Surface Display of Avian H5 and H9 Hemagglutinin Antigens on Non-Genetically Modified Lactobacillus Cells for Bivalent Oral AIV Vaccine Development
Abstract
1. Introduction
2. Materials and Methods
2.1. Virus Propagation and Microbial Culture Conditions
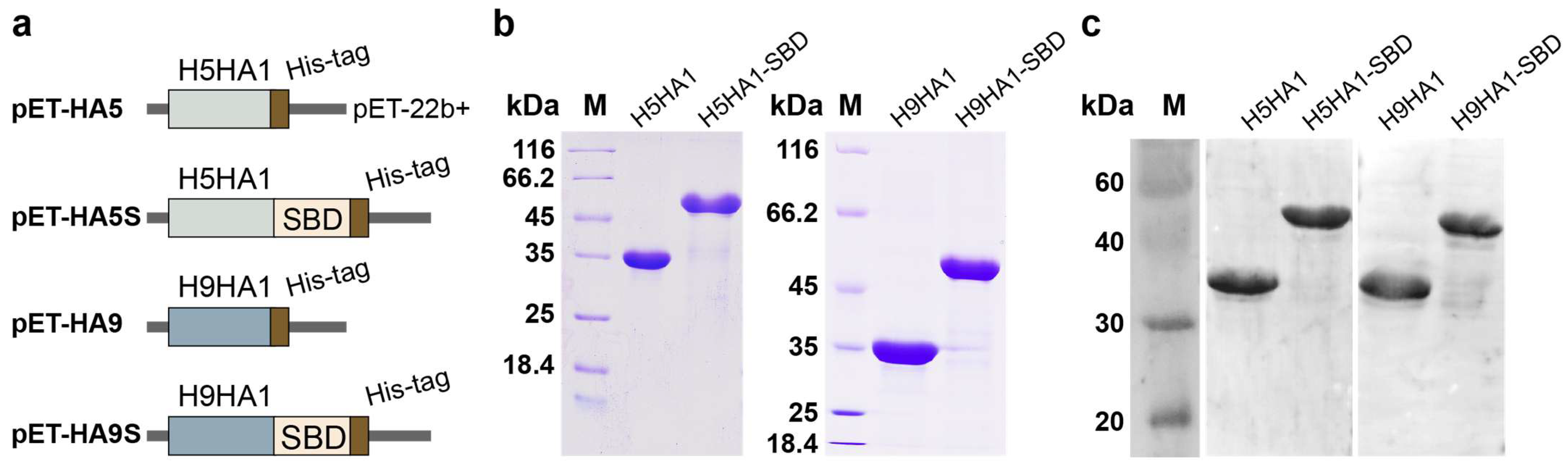
2.2. Construction of Expression Plasmids for HA and HA-SBD Fusion Proteins
2.3. Expression and Purification of the HA1 and HA1-SBD Proteins in E. coli
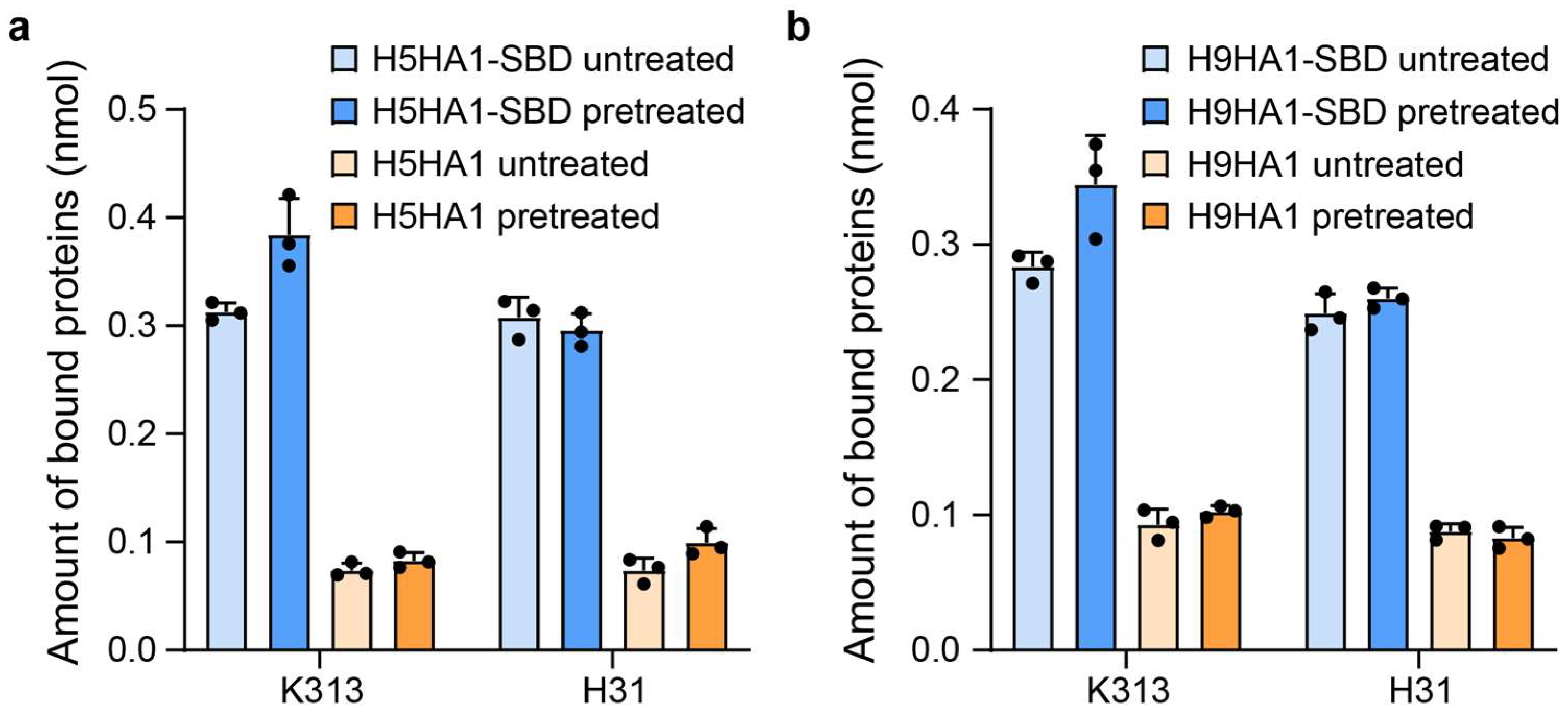
2.4. Binding of HA-SBD Proteins to Cell Surfaces of Lactobacillus
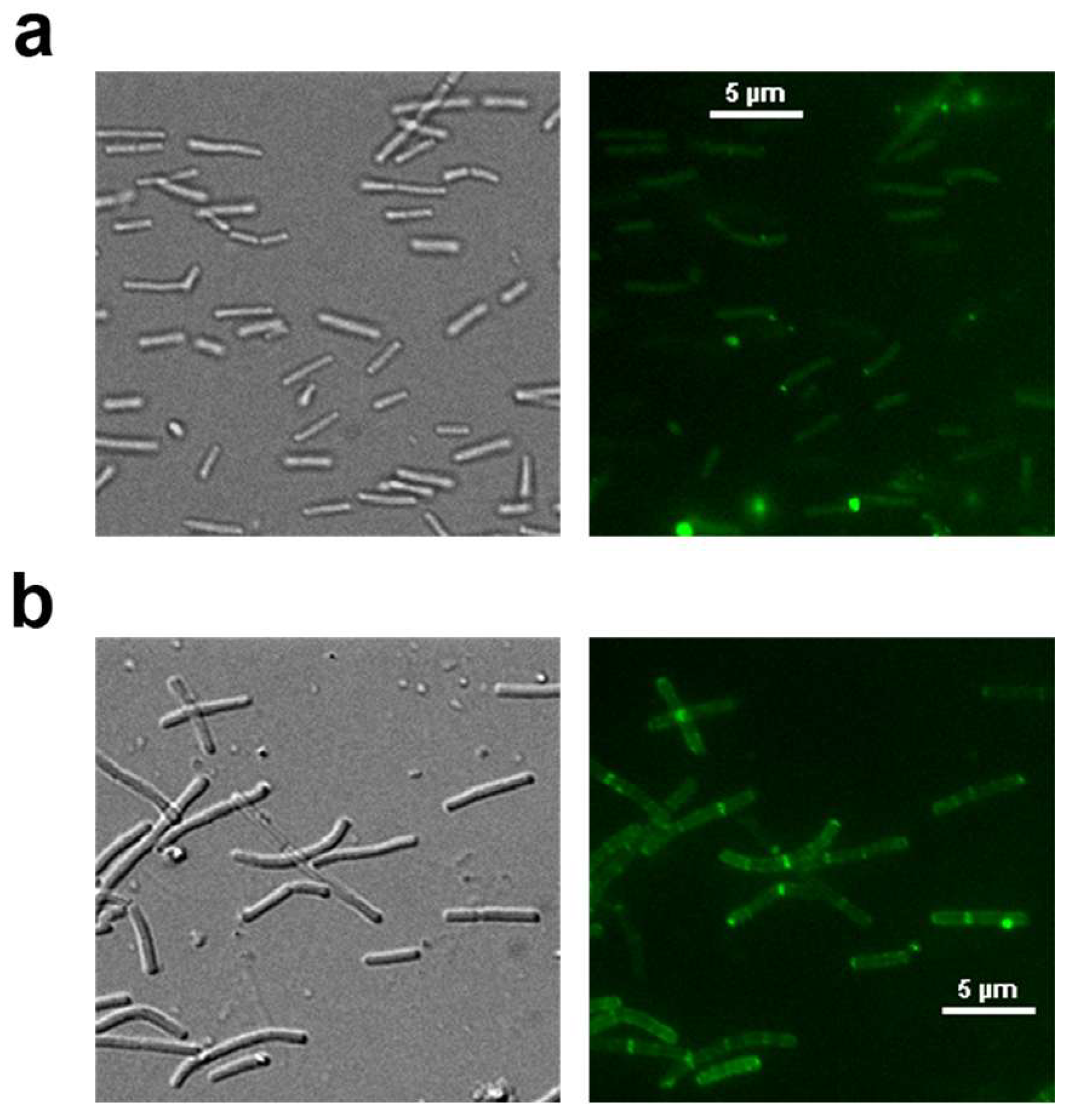
2.5. Immunofluorescence Detection of HA1-SBD on Lactobacillus Cell Surfaces
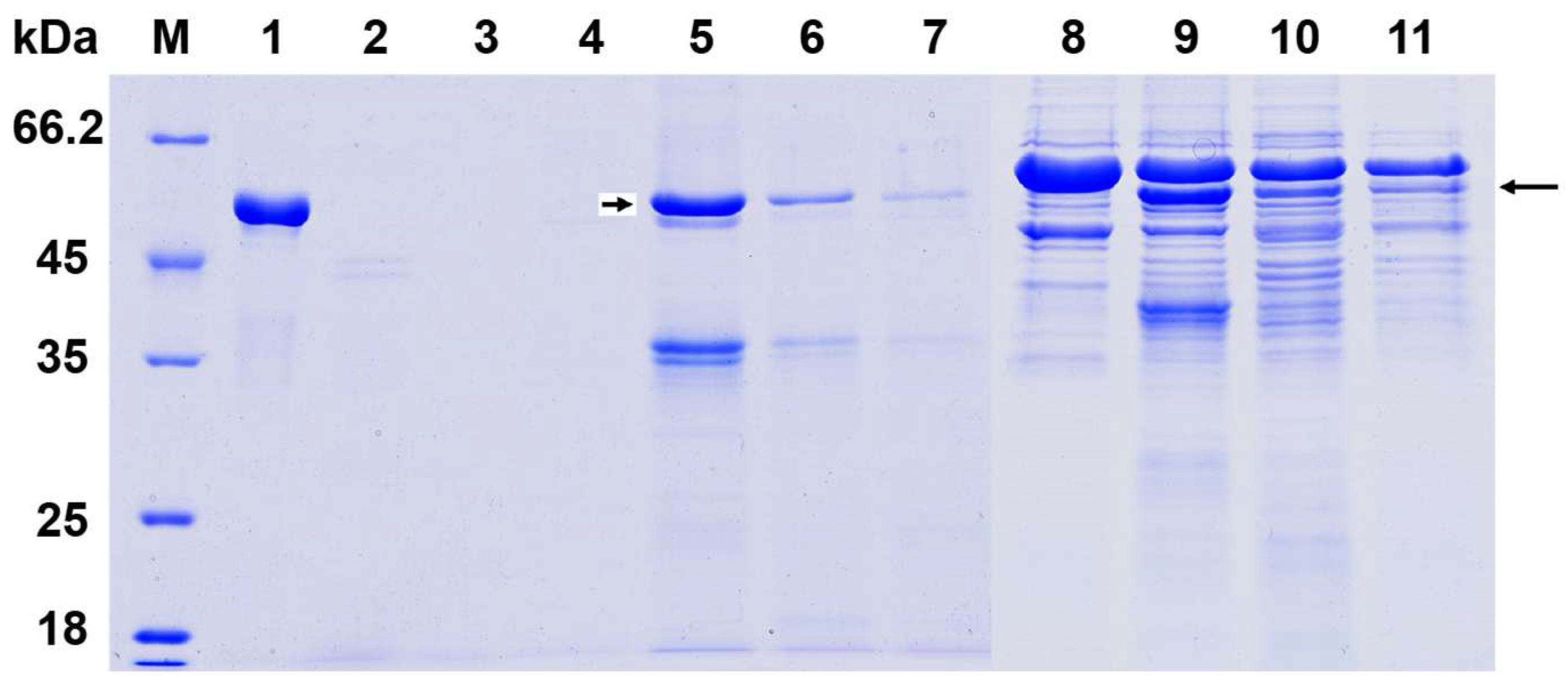
2.6. Enzymatic Treatment of Surface-Anchored HA1-SBD on Lactobacillus Cells
2.7. Vaccine Preparation and Immunization of Mice
2.8. Measurement of Specific Antibodies in Serum and Intestinal Lavage Fluids
3. Results
3.1. Expression and Purification of HA1 and HA1-SBD Proteins in E. coli
3.2. Binding of the Purified Fusion Proteins to the Cell Wall Surface of Lactobacillus
3.3. Protease Tolerance of Surface-Displayed Fusion Proteins on Lactobacillus
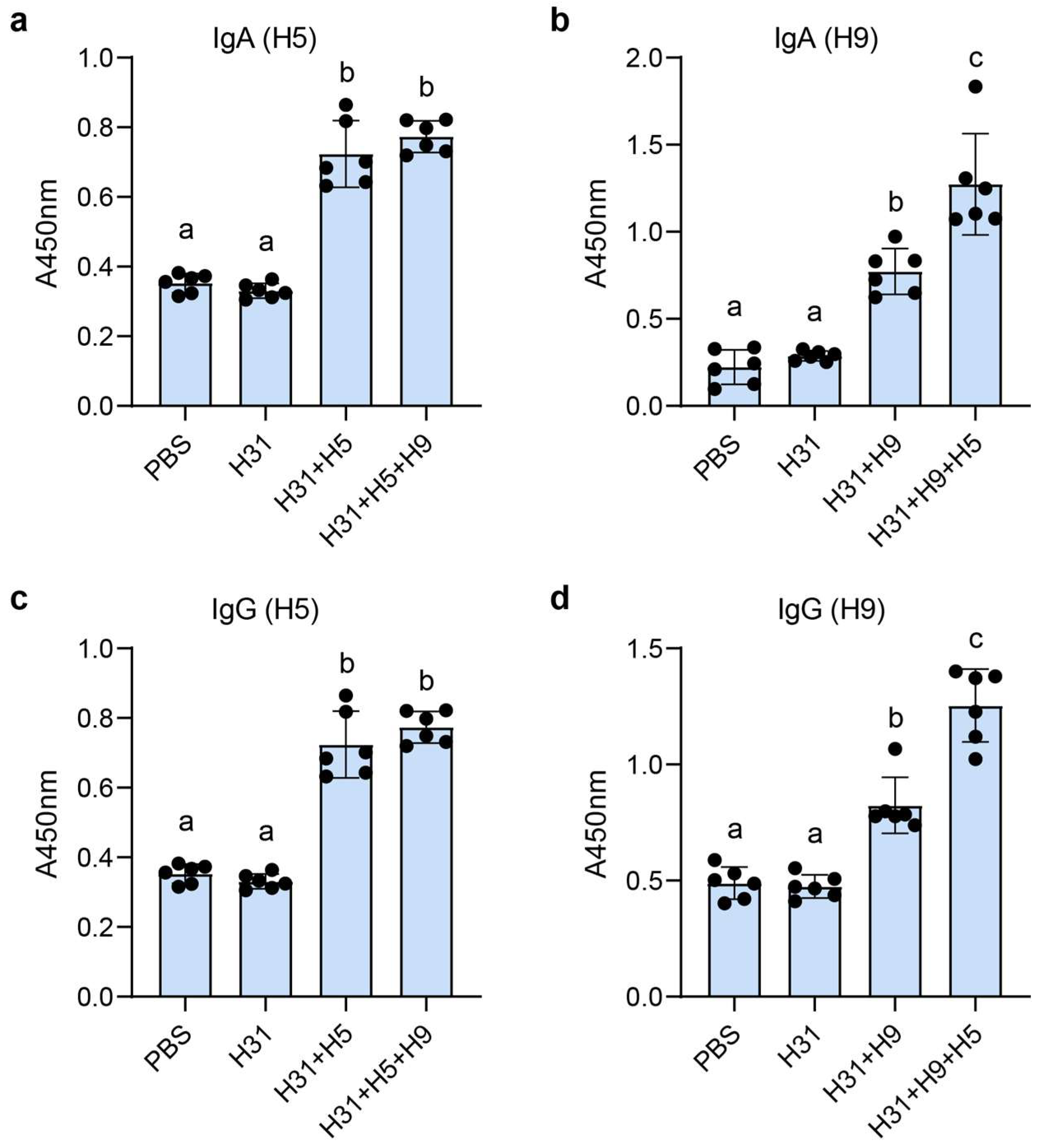
3.4. HA-Specific IgG and IgA Responses After Oral Administration
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fernández, M.F.; Boris, S.; Barbes, C. Probiotic properties of human lactobacilli strains to be used in the gastrointestinal tract. J. Appl. Microbiol. 2003, 94, 449–455. [Google Scholar] [CrossRef] [PubMed]
- O’Callaghan, J.; O’Toole, P.W. Lactobacillus: Host–microbe relationships. In Between Pathogenicity and Commensalism; Springer: Berlin/Heidelberg, Germany, 2013; pp. 119–154. [Google Scholar]
- Wells, J.M. Immunomodulatory mechanisms of lactobacilli. Microb. Cell Factories 2011, 10, S17. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, E.; Corr, S.C. Lactobacillus spp. for gastrointestinal health: Current and future perspectives. Front. Immunol. 2022, 13, 840245. [Google Scholar] [CrossRef] [PubMed]
- Maassen, C.; Laman, J.; den Bak-Glashouwer, M.H.; Tielen, F.; van Holten-Neelen, J.; Hoogteijling, L.; Antonissen, C.; Leer, R.; Pouwels, P.; Boersma, W. Instruments for oral disease-intervention strategies: Recombinant Lactobacillus casei expressing tetanus toxin fragment C for vaccination or myelin proteins for oral tolerance induction in multiple sclerosis. Vaccine 1999, 17, 2117–2128. [Google Scholar] [CrossRef]
- Seegers, J.F. Lactobacilli as live vaccine delivery vectors: Progress and prospects. Trends Biotechnol. 2002, 20, 508–515. [Google Scholar] [CrossRef]
- Bermúdez-Humarán, L.G.; Kharrat, P.; Chatel, J.-M.; Langella, P. Lactococci and lactobacilli as mucosal delivery vectors for therapeutic proteins and DNA vaccines. Microb. Cell Factories 2011, 10, S4. [Google Scholar] [CrossRef]
- Wen, L.-J.; Hou, X.-L.; Wang, G.-H.; Yu, L.-Y.; Wei, X.-M.; Liu, J.-K.; Liu, Q.; Wei, C.-H. Immunization with recombinant Lactobacillus casei strains producing K99, K88 fimbrial protein protects mice against enterotoxigenic Escherichia coli. Vaccine 2012, 30, 3339–3349. [Google Scholar] [CrossRef]
- Wyszyńska, A.; Kobierecka, P.; Bardowski, J.; Jagusztyn-Krynicka, E.K. Lactic acid bacteria—20 years exploring their potential as live vectors for mucosal vaccination. Appl. Microbiol. Biotechnol. 2015, 99, 2967–2977. [Google Scholar] [CrossRef]
- Raha, A.; Varma, N.; Yusoff, K.; Ross, E.; Foo, H. Cell surface display system for Lactococcus lactis: A novel development for oral vaccine. Appl. Microbiol. Biotechnol. 2005, 68, 75–81. [Google Scholar] [CrossRef]
- Antikainen, J.; Anton, L.; Sillanpää, J.; Korhonen, T.K. Domains in the S-layer protein CbsA of Lactobacillus crispatus involved in adherence to collagens, laminin and lipoteichoic acids and in self-assembly. Mol. Microbiol. 2002, 46, 381–394. [Google Scholar] [CrossRef]
- Smit, E.; Jager, D.; Martinez, B.; Tielen, F.J.; Pouwels, P.H. Structural and functional analysis of the S-layer protein crystallisation domain of Lactobacillus acidophilus ATCC 4356: Evidence for protein–protein interaction of two subdomains. J. Mol. Biol. 2002, 324, 953–964. [Google Scholar] [CrossRef] [PubMed]
- Åvall-Jääskeläinen, S.; Hynönen, U.; Ilk, N.; Pum, D.; Sleytr, U.B.; Palva, A. Identification and characterization of domains responsible for self-assembly and cell wall binding of the surface layer protein of Lactobacillus brevis ATCC 8287. BMC Microbiol. 2008, 8, 165. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Kong, J.; Sun, Z.; Han, L.; Kong, W.; Yang, P. Heterologous protein display on the cell surface of lactic acid bacteria mediated by the s-layer protein. Microb. Cell Factories 2011, 10, 86. [Google Scholar] [CrossRef]
- Sun, Z.; Kong, J.; Hu, S.; Kong, W.; Lu, W.; Liu, W. Characterization of a S-layer protein from Lactobacillus crispatus K313 and the domains responsible for binding to cell wall and adherence to collagen. Appl. Microbiol. Biotechnol. 2013, 97, 1941–1952. [Google Scholar] [CrossRef]
- Uriza, P.J.; Trautman, C.; Palomino, M.M.; Fina Martin, J.; Ruzal, S.M.; Roset, M.S.; Briones, G. Development of an antigen delivery platform using Lactobacillus acidophilus decorated with heterologous proteins: A sheep in wolf’s clothing story. Front. Microbiol. 2020, 11, 509380. [Google Scholar] [CrossRef]
- Spackman, E. A Brief Introduction to Avian Influenza Virus. Methods Mol. Biol. 2020, 2123, 83–92. [Google Scholar]
- Tong, S.; Zhu, X.; Li, Y.; Shi, M.; Zhang, J.; Bourgeois, M.; Yang, H.; Chen, X.; Recuenco, S.; Gomez, J. New world bats harbor diverse influenza A viruses. PLoS Pathog. 2013, 9, e1003657. [Google Scholar] [CrossRef]
- Ciminski, K.; Schwemmle, M. Bat-borne influenza A viruses: An awakening. Cold Spring Harb. Perspect. Med. 2021, 11, a038612. [Google Scholar] [CrossRef]
- Wu, N.C.; Wilson, I.A. Influenza hemagglutinin structures and antibody recognition. Cold Spring Harb. Perspect. Med. 2020, 10, a038778. [Google Scholar] [CrossRef]
- Shirvani, E.; Paldurai, A.; Varghese, B.P.; Samal, S.K. Contributions of HA1 and HA2 subunits of highly pathogenic avian influenza virus in induction of neutralizing antibodies and protection in chickens. Front. Microbiol. 2020, 11, 1085. [Google Scholar] [CrossRef]
- Carascal, M.B.; Pavon, R.D.N.; Rivera, W.L. Recent progress in recombinant influenza vaccine development toward heterosubtypic immune response. Front. Immunol. 2022, 13, 878943. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Xu, T.; Li, Z.; Li, L.; Li, C.; Li, X.; Wang, Z.; Wang, S.; Wang, X.; Zhang, H. Vaccination with recombinant Lactococcus lactis expressing HA1-IgY Fc fusion protein provides protective mucosal immunity against H9N2 avian influenza virus in chickens. Virol. J. 2023, 20, 76. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Peng, C.; Chen, L.; Wang, P.; Wang, F. Construction and Immunogenicity Evaluation of Recombinant Bacillus subtilis Expressing HA1 Protein of H9N2 Avian Influenza Virus. Curr. Microbiol. 2024, 81, 25. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Liu, Y.; Luo, C.; Zhou, M.; Wang, K.; Xie, Q.; Zhang, Q.; Zhang, Q.; Li, Q.; Pan, Z. Identification and characterization of a broadly neutralizing and protective nanobody against the HA1 domain of H5 avian influenza virus hemagglutinin. J. Virol. 2025, 99, e02090-24. [Google Scholar] [CrossRef]
- Hoffmann, E.; Stech, J.; Guan, Y.; Webster, R.; Perez, D. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 2001, 146, 2275–2289. [Google Scholar] [CrossRef]
- Vasquez, R.; Bagon, B.B.; Song, J.H.; Han, N.S.; Kang, D.-K. A novel, non-GMO surface display in Limosilactobacillus fermentum mediated by cell surface hydrolase without anchor motif. BMC Microbiol. 2022, 22, 190. [Google Scholar] [CrossRef]
- Hagen, K.E.; Guan, L.L.; Tannock, G.W.; Korver, D.R.; Allison, G.E. Detection, characterization, and in vitro and in vivo expression of genes encoding S-proteins in Lactobacillus gallinarum strains isolated from chicken crops. Appl. Environ. Microbiol. 2005, 71, 6633–6643. [Google Scholar] [CrossRef]
- Hu, S.; Kong, J.; Kong, W.; Guo, T.; Ji, M. Characterization of a novel LysM domain from Lactobacillus fermentum bacteriophage endolysin and its use as an anchor to display heterologous proteins on the surfaces of lactic acid bacteria. Appl. Environ. Microbiol. 2010, 76, 2410–2418. [Google Scholar] [CrossRef]
- Bosma, T.; Kanninga, R.; Neef, J.; Audouy, S.A.; van Roosmalen, M.L.; Steen, A.; Buist, G.; Kok, J.; Kuipers, O.P.; Robillard, G. Novel surface display system for proteins on non-genetically modified gram-positive bacteria. Appl. Environ. Microb. 2006, 72, 880–889. [Google Scholar] [CrossRef]
- Åvall-Jääskeläinen, S.; Kylä-Nikkilä, K.; Kahala, M.; Miikkulainen-Lahti, T.; Palva, A. Surface Display of Foreign Epitopes on the Lactobacillus brevis S-Layer. Appl. Environ. Microbiol. 2002, 68, 5943–5951. [Google Scholar] [CrossRef]
- Mathiesen, G.; Øverland, L.; Kuczkowska, K.; Eijsink, V.G.H. Anchoring of heterologous proteins in multiple Lactobacillus species using anchors derived from Lactobacillus plantarum. Sci. Rep. 2020, 10, 9640. [Google Scholar] [CrossRef] [PubMed]
- Reveneau, N.; Geoffroy, M.-C.; Locht, C.; Chagnaud, P.; Mercenier, A. Comparison of the immune responses induced by local immunizations with recombinant Lactobacillus plantarum producing tetanus toxin fragment C in different cellular locations. Vaccine 2002, 20, 1769–1777. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, E.E.; Mollet, B.; Willem, M.d. Functionality of probiotics and intestinal lactobacilli: Light in the intestinal tract tunnel. Curr. Opin. Biotechnol. 1999, 10, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.H.-C.; Savage, D.C. Host specificity of the colonization of murine gastric epithelium by lactobacilli. FEMS Microbiol. Lett. 1984, 24, 67–71. [Google Scholar] [CrossRef]
- Ravikumar, R.; Chan, J.; Prabakaran, M. Vaccines against Major Poultry Viral Diseases: Strategies to Improve the Breadth and Protective Efficacy. Viruses 2022, 14, 1195. [Google Scholar] [CrossRef]
- LeCureux, J.S.; Dean, G.A. Lactobacillus Mucosal Vaccine Vectors: Immune Responses against Bacterial and Viral Antigens. mSphere 2018, 3, e00061-18. [Google Scholar] [CrossRef]
| Material | Relevant Features | Source or Reference |
|---|---|---|
| Virus | ||
| Influenza A virus (A/chicken/Shandong/ K01/2004(H5N1)) | Used for cloning hemagglutinin gene | This study |
| Influenza A virus (A/chicken/Shandong/ K02/2004(H9N2)) | Used for cloning hemagglutinin gene | This study |
| Strains | ||
| E. coli DH5α | Cloning host | TaKaRa |
| Origami B (DE3) | Expression host | Novagen |
| Lactobacillus crispatus K313 | Used for cloning the S-layer protein and binding the antigen | [15] |
| Lactobacillus johnsonii H31 | Used for binding the antigen | [15] |
| Plasmids | ||
| pET-22b (+) | E. coli expression vector, T7 promoter, AmpR | Novagen |
| pET-SBD | pET2209; pET-22b (+) carrying S-layer protein cell wall binding domain (from 342 aa to 501 aa) of Lactobacillus crispatus K313; expressing His6-tagged SBD | [15] |
| pET-HA5 | pET-22b (+) vector containing H5HA1 gene inserted between NdeI and BamHI restriction sites for expression of His6-tagged H5HA1 protein | This study |
| pET-HA5S | H5HA1 was inserted into NdeI/BamHI sites of pET-SBD to express His6-tagged H5HA1-SBD fusion protein | This study |
| pET-HA9 | pET-22b (+) vector containing H9HA1 gene inserted between NdeI and BamHI restriction sites for expression of His6-tagged H9HA1 protein | This study |
| pET-HA9S | H9HA1 was inserted into NdeI/BamHI sites of pET-SBD to express His6-tagged H5HA1-SBD fusion protein | This study |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, F.; Chang, J.; Huang, J.; Liao, Y.; Deng, X.; Guo, T.; Kong, J.; Kong, W. Surface Display of Avian H5 and H9 Hemagglutinin Antigens on Non-Genetically Modified Lactobacillus Cells for Bivalent Oral AIV Vaccine Development. Microorganisms 2025, 13, 1649. https://doi.org/10.3390/microorganisms13071649
Liu F, Chang J, Huang J, Liao Y, Deng X, Guo T, Kong J, Kong W. Surface Display of Avian H5 and H9 Hemagglutinin Antigens on Non-Genetically Modified Lactobacillus Cells for Bivalent Oral AIV Vaccine Development. Microorganisms. 2025; 13(7):1649. https://doi.org/10.3390/microorganisms13071649
Chicago/Turabian StyleLiu, Fuyi, Jingbo Chang, Jingqi Huang, Yuping Liao, Xiaonan Deng, Tingting Guo, Jian Kong, and Wentao Kong. 2025. "Surface Display of Avian H5 and H9 Hemagglutinin Antigens on Non-Genetically Modified Lactobacillus Cells for Bivalent Oral AIV Vaccine Development" Microorganisms 13, no. 7: 1649. https://doi.org/10.3390/microorganisms13071649
APA StyleLiu, F., Chang, J., Huang, J., Liao, Y., Deng, X., Guo, T., Kong, J., & Kong, W. (2025). Surface Display of Avian H5 and H9 Hemagglutinin Antigens on Non-Genetically Modified Lactobacillus Cells for Bivalent Oral AIV Vaccine Development. Microorganisms, 13(7), 1649. https://doi.org/10.3390/microorganisms13071649





