Central Nervous System Infections Caused by Bacillus Calmette–Guerin: Case Report and Narrative Literature Review
Abstract
1. Introduction
2. Case Presentation
2.1. Past Medical History and Presentation of Symptoms
2.2. First Hospital Admission
2.3. Second Hospital Admission
2.4. Third Hospital Admission
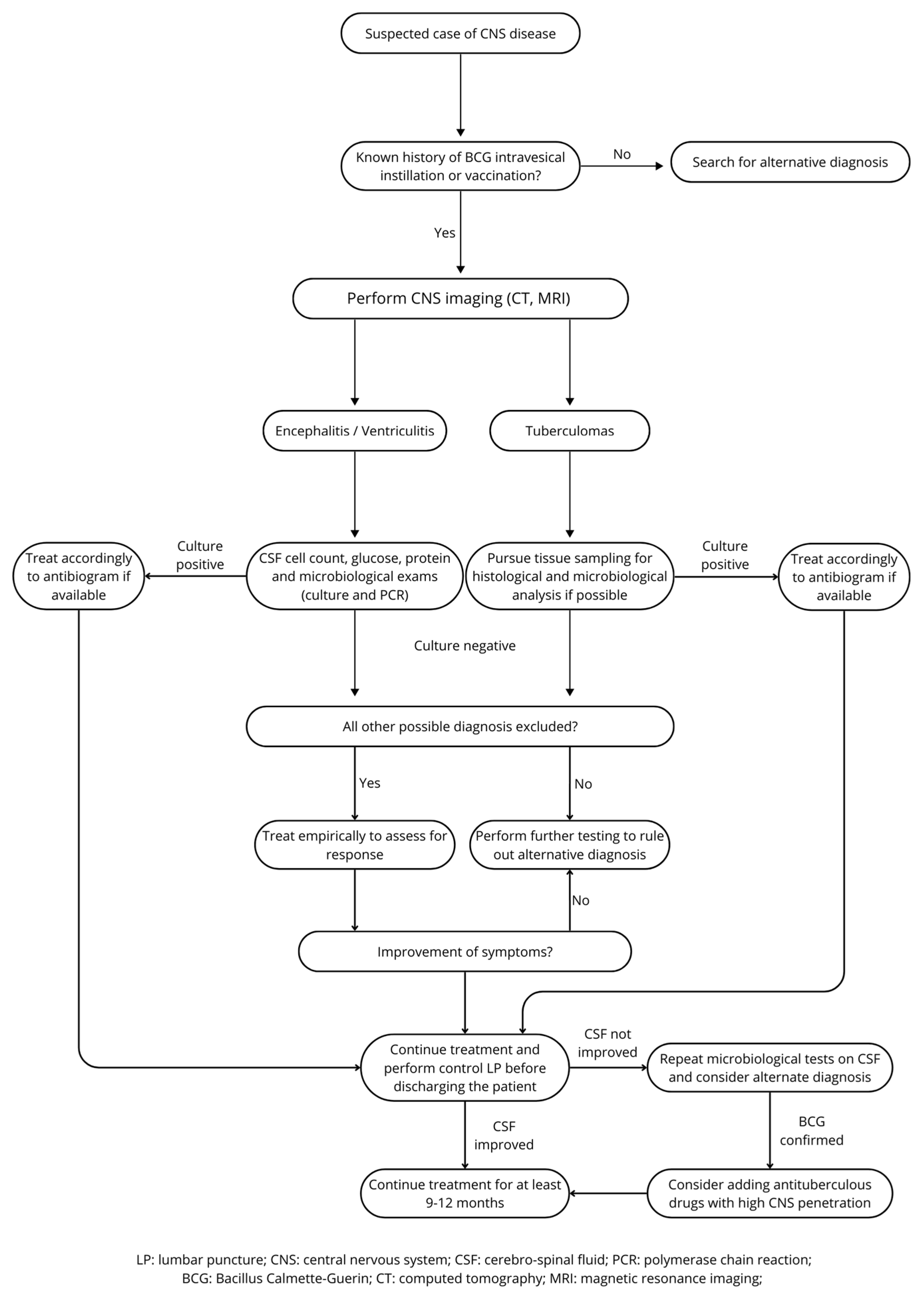
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BCG | Bacillus Calmette–Guerin |
| MRI | Magnetic resonance imaging |
| CSF | Cerebrospinal fluid |
| NMIBC | Non-muscle-invasive bladder cancer |
| CNS | Central nervous system |
| EEG | Electroencephalography |
| LP | Lumbar puncture |
| CT | Computed tomography |
| SIADH | Inappropriate antidiuretic hormone secretion |
| EVD | External ventricular drain |
| AFB | Acid-fast bacilli |
| AIDS | Acquired immunodeficiency syndrome |
| RIF | Rifampicin |
| EMB | Ethambutol |
| MOX | Moxifloxacin |
| INH | Isoniazid |
| PZA | Pyrazinamide |
| ETI | Ethionamide |
| STP | Streptomycin |
| LEV | Levofloxacin |
| ALL | Acute lymphoblastic leukemia |
| SCID | Severe combined immunodeficiency |
| CFZ | Clofazimine |
| CAM | Clarithromycin |
| CIP | Ciprofloxacin |
| N.R. | Not reported |
| AMK | Amikacin |
| N.A. | Not applicable |
| SR | Symptom resolution |
References
- Burger, M.; Catto, J.W.F.; Dalbagni, G.; Grossman, H.B.; Herr, H.; Karakiewicz, P.; Kassouf, W.; Kiemeney, L.A.; La Vecchia, C.; Shariat, S.; et al. Epidemiology and Risk Factors of Urothelial Bladder Cancer. Eur. Urol. 2013, 63, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Dominguez Escrig, J.L.; Gontero, P.; Liedberg, F.; Masson-Lecomte, A.; Mostafid, A.H.; et al. European Association of Urology Guidelines on Non–Muscle-Invasive Bladder Cancer (Ta, T1, and Carcinoma in Situ). Eur. Urol. 2022, 81, 75–94. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.S.; Boorjian, S.A.; Chou, R.; Clark, P.E.; Daneshmand, S.; Konety, B.R.; Pruthi, R.; Quale, D.Z.; Ritch, C.R.; Seigne, J.D.; et al. Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Guideline. J. Urol. 2016, 196, 1021–1069. [Google Scholar] [CrossRef]
- Pérez-Jacoiste Asín, M.A.; Fernández-Ruiz, M.; López-Medrano, F.; Lumbreras, C.; Tejido, Á.; San Juan, R.; Arrebola-Pajares, A.; Lizasoain, M.; Prieto, S.; Aguado, J.M. Bacillus Calmette-Guérin (BCG) Infection Following Intravesical BCG Administration as Adjunctive Therapy for Bladder Cancer: Incidence, Risk Factors, and Outcome in a Single-Institution Series and Review of the Literature. Medicine 2014, 93, 236–254. [Google Scholar] [CrossRef]
- González-Del Vecchio, M.; Ruíz-Serrano, M.J.; Gijón, P.; Sánchez-Somolinos, M.; de Egea, V.; García de Viedma, D.; Sánchez Fresneda, M.N.; Bouza, E. Differences between a Probable and Proven BCG Infection Following Intravesical Instillations: 16 Years Experience in a Tertiary Care Hospital. Diagn. Microbiol. Infect. Dis. 2016, 85, 338–343. [Google Scholar] [CrossRef]
- Larsen, E.S.; Nordholm, A.C.; Lillebaek, T.; Holden, I.K.; Johansen, I.S. The Epidemiology of Bacille Calmette-Guérin Infections after Bladder Instillation from 2002 through 2017: A Nationwide Retrospective Cohort Study. BJU Int. 2019, 124, 910–916. [Google Scholar] [CrossRef] [PubMed]
- Steg, A.; Leleu, C.; Debré, B.; Boccon-Gibod, L.; Sieard, D. Systemic Bacillus Calmette-Guérin Infection, “BCGitis”, in Patients Treated by Intravesical Bacillus Calmette-Guérin Therapy for Bladder Cancer. Eur. Urol. 1989, 16, 161–164. [Google Scholar] [CrossRef]
- Lamm, D.L.; van der Meijden, P.M.; Morales, A.; Brosman, S.A.; Catalona, W.J.; Herr, H.W.; Soloway, M.S.; Steg, A.; Debruyne, F.M. Incidence and Treatment of Complications of Bacillus Calmette-Guerin Intravesical Therapy in Superficial Bladder Cancer. J. Urol. 1992, 147, 596–600. [Google Scholar] [CrossRef]
- Nummi, A.; Järvinen, R.; Sairanen, J.; Huotari, K. A Retrospective Study on Tolerability and Complications of Bacillus Calmette-Guérin (BCG) Instillations for Non-Muscle-Invasive Bladder Cancer. Scand. J. Urol. 2019, 53, 116–122. [Google Scholar] [CrossRef]
- Golub, V.; Malhotra, P.; Patel, S. Mycobacterial Brain Tuberculomas Due to Bacille Calmette-Guérin Intravesical Chemotherapy for Bladder Cancer: A Case Report and Literature Review. Can. J. Infect. Dis. Med. Microbiol. 2011, 22, 104–106. [Google Scholar] [CrossRef]
- Parent, M.-E.; Richer, M.; Liang, P. The First Case of Bacillus Calmette-Guérin-Induced Small-Vessel Central Nervous System Vasculitis. Clin. Rheumatol. 2018, 37, 2297–2302. [Google Scholar] [CrossRef] [PubMed]
- Sheron, M.W.; Holt, S.L.; Ingram, C.W. Mycobacterium Bovis Cerebellar Abscess Following Treatment with Bacillus Calmette-Guérin. J. Pharm. Pract. 2017, 30, 378–380. [Google Scholar] [CrossRef] [PubMed]
- Tariq, M.; Clarke, N.; Chen, M. Mycobacterial Meningitis as an Early Complication of Bacille Calmette-Guerin Intravesical Chemotherapy in the Setting of a Systemic Infection. Neurology 2022, 98 (Suppl. S18), 112. [Google Scholar] [CrossRef]
- Shoskes, A.; Amin, M. Central Nervous System Miliary Mycobacterium Bovis Infection Secondary to Intravesical BCG Instillation. Neurology 2021, 96 (Suppl. S15), 2719. [Google Scholar] [CrossRef]
- Schwartz, S.; Amaya, S.; Kirby, J.; Varma, H. Mycobacterium Bovis Infection of the Brain Following Intravesical BCG Treatment. J. Neuropathol. Exp. Neurol. 2023, 82, 583–584. [Google Scholar]
- Furuichi, M.; Mori, F.; Uejima, Y.; Sato, S.; Kurihara, J.; Kawano, Y.; Suganuma, E. A Case of Mycobacterium Bovis Bacillus Calmette-Guérin (BCG) Strain Meningitis and Ventriculitis Following BCG Vaccination. Int. J. Infect. Dis. 2020, 100, 373–376. [Google Scholar] [CrossRef]
- Sharifi, G.; Mousavinejad, S.A.; Moradian, K.; Ebrahimzadeh, K.; Samadian, M.; Zerehpoosh, F.B.; Rezaei, O. Pineal Region Tuberculoma Caused by Mycobacterium bovis as a Complication of Bacille Calmette-Guérin Vaccine: Case Report and Review of the Literature. World Neurosurg. 2020, 133, 416–418. [Google Scholar] [CrossRef]
- van Deutekom, H.; Smulders, Y.M.; Roozendaal, K.J.; van Soolingen, D. Bacille Calmette-Cuerin (BCG) Meningitis in an AIDS Patient 12 Years After Vaccination with BCG. Clin. Infect. Dis. 1996, 22, 870–871. [Google Scholar] [CrossRef]
- Tardieu, M.; Truffot-Pernot, C.; Carriere, J.P.; Dupic, Y.; Landrieu, P. Tuberculous Meningitis Due to BCG in Two Previously Healthy Children. Lancet 1988, 331, 440–441. [Google Scholar] [CrossRef]
- Eser, I.; Uyan, Z.S.; Kilic, S.C.; Uyur, E.; Arisoy, E.S.; Tezcan, G.; Aydogan, M. Intracranial Calcification after Probable Disseminated Bacillus Calmette–Guérin Infection in a Child with Severe Combined Immunodeficiency. J. Pediatr. Infect. Dis. 2018, 15, 48–52. [Google Scholar] [CrossRef]
- Stone, M.M.; Vannier, A.M.; Storch, S.K.; Peterson, C.; Nitta, A.T.; Zhang, Y. Brief Report: Meningitis Due to Iatrogenic BCG Infection in Two Immunocompromised Children. New Engl. J. Med. 1995, 333, 561–563. [Google Scholar] [CrossRef] [PubMed]
- Misra, U.K.; Kalita, J.; Tuberculous Meningitis International Research Consortium. Mechanism, Spectrum, Consequences and Management of Hyponatremia in Tuberculous Meningitis. Wellcome Open Res. 2019, 4, 189. [Google Scholar] [CrossRef]
- Bernatowska, E.A.; Wolska-Kusnierz, B.; Pac, M.; Kurenko-Deptuch, M.; Zwolska, Z.; Casanova, J.-L.; Piatosa, B.; Van Dongen, J.; Roszkowski, K.; Mikoluc, B.; et al. Disseminated Bacillus Calmette-Guérin Infection and Immunodeficiency. Emerg. Infect. Dis. 2007, 13, 799–801. [Google Scholar] [CrossRef]
- Barcenas-Morales, G.; Cortes-Acevedo, P.; Doffinger, R. Anticytokine Autoantibodies Leading to Infection: Early Recognition, Diagnosis and Treatment Options. Curr. Opin. Infect. Dis. 2019, 32, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Barricarte, R.; Markle, J.G.; Ma, C.S.; Deenick, E.K.; Ramírez-Alejo, N.; Mele, F.; Latorre, D.; Mahdaviani, S.A.; Aytekin, C.; Mansouri, D.; et al. Human IFN-γ Immunity to Mycobacteria Is Governed by Both IL-12 and IL-23. Sci. Immunol. 2018, 3, eaau6759. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Kashyap, A.; Salvator, H.; Rosen, L.B.; Colby, D.; Ardeshir-Larijani, F.; Loehrer, P.J.; Ding, L.; Lugo Reyes, S.O.; Riminton, S.; et al. Anti–Interleukin-23 Autoantibodies in Adult-Onset Immunodeficiency. N. Engl. J. Med. 2024, 390, 1105–1117. [Google Scholar] [CrossRef]
- Bowyer, L.; Hall, R.R.; Reading, J.; Marsh, M.M. The Persistence of Bacille Calmette-Guérin in the Bladder after Intravesical Treatment for Bladder Cancer. Br. J. Urol. 1995, 75, 188–192. [Google Scholar] [CrossRef]
- Solomons, R.S.; Visser, D.H.; Donald, P.R.; Marais, B.J.; Schoeman, J.F.; van Furth, A.M. The Diagnostic Value of Cerebrospinal Fluid Chemistry Results in Childhood Tuberculous Meningitis. Child’s Nerv. Syst. 2015, 31, 1335–1340. [Google Scholar] [CrossRef]
- Durek, C.; Rüsch-Gerdes, S.; Jocham, D.; Böhle, A. Sensitivity of BCG to Modern Antibiotics. Eur. Urol. 2000, 37 (Suppl. S1), 21–25. [Google Scholar] [CrossRef]
- Pommier, J.D.; Ben Lasfar, N.; Van Grunderbeeck, N.; Burdet, C.; Laouénan, C.; Rioux, C.; Pierre-Audigier, C.; Meybeck, A.; Choudat, L.; Benchikh, A.; et al. Complications Following Intravesical Bacillus Calmette-Guerin Treatment for Bladder Cancer: A Case Series of 22 Patients. Infect. Dis. 2015, 47, 725–731. [Google Scholar] [CrossRef]
- Audenet, F.; Sotto, A.; Roumiguié, M.; Allory, Y.; Andrejak, C.; Leon, P.; Loriot, Y.; Masson-Lecomte, A.; Pradère, B.; Seisen, T.; et al. Recommandations Des Comités de Cancérologie (CC-AFU) et d’infectiologie (CI-AFU) de l’Association Française d’urologie Pour La Prise En Charge Effets Indésirables et Complications Du BCG. Prog. Urol. 2022, 32, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Nahid, P.; Mase, S.R.; Migliori, G.B.; Sotgiu, G.; Bothamley, G.H.; Brozek, J.L.; Cattamanchi, A.; Cegielski, J.P.; Chen, L.; Daley, C.L.; et al. Treatment of Drug-Resistant Tuberculosis. An Official ATS/CDC/ERS/IDSA Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2019, 200, e93–e142. [Google Scholar] [CrossRef] [PubMed]
- Roglić, S.; Dickson, D.; Miše, B.; Višković, K.; Katalinić-Janković, V.; Rutherford, G.; Begovac, J. Successful Treatment of Disseminated Bacillus Calmette-Guérin Disease in an HIV-Infected Child with a Linezolid-Containing Regimen. Case Rep. Infect. Dis. 2016, 2016, 1528981. [Google Scholar] [CrossRef]
- Nau, R.; Sörgel, F.; Eiffert, H. Penetration of Drugs through the Blood-Cerebrospinal Fluid/Blood-Brain Barrier for Treatment of Central Nervous System Infections. Clin. Microbiol. Rev. 2010, 23, 858–883. [Google Scholar] [CrossRef]
- Thwaites, G.E.; Bhavnani, S.M.; Chau, T.T.H.; Hammel, J.P.; Török, M.E.; Van Wart, S.A.; Mai, P.P.; Reynolds, D.K.; Caws, M.; Dung, N.T.; et al. Randomized Pharmacokinetic and Pharmacodynamic Comparison of Fluoroquinolones for Tuberculous Meningitis. Antimicrob. Agents Chemother. 2011, 55, 3244–3253. [Google Scholar] [CrossRef] [PubMed]
- Nahid, P.; Dorman, S.E.; Alipanah, N.; Barry, P.M.; Brozek, J.L.; Cattamanchi, A.; Chaisson, L.H.; Chaisson, R.E.; Daley, C.L.; Grzemska, M.; et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Clin. Infect. Dis. 2016, 63, e147–e195. [Google Scholar] [CrossRef]
- WHO Consolidated Guidelines on Tuberculosis: Module 4: Treatment: Drug-Susceptible Tuberculosis Treatment. Available online: https://www.who.int/publications/i/item/9789240048126 (accessed on 21 March 2025).
- Thwaites, G.E.; Nguyen, D.B.; Nguyen, H.D.; Hoang, T.Q.; Do, T.T.O.; Nguyen, T.C.T.; Nguyen, Q.H.; Nguyen, T.T.; Nguyen, N.H.; Nguyen, T.N.L.; et al. Dexamethasone for the Treatment of Tuberculous Meningitis in Adolescents and Adults. N. Engl. J. Med. 2004, 351, 1741–1751. [Google Scholar] [CrossRef]
| N° | Author [Reference] | Age, Yrs/ Sex | Clinical Presentation | Lesion Site | BCG Infection Type | BCG Isolation Site | CSF Alterations | Therapy | Immuno- Deficient | Adjunctive Corticosteroids | Therapy Duration, Months | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BCG origin: Intravesical instillations | ||||||||||||
| 1 | Golub et al. [10] | 73/M | Headaches, dizziness, right hand tremor | Frontal, temporal, and basal ganglia | Tuberculomas | Brain tissue culture | Lymphocytic Pleocytosis and hyperproteinorrachia | RIF + EMB + MOX | No | No | 12 | SR |
| 2 | Parent et al. [11] | 89/M | Right upper limb hyposthenia, dysarthria | Multiple left-sided white matter lesions | Vasculitis, endophthalmitis | Brain tissue, humor vitreo | Pleocytosis | INH + RIF + MOX + EMB | No | Yes | N.R. | SR |
| 3 | Sheron et al. [12] | 74/M | Dizziness, vertigo, gait ataxia | Cerebellum | Abscess | Brain tissue culture | N.R. | INH + RIF + EMB | No | Yes | 12 | SR |
| 4 | Tariq et al. [13] | 80/M | Severe ataxia, dysmetria | Nodular leptomeningeal enhancement involving cranial nerves, brainstem, and superior cerebellum | Meningitis | CSF | Lymphocytic Pleocytosis, hypoglycorrhachia, and hyperproteinorrachia | RIF + EMB + MOX | No | Yes | 12 | Improvement of symptoms; remaining dysmetria |
| 5 | Shoskes et al. [14] | 67/M | Fever, encephalopathy, respiratory failure | Hyperintense lesions in cortex, subcortical white matter, and brainstem | Miliary infection | Biopsy | N.R. | RIF + INH + EMB + AZM | No | Yes | 6 | SR |
| 6 | Schwartz et al. [15] | 88/M | Aphasia | Frontotemporal lesions | Tuberculomas | Tissue biopsy | N.R. | None | No | No | 0 | Death |
| 7 | Pérez-Jacoiste et al. [4] | 73/M | N.R. | Inflammation of meninges | Lymphocytic meningitis | Only urine | N.R. | RIF + INH + LEV | Yes | N.R. | 6 | SR |
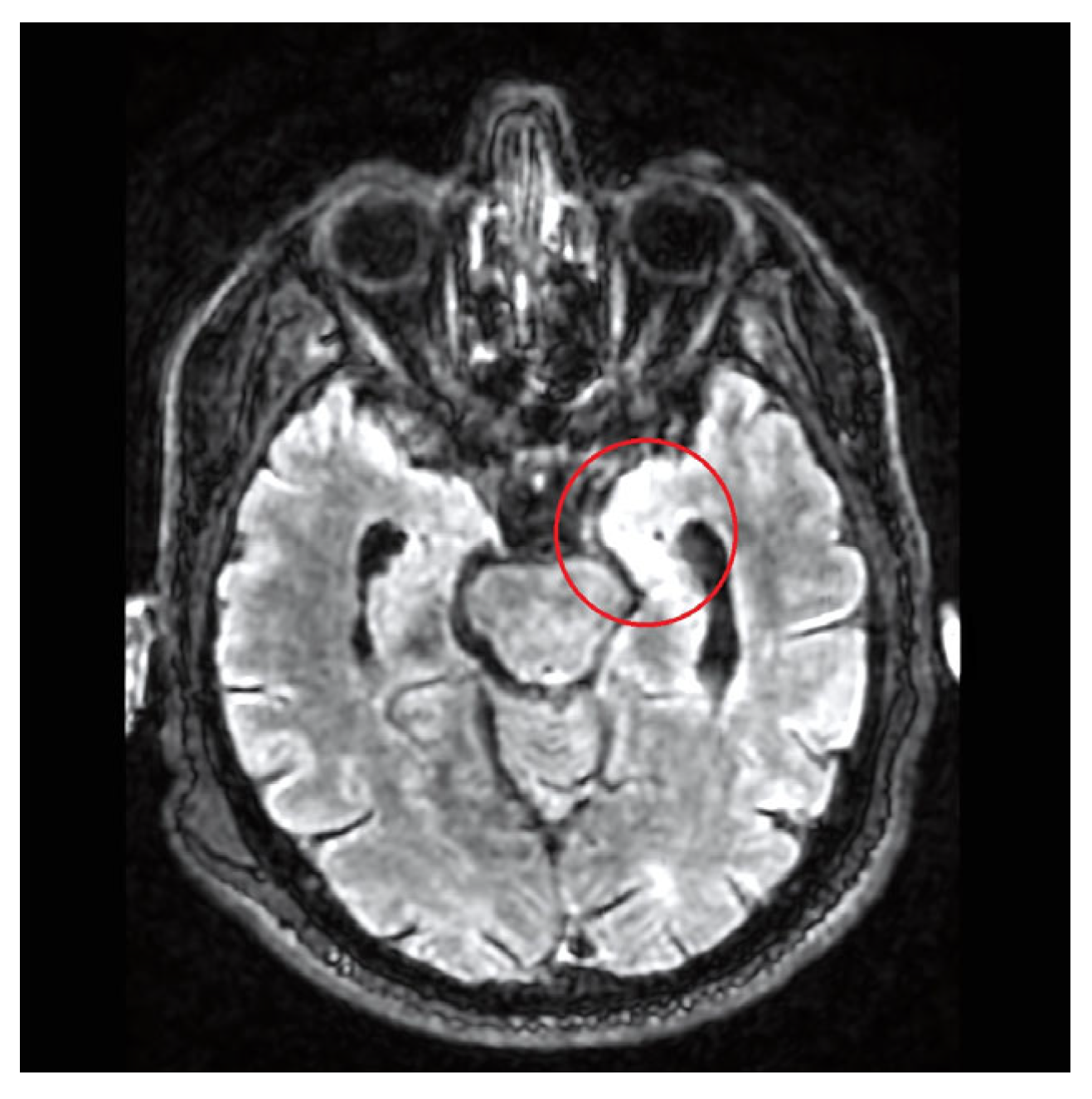
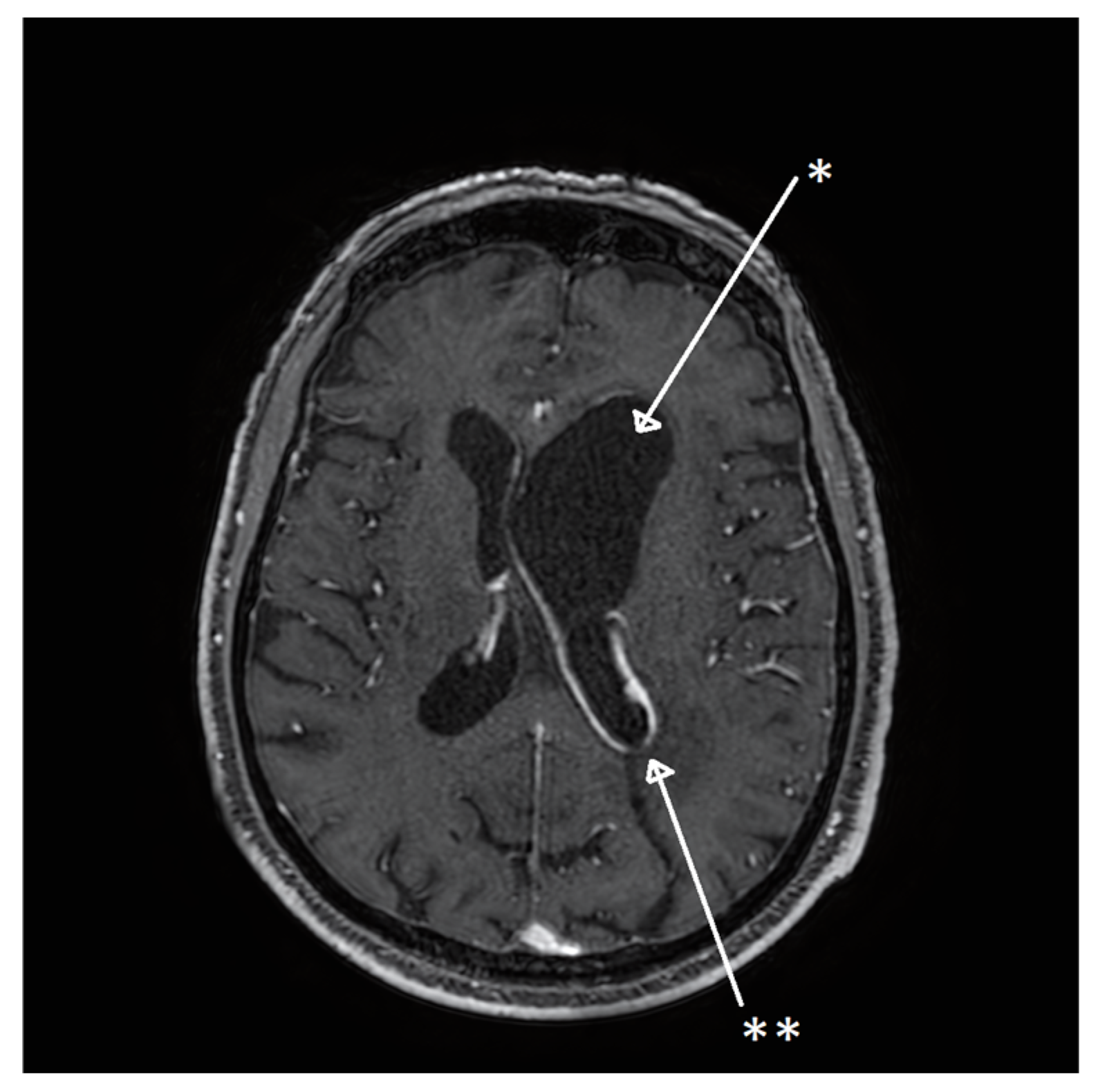
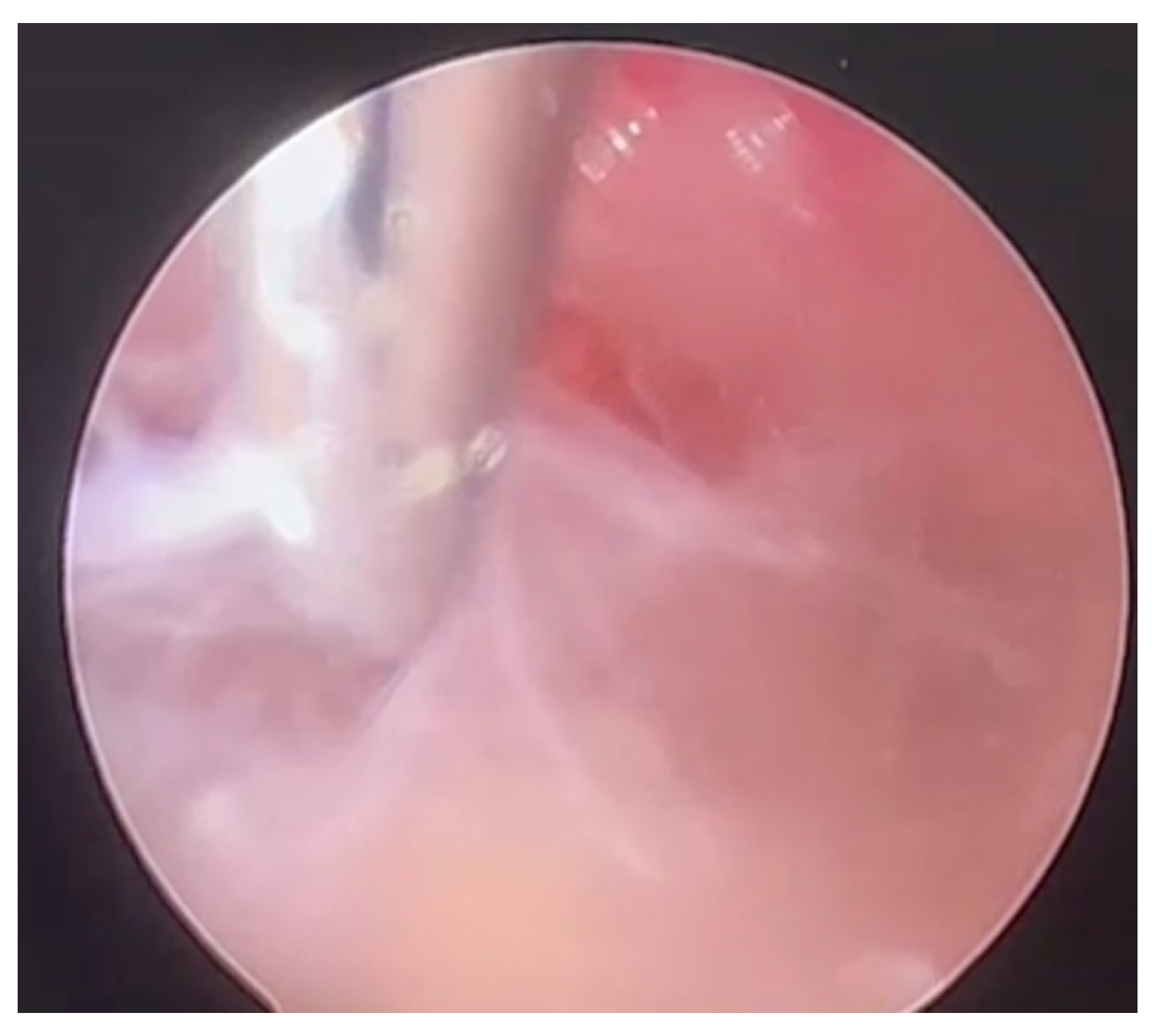
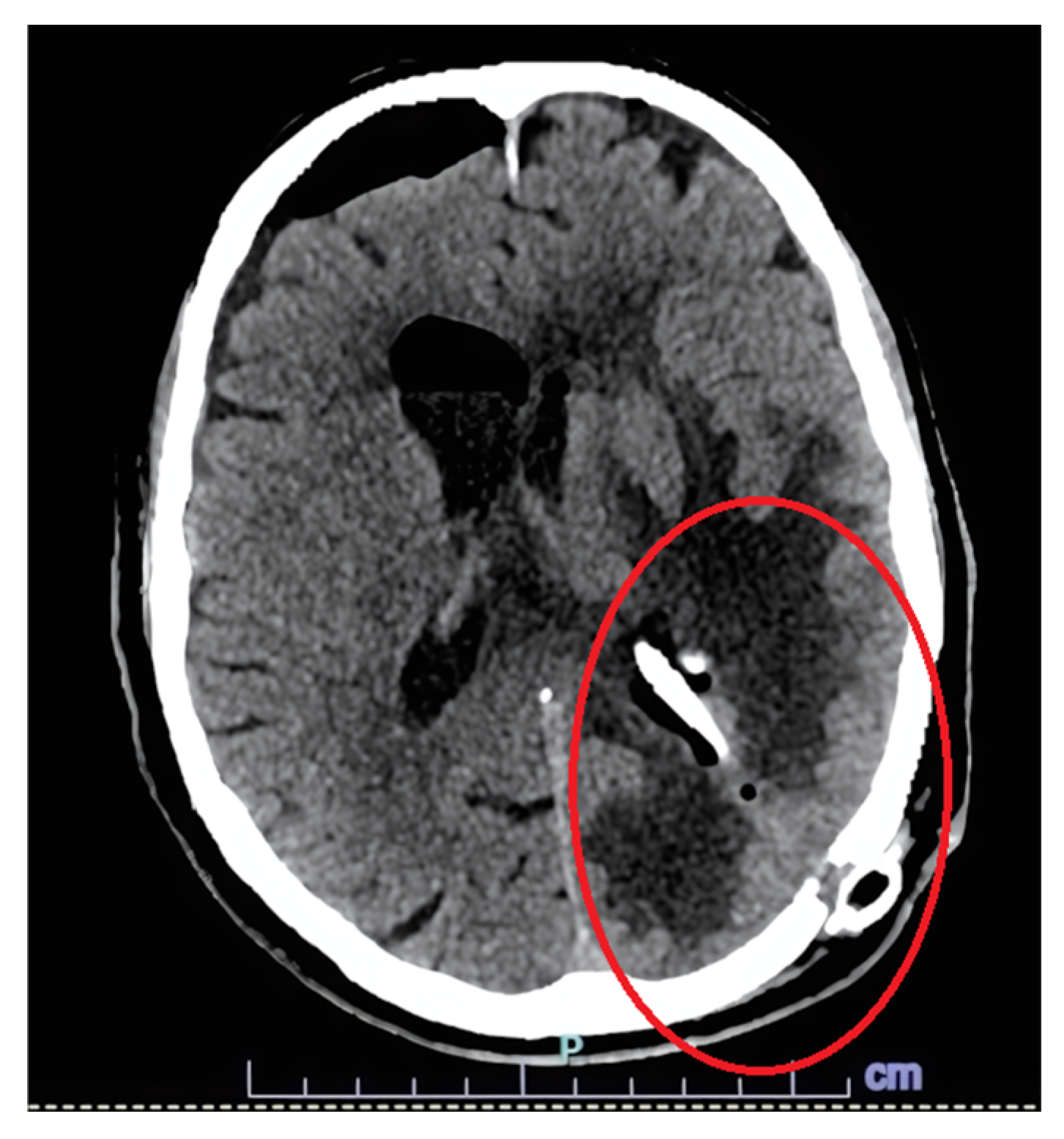
| 8 | Our case | 77/M | Fever, confusion | Right frontal lobe hyperintensity and left lateral ventricle exclusion. | Encephalitis and ventriculitis | CSF | Pleocytosis, hypoglycorrhachia, and hyperproteinorrachia | INH + RIF + EMB + LEV; LIN (2 weeks) | No | Yes | 14 | SR |
| BCG origin: Vaccination | ||||||||||||
| 9 | Furuichi et al. [16] | 1.3/M | gait disturbances | third ventricle | Ventriculitis | CSF and brain tissue | Lymphocytic Pleocytosis, hypoglycorrhachia, and hyperproteinorrachia | INH + RIF + EMB | No | Yes | 24 | Improvement of symptoms; remaining gait disturbances |
| 10 | Sharifi et al. [17] | 0.5/M | Poor feeding, nausea, vomiting | Pineal gland | Tuberculoma | Brain tissue culture | Within range | N.R. | No | N.R. | N.R. | SR |
| 11 | Van Deutekom et al. [18] | 31/M | Fever, neck stiffness, headache | N.A. | Meningitis | CSF | Hyperproteinorrachia and pleocytosis | INH + RIF + PZA | Yes (AIDS) | No | 0.3 | Death |
| 12 | Tardieu et al. [19] | 5/M | Fever, rigor | Hyperintensity of subarachnoid space exclusion of fourth ventricle | Ventriculitis | CSF | Pleocytosis, hypoglycorrhachia, and hyperproteinorrachia | INH + RIF + EMB | No | No | 18 | SR |
| 13 | Tardieu et al. [19] | 4/M | Fever, rigor | N.A. | Meningitis | CSF | Pleocytosis, hypoglycorrhachia, and hyperproteinorrachia | INH + RIF + EMB | No | No | 18 | SR |
| 14 | Eser et al. [20] | 0.25/M | Afebrile seizures | Calcification of the subcortical and periventricular regions | Calcifications, Tuberculomas | Lymph nodes * | Within range | INH + RIF + CAM + CFZ + CIP + AMK (2 mo) | Yes (SCID) | No | 12 | Microcephaly and persistence of axial hypotonia |
| BCG origin: Unknown (LP contamination?) | ||||||||||||
| 15 | Stone et al. [21] | 3/F | Headache | N.A. | Meningitis | CSF | Pleocytosis | INH + RIF + ETI + STP | Yes (ALL in active chemotherapy *) | No | 12 | SR |
| 16 | Stone et al. [21] | 5/M | Headache, fever, weight loss | N.A. | Meningitis | CSF | Pleocytosis, hypoglycorrhachia, and hyperproteinorrachia | INH + RIF + STP + ETI | Yes (ALL in active chemotherapy *) | No | 12 | SR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chemello, D.; Albertini, M.; Chester, J.; Esperti, S.; Ghidoni, E.; Orlando, G.; Franceschi, G.; Iaccarino, C.; Lucchesi, L.; Pavesi, G.; et al. Central Nervous System Infections Caused by Bacillus Calmette–Guerin: Case Report and Narrative Literature Review. Microorganisms 2025, 13, 1283. https://doi.org/10.3390/microorganisms13061283
Chemello D, Albertini M, Chester J, Esperti S, Ghidoni E, Orlando G, Franceschi G, Iaccarino C, Lucchesi L, Pavesi G, et al. Central Nervous System Infections Caused by Bacillus Calmette–Guerin: Case Report and Narrative Literature Review. Microorganisms. 2025; 13(6):1283. https://doi.org/10.3390/microorganisms13061283
Chicago/Turabian StyleChemello, Davide, Maddalena Albertini, Johanna Chester, Sara Esperti, Elena Ghidoni, Gabriella Orlando, Giacomo Franceschi, Corrado Iaccarino, Lucio Lucchesi, Giacomo Pavesi, and et al. 2025. "Central Nervous System Infections Caused by Bacillus Calmette–Guerin: Case Report and Narrative Literature Review" Microorganisms 13, no. 6: 1283. https://doi.org/10.3390/microorganisms13061283
APA StyleChemello, D., Albertini, M., Chester, J., Esperti, S., Ghidoni, E., Orlando, G., Franceschi, G., Iaccarino, C., Lucchesi, L., Pavesi, G., Mussini, C., & Franceschini, E. (2025). Central Nervous System Infections Caused by Bacillus Calmette–Guerin: Case Report and Narrative Literature Review. Microorganisms, 13(6), 1283. https://doi.org/10.3390/microorganisms13061283







