Occupational Risk from Avian Influenza Viruses at Different Ecological Interfaces Between 1997 and 2019
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.1.1. Poultry
PubMed
Scopus
2.1.2. Wild Birds
PubMed
Scopus
2.2. Eligibility Criteria
- -
- Articles published in peer-reviewed journals;
- -
- English language;
- -
- Publication period: no limit of years (up to August 2019);
- -
- Observational studies (including cross-sectional, seroprevalence, retrospective, case–control, case-report);
- -
- Occupational exposure to AIV;
- -
- Working population: all ages, both sexes, all ethnic groups;
- -
- Avian influenza viruses: all subtypes;
- -
- Tests used in virological studies: AIV molecular detection and characterization (PCR, sequencing); virus isolation methods (embryonated chicken eggs, cell cultures); AIV serological characterization by haemagglutination inhibition assay (HIA), neuraminidase inhibition assay (NIA);
- -
- Tests used in serological studies: HIA; enzyme-linked immunosorbent assay (ELISA); neutralization test (NT), microneutralization assay (MNA), plaque neutralization assay (PNA); Western blot assay (WBA); single radial haemolysis (SRH) assay; IFA, immunofluorescence assay; protein microarray;
- -
- Only studies including tests on humans.
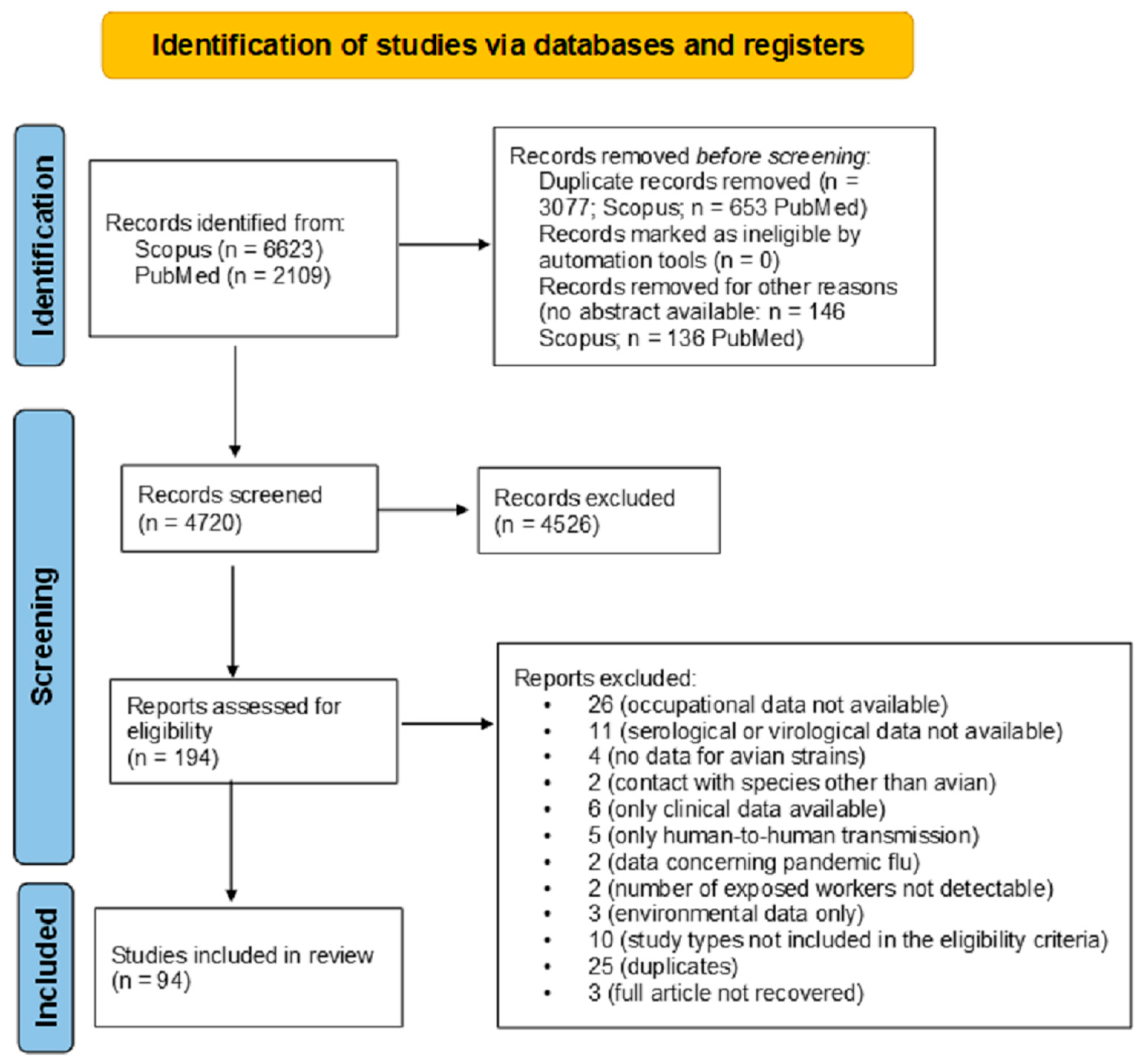
2.3. Study Selection
2.4. Synthesis
3. Results
3.1. Search Results
3.2. Results from the Selected Studies
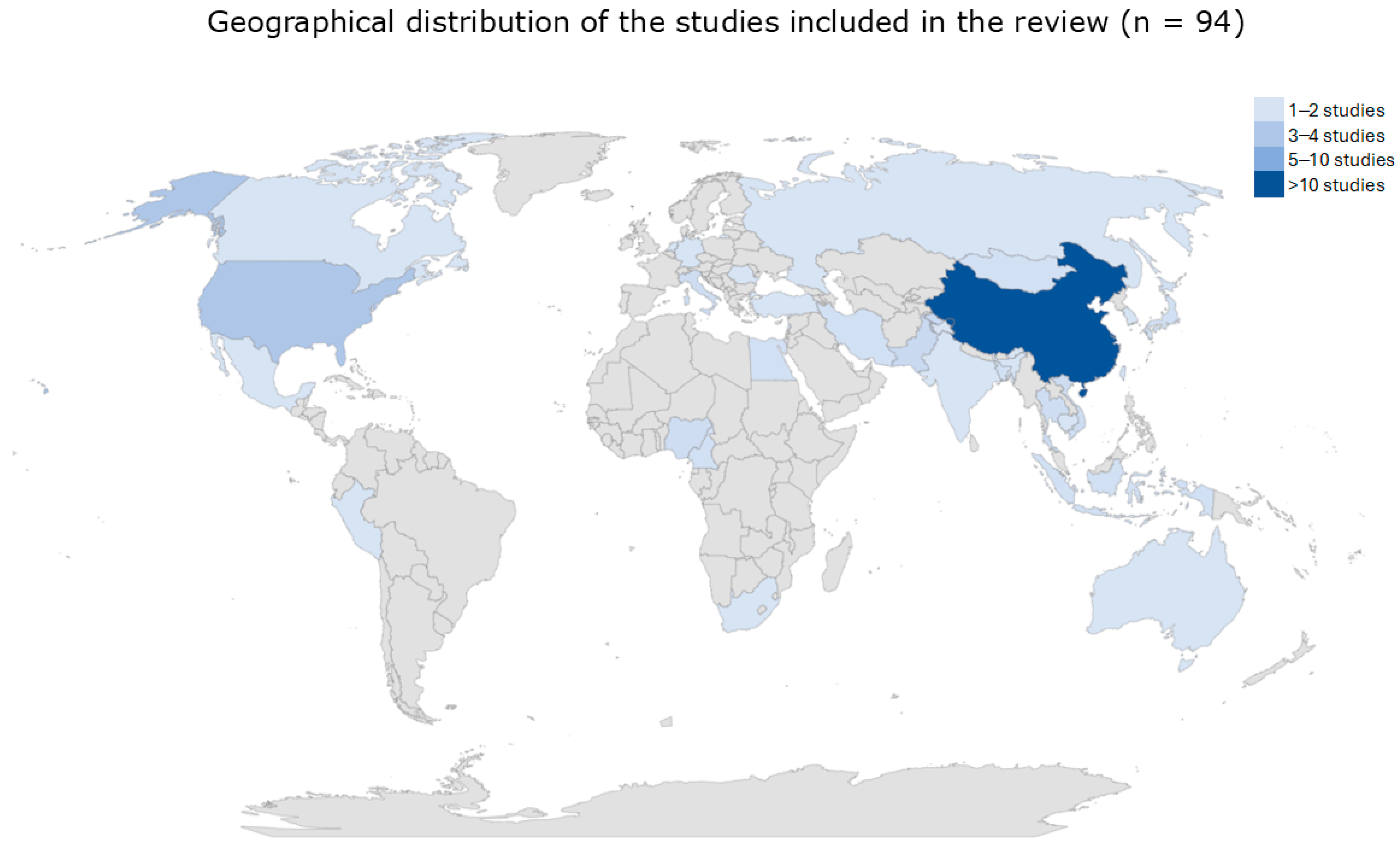
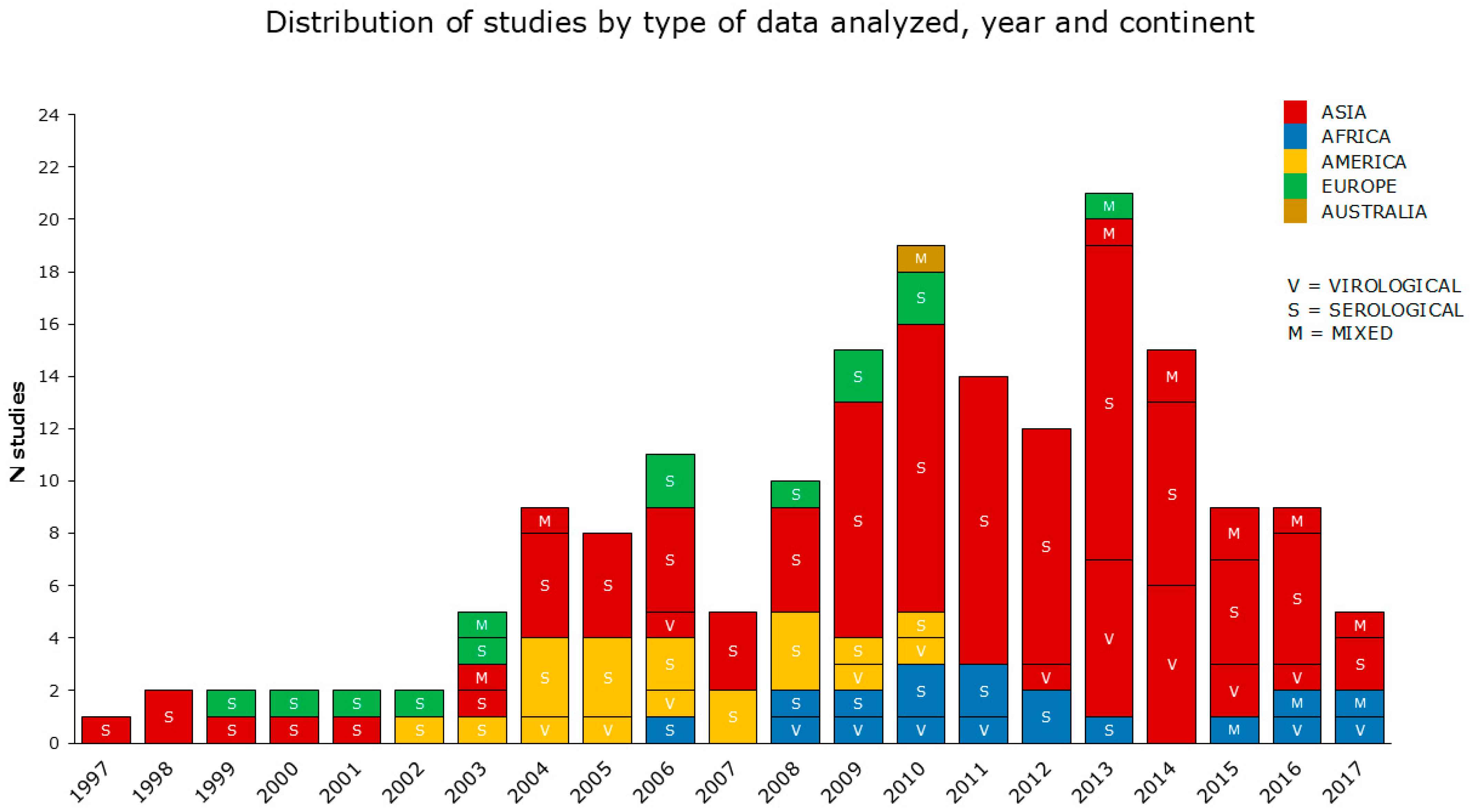
3.2.1. Data Overview
3.2.2. Virological Data
3.2.3. Serological Data
3.2.4. Mixed—Serological and Virological—Data
3.2.5. Occupational Exposure Inferred from Serological Data
3.2.6. Occupational Exposure by Workplace and Work Activities
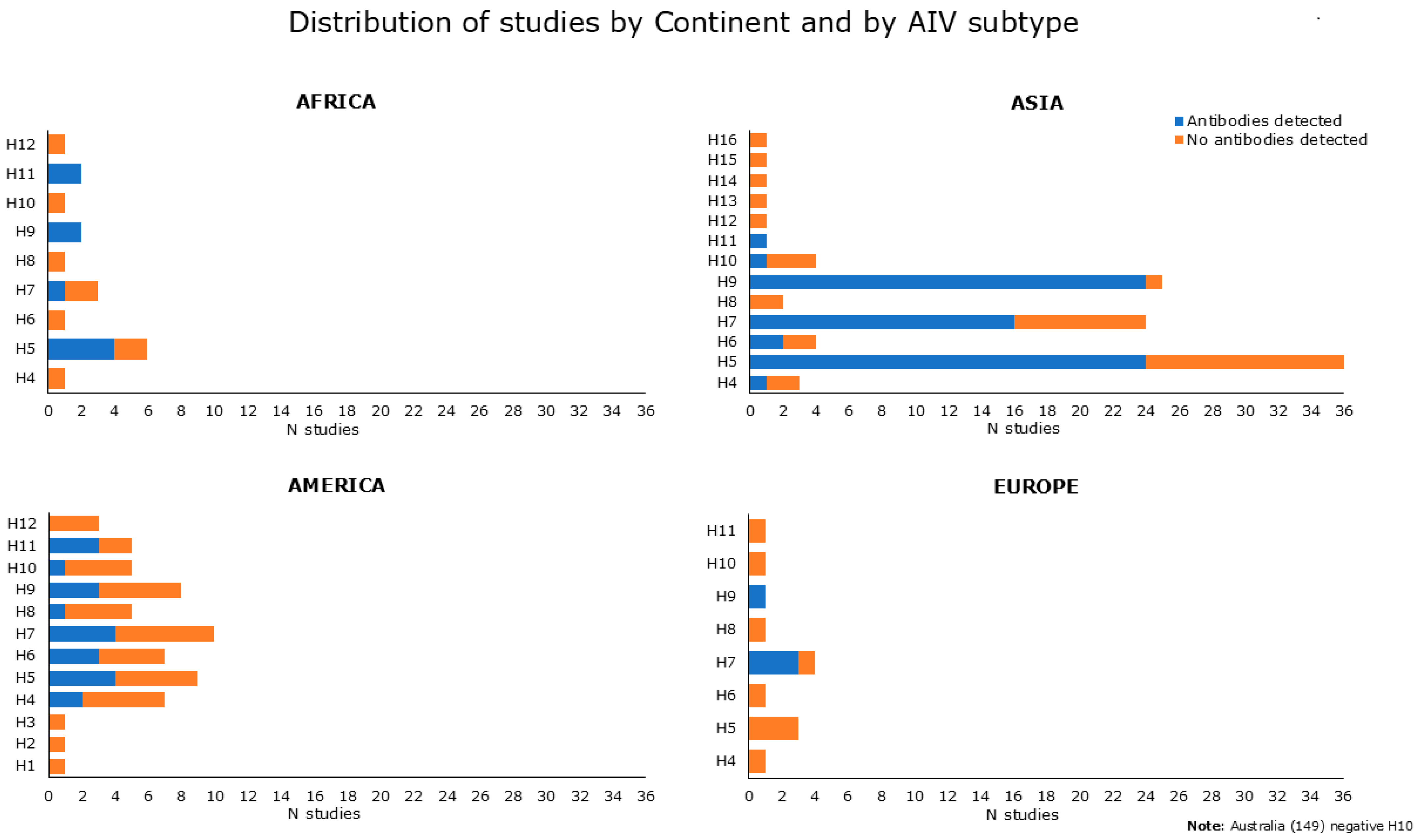
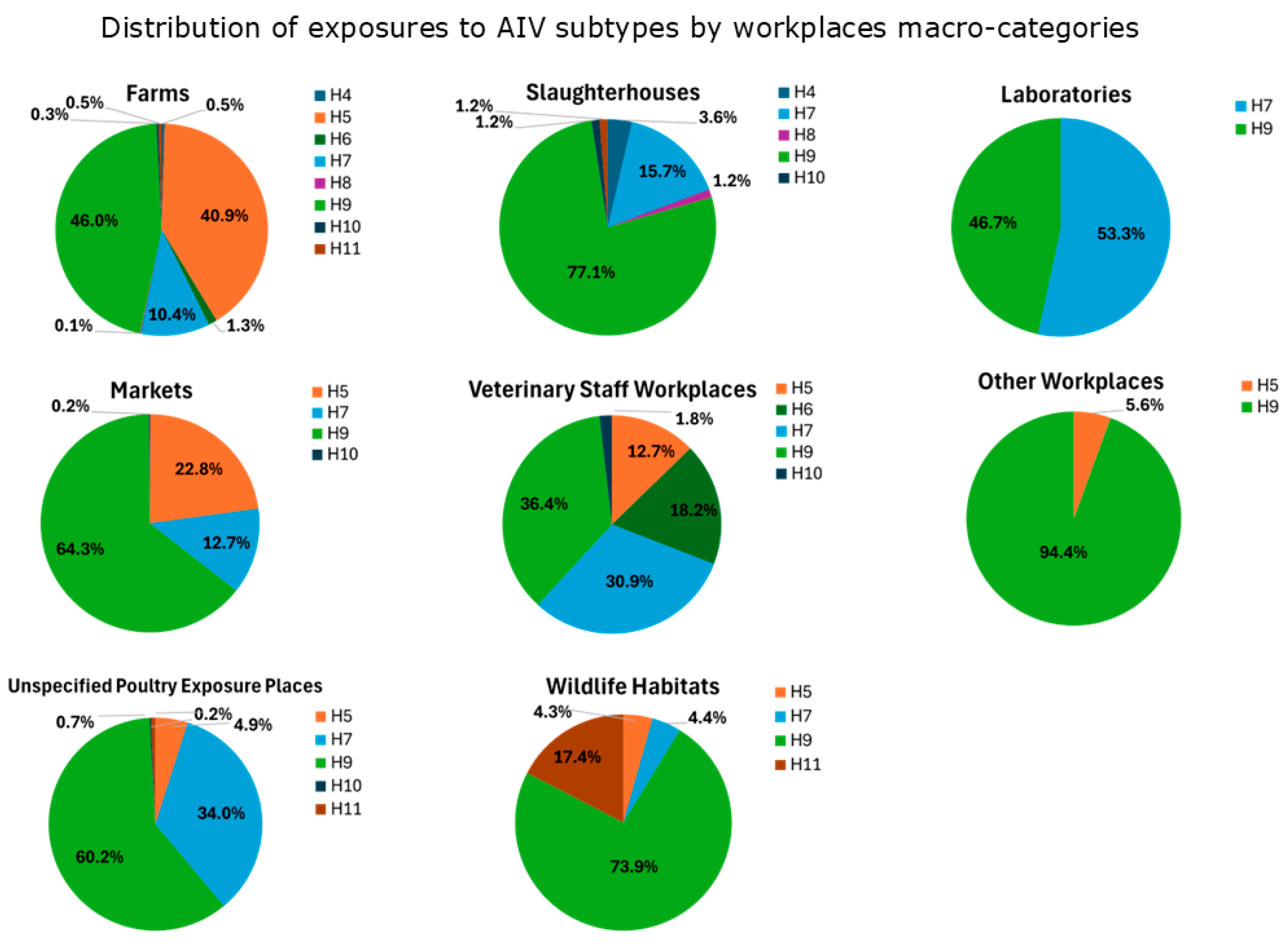
- Exposures to H9 are prevalent across all the workplaces (except for “Laboratories”). “Slaughterhouses”, “Wildlife Habitats”, “Markets” and “Unspecified Poultry Exposure Places” had the highest percentages of exposures (>60%). Studies reporting H9-positive serological results were mostly from Asia (China, Vietnam, Mongolia, Iran, India, Pakistan, and Cambodia) in a time period ranging from 2001 to 2017, but also from Africa (Nigeria) in the period 2008–2011, America (USA) between 2004 and 2010, and Europe (Romania) in the period 2009–2010 (see Appendix B.1).
- Exposures to H7 are more widespread in “Laboratories”, “Unspecified Poultry Exposure Places”, “Veterinary Staff Workplaces”, with percentages over 30%. H7-positive serological results were observed in studies from Asia (China, Pakistan, Taiwan) during a time period that ranged from 2004 to 2016, followed by America (USA) from 2002 to 2010, Europe (Italy, England) in periods between 1999 and 2010, and Africa (South Africa) in the period 2011–2012 (see Appendix B.1).
- The majority of exposures to H5 have been observed in “Farms” (40.9%), “Markets” (22.8%), and “Veterinary Staff Workplaces” (12.7%). H5-positive serological results were observed in Asian studies conducted in many countries (China, Vietnam, South Korea, Japan, Thailand, Mongolia, Bangladesh, Taiwan, Cambodia, Indonesia) in periods varying from 1997 to 2016. Also, studies originating from Africa (Nigeria, South Africa, Cameroon) reported H5-positive serological results in periods between 2008 and 2017, as well as from America (USA) in periods ranging from 2004 to 2010 (see Appendix B.1).
- Regarding other subtypes, exposures to H6 were mainly observed in “Veterinary Staff Workplaces” (18.2%), to H11 in “Wildlife Habitats” (17.4%) and to H4 in “Slaughterhouses” (3.6%). Other subtypes were less represented (H8 in “Farms” and “Slaughterhouses”, less than 1.5%; H10 in “Farms”, “Markets”, “Unspecified Poultry Exposure Places”, “Slaughterhouses”, “Veterinary Staff Workplaces”, less than 1.8%). Studies reporting positive results for these AIV subtypes were conducted in Asia and America (except for H11, which was also in Africa) (see Appendix B.1).
3.2.7. One-Health Approach
3.2.8. Study Design Comparison
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Workplace Macro-Categories Grouping Work Activities (n = 8) | Work Activities (n = 15) | Worker Acronym | Acronym Detail |
|---|---|---|---|
| WLH (Wildlife Habitats) | Wild Bird-Exposed Worker(s) | BBa | bird bander(s) |
| BHa | bird handler(s) | ||
| WBHW | wild bird habitat worker(s) | ||
| WLB | wildlife biologist(s) | ||
| WLE | wildlife exposed | ||
| WLE-GoW | wildlife exposed government worker(s) | ||
| Wild Bird-Exposed Hunter(s) | BHu | bird hunter(s) | |
| DHu | duck hunter(s) | ||
| RSBu | rural subsistence bird hunter | ||
| USpHu | urban sport hunter(s) | ||
| WBHu | wild bird hunter(s) | ||
| F (Farms) | Large-Scale Commercial/Industrial Poultry Farm Worker(s) | CoCFW | commercial chicken farm worker(s) |
| CoPFW | commercial poultry farm worker(s) | ||
| CoPG | commercial poultry grower(s) | ||
| InPFW | industrial poultry farm worker(s) | ||
| InTFW | industrial turkey farm worker(s) | ||
| Large-scale PFW | large-scale poultry farm worker(s) | ||
| PInW | poultry industry worker(s) | ||
| Agricultural Worker(s) | AgW | agricultural worker(s) | |
| AnFW | animal farm worker(s) | ||
| FW | farm worker(s) | ||
| Small-Scale and Backyard Poultry Farm Worker(s) | BaPFW | backyard poultry farm worker(s) | |
| BaPG | backyard poultry grower(s) | ||
| BaTG | backyard turkey grower(s) | ||
| Small-scale PFW | small-scale poultry farm worker(s) | ||
| Poultry Depopulation Worker(s) | DeW | depopulation worker(s) | |
| GoPDeW | government poultry depopulation worker(s) | ||
| GoW | government worker(s) | ||
| PCu | poultry culler(s) | ||
| PDeW | poultry depopulation worker(s) | ||
| Swine Farm Worker(s) | SFW | swine farm worker(s) | |
| CoSFW | commercial swine farm worker(s) | ||
| Poultry Farm Worker(s) * | DFW | duck farm worker(s) | |
| PFW | poultry farm worker(s) | ||
| PG | poultry grower(s) | ||
| M (Markets) | Bird-Exposed Market Worker(s) | LBMW | live bird market worker(s) |
| LPM butcher | live poultry market butcher(s) | ||
| LPMW | live poultry market worker(s) | ||
| LPV | live poultry vendor(s) | ||
| PMW | poultry market worker(s) | ||
| Wholesale market seller | wholesale market seller(s) | ||
| WMW | wet marker worker(s) | ||
| SH (Slaughterhouses) | Slaughterhouse and Poultry Meat-Processing Plant Worker(s) | SHW | slaughterhouse worker(s) |
| PMePr | poultry meat processor(s) | ||
| L (Laboratories) | Laboratory Worker(s) | LW | laboratory worker(s) |
| V (Veterinary Staff Workplaces) | Veterinary Staff Worker(s) | Vaccinators | — |
| Vet | veterinarian(s) | ||
| Veterinary staff | — | ||
| P (Unspecified Poultry Exposure Places) | Poultry Worker(s) | PW | poultry worker(s) |
| (Live/Dead) Poultry Exposed Worker(s) ** | WpE(L/D)PW | worker(s) in workplace(s) involving exposure to (live/dead) poultry | |
| OW (Other Workplaces) | Other Worker(s) | OW | other worker(s) |
Appendix B
Appendix B.1. Distribution of AIV Positive Serological Results
Appendix B.2. Seroconversion Results in AIV Exposed Workers
References
- Webster, R.G.; Bean, W.J.; Gorman, O.T.; Chambers, T.M.; Kawaoka, Y. Evolution and ecology of influenza A viruses. Microbiol. Rev. 1992, 56, 152–179. [Google Scholar] [CrossRef] [PubMed]
- Krammer, F.; Smith, G.J.D.; Fouchier, R.A.M.; Peiris, M.; Kedzierska, K.; Doherty, P.C.; Palese, P.; Shaw, M.L.; Treanor, J.; Webster, R.G.; et al. Influenza. Nat. Rev. Dis. Primers. 2018, 4, 3. [Google Scholar] [CrossRef] [PubMed]
- Webster, R.G.; Govorkova, E.A. Continuing challenges in influenza. Ann. N. Y. Acad. Sci. 2014, 1323, 115–139. [Google Scholar] [CrossRef]
- Runstadler, J.A.; Puryear, W.B. The virus is out of the barn: The emergence of HPAI as a pathogen of avian and mammalian wildlife around the globe. Am. J. Vet Res. 2024, 85, ajvr-24. [Google Scholar] [CrossRef]
- De Jong, J.C.; Rimmelzwaan, G.F.; Fouchier, R.A.; Osterhaus, A.D. Influenza virus: A master of metamorphosis. J. Infect. 2000, 40, 218–228. [Google Scholar] [CrossRef]
- Lycett, S.J.; Duchatel, F.; Digard, P. A brief history of bird flu. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2019, 374, 20180257. [Google Scholar] [CrossRef]
- Morens, D.M.; Taubenberger, J.K. Pandemic influenza: Certain uncertainties. Rev. Med. Virol. 2011, 21, 262–284. [Google Scholar] [CrossRef] [PubMed]
- Neumann, G.; Kawaoka, Y. Transmission of influenza A viruses. Virology 2015, 479, 234–246. [Google Scholar] [CrossRef]
- Sutton, T.C. The pandemic threat of emerging H5 and H7 Avian Influenza viruses. Viruses 2018, 10, 461. [Google Scholar] [CrossRef]
- Mostafa, A.; Abdelwhab, E.M.; Mettenleiter, T.C.; Pleschka, S. Zoonotic potential of Influenza A viruses: A comprehensive over-view. Viruses 2018, 10, 497. [Google Scholar] [CrossRef]
- Van Kerkhove, M.D.; Mumford, E.; Mounts, A.W.; Bresee, J.; Ly, S.; Bridges, C.B.; Otte, J. Highly pathogenic avian influenza (H5N1): Pathways of exposure at the animal-human interface, a systematic review. PLoS ONE 2011, 6, e14582. [Google Scholar] [CrossRef] [PubMed]
- Halpin, J. Avian flu from an occupational health perspective. Arch. Environ. Occup. Health 2005, 60, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Bahl, J.; Pham, T.T.; Hill, N.J.; Hussein, I.T.; Ma, E.J.; Easterday, B.C.; Halpin, R.A.; Stockwell, T.B.; Wentworth, D.E.; Kayali, G.; et al. Ecosystem Interactions Underlie the Spread of Avian Influenza A Viruses with Pandemic Potential. PLoS Pathog. 2016, 12, e1005620. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.; Qin, Y.; Cowling, B.J.; Ren, X.; Wardrop, N.A.; Gilbert, M.; Tsang, T.K.; Wu, P.; Feng, L.; Jiang, H.; et al. Global epidemiology of avian influenza A H5N1 virus infection in humans, 1997–2015: A systematic review of individual case data. Lancet Infect. Dis. 2016, 16, e108–e118. [Google Scholar] [CrossRef]
- Freidl, G.S.; Meijer, A.; de Bruin, E.; de Nardi, M.; Munoz, O.; Capua, I.; Breed, A.C.; Harris, K.; Hill, A.; Kosmider, R.; et al. FLURISK Consortium. Influenza at the animal-human interface: A review of the literature for virological evidence of human infection with swine or avian influenza viruses other than A(H5N1). Eurosurveillance 2014, 19, 20793. [Google Scholar] [CrossRef]
- Sikkema, R.S.; Freidl, G.S.; de Bruin, E.; Koopmans, M. Weighing serological evidence of human exposure to animal influenza viruses—A literature review. Eurosurveillance 2016, 21, 30388. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Mattioli, S.; Zanardi, F.; Baldasseroni, A.; Schaafsma, F.; Cooke, R.M.; Mancini, G.; Fierro, M.; Santangelo, C.; Farioli, A.; Fucksia, S.; et al. Search strings for the study of putative occupational determinants of disease. Occup. Environ. Med. 2010, 67, 436–443. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Koopmans, M.; Wilbrink, B.; Conyn, M.; Natrop, G.; van der Nat, H.; Vennema, H.; Meijer, A.; van Steenbergen, J.; Fouchier, R.; Osterhaus, A.; et al. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 2004, 363, 587–593. [Google Scholar] [CrossRef]
- Tran, T.H.; Nguyen, T.L.; Nguyen, T.D.; Luong, T.S.; Pham, P.M.; Nguyen, V.V.; Pham, T.S.; Vo, C.D.; Le, T.Q.; Ngo, T.T.; et al. Avian influenza A (H5N1) in 10 patients in Vietnam. N. Engl. J. Med. 2004, 350, 1179–1188. [Google Scholar] [PubMed]
- Lopez-Martinez, I.; Balish, A.; Barrera-Badillo, G.; Jones, J.; Nuñez-García, T.E.; Jang, Y.; Aparicio-Antonio, R.; Azziz-Baumgartner, E.; Belser, J.A.; Ramirez-Gonzalez, J.E.; et al. Highly pathogenic avian influenza A(H7N3) virus in poultry workers, Mexico, 2012. Emerg. Infect. Dis. 2013, 19, 1531–1534. [Google Scholar] [CrossRef]
- Lv, H.; Han, J.; Zhang, P.; Lu, Y.; Wen, D.; Cai, J.; Liu, S.; Sun, J.; Yu, Z.; Zhang, H.; et al. Mild illness in avian influenza A(H7N9) virus-infected poultry worker, Huzhou, China, April 2013. Emerg. Infect. Dis. 2013, 19, 1885–1888. [Google Scholar] [CrossRef]
- Puzelli, S.; Rossini, G.; Facchini, M.; Vaccari, G.; Di Trani, L.; Di Martino, A.; Gaibani, P.; Vocale, C.; Cattoli, G.; Bennett, M.; et al. Human infection with highly pathogenic A(H7N7) avian influenza virus, Italy, 2013. Emerg. Infect. Dis. 2014, 20, 1745–1749. [Google Scholar] [CrossRef]
- Bi, Y.; Liu, J.; Xiong, H.; Zhang, Y.; Liu, D.; Liu, Y.; Gao, G.F.; Wang, B. A new reassortment of influenza A (H7N9) virus causing human infection in Beijing, 2014. Sci. Rep. 2016, 6, 6624. [Google Scholar] [CrossRef]
- Fan, M.; Huang, B.; Wang, A.; Deng, L.; Wu, D.; Lu, X.; Zhao, Q.; Xu, S.; Havers, F.; Wang, Y.; et al. Human influenza A(H7N9) virus infection associated with poultry farm, Northeastern China. Emerg. Infect. Dis. 2014, 11, 1902–1905. [Google Scholar] [CrossRef] [PubMed]
- Gharieb, R.; Mohamed, M.; Khalil, A.; Ali, A. Influenza A viruses in birds and humans: Prevalence, molecular characterization, zoonotic significance and risk factors’ assessment in poultry farms. Comp. Immunol. Microbiol. Infect. Dis. 2019, 63, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Yaqub, T.; Mukhtar, N.; Imran, M.; Ghafoor, A.; Shahid, M.F.; Naeem, M.; Iqbal, M.; Smith, G.J.D.; Su, Y.C.F. Avian Influenza A(H9N2) virus in poultry worker, Pakistan, 2015. Emerg. Infect. Dis. 2019, 25, 136–139. [Google Scholar] [CrossRef]
- Kouam, M.K.; Tchouankui, H.N.; Ngapagna, A.N. Epidemiological Features of Highly Pathogenic Avian Influenza in Cameroon. Vet. Med. Int. 2019, 2019, 3796369. [Google Scholar] [CrossRef]
- Ryu, S.; Lim, J.S.; Cowling, B.J.; Chun, B.C. Low risk of avian influenza A (H5N6) transmission to depopulation workers in Korea. Influenza Other Respir. Viruses 2018, 12, 412–415. [Google Scholar] [CrossRef]
- Bridges, C.B.; Lim, W.; Hu-Primmer, J.; Sims, L.; Fukuda, K.; Mak, K.H.; Rowe, T.; Thompson, W.W.; Conn, L.; Lu, X.; et al. Risk of influenza A (H5N1) infection among poultry workers, Hong Kong, 1997–1998. J. Infect. Dis. 2002, 185, 1005–1010. [Google Scholar] [CrossRef] [PubMed]
- Yen, H.; Cheng, M.C.; Liu, J.; Kao, C.; Shih, S.; Cox, N.; Webster, R.G.; King, C. Influenza surveillance in poultry market and its inter-species transmission in Taiwan. Int. Congr. Ser. 2001, 1219, 201–211. [Google Scholar] [CrossRef]
- Puzelli, S.; Di Trani, L.; Fabiani, C.; Campitelli, L.; De Marco, M.A.; Capua, I.; Aguilera, J.F.; Zambon, M.; Donatelli, I. Serological analysis of serum samples from humans exposed to avian H7 influenza viruses in Italy between 1999 and 2003. J. Infect. Dis. 2005, 192, 1318–1322. [Google Scholar] [CrossRef]
- Uyeki, T.M.; Nguyen, D.C.; Rowe, T.; Lu, X.; Hu-Primmer, J.; Huynh, L.P.; Hang, N.L.; Katz, J.M. Seroprevalence of antibodies to avian influenza A (H5) and A (H9) viruses among market poultry workers, Hanoi, Vietnam, 2001. PLoS ONE 2012, 7, e43948. [Google Scholar] [CrossRef]
- Terebuh, P.; Adija, A.; Edwards, L.; Rowe, T.; Jenkins, S.; Kleene, J.; Fukuda, K.; Katz, J.M.; Bridges, C.B. Human infection with avian influenza A(H7N2) virus-Virginia, 2002. Influenza Other Respir. Viruses 2018, 12, 529–532. [Google Scholar] [CrossRef]
- Leibler, J.H.; Silbergeld, E.K.; Pekosz, A.; Gray, G.C. No evidence of infection with avian influenza viruses among US poultry workers in the Delmarva Peninsula, Maryland and Virginia, USA. J. Agromed. 2011, 16, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.; Lee, J.Y.; Choi, W.; Choi, J.H.; Chung, Y.S.; Lee, N.J.; Cheong, H.M.; Katz, J.M.; Oh, H.B.; Cho, H.; et al. Avian influenza a (H5N1) virus antibodies in poultry cullers, South Korea, 2003–2004. Emerg. Infect. Dis. 2012, 18, 986–988. [Google Scholar] [CrossRef]
- Skowronski, D.M.; Li, Y.; Tweed, S.A.; Tam, T.W.; Petric, M.; David, S.T.; Marra, F.; Bastien, N.; Lee, S.W.; Krajden, M.; et al. Protective measures and human antibody response during an avian influenza H7N3 outbreak in poultry in British Columbia, Canada. Can. Med Assoc. J. 2007, 176, 47–53. [Google Scholar] [CrossRef]
- Gill, J.S.; Webby, R.; Gilchrist, M.J.; Gray, G.C. Avian influenza among waterfowl hunters and wildlife professionals. Emerg. Infect. Dis. 2006, 12, 1284–1286. [Google Scholar] [CrossRef]
- Myers, K.P.; Setterquist, S.F.; Capuano, A.W.; Gray, G.C. Infection due to 3 avian influenza subtypes in United States veterinarians. Clin. Infect. Dis. 2007, 45, 4–9. [Google Scholar] [CrossRef]
- Lu, C.Y.; Lu, J.H.; Chen, W.Q.; Jiang, L.F.; Tan, B.Y.; Ling, W.H.; Zheng, B.J.; Sui, H.Y. Potential infections of H5N1 and H9N2 avian influenza do exist in Guangdong populations of China. Chin. Med. J. 2008, 121, 2050–2053. [Google Scholar] [CrossRef] [PubMed]
- Hinjoy, S.; Puthavathana, P.; Laosiritaworn, Y.; Limpakarnjanarat, K.; Pooruk, P.; Chuxnum, T.; Simmerman, J.M.; Ungchusak, K. Low frequency of infection with avian influenza virus (H5N1) among poultry farmers, Thailand, 2004. Emerg. Infect. Dis. 2008, 14, 499–501. [Google Scholar] [CrossRef]
- Schultsz, C.; Nguyen, V.D.; Hai, L.T.; Do, Q.H.; Peiris, J.S.; Lim, W.; Garcia, J.M.; Nguyen, D.T.; Nguyen, T.H.; Huynh, H.T.; et al. Prevalence of antibodies against avian influenza A (H5N1) virus among Cullers and poultry workers in Ho Chi Minh City, 2005. PLoS ONE 2009, 4, e7948. [Google Scholar] [CrossRef] [PubMed]
- Ogata, T.; Yamazaki, Y.; Okabe, N.; Nakamura, Y.; Tashiro, M.; Nagata, N.; Itamura, S.; Yasui, Y.; Nakashima, K.; Doi, M.; et al. Human H5N2 avian influenza infection in Japan and the factors associated with high H5N2-neutralizing antibody titer. J. Epidemiol. 2008, 18, 160–166. [Google Scholar] [CrossRef]
- Dejpichai, R.; Laosiritaworn, Y.; Phuthavathana, P.; Uyeki, T.M.; O’Reilly, M.; Yampikulsakul, N.; Phurahong, S.; Poorak, P.; Prasertsopon, J.; Kularb, R.; et al. Seroprevalence of antibodies to avian influenza virus A (H5N1) among residents of villages with human cases, Thailand, 2005. Emerg. Infect. Dis. 2009, 15, 756–760. [Google Scholar] [CrossRef] [PubMed]
- Apisarnthanarak, A.; Puthavathana, P.; Mundy, L.M. Detection by microneutralization of antibodies against avian influenza virus in an endemic avian influenza region. Clin. Microbiol. Infect. 2010, 16, 1354–1357. [Google Scholar] [CrossRef]
- Ortiz, E.J.; Kochel, T.J.; Capuano, A.W.; Setterquist, S.F.; Gray, G.C. Avian influenza and poultry workers, Perù, 2006. Influenza Other Respir. Viruses 2007, 1, 65–69. [Google Scholar] [CrossRef]
- Ortiz, J.R.; Katz, M.A.; Mahmoud, M.N.; Ahmed, S.; Bawa, S.I.; Farnon, E.C.; Sarki, M.B.; Nasidi, A.; Ado, M.S.; Yahaya, A.H.; et al. Lack of evidence of avian-to-human transmission of avian influenza A (H5N1) virus among poultry workers, Kano, Nigeria, 2006. J. Infect. Dis. 2007, 196, 1685–1691. [Google Scholar] [CrossRef]
- Ceyhan, M.; Yildirim, I.; Ferraris, O.; Bouscambert-Duchamp, M.; Frobert, E.; Uyar, N.; Tezer, H.; Oner, A.F.; Buzgan, T.; Torunoglu, M.A.; et al. Serosurveillance study on transmission of H5N1 virus during a 2006 avian influenza epidemic. Epidemiol. Infect. 2010, 138, 1274–1280. [Google Scholar] [CrossRef]
- Cai, W.; Schweiger, B.; Buchholz, U.; Buda, S.; Littmann, M.; Heusler, J.; Haas, W. Protective measures and H5N1-seroprevalence among personnel tasked with bird collection during an outbreak of avian influenza A/H5N1 in wild birds, Ruegen, Germany, 2006. BMC Infect. Dis. 2009, 9, 170. [Google Scholar] [CrossRef]
- Yamazaki, Y.; Doy, M.; Okabe, N.; Yasui, Y.; Nakashima, K.; Fujieda, T.; Yamato, S.; Kawata, Y.; Ogata, T. Serological survey of avian H5N2-subtype influenza virus infections in human populations. Arch. Virol. 2009, 154, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Morgan, O.; Kuhne, M.; Nair, P.; Verlander, N.Q.; Preece, R.; McDougal, M.; Zambon, M.; Reacher, M. Personal protective equipment and risk for avian influenza (H7N3). Emerg. Infect. Dis. 2009, 15, 59–62. [Google Scholar] [CrossRef]
- Jia, N.; de Vlas, S.J.; Liu, Y.X.; Zhang, J.S.; Zhan, L.; Dang, R.L.; Ma, Y.H.; Wang, X.J.; Liu, T.; Yang, G.P.; et al. Serological reports of human infections of H7 and H9 avian influenza viruses in Northern China. J. Clin. Virol. 2009, 44, 225–229. [Google Scholar] [CrossRef]
- Reed, C.; Bruden, D.; Byrd, K.K.; Veguilla, V.; Bruce, M.; Hurlburt, D.; Wang, D.; Holiday, C.; Hancock, K.; Ortiz, J.R.; et al. Characterizing wild bird contact and seropositivity to highly pathogenic avian influenza A (H5N1) virus in Alaskan residents. Influenza Other Respir. Viruses 2014, 8, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Kayali, G.; Ortiz, E.J.; Chorazy, M.L.; Gray, G.C. Evidence of previous avian influenza infection among US turkey workers. Zoonoses Public Health 2010, 57, 265–272. [Google Scholar] [CrossRef]
- Robert, M.; van Beest Holle, D.R.; Setiawaty, V.; Pangesti, K.N.; Sedyaningsih, E.R. Seroprevalence of avian influenza A/H5N1 among poultry farmers in rural Indonesia, 2007. Southeast Asian J. Trop. Med. Public Health 2010, 41, 1095–1103. [Google Scholar] [PubMed]
- Shafir, S.C.; Fuller, T.; Smith, T.B.; Rimoin, A.W. A national study of individuals who handle migratory birds for evidence of avian and swine-origin influenza virus infections. J. Clin. Virol. 2012, 54, 364–367. [Google Scholar] [CrossRef]
- Okoye, J.; Eze, D.; Krueger, W.S.; Heil, G.L.; Friary, J.A.; Gray, G.C. Serologic evidence of avian influenza virus infections among Nigerian agricultural workers. J. Med. Virol. 2013, 85, 670–676. [Google Scholar] [CrossRef]
- Wang, Q.; Ju, L.; Liu, P.; Zhou, J.; Lv, X.; Li, L.; Shen, H.; Su, H.; Jiang, L.; Jiang, Q. Serological and virological surveillance of avian influenza A virus H9N2 subtype in humans and poultry in Shanghai, China, between 2008 and 2010. Zoonoses Public Health 2015, 62, 131–140. [Google Scholar] [CrossRef]
- Cao, N.; Zhu, W.; Chen, Y.; Tan, L.; Zhou, P.; Cao, Z.; Ke, C.; Li, Y.; Wu, J.; Qi, W.; et al. Avian influenza A (H5N1) virus antibodies in pigs and residents of swine farms, southern China. J. Clin. Virol. 2013, 58, 647–651. [Google Scholar] [CrossRef]
- Di Trani, L.; Porru, S.; Bonfanti, L.; Cordioli, P.; Cesana, B.M.; Boni, A.; Di Carlo, A.S.; Arici, C.; Donatelli, I.; Tomao, P.; et al. Serosurvey against H5 and H7 avian influenza viruses in Italian poultry workers. Avian Dis. 2012, 56, 1068–1071. [Google Scholar] [CrossRef] [PubMed]
- Nasreen, S.; Uddin Khan, S.; Azziz-Baumgartner, E.; Hancock, K.; Veguilla, V.; Wang, D.; Rahman, M.; Alamgir, A.S.; Sturm-Ramirez, K.; Gurley, E.S.; et al. Seroprevalence of antibodies against highly pathogenic avian influenza A (H5N1) virus among poultry workers in Bangladesh, 2009. PLoS ONE 2013, 8, e73200. [Google Scholar] [CrossRef]
- Khurelbaatar, N.; Krueger, W.S.; Heil, G.L.; Darmaa, B.; Ulziimaa, D.; Tserennorov, D.; Baterdene, A.; Anderson, B.D.; Gray, G.C. Sparse evidence for equine or avian influenza virus infections among Mongolian adults with animal exposures. Influenza Other Respir. Viruses 2013, 7, 1246–1250. [Google Scholar] [CrossRef] [PubMed]
- Hadipour, M. Seroprevalence of H9N2 Avian Influenza Virus in Human Population in Boushehr Province, Iran. Asian J. Anim. Vet. Adv. 2011, 6, 196–200. [Google Scholar] [CrossRef]
- Nasreen, S.; Khan, S.U.; Luby, S.P.; Gurley, E.S.; Abedin, J.; Zaman, R.U.; Sohel, B.M.; Rahman, M.; Hancock, K.; Levine, M.Z.; et al. Highly pathogenic Avian Influenza A(H5N1) virus infection among workers at live bird markets, Bangladesh, 2009–2010. Emerg. Infect. Dis. 2015, 21, 629–637. [Google Scholar] [CrossRef]
- Coman, A.; Maftei, D.N.; Krueger, W.S.; Heil, G.L.; Friary, J.A.; Chereches, R.M.; Sirlincan, E.; Bria, P.; Dragnea, C.; Kasler, I.; et al. Serological evidence for avian H9N2 influenza virus infections among Romanian agriculture workers. J. Infect. Public Health 2013, 6, 438–447. [Google Scholar] [CrossRef]
- Yu, Q.; Liu, L.; Pu, J.; Zhao, J.; Sun, Y.; Shen, G.; Wei, H.; Zhu, J.; Zheng, R.; Xiong, D.; et al. Risk perceptions for avian influenza virus infection among poultry workers, China. Emerg. Infect. Dis. 2013, 19, 313–316. [Google Scholar] [CrossRef]
- Li, X.; Tian, B.; Zhou, J.; Chen, Y.; Li, X.; Zhu, W.; Li, Y.; Tang, J.; Guo, J.; Chen, T.; et al. A comprehensive retrospective study of the seroprevalence of H9N2 avian influenza viruses in occupationally exposed populations in China. PLoS ONE 2017, 12, e0178328. [Google Scholar] [CrossRef]
- Zhou, P.; Zhu, W.; Gu, H.; Fu, X.; Wang, L.; Zheng, Y.; He, S.; Ke, C.; Wang, H.; Yuan, Z.; et al. Avian influenza H9N2 seroprevalence among swine farm residents in China. J. Med. Virol. 2014, 86, 597–600. [Google Scholar] [CrossRef]
- Gomaa, M.R.; Kandeil, A.; Kayed, A.S.; Elabd, M.A.; Zaki, S.A.; Abuzeid, D.; El Rifay, A.S.; Mousa, A.A.; Farag, M.M.; McKenzie, P.P.; et al. Serological evidence of human infection with avian influenza A H7 virus in Egyptian poultry growers. PLoS ONE 2016, 11, e0155294. [Google Scholar] [CrossRef]
- Huo, X.; Zu, R.; Qi, X.; Qin, Y.; Li, L.; Tang, F.; Hu, Z.; Zhu, F. Seroprevalence of avian influenza A (H5N1) virus among poultry workers in Jiangsu Province, China: An observational study. BMC Infect. Dis. 2012, 12, 93. [Google Scholar] [CrossRef]
- Kayali, G.; Barbour, E.; Dbaibo, G.; Tabet, C.; Saade, M.; Shaib, H.A.; Debeauchamp, J.; Webby, R.J. Evidence of infection with H4 and H11 avian influenza viruses among Lebanese chicken growers. PLoS ONE 2011, 6, e26818. [Google Scholar] [CrossRef]
- Pawar, S.D.; Tandale, B.V.; Raut, C.G.; Parkhi, S.S.; Barde, T.D.; Gurav, Y.K.; Kode, S.S.; Mishra, A.C. Avian influenza H9N2 seroprevalence among poultry workers in Pune, India, 2010. PLoS ONE 2012, 7, e36374. [Google Scholar] [CrossRef] [PubMed]
- Ahad, A.; Thornton, R.N.; Rabbani, M.; Yaqub, T.; Younus, M.; Muhammad, K.; Mahmood, A.; Shabbir, M.Z.; Kashem, M.A.; Islam, M.Z.; et al. Risk factors for H7 and H9 infection in commercial poultry farm workers in provinces within Pakistan. Prev. Vet. Med. 2014, 117, 610–614. [Google Scholar] [CrossRef] [PubMed]
- Li, L.H.; Yu, Z.; Chen, W.S.; Liu, S.L.; Lu, Y.; Zhang, Y.J.; Chen, E.F.; Lin, J.F. Evidence for H5 avian influenza infection in Zhejiang province, China, 2010–2012: A cross-sectional study. J. Thorac. Dis. 2013, 5, 790–796. [Google Scholar]
- Venter, M.; Treurnicht, F.K.; Buys, A.; Tempia, S.; Samudzi, R.; McAnerney, J.; Jacobs, C.A.; Thomas, J.; Blumberg, L. Risk of human infections with highly pathogenic H5N2 and low pathogenic H7N1 avian influenza strains during outbreaks in ostriches in South Africa. J. Infect. Dis. 2017, 216, S512–S519. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Ma, C.; Shi, W.; Cui, S.; Lu, G.; Peng, X.; Zhang, D.; Liu, Y.; Liang, H.; Zhang, Y.; et al. A serological survey of antibodies to H5, H7 and H9 avian influenza viruses amongst the duck-related workers in Beijing, China. PLoS ONE 2012, 7, e50770. [Google Scholar] [CrossRef]
- Ahad, A.; Rabbani, M.; Yaqub, T.; Younus, M.; Mahmood, A.; Shabbir, M.Z.; Fatima, Z.; Khalid, R.K.; Rasheed, M. Serosurveillance to H9 and H7 avian influenza virus among poultry workers in Punjab Province, Pakistan. Pak. Vet. J. 2013, 33, 107–112. [Google Scholar]
- Dung, T.C.; Dinh, P.N.; Nam, V.S.; Tan, L.M.; Hang, N.L.K.; Thanh, L.T.; Mai, L.Q. Seroprevalence survey of avian influenza A(H5N1) among live poultry market workers in northern Viet Nam, 2011. West. Pac. Surveill. Response J. 2014, 5, 21–26. [Google Scholar]
- Su, S.; Ning, Z.; Zhu, W.; Jiao, P.; Ke, C.; Qi, W.; Huang, Z.; Tian, J.; Cao, L.; Tan, L.; et al. Lack of evidence of avian-to-human transmission of avian influenza A (H5N1) virus among veterinarians, Guangdong, China, 2012. J. Clin. Virol. 2013, 56, 365–366. [Google Scholar] [CrossRef]
- Li, S.; Zhou, Y.; Song, W.; Pang, Q.; Miao, Z. Avian influenza virus H9N2 seroprevalence and risk factors for infection in occupational poultry-exposed workers in Tai’an of China. J. Med. Virol. 2016, 88, 1453–1456. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Wang, A.R.; Liu, Z.H.; Liang, W.; Li, X.X.; Tang, Y.J.; Miao, Z.M.; Chai, T.J. Seroprevalence of avian influenza H9N2 among poultry workers in Shandong Province, China. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 1347–1351. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.Y.; Yang, J.R.; Lin, Y.J.; Yang, C.H.; Cheng, M.C.; Liu, M.T.; Wu, H.S.; Chang, F.Y. Serological comparison of antibodies to avian influenza viruses, subtypes H5N2, H6N1, H7N3 and H7N9 between poultry workers and non-poultry workers in Taiwan in 2012. Epidemiol. Infect. 2015, 143, 2965–2974. [Google Scholar] [CrossRef]
- Heidari, A.; Mancin, M.; Nili, H.; Pourghanbari, G.H.; Lankarani, K.B.; Leardini, S.; Cattoli, G.; Monne, I.; Piccirillo, A. Serological evidence of H9N2 avian influenza virus exposure among poultry workers from Fars province of Iran. Virol. J. 2016, 13, 16. [Google Scholar] [CrossRef] [PubMed]
- de Bruin, E.; Zhang, X.; Ke, C.; Sikkema, R.; Koopmans, M. Serological evidence for exposure to avian influenza viruses within poultry workers in southern China. Zoonoses Public Health 2017, 64, e51–e59. [Google Scholar] [CrossRef]
- Horm, S.V.; Tarantola, A.; Rith, S.; Ly, S.; Gambaretti, J.; Duong, V.; Y, P.; Sorn, S.; Holl, D.; Allal, L.; et al. Intense circulation of A/H5N1 and other avian influenza viruses in Cambodian live-bird markets with serological evidence of sub-clinical human infections. Emerg. Microbes Infect. 2016, 5, e70. [Google Scholar] [CrossRef]
- Sun, L.; Wang, L.; Zhang, W.; Sun, Y.; Luo, Y.; Sun, Y.; Yuan, Z.; Wang, H.; Ning, Z.; Jia, K.; et al. Lack of exposure of H10N8 avian influenza virus among veterinarians in Guangdong Province, China. J. Med. Virol. 2015, 87, 2018–2020. [Google Scholar] [CrossRef]
- Qi, W.; Su, S.; Xiao, C.; Zhou, P.; Li, H.; Ke, C.; Gray, G.C.; Zhang, G.; Liao, M. Antibodies against H10N8 avian influenza virus among animal workers in Guangdong Province before November 30, 2013, when the first human H10N8 case was recognized. BMC Med. 2014, 12, 205. [Google Scholar] [CrossRef]
- Xiang, N.; Bai, T.; Kang, K.; Yuan, H.; Zhou, S.; Ren, R.; Li, X.; Wu, J.; Deng, L.; Zeng, G.; et al. Sero-epidemiologic study of influenza A(H7N9) infection among exposed populations, China 2013–2014. Influenza Other Respir. Viruses 2017, 11, 170–176. [Google Scholar] [CrossRef]
- Chen, J.; Ma, J.; White, S.K.; Cao, Z.; Zhen, Y.; He, S.; Zhu, W.; Ke, C.; Zhang, Y.; Su, S.; et al. Live poultry market workers are susceptible to both avian and swine influenza viruses, Guangdong Province, China. Vet. Microbiol. 2015, 181, 230–235. [Google Scholar] [CrossRef]
- To, K.K.; Hung, I.F.; Lui, Y.M.; Mok, F.K.; Chan, A.S.; Li, P.T.; Wong, T.L.; Ho, D.T.; Chan, J.F.; Chan, K.H.; et al. Ongoing transmission of avian influenza A viruses in Hong Kong despite very comprehensive poultry control measures: A prospective seroepidemiology study. J. Infect. 2016, 72, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Ma, C.; Cui, S.; Zhang, D.; Shi, W.; Pan, Y.; Sun, Y.; Lu, G.; Peng, X.; Zhao, J.; et al. Avian influenza A(H7N9) and (H5N1) infections among poultry and swine workers and the general population in Beijing, China, 2013–2015. Sci. Rep. 2016, 6, 33877. [Google Scholar] [CrossRef]
- Ma, M.J.; Zhao, T.; Chen, S.H.; Xia, X.; Yang, X.X.; Wang, G.L.; Fang, L.Q.; Ma, G.Y.; Wu, M.N.; Qian, Y.H.; et al. Avian influenza A virus infection among workers at live poultry markets, China, 2013–2016. Emerg. Infect. Dis. 2018, 24, 1246–1256. [Google Scholar] [CrossRef]
- Ma, C.; Cui, S.; Sun, Y.; Zhao, J.; Zhang, D.; Zhang, L.; Zhang, Y.; Pan, Y.; Wu, S.; Duan, W.; et al. Avian influenza A (H9N2) virus infections among poultry workers, swine workers, and the general population in Beijing, China, 2013–2016: A serological cohort study. Influenza Other Respir. Viruses 2019, 13, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.Y.; Lau, E.H.; Yuan, J.; Lu, M.L.; Xie, C.J.; Li, K.B.; Ma, X.W.; Chen, J.D.; Liu, Y.H.; Cao, L.; et al. Transmission risk of avian influenza virus along poultry supply chains in Guangdong, China. J. Infect. 2019, 79, 43–48. [Google Scholar] [CrossRef]
- Tahir, M.F.; Abbas, M.A.; Ghafoor, T.; Dil, S.; Shahid, M.A.; Bullo, M.M.H.; Ain, Q.U.; Ranjha, M.A.; Khan, M.A.; Naseem, M.T. Seroprevalence and risk factors of avian influenza H9 virus among poultry professionals in Rawalpindi, Pakistan. J. Infect. Public Health 2019, 12, 482–485. [Google Scholar] [CrossRef]
- Ryu, S.; Kim, C.K.; Kim, K.; Woo, S.H.; Chun, B.C. Serosurveillance of avian influenza A/H5N6 virus infection in poultry farmers, Gyeonggi Province, Republic of Korea, 2016–2017. Int. J. Infect. Dis. 2018, 75, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Gray, G.C.; McCarthy, T.; Capuano, A.W.; Setterquist, S.F.; Alavanja, M.C.; Lynch, C.F. Evidence for avian influenza A infections among Iowa’s agricultural workers. Influenza Other Respir. Viruses 2008, 2, 61–69. [Google Scholar] [CrossRef]
- Wang, M.; Di, B.; Zhou, D.H.; Zheng, B.J.; Jing, H.; Lin, Y.P.; Liu, Y.F.; Wu, X.W.; Qin, P.Z.; Wang, Y.L.; et al. Food markets with live birds as source of avian influenza. Emerg. Infect. Dis. 2006, 12, 1773–1775. [Google Scholar] [CrossRef]
- Okoye, J.O.; Eze, D.C.; Krueger, W.S.; Heil, G.L.; White, S.K.; Merrill, H.R.; Gray, G.C. Evidence for subclinical H5N1 avian influenza infections among Nigerian poultry workers. J. Med. Virol. 2014, 86, 2070–2075. [Google Scholar] [CrossRef]
- Gray, G.C.; Ferguson, D.D.; Lowther, P.E.; Heil, G.L.; Friary, J.A. A national study of US bird banders for evidence of avian influenza virus infections. J. Clin. Virol. 2011, 51, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Khurelbaatar, N.; Krueger, W.S.; Heil, G.L.; Darmaa, B.; Ulziimaa, D.; Tserennorov, D.; Baterdene, A.; Anderson, B.D.; Gray, G.C. Little evidence of avian or equine influenza virus infection among a cohort of Mongolian adults with animal exposures, 2010–2011. PLoS ONE 2014, 9, e85616. [Google Scholar] [CrossRef]
- Arzey, G.G.; Kirkland, P.D.; Arzey, K.E.; Frost, M.; Maywood, P.; Conaty, S.; Hurt, A.C.; Deng, Y.M.; Iannello, P.; Barr, I.; et al. Influenza virus A (H10N7) in chickens and poultry abattoir workers, Australia. Emerg. Infect. Dis. 2012, 18, 814–816. [Google Scholar] [CrossRef]
- Shimizu, K.; Wulandari, L.; Poetranto, E.D.; Setyoningrum, R.A.; Yudhawati, R.; Sholikhah, A.; Nastri, A.M.; Poetranto, A.L.; Candra, A.Y.; Puruhito, E.F.; et al. Seroevidence for a high prevalence of subclinical infection with avian influenza A(H5N1) virus among workers in a live-poultry market in Indonesia. J. Infect. Dis. 2016, 214, 1929–1936. [Google Scholar] [CrossRef]
- Yang, S.; Chen, Y.; Cui, D.; Yao, H.; Lou, J.; Huo, Z.; Xie, G.; Yu, F.; Zheng, S.; Yang, Y.; et al. Avian-origin influenza A(H7N9) infection in influenza A(H7N9)-affected areas of China: A serological study. J. Infect. Dis. 2014, 209, 265–269. [Google Scholar] [CrossRef]
- Li, Q.; Zhou, L.; Zhou, M.; Chen, Z.; Li, F.; Wu, H.; Xiang, N.; Chen, E.; Tang, F.; Wang, D.; et al. Epidemiology of human infections with avian influenza A(H7N9) virus in China. N. Engl. J. Med. 2014, 370, 520–532. [Google Scholar] [CrossRef]
- He, F.; Chen, E.F.; Li, F.D.; Wang, X.Y.; Wang, X.X.; Lin, J.F. Human infection and environmental contamination with Avian Influenza A (H7N9) Virus in Zhejiang Province, China: Risk trend across the three waves of infection. BMC Public Health 2015, 15, 931. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Li, K.; Luo, L.; Lu, E.; Yuan, J.; Liu, H.; Lu, J.; Di, B.; Xiao, X.; Yang, Z. Detection of avian influenza A(H7N9) virus from live poultry markets in Guangzhou, China: A surveillance report. PLoS ONE 2014, 9, e107266. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Fang, S.; Lu, X.; Xu, C.; Cowling, B.J.; Tang, X.; Peng, B.; Wu, W.; He, J.; Tang, Y.; et al. Seroprevalence to avian influenza A(H7N9) virus among poultry workers and the general population in southern China: A longitudinal study. Clin. Infect. Dis. 2014, 59, e76–e83. [Google Scholar] [CrossRef]
- Ding, H.; Chen, Y.; Yu, Z.; Horby, P.W.; Wang, F.; Hu, J.; Yang, X.; Mao, H.; Qin, S.; Chai, C.; et al. A family cluster of three confirmed cases infected with avian influenza A (H7N9) virus in Zhejiang Province of China. BMC Infect. Dis. 2014, 14, 698. [Google Scholar] [CrossRef]
- Wu, D.; Zou, S.; Bai, T.; Li, J.; Zhao, X.; Yang, L.; Liu, H.; Li, X.; Yang, X.; Xin, L.; et al. Poultry farms as a source of avian influenza A (H7N9) virus reassortment and human infection. Sci. Rep. 2015, 5, 7630. [Google Scholar] [CrossRef] [PubMed]
- Svyatchenko, S.V.; Durymanov, A.G.; Susloparov, I.M.; Kolosova, N.P.; Goncharova, N.I.; Mikheev, V.N.; Ryzhikov, A.B.; Ilyicheva, T.N. Severe and fatal influenza cases in Russia in 2014–2015. Online J. Biol. Sci. 2016, 16, 184–192. [Google Scholar] [CrossRef][Green Version]
- Monamele, C.G.; Y, P.; Karlsson, E.A.; Vernet, M.A.; Wade, A.; Okomo, M.A.; Abah, A.S.A.; Yann, S.; Etoundi, G.A.M.; Mo-hamadou, N.R.; et al. Evidence of exposure and human seroconversion during an outbreak of avian influenza A(H5N1) among poultry in Cameroon. Emerg. Microbes Infect. 2019, 8, 186–196. [Google Scholar] [CrossRef]
- AbuBakar, U.; Amrani, L.; Kamarulzaman, F.A.; Karsani, S.A.; Hassandarvish, P.; Khairat, J.E. Avian influenza virus tropism in humans. Viruses 2023, 15, 833. [Google Scholar] [CrossRef]
- Takala, J.; Descatha, A.; Oppliger, A.; Hamzaoui, H.; Bråkenhielm, C.; Neupane, S. Global estimates on biological risks at work. Saf. Health Work. 2023, 14, 390–397. [Google Scholar] [CrossRef]
- Abdelwhab, E.M.; Mettenleiter, T.C. Zoonotic animal influenza virus and potential mixing vessel hosts. Viruses 2023, 15, 980. [Google Scholar] [CrossRef]
- Catalan Saenz, H.S.; Cruz-Ausejo, L. Preventive, safety and control measures against Avian Influenza A(H5N1) in occupationally exposed groups: A scoping review. One Health 2024, 19, 100766. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.M.; Hoque, M.A.; Debnath, N.C.; Yamage, M.; Klaassen, M. Are poultry or wild birds the main reservoirs for avian influenza in Bangladesh? Ecohealth 2017, 14, 490–500. [Google Scholar] [CrossRef] [PubMed]
- De Marco, M.A.; Delogu, M.; Cotti, C. Special Issue “Ecology of Influenza A Viruses”: Editorial. Microorganisms 2023, 11, 1287. [Google Scholar] [CrossRef]
- He, J.; Kam, Y.W. Insights from avian influenza: A review of its multifaceted nature and future pandemic preparedness. Viruses 2024, 16, 458. [Google Scholar] [CrossRef]
- De Marco, M.A.; Delogu, M.; Facchini, M.; Di Trani, L.; Boni, A.; Cotti, C.; Graziosi, G.; Venturini, D.; Regazzi, D.; Ravaioli, V.; et al. Serologic evidence of occupational exposure to avian influenza viruses at the wildfowl/poultry/human interface. Microorganisms 2021, 9, 2153. [Google Scholar] [CrossRef] [PubMed]
- Swayne, D.E. Occupational and consumer risks from avian influenza viruses. Dev. Biol. 2006, 124, 85–90. [Google Scholar]
- Wang, D.; Zhu, W.; Yang, L.; Shu, Y. The epidemiology, virology, and pathogenicity of human infections with Avian Influenza viruses. Cold Spring Harb. Perspect. Med. 2021, 11, a038620. [Google Scholar] [CrossRef] [PubMed]
- WHO. Cumulative Number of Confirmed Human Cases for Avian Influenza A(H5N1) Reported to WHO, 2003–2024, 22 April 2025. Available online: https://www.who.int/publications/m/item/cumulative-number-of-confirmed-human-cases-for-avian-influenza-a(h5n1)-reported-to-who--2003-2025--22-april-2025 (accessed on 29 May 2025).
- WOAH. Avian Influenza. Chapter 3.3.4. Avian Influenza (Including Infection with High Pathogenicity Avian Influenza Viruses). Available online: https://www.woah.org/fileadmin/Home/eng/Health_standards/tahm/3.03.04_AI.pdf (accessed on 2 January 2025).
- Li, K.S.; Xu, K.M.; Peiris, J.S.; Poon, L.L.; Yu, K.Z.; Yuen, K.Y.; Shortridge, K.F.; Webster, R.G.; Guan, Y. Characterization of H9 subtype influenza viruses from the ducks of southern China: A candidate for the next influenza pandemic in humans? J. Virol. 2003, 77, 6988–6994. [Google Scholar] [CrossRef]
- Van Kerkhove, M.D. Brief literature review for the WHO global influenza research agenda–highly pathogenic avian influenza H5N1 risk in humans. Influenza Other Respir Viruses 2013, 7 (Suppl. S2), 26–33. [Google Scholar] [CrossRef]
- Chen, X.; Wang, W.; Wang, Y.; Lai, S.; Yang, J.; Cowling, B.J.; Horby, P.W.; Uyeki, T.M.; Yu, H. Serological evidence of human infections with highly pathogenic avian influenza A(H5N1) virus: A systematic review and meta-analysis. BMC Med. 2020, 18, 377. [Google Scholar] [CrossRef]
- Qi, Y.; Guo, W.; Liu, C.; Li, W.; Gu, Y.; Li, S.; Chen, X. Seroprevalence of influenza A (H9N2) virus infection among humans in China: A meta-analysis. Microb. Pathog. 2021, 155, 104881. [Google Scholar] [CrossRef]
- Webster, R.G. Wet markets—A continuing source of severe acute respiratory syndrome and influenza? Lancet 2004, 363, 234–236. [Google Scholar] [CrossRef]
- Fournié, G.; Høg, E.; Barnett, T.; Pfeiffer, D.U.; Mangtani, P. A Systematic Review and Meta-Analysis of Practices Exposing Humans to Avian Influenza Viruses, Their Prevalence, and Rationale. Am. J. Trop. Med. Hyg. 2017, 97, 376–388. [Google Scholar] [CrossRef]
- Shriner, S.A.; Root, J.J. A Review of Avian Influenza A Virus Associations in Synanthropic Birds. Viruses 2020, 12, 1209. [Google Scholar] [CrossRef]
- Shen, J.; Zhang, H.; Sun, X.; Zhang, Y.; Wang, M.; Guan, M.; Liu, L.; Li, W.; Xu, H.; Xie, Y.; et al. Evolution and biological characteristics of H11 avian influenza viruses isolated from migratory birds and pigeons. Emerg. Microbes Infect. 2024, 13, 2398641. [Google Scholar] [CrossRef] [PubMed]
- Global Influenza Programme (GIP). Practical Interim Guidance to Reduce the Risk of Infection in People Exposed to Avian Influenza Viruses; World Health Organization: Geneva, Switzerland, 2024; pp. 1–5. [Google Scholar]
- Islam, A.; Rahman, M.Z.; Hassan, M.M.; Epstein, J.H.; Klaassen, M. Farm biosecurity practices affecting avian influenza virus circulation in commercial chicken farms in Bangladesh. One Health 2024, 18, 100681. [Google Scholar] [CrossRef]
- Kang, M.; Li, H.P.; Tang, J.; Wang, X.Y.; Wang, L.F.; Baele, G.; Lou, J.T.; Lemey, P.; Su, S. Changing epidemiological patterns in human avian influenza virus infections. Lancet Microbe 2024, 5, 100918. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Lei, Z. The Alarming Situation of Highly Pathogenic Avian Influenza Viruses in 2019–2023. Glob. Med. Genet. 2024, 11, 200–213. [Google Scholar]
- Webby, R.J.; Uyeki, T.M. An Update on Highly Pathogenic Avian Influenza A(H5N1) Virus, Clade 2.3.4.4b. J. Infect. Dis. 2024, 230, 533–542. [Google Scholar] [CrossRef]
- Aznar, E.; Casas, I.; González Praetorius, A.; Ruano Ramos, M.J.; Pozo, F.; Sierra Moros, M.J.; García Rivera, M.V.; Sánchez Sánchez, A.; García Villacieros, E.; Saravia, G.; et al. Influenza A(H5N1) detection in two asymptomatic poultry farm workers in Spain, September to October 2022: Suspected environmental contamination. Eurosurveillance 2023, 28, 2300107. [Google Scholar] [CrossRef]
- European Food Safety Authority; European Centre for Disease Prevention and Control; European Union Reference Laboratory for Avian Influenza; Alexakis, L.; Buczkowski, H.; Ducatez, M.; Fusaro, A.; Gonzales, J.L.; Kuiken, T.; Ståhl, K.; et al. Avian influenza overview December 2024–March 2025. Efsa J. 2025, 23, e9352. [Google Scholar] [PubMed]
- Neumann, G.; Kawaoka, Y. Highly pathogenic H5N1 avian influenza virus outbreak in cattle: The knowns and unknowns. Nat. Rev. Microbiol. 2024, 22, 525–526. [Google Scholar] [CrossRef]
- Perez-Acle, T.; Ravello, C.; Rosemblatt, M. Are we cultivating the perfect storm for a human avian influenza pandemic? Biol. Res. 2024, 57, 96. [Google Scholar] [CrossRef]
- Koopmans, M.P.G.; Barton Behravesh, C.; Cunningham, A.A.; Adisasmito, W.B.; Almuhairi, S.; Bilivogui, P.; Bukachi, S.A.; Casas, N.; Cediel Becerra, N.; Charron, D.F.; et al. One Health High-Level Expert Panel. The panzootic spread of highly pathogenic avian influenza H5N1 sublineage 2.3.4.4b: A critical appraisal of One Health preparedness and prevention. Lancet Infect Dis. 2024, 24, e774–e781. [Google Scholar] [CrossRef]
- Chaudhry, M.; Webby, R.; Swayne, D.; Rashid, H.B.; DeBeauchamp, J.; Killmaster, L.; Criado, M.F.; Lee, D.H.; Webb, A.; Yousaf, S.; et al. Avian influenza at animal-human interface: One-health challenge in live poultry retail stalls of Chakwal, Pakistan. Influenza Other Respir Viruses 2020, 14, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Germeraad, E.A.; Sanders, P.; Hagenaars, T.J.; Jong, M.C.M.; Beerens, N.; Gonzales, J.L. Virus Shedding of Avian Influenza in Poultry: A Systematic Review and Meta-Analysis. Viruses 2019, 11, 812. [Google Scholar] [CrossRef]
- Wu, T.; Perrings, C.; Shang, C.; Collins, J.P.; Daszak, P.; Kinzig, A.; Minteer, B.A. Protection of wetlands as a strategy for reducing the spread of avian influenza from migratory waterfowl. Ambio 2020, 49, 939–949. [Google Scholar] [CrossRef] [PubMed]
- de la Rocque, S.; Errecaborde, K.M.M.; Belot, G.; Brand, T.; Shadomy, S.; von Dobschuetz, S.; Aguanno, R.; Carron, M.; Caya, F.; Ding, S.; et al. One health systems strengthening in countries: Tripartite tools and approaches at the human-animal-environment interface. BMJ Glob. Health 2023, 8, e011236. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization, Food and Agriculture Organization of the United Nations & World Organization for Animal Health. Taking a Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries. 2019. Available online: https://iris.who.int/handle/10665/325620 (accessed on 24 January 2025).
- Ajuwon, B.I.; Roper, K.; Richardson, A.; Lidbury, B.A. One Health approach: A data-driven priority for mitigating outbreaks of emerging and re-emerging zoonotic infectious diseases. Trop. Med. Infect. Dis. 2021, 7, 4. [Google Scholar] [CrossRef]
- Donatelli, I.; Castrucci, M.R.; De Marco, M.A.; Delogu, M.; Webster, R.G. Human-Animal interface: The case for influenza interspecies transmission. Adv. Exp. Med. Biol. 2017, 972, 17–33. [Google Scholar]
- Sreenivasan, C.C.; Li, F.; Wang, D. Emerging Threats of Highly Pathogenic Avian Influenza A (H5N1) in US Dairy Cattle: Understanding Cross-Species Transmission Dynamics in Mammalian Hosts. Viruses 2024, 16, 1703. [Google Scholar] [CrossRef]
- Musa, E.; Nia, Z.M.; Bragazzi, N.L.; Leung, D.; Lee, N.; Kong, J.D. Avian Influenza: Lessons from Past Outbreaks and an Inventory of Data Sources, Mathematical and AI Models, and Early Warning Systems for Forecasting and Hotspot Detection to Tackle Ongoing Outbreaks. Healthcare 2024, 12, 1959. [Google Scholar] [CrossRef]
| Study Characteristics | Overall | Asia | America | Europe | Africa | References | |
|---|---|---|---|---|---|---|---|
| All, n (%) | 11 (100) | 6 (54.5) | 1 (9.1) | 2 (18.2) | 2 (18.2) | [20,21,22,23,24,25,26,27,28,29,30] | |
| Study design, n (%) ^ | |||||||
| Case report study | 6 (54.5) | 4 (66.7) | 1 (100) | 1 (50.0) | — | [21,22,23,24,25,26] | |
| Cross-sectional study | 2 (18.2) | — | — | 1 (50.0) | 1 (50.0) | [20,29] | |
| Longitudinal study | 3 (27.3) | 2 (33.4) | — | — | 1 (50.0) | [27,28,30] | |
| Workplace macro-categories, n (% ^) | |||||||
| F | 7 (63.6) | 3 (50.0) | 1(100) | 2 (100) | 1 (50.0) | [20,22,24,26,27,28,30] | |
| F+P | 1 (9.1) | 1 (16.7) | — | — | — | [21] | |
| M | 1 (9.1) | 1 (16.7) | — | — | — | [23] | |
| P | 1 (9.1) | 1 (16.7) | — | — | — | [25] | |
| F+M | 1 (9.1) | — | — | — | 1 (50.0) | [29] | |
| One-health approach *, n (%) | |||||||
| Yes | 3 (27.3) | 1 (16.7) | — | — | 2 (100) | [26,27,29] | |
| No | 8 (72.7) | 5 (83.3) | 1 (100) | 2 (100) | — | [20,21,22,23,24,25,28,30] [22] [23] [24] [25] [26] | |
| Study Characteristics | Overall | Asia | America | Europe | Africa | References | |
|---|---|---|---|---|---|---|---|
| All, n (%) | 67 (100) | 49 (73.1) | 9 (13.4) | 5 (7.5) | 4 (6.0) | [31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97] | |
| Study design, n (%) ^ | |||||||
| Cross-sectional study | 7 (10.4) | 4 (8.2) | 3 (33.3) | — | [42,54,55,57,74,75,90] | ||
| Longitudinal study | 11 (16.4) | 7 (14.3) | 2 (22.2) | 1 (20.0) | 1 (25.0) | [32,35,38,46,48,52,86,92,93,94,95] | |
| Seroprevalence study | 49 (73.1) | 37 (75.5) | 4 (44.4) | 4 (80.0) | 3 (75.0) | [31,33,34,36,37,39,40,41,43,44,45,47,49,50,51,53,56,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,76,77,78,79,80,81,82,83,84,85,87,88,89,91,96,97] | |
| Workplace macro-categories, n (%) ^ | |||||||
| F | 26 (38.8) | 18 (36.7) | 4 (44.4) | 3 (60.0) | — | [33,35,36,37,38,41,42,43,44,45,46,47,49,56,60,61,63,66,69,71,72,74,77,82,83,97] | |
| F+M | 10 (14.9) | 8 (16.3) | — | — | 2 (3.0) | [31,32,58,62,70,73,78,85,87,89] | |
| F+SH | 6 (9.0) | 5 (10.2) | 1 (11.1) | — | — | [53,55,64,67,92,94] | |
| M | 6 (9.0) | 6 (12.2) | — | — | — | [34,59,65,79,86,93] | |
| WLH | 4 (6.0) | — | 3 (33.3) | 1 (20.0) | — | [39,50,54,57] | |
| P | 4 (6.0) | 2 (4.0) | 1 (11.1) | 1 (20.0) | — | [40,51,52,80] | |
| F+SH+M | 3 (4.5) | 3 (6.1) | — | — | — | [75,81,95] | |
| F+M+V | 1 (1.5) | 1 (2.0) | — | — | — | [90] | |
| F+V+SH+M | 1 (1.5) | 1 (2.0) | — | — | — | [88] | |
| F+M+L | 1 (1.5) | — | — | — | 1 (1.5) | [48] | |
| F+SH+V | 1 (1.5) | 1 (2.0) | — | — | — | [84] | |
| M+F+SH+WLH | 1 (1.5) | 1 (2.0) | — | — | — | [68] | |
| M+SH | 1 (1.5) | 1 (2.0) | — | — | — | [91] | |
| P+SH+L | 1 (1.5) | 1 (2.0) | — | — | — | [96] | |
| OW | 1 (1.5) | — | — | 1 (20.0) | — | [76] | |
| One-health approach *, n (%) | |||||||
| Yes | 10 (14.9) | 9 (18.4) | — | — | 1 (25.0) | [32,43,48,59,60,65,75,86,93,95] | |
| No | 57 (85.1) | 40 (81.6) | 9 (100) | 5 (100) | 3 (75.0) | [31,33,34,35,36,37,38,39,40,41,42,44,45,46,47,49,50,51,52,53,54,55,56,57,58,61,62,63,64,66,67,68,69,70,71,72,73,74,76,77,78,79,80,81,82,83,84,85,87,88,89,90,91,92,94,95,96,97] | |
| Study Characteristics | Overall | Asia | America | Europe | Africa | Australia | References | |
|---|---|---|---|---|---|---|---|---|
| All, n (%) | 16 (100) | 11 (68.7) | 2 (12.5) | — | 2 (12.5) | 1 (6.3) | [98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113] | |
| Study design, n (%) ^ | — | |||||||
| Case report study | 3 (18.7) | 2 (18.2) | — | — | — | 1 (100) | [99,103,106] | |
| Cross-sectional study | 2 (12.5) | 1 (9.1) | 1 (50.0) | — | — | — | [101,107] | |
| Longitudinal study | 5 (31.2) | 2 (18.2) | 1 (50.0) | — | 2 (100) | — | [98,100,102,110,113] | |
| Seroprevalence study | 6 (37.5) | 6 (54.5) | — | — | — | — | [104,105,108,109,111,112] | |
| Workplace macro-categories, n (%) ^ | — | — | ||||||
| F | 3 (18.7) | 3 (27.3) | — | — | — | — | [102,111,112] | |
| F+M | 3 (18.7) | 1 (9.1) | — | — | 2 (100) | — | [100,108,113] | |
| M | 6 (37.5) | 6 (54.5) | — | — | — | — | [99,104,105,106,109,110] | |
| F+SH | 1 (6.3) | — | — | — | — | 1 (100) | [103] | |
| WLH | 1 (6.3) | — | 1 (50.0) | — | — | — | [101] | |
| F+M+SH+WLH+P | 1 (6.3) | 1 (9.1) | — | — | — | — | [107] | |
| F+SH+WLH | 1 (6.3) | — | 1 (50.0) | — | — | — | [98] | |
| One-health approach *, n (%) | ||||||||
| Yes | 8 (50.0) | 6 (54.5) | — | — | 1 (50.0) | 1 (100) | [99,103,104,107,108,110,111,113] | |
| No | 8 (50.0) | 5 (45,5) | 2 (100) | — | 1 (50,0) | — | [98,100,101,102,105,106,109,112] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Marco, M.A.; Binazzi, A.; Melis, P.; Cotti, C.; Bonafede, M.; Delogu, M.; Tomao, P.; Vonesch, N. Occupational Risk from Avian Influenza Viruses at Different Ecological Interfaces Between 1997 and 2019. Microorganisms 2025, 13, 1391. https://doi.org/10.3390/microorganisms13061391
De Marco MA, Binazzi A, Melis P, Cotti C, Bonafede M, Delogu M, Tomao P, Vonesch N. Occupational Risk from Avian Influenza Viruses at Different Ecological Interfaces Between 1997 and 2019. Microorganisms. 2025; 13(6):1391. https://doi.org/10.3390/microorganisms13061391
Chicago/Turabian StyleDe Marco, Maria Alessandra, Alessandra Binazzi, Paola Melis, Claudia Cotti, Michela Bonafede, Mauro Delogu, Paola Tomao, and Nicoletta Vonesch. 2025. "Occupational Risk from Avian Influenza Viruses at Different Ecological Interfaces Between 1997 and 2019" Microorganisms 13, no. 6: 1391. https://doi.org/10.3390/microorganisms13061391
APA StyleDe Marco, M. A., Binazzi, A., Melis, P., Cotti, C., Bonafede, M., Delogu, M., Tomao, P., & Vonesch, N. (2025). Occupational Risk from Avian Influenza Viruses at Different Ecological Interfaces Between 1997 and 2019. Microorganisms, 13(6), 1391. https://doi.org/10.3390/microorganisms13061391






