |
| Bone and Joint Specimens (N = 309) | Gram PMN (N = 309, 23.0%) | Gram Organism (N = 309, 23.0%) | WBC > 9.0 × 109/L (N = 274, 23.7%) | Neutrophils HIGH (N = 166, 28.9%) | CRP > 50 mg/L (N = 249, 25.3%) |
|---|---|---|---|---|---|
| TRUE POSITIVE (Parameter predicts positive/16S positive) | 55 | 5 | 42 | 12 | 38 |
| FALSE POSITIVE (Parameter predicts positive/16S negative) | 128 | 13 | 131 | 45 | 103 |
| FALSE NEGATIVE (Parameter predicts negative/16S positive) | 16 | 66 | 23 | 36 | 25 |
| TRUE NEGATIVE (Parameter predicts negative/16S negative) | 110 | 225 | 78 | 73 | 83 |
| BR 16S PCR Assay Performance | |||||
| Sensitivity (correct prediction of positive) | 77.5% (95% CI: 66.0–86.5%) | 7.0% (95% CI: 2.3–15.7%) | 64.6% (95% CI: 51.8–76.1%) | 25.0% (95% CI: 13.6–39.6%) | 60.3% (95% CI: 47.2–72.4%) |
| Specificity (correct prediction of negative) | 46.2% (95% CI: 39.8–52.8%) | 94.5% (95% CI: 90.8–97.1%) | 37.3% (95% CI: 30.8–44.4%) | 61.9% (95% CI: 52.5–70.65%) | 45.0% (95% CI: 37.4–52.1%) |
| Positive Predictive Value | 30.1% (95% CI: 26.6–33.8%) | 27.8% (95% CI: 12.4–51.0%) | 24.3% (95% CI: 20.7–28.3%) | 21.1% (95% CI: 13.4–31.4%) | 27.0% (95% CI: 22.5–31.9%) |
| Negative Predictive Value | 87.3% (95% CI: 81.4–91.5%) | 77.3% (95% CI: 76.1–78.5%) | 77.2% (95% CI: 70.0–83.1%) | 67.0% (95% CI: 62.0–71.6%) | 76.9% (95% CI: 70.2–82.4%) |
| Accuracy | 53.4% (95% CI: 47.7–59.1%) | 74.4% (95% CI: 69.1–79.2%) | 43.0% (95% CI: 37.8–49.9%) | 51.2% (95% CI: 43.3–59.0%) | 48.6% (95% CI: 42.2–55.0%) |
| Odds Ratio | 2.95 | 1.31 | 1.09 | 0.54 | 1.22 |
| Relative Risk | 2.37 | 1.22 | 1.07 | 0.64 | 1.16 |
| CVR Specimens (N = 158) | Gram PMN (N = 158, 55.7%) | Gram Organism (N = 158, 55.7%) | WBC > 9.0 × 109/L (N = 148, 56.1%) | Neutrophils HIGH (N = 59, 54.2%) | CRP > 50 mg/L (N = 47, 68.1%) |
|---|---|---|---|---|---|
| TRUE POSITIVE (Parameter predicts positive/16S positive) | 42 | 20 | 82 | 26 | 26 |
| FALSE POSITIVE (Parameter predicts positive/16S negative) | 15 | 2 | 58 | 13 | 8 |
| FALSE NEGATIVE (Parameter predicts negative/16S positive) | 46 | 68 | 1 | 6 | 6 |
| TRUE NEGATIVE (Parameter predicts negative/16S negative) | 55 | 68 | 5 | 14 | 7 |
| BR 16S PCR Assay Performance | |||||
| Sensitivity (correct prediction of positive) | 47.7% (95% CI: 37.0–58.7%) | 22.7% (95% CI: 14.5–32.9%) | 98.8% (95% CI: 93.5–99.9%) | 81.3% (95% CI: 63.6–92.8%) | 81.3% (95% CI: 63.6–92.8%) |
| Specificity (correct prediction of negative) | 78.6% (95% CI: 67.1–87.5%) | 97.1% (95% CI: 90.1–99.7%) | 7.9% (95% CI: 2.6–17.6%) | 51.9% (95% CI: 32.9–71.3%) | 46.7% (95% CI: 21.3–73.4%) |
| Positive Predictive Value | 73.7% (95% CI: 63.0–82.2%) | 90.9% (95% CI: 70.8–97.6%) | 58.6% (95% CI: 56.7–60.4%) | 66.7% (95% CI: 56.6–75.4%) | 76.5% (95% CI: 66.3–84.3%) |
| Negative Predictive Value | 54.5% (95% CI: 48.6–60.2%) | 50.0% (95% CI: 47.0–53.0%) | 83.3% (95% CI: 37.5–97.7%) | 70.0% (95% CI: 60.0–84.0%) | 53.9% (95% CI: 32.1–74.2%) |
| Accuracy | 61.4% (95% CI: 53.3–69.0%) | 55.7% (95% CI: 47.6–63.6%) | 59.6% (95% CI: 51.2–67.6%) | 67.8% (95% CI: 54.4–79.4%) | 70.2% (95% CI: 55.1–82.7%) |
| Odds Ratio | 3.35 | 10.00 | 7.07 | 4.67 | 3.79 |
| Relative Risk | 1.62 | 1.82 | 3.51 | 2.22 | 1.66 |
| CSF Specimens (N = 101) | Gram PMN (N = 101, 24.8%) | Gram Organism (N = 101, 24.8%) | WBC > 9.0 × 109/L (N = 95, 24.2%) | Neutrophils HIGH (N = 69, 21.7%) | CRP > 50 mg/L (N = 66, 22.7%) |
|---|---|---|---|---|---|
| TRUE POSITIVE (Parameter predicts positive/16S positive) | 24 | 14 | 22 | 11 | 11 |
| FALSE POSITIVE (Parameter predicts positive/16S negative) | 36 | 2 | 49 | 19 | 13 |
| FALSE NEGATIVE (Parameter predicts negative/16S positive) | 1 | 11 | 1 | 4 | 4 |
| TRUE NEGATIVE (Parameter predicts negative/16S negative) | 40 | 74 | 23 | 35 | 38 |
| BR 16S PCR Assay Performance | |||||
| Sensitivity (correct prediction of positive) | 96% (95% CI: 79.7–99.9%) | 56% (95% CI: 34.9–75.6%) | 95.7% (95% CI: 78.1–99.9%) | 73.3% (95% CI: 44.9–92.2%) | 73.3% (95% CI: 44.9–92.2%) |
| Specificity (correct prediction of negative) | 52.6% (95% CI: 40.8–64.2%) | 97.4% (95% CI: 90.8–99.7%) | 31.9% (95% CI: 21.4–44.0%) | 64.8% (95% CI: 50.6–77.3%) | 74.5% (95% CI: 60.4–85.7%) |
| Positive Predictive Value | 40.0% (95% CI: 34.2–46.1%) | 87.5% (95% CI: 63.1–96.6%) | 31.0% (95% CI: 27.3–35.0%) | 36.7% (95% CI: 26.5–48.2%) | 45.8% (95% CI: 32.6–59.7%) |
| Negative Predictive Value | 97.6% (95% CI: 85.3–99.6%) | 87.1% (95% CI: 81.2–91.3%) | 95.8% (95% CI: 76.7–99.4%) | 89.7% (95% CI: 78.7–95.4%) | 90.5% (95% CI: 80.2–95.7%) |
| Accuracy | 63.4% (95% CI: 53.2–72.7%) | 87.1% (95% CI: 79.0–93.0%) | 47.4% (95% CI: 37.0–57.9%) | 66.7% (95% CI: 54.3–77.6%) | 74.2% (95% CI: 62.0–84.2%) |
| Odds Ratio | 26.67 | 47.09 | 10.33 | 5.07 | 8.04 |
| Relative Risk | 16.40 | 6.76 | 7.44 | 3.58 | 4.81 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Griener, T.; Chow, B.; Church, D. Detection of Pathogens by a Novel User-Developed Broad-Range BR 16S PCR rRNA Polymerase Chain Reaction/Gene Sequencing Assay: Multiyear Experience in a Large Canadian Healthcare Zone. Microorganisms 2026, 14, 240. https://doi.org/10.3390/microorganisms14010240
Griener T, Chow B, Church D. Detection of Pathogens by a Novel User-Developed Broad-Range BR 16S PCR rRNA Polymerase Chain Reaction/Gene Sequencing Assay: Multiyear Experience in a Large Canadian Healthcare Zone. Microorganisms. 2026; 14(1):240. https://doi.org/10.3390/microorganisms14010240
Chicago/Turabian StyleGriener, Thomas, Barbara Chow, and Deirdre Church. 2026. "Detection of Pathogens by a Novel User-Developed Broad-Range BR 16S PCR rRNA Polymerase Chain Reaction/Gene Sequencing Assay: Multiyear Experience in a Large Canadian Healthcare Zone" Microorganisms 14, no. 1: 240. https://doi.org/10.3390/microorganisms14010240
APA StyleGriener, T., Chow, B., & Church, D. (2026). Detection of Pathogens by a Novel User-Developed Broad-Range BR 16S PCR rRNA Polymerase Chain Reaction/Gene Sequencing Assay: Multiyear Experience in a Large Canadian Healthcare Zone. Microorganisms, 14(1), 240. https://doi.org/10.3390/microorganisms14010240






