Emergence of NDM-1- and OXA-23-Co-Producing Acinetobacter baumannii ST1 Isolates from a Burn Unit in Spain
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Identification of Bacterial Isolates and Extraction of Carbapenemases Gene
2.3. Antibiotic Susceptibility Tests
2.4. Whole-Genome Sequencing and Read Assembly
2.5. Phylogenetic Analysis and Diversity
2.6. Antibiotic Resistance Genes, Virulence-Associated Genes, and Plasmids
2.7. Insertion Sequences in Carbapenem-Resistant A. baumannii
3. Results
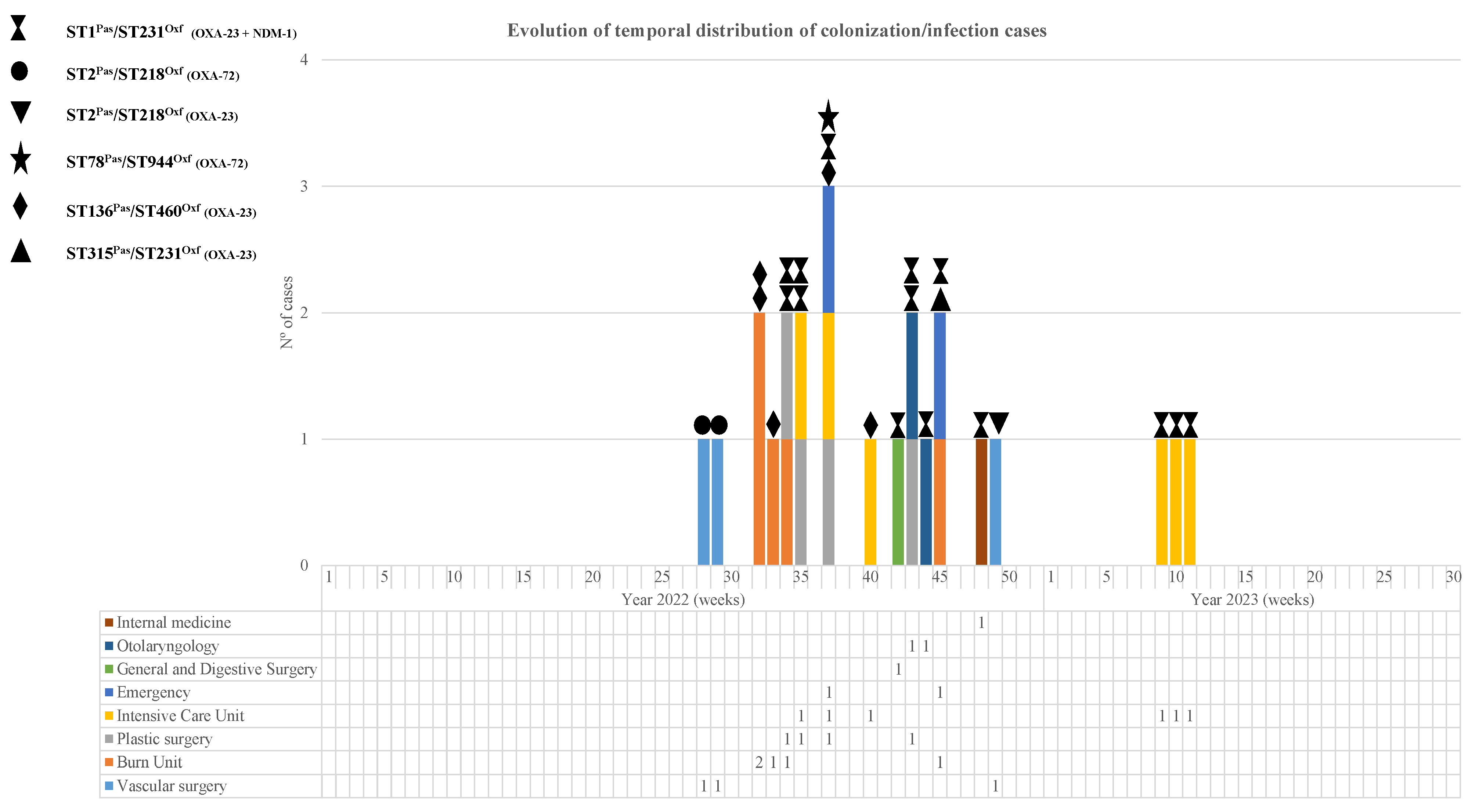
3.1. Patients and Description of the Outbreak
3.2. Carbapenemase Types and Phylogenetic Analysis of CRAB Isolates
3.3. Antibiotic Susceptibility Testing of CRAB Isolates
3.4. Resistome and Virulome of Carbapenemases-Producing CRAB
3.5. Characterization of the Virulence-Associated Genes
3.6. Capsular Exopolysaccharide in CRAB Isolates
3.7. Detection of Plasmids in CRAB Isolates
3.8. Infection Control Measures and Outcome
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MDRAB | Multidrug-resistant Acinetobacter baumannii |
| ICU | intensive care unit |
| CRAB | Carbapenem-resistant Acinetobacter baumannii |
| EARS-Net | European Antimicrobial Resistance Surveillance Network |
| HUG | University Hospital Getafe |
| AST | Antibiotic susceptibility testing |
| EUCAST | European Committee on Antimicrobial Susceptibility Testing |
| CgMLST | Multi-Locus Sequence-Typing analysis |
| ARGs | Acquired antibiotic resistance genes |
| KL | K locus |
| OCL | OC locus |
References
- Restrepo-Arbeláez, N.; García-Betancur, J.C.; Pallares, C.J.; El Ayoubi, L.W.; Kiratisin, P.; Kanj, S.S.; Villegas, M.V. Can Risk Factors and Risk Scores Help Predict Colonization and Infection in Multidrug-Resistant Gram-Negative Bacteria? Antimicrob. Steward. Healthc. Epidemiol. 2024, 4, e196. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.; Cerceo, E. Trends, Epidemiology, and Management of Multi-Drug Resistant Gram-Negative Bacterial Infections in the Hospitalized Setting. Antibiotics 2020, 9, 196. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-R.; Lee, J.H.; Park, M.; Park, K.S.; Bae, I.K.; Kim, Y.B.; Cha, C.-J.; Jeong, B.C.; Lee, S.H. Biology of Acinetobacter Baumannii: Pathogenesis, Antibiotic Resistance Mechanisms, and Prospective Treatment Options. Front. Cell Infect. Microbiol. 2017, 7, 55. [Google Scholar] [CrossRef]
- McConnell, M.J.; Actis, L.; Pachón, J. Acinetobacter Baumannii: Human Infections, Factors Contributing to Pathogenesis and Animal Models. FEMS Microbiol. Rev. 2013, 37, 130–155. [Google Scholar] [CrossRef]
- Gautam, D.; Dolma, K.G.; Khandelwal, B.; Mitsuwan, W.; Mahboob, T.; Pereira, M.L.; Nawaz, M.; Wiart, C.; Ardebili, A.; Siyadatpanah, A.; et al. Acinetobacter Baumannii: An Overview of Emerging Multidrug-Resistant Pathogen. Med. J. Malays. 2022, 77, 357–370. [Google Scholar]
- National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States 2019; U.S. Department of Health and Human Services, CDC: Atlanta, GA, USA, 2019. [Google Scholar]
- Girerd-Genessay, I.; Bénet, T.; Vanhems, P. Multidrug-Resistant Bacterial Outbreaks in Burn Units: A Synthesis of the Literature According to the ORION Statement. J. Burn Care Res. 2016, 37, 172–180. [Google Scholar] [CrossRef]
- Tacconelli, E.; Carrara, E.; Savoldi, A.; Harbarth, S.; Mendelson, M.; Monnet, D.L.; Pulcini, C.; Kahlmeter, G.; Kluytmans, J.; Carmeli, Y.; et al. Discovery, Research, and Development of New Antibiotics: The WHO Priority List of Antibiotic-Resistant Bacteria and Tuberculosis. Lancet Infect. Dis. 2018, 18, 318–327. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Antimicrobial Resistance in the EU/EEA (EARS-Net)—Annual Epidemiological Report for 2021; ECDC: Stockholm, Sweden, 2022.
- WHO. GLASS, 2019 WHO. Global Antimicrobial Resistance Surveillance System; WHO: Geneva, Switzerland, 2019.
- WHO. CAESAR, 2019. Central Asian and European Surveillance of Antimicrobial Resistance; WHO: Geneva, Switzerland, 2019.
- WHO. CHINET, 2017. China Antimicrobial Surveillance Network; WHO: Geneva, Switzerland, 2017.
- Amudhan, M.S.; Sekar, U.; Kamalanathan, A.; Balaraman, S. Bla(IMP) and Bla(VIM) Mediated Carbapenem Resistance in Pseudomonas and Acinetobacter Species in India. J. Infect. Dev. Ctries. 2012, 6, 757–762. [Google Scholar] [CrossRef]
- Khan, A.U.; Maryam, L.; Zarrilli, R. Structure, Genetics and Worldwide Spread of New Delhi Metallo-β-Lactamase (NDM): A Threat to Public Health. BMC Microbiol. 2017, 17, 101. [Google Scholar] [CrossRef]
- López, C.; Ayala, J.A.; Bonomo, R.A.; González, L.J.; Vila, A.J. Protein Determinants of Dissemination and Host Specificity of Metallo-β-Lactamases. Nat. Commun. 2019, 10, 3617. [Google Scholar] [CrossRef]
- Mathlouthi, N.; El Salabi, A.A.; Ben Jomàa-Jemili, M.; Bakour, S.; Al-Bayssari, C.; Zorgani, A.A.; Kraiema, A.; Elahmer, O.; Okdah, L.; Rolain, J.-M.; et al. Early Detection of Metallo-β-Lactamase NDM-1- and OXA-23 Carbapenemase-Producing Acinetobacter Baumannii in Libyan Hospitals. Int. J. Antimicrob. Agents 2016, 48, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Maamar, E.; Alonso, C.A.; Ferjani, S.; Jendoubi, A.; Hamzaoui, Z.; Jebri, A.; Saidani, M.; Ghedira, S.; Torres, C.; Boubaker, I.B.-B. NDM-1- and OXA-23-Producing Acinetobacter Baumannii Isolated from Intensive Care Unit Patients in Tunisia. Int. J. Antimicrob. Agents 2018, 52, 910–915. [Google Scholar] [CrossRef]
- Revathi, G.; Siu, L.K.; Lu, P.-L.; Huang, L.-Y. First Report of NDM-1-Producing Acinetobacter Baumannii in East Africa. Int. J. Infect. Dis. 2013, 17, e1255–e1258. [Google Scholar] [CrossRef]
- Uwingabiye, J.; Lemnouer, A.; Roca, I.; Alouane, T.; Frikh, M.; Belefquih, B.; Bssaibis, F.; Maleb, A.; Benlahlou, Y.; Kassouati, J.; et al. Clonal Diversity and Detection of Carbapenem Resistance Encoding Genes among Multidrug-Resistant Acinetobacter Baumannii Isolates Recovered from Patients and Environment in Two Intensive Care Units in a Moroccan Hospital. Antimicrob. Resist. Infect. Control 2017, 6, 99. [Google Scholar] [CrossRef] [PubMed]
- Ragueh, A.A.; Aboubaker, M.H.; Mohamed, S.I.; Rolain, J.-M.; Diene, S.M. Emergence of Carbapenem-Resistant Gram-Negative Isolates in Hospital Settings in Djibouti. Antibiotics 2023, 12, 1132. [Google Scholar] [CrossRef] [PubMed]
- Abouelfetouh, A.; Torky, A.S.; Aboulmagd, E. Phenotypic and Genotypic Characterization of Carbapenem-Resistant Acinetobacter Baumannii Isolates from Egypt. Antimicrob. Resist. Infect. Control 2019, 8, 185. [Google Scholar] [CrossRef]
- Ayoub Moubareck, C.; Hammoudi Halat, D.; Nabi, A.; AlSharhan, M.A.; AlDeesi, Z.O.; Han, A.; Celiloglu, H.; Karam Sarkis, D. Detection of OXA-23, GES-11 and NDM-1 among Carbapenem-Resistant Acinetobacter Baumannii in Dubai: A Preliminary Study. J. Glob. Antimicrob. Resist. 2021, 24, 27–28. [Google Scholar] [CrossRef]
- Karthikeyan, K.; Thirunarayan, M.A.; Krishnan, P. Coexistence of blaOXA-23 with blaNDM-1 and armA in Clinical Isolates of Acinetobacter Baumannii from India. J. Antimicrob. Chemother. 2010, 65, 2253–2254. [Google Scholar] [CrossRef]
- Joshi, P.R.; Acharya, M.; Kakshapati, T.; Leungtongkam, U.; Thummeepak, R.; Sitthisak, S. Co-Existence of blaOXA-23 and blaNDM-1 Genes of Acinetobacter Baumannii Isolated from Nepal: Antimicrobial Resistance and Clinical Significance. Antimicrob. Resist. Infect. Control 2017, 6, 21. [Google Scholar] [CrossRef]
- Leungtongkam, U.; Thummeepak, R.; Wongprachan, S.; Thongsuk, P.; Kitti, T.; Ketwong, K.; Runcharoen, C.; Chantratita, N.; Sitthisak, S. Dissemination of blaOXA-23, blaOXA-24, blaOXA-58, and blaNDM-1 Genes of Acinetobacter Baumannii Isolates from Four Tertiary Hospitals in Thailand. Microb. Drug Resist. 2018, 24, 55–62. [Google Scholar] [CrossRef]
- Krizova, L.; Bonnin, R.A.; Nordmann, P.; Nemec, A.; Poirel, L. Characterization of a Multidrug-Resistant Acinetobacter Baumannii Strain Carrying the blaNDM-1 and blaOXA-23 Carbapenemase Genes from the Czech Republic. J. Antimicrob. Chemother. 2012, 67, 1550–1552. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lukovic, B.; Gajic, I.; Dimkic, I.; Kekic, D.; Zornic, S.; Pozder, T.; Radisavljevic, S.; Opavski, N.; Kojic, M.; Ranin, L. The First Nationwide Multicenter Study of Acinetobacter Baumannii Recovered in Serbia: Emergence of OXA-72, OXA-23 and NDM-1-Producing Isolates. Antimicrob. Resist. Infect. Control 2020, 9, 101. [Google Scholar] [CrossRef] [PubMed]
- Garner, J.S.; Jarvis, W.R.; Emori, T.G.; Horan, T.C.; Hughes, J.M. CDC Definitions for Nosocomial Infections, 1988. Am. J. Infect. Control 1988, 16, 128–140. [Google Scholar] [CrossRef]
- Girlich, D.; Bogaerts, P.; Bouchahrouf, W.; Bernabeu, S.; Langlois, I.; Begasse, C.; Arangia, N.; Dortet, L.; Huang, T.-D.; Glupczynski, Y.; et al. Evaluation of the Novodiag CarbaR+, a Novel Integrated Sample to Result Platform for the Multiplex Qualitative Detection of Carbapenem and Colistin Resistance Markers. Microb. Drug Resist. 2021, 27, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Holma, T.; Antikainen, J.; Haiko, J. Evaluation of Three Molecular Carbapenemase Tests: Eazyplex SuperBug Complete B, Novodiag CarbaR+, and Amplidiag CarbaR+MCR. J. Microbiol. Methods 2021, 180, 106105. [Google Scholar] [CrossRef]
- ISO 20776-1:2019; Susceptibility Testing of Infectious Agents and Evaluation of Performance of Antimicrobial Susceptibility Test Devices. Part 1: Broth Micro-Dilution Reference Method for Testing the In Vitro Activity of Antimicrobial Agents Against Rapidly Growing Aerobic Bacteria Involved in Infectious Diseases. International Organization for Standardization: Geneva, Switzerland, 2019.
- EUCAST. Breakpoint Tables for Interpretation of MICs and Zone Diameters, version 12.0; EUCAST: Växjö, Sweden, 2022. [Google Scholar]
- M100; Performance Standards for Antimicrobial Susceptibility Testing, 33rd Edition. Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2023.
- Chen, S.; Zhou, Y.; Chen, Y.; Gu, J. Fastp: An Ultra-Fast All-in-One FASTQ Preprocessor. Bioinformatics 2018, 34, i884–i890. [Google Scholar] [CrossRef]
- Wick, R.R.; Judd, L.M.; Gorrie, C.L.; Holt, K.E. Unicycler: Resolving Bacterial Genome Assemblies from Short and Long Sequencing Reads. PLoS Comput. Biol. 2017, 13, e1005595. [Google Scholar] [CrossRef]
- Seemann, T. Prokka: Rapid Prokaryotic Genome Annotation. Bioinformatics 2014, 30, 2068–2069. [Google Scholar] [CrossRef]
- Hunt, M.; Mather, A.E.; Sánchez-Busó, L.; Page, A.J.; Parkhill, J.; Keane, J.A.; Harris, S.R. ARIBA: Rapid Antimicrobial Resistance Genotyping Directly from Sequencing Reads. Microb. Genom. 2017, 3, e000131. [Google Scholar] [CrossRef]
- Diancourt, L.; Passet, V.; Nemec, A.; Dijkshoorn, L.; Brisse, S. The Population Structure of Acinetobacter Baumannii: Expanding Multiresistant Clones from an Ancestral Susceptible Genetic Pool. PLoS ONE 2010, 5, e10034. [Google Scholar] [CrossRef]
- Bartual, S.G.; Seifert, H.; Hippler, C.; Luzon, M.A.D.; Wisplinghoff, H.; Rodríguez-Valera, F. Development of a Multilocus Sequence Typing Scheme for Characterization of Clinical Isolates of Acinetobacter Baumannii. J. Clin. Microbiol. 2005, 43, 4382–4390. [Google Scholar] [CrossRef]
- Lucidi, M.; Visaggio, D.; Migliaccio, A.; Capecchi, G.; Visca, P.; Imperi, F.; Zarrilli, R. Pathogenicity and Virulence of Acinetobacter Baumannii: Factors Contributing to the Fitness in Healthcare Settings and the Infected Host. Virulence 2024, 15, 2289769. [Google Scholar] [CrossRef]
- Pérez-Vazquez, M.; Oteo-Iglesias, J.; Sola-Campoy, P.J.; Carrizo-Manzoni, H.; Bautista, V.; Lara, N.; Aracil, B.; Alhambra, A.; Martínez-Martínez, L.; Campos, J.; et al. Characterization of Carbapenemase-Producing Klebsiella Oxytoca in Spain, 2016–2017. Antimicrob. Agents Chemother. 2019, 63, e02529-18. [Google Scholar] [CrossRef] [PubMed]
- Wyres, K.L.; Cahill, S.M.; Holt, K.E.; Hall, R.M.; Kenyon, J.J. Identification of Acinetobacter Baumannii Loci for Capsular Polysaccharide (KL) and Lipooligosaccharide Outer Core (OCL) Synthesis in Genome Assemblies Using Curated Reference Databases Compatible with Kaptive. Microb. Genom. 2020, 6, e000339. [Google Scholar] [CrossRef] [PubMed]
- Hawkey, J.; Hamidian, M.; Wick, R.R.; Edwards, D.J.; Billman-Jacobe, H.; Hall, R.M.; Holt, K.E. ISMapper: Identifying Transposase Insertion Sites in Bacterial Genomes from Short Read Sequence Data. BMC Genom. 2015, 16, 667. [Google Scholar] [CrossRef]
- Adams, M.D.; Bishop, B.; Wright, M.S. Quantitative Assessment of Insertion Sequence Impact on Bacterial Genome Architecture. Microb. Genom. 2016, 2, e000062. [Google Scholar] [CrossRef]
- Holt, K.E.; Hamidian, M.; Kenyon, J.J.; Wynn, M.T.; Hawkey, J.; Pickard, D.; Hall, R.M. Genome Sequence of Acinetobacter Baumannii Strain A1, an Early Example of Antibiotic-Resistant Global Clone 1. Genome Announc. 2015, 3, e00032-15. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Kim, C.-K.; Lee, H.; Jeong, S.H.; Yong, D.; Lee, K. A Novel Insertion Sequence, ISAba10, Inserted into ISAba1 Adjacent to the Bla(OXA-23) Gene and Disrupting the Outer Membrane Protein Gene carO in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2011, 55, 361–363. [Google Scholar] [CrossRef]
- Smani, Y.; Fàbrega, A.; Roca, I.; Sánchez-Encinales, V.; Vila, J.; Pachón, J. Role of OmpA in the Multidrug Resistance Phenotype of Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2014, 58, 1806–1808. [Google Scholar] [CrossRef]
- Sun, X.; Ni, Z.; Tang, J.; Ding, Y.; Wang, X.; Li, F. The abaI/abaR Quorum Sensing System Effects on Pathogenicity in Acinetobacter Baumannii. Front. Microbiol. 2021, 12, 679241. [Google Scholar] [CrossRef]
- Choi, A.H.K.; Slamti, L.; Avci, F.Y.; Pier, G.B.; Maira-Litrán, T. The pgaABCD Locus of Acinetobacter Baumannii Encodes the Production of Poly-Beta-1-6-N-Acetylglucosamine, Which Is Critical for Biofilm Formation. J. Bacteriol. 2009, 191, 5953–5963. [Google Scholar] [CrossRef]
- Neres, J.; Wilson, D.J.; Celia, L.; Beck, B.J.; Aldrich, C.C. Aryl Acid Adenylating Enzymes Involved in Siderophore Biosynthesis: Fluorescence Polarization Assay, Ligand Specificity, and Discovery of Non-Nucleoside Inhibitors via High-Throughput Screening. Biochemistry 2008, 47, 11735–11749. [Google Scholar] [CrossRef]
- Tomaras, A.P.; Dorsey, C.W.; Edelmann, R.E.; Actis, L.A. Attachment to and Biofilm Formation on Abiotic Surfaces by Acinetobacter Baumannii: Involvement of a Novel Chaperone-Usher Pili Assembly System. Microbiology 2003, 149, 3473–3484. [Google Scholar] [CrossRef]
- Singh, M.; De Silva, P.M.; Al-Saadi, Y.; Switala, J.; Loewen, P.C.; Hausner, G.; Chen, W.; Hernandez, I.; Castillo-Ramirez, S.; Kumar, A. Characterization of Extremely Drug-Resistant and Hypervirulent Acinetobacter Baumannii AB030. Antibiotics 2020, 9, 328. [Google Scholar] [CrossRef] [PubMed]
- Lötsch, F.; Albiger, B.; Monnet, D.L.; Struelens, M.J.; Seifert, H.; Kohlenberg, A.; European Antimicrobial Resistance Genes Surveillance Network (EURGen-Net) Carbapenem-Resistant Acinetobacter Baumannii Capacity Survey Group; EURGen-Net Carbapenem-Resistant Acinetobacter Baumannii Capacity Survey Group. Epidemiological Situation, Laboratory Capacity and Preparedness for Carbapenem-Resistant Acinetobacter Baumannii in Europe, 2019. Euro Surveill. 2020, 25, 2001735. [Google Scholar] [CrossRef] [PubMed]
- Doughty, E.L.; Liu, H.; Moran, R.A.; Hua, X.; Ba, X.; Guo, F.; Chen, X.; Zhang, L.; Holmes, M.; van Schaik, W.; et al. Endemicity and Diversification of Carbapenem-Resistant Acinetobacter Baumannii in an Intensive Care Unit. Lancet Reg. Health West. Pac. 2023, 37, 100780. [Google Scholar] [CrossRef] [PubMed]
- Medioli, F.; Bacca, E.; Faltoni, M.; Burastero, G.J.; Volpi, S.; Menozzi, M.; Orlando, G.; Bedini, A.; Franceschini, E.; Mussini, C.; et al. Is It Possible to Eradicate Carbapenem-Resistant Acinetobacter baumannii (CRAB) from Endemic Hospitals? Antibiotics 2022, 11, 1015. [Google Scholar] [CrossRef] [PubMed]
- Bedenić, B.; Bratić, V.; Mihaljević, S.; Lukić, A.; Vidović, K.; Reiner, K.; Schöenthaler, S.; Barišić, I.; Zarfel, G.; Grisold, A. Multidrug-Resistant Bacteria in a COVID-19 Hospital in Zagreb. Pathogens 2023, 12, 117. [Google Scholar] [CrossRef]
- Huang, W.; Qiao, F.; Cai, L.; Zong, Z.; Zhang, W. Effect of Daily Chlorhexidine Bathing on Reducing Infections Caused by Multidrug-Resistant Organisms in Intensive Care Unit Patients: A Semiexperimental Study with Parallel Controls. J. Evid. Based Med. 2023, 16, 32–38. [Google Scholar] [CrossRef]
- Mangioni, D.; Fox, V.; Chatenoud, L.; Bolis, M.; Bottino, N.; Cariani, L.; Gentiloni Silverj, F.; Matinato, C.; Monti, G.; Muscatello, A.; et al. Genomic Characterization of Carbapenem-Resistant Acinetobacter Baumannii (CRAB) in Mechanically Ventilated COVID-19 Patients and Impact of Infection Control Measures on Reducing CRAB Circulation during the Second Wave of the SARS-CoV-2 Pandemic in Milan, Italy. Microbiol. Spectr. 2023, 11, e0020923. [Google Scholar] [CrossRef]
- Xiong, L.; Deng, C.; Yang, G.; Shen, M.; Chen, B.; Tian, R.; Zha, H.; Wu, K. Molecular Epidemiology and Antimicrobial Resistance Patterns of Carbapenem-Resistant Acinetobacter Baumannii Isolates from Patients Admitted at ICUs of a Teaching Hospital in Zunyi, China. Front. Cell Infect. Microbiol. 2023, 13, 1280372. [Google Scholar] [CrossRef] [PubMed]
- Müller, C.; Reuter, S.; Wille, J.; Xanthopoulou, K.; Stefanik, D.; Grundmann, H.; Higgins, P.G.; Seifert, H. A Global View on Carbapenem-Resistant Acinetobacter Baumannii. mBio 2023, 14, e0226023. [Google Scholar] [CrossRef]
- Ejaz, H.; Ahmad, M.; Younas, S.; Junaid, K.; Abosalif, K.O.A.; Abdalla, A.E.; Alameen, A.A.M.; Elamir, M.Y.M.; Bukhari, S.N.A.; Ahmad, N.; et al. Molecular Epidemiology of Extensively-Drug Resistant Acinetobacter Baumannii Sequence Type 2 Co-Harboring Bla NDM and Bla OXA From Clinical Origin. Infect. Drug Resist. 2021, 14, 1931–1939. [Google Scholar] [CrossRef] [PubMed]
- Choby, J.E.; Ozturk, T.; Satola, S.W.; Jacob, J.T.; Weiss, D.S. Widespread Cefiderocol Heteroresistance in Carbapenem-Resistant Gram-Negative Pathogens. Lancet Infect. Dis. 2021, 21, 597–598. [Google Scholar] [CrossRef]
- Shahryari, S.; Mohammadnejad, P.; Noghabi, K.A. Screening of Anti-Acinetobacter Baumannii Phytochemicals, Based on the Potential Inhibitory Effect on OmpA and OmpW Functions. R. Soc. Open Sci. 2021, 8, 201652. [Google Scholar] [CrossRef]
- Lioy, V.S.; Goussard, S.; Guerineau, V.; Yoon, E.-J.; Courvalin, P.; Galimand, M.; Grillot-Courvalin, C. Aminoglycoside Resistance 16S rRNA Methyltransferases Block Endogenous Methylation, Affect Translation Efficiency and Fitness of the Host. RNA 2014, 20, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.J.; Rather, P.N.; Hare, R.S.; Miller, G.H. Molecular Genetics of Aminoglycoside Resistance Genes and Familial Relationships of the Aminoglycoside-Modifying Enzymes. Microbiol. Rev. 1993, 57, 138–163. [Google Scholar] [CrossRef]
- El-Sayed-Ahmed, M.A.E.-G.; Amin, M.A.; Tawakol, W.M.; Loucif, L.; Bakour, S.; Rolain, J.-M. High Prevalence of Bla(NDM-1) Carbapenemase-Encoding Gene and 16S rRNA armA Methyltransferase Gene among Acinetobacter Baumannii Clinical Isolates in Egypt. Antimicrob. Agents Chemother. 2015, 59, 3602–3605. [Google Scholar] [CrossRef]
- Sánchez-Urtaza, S.; Ocampo-Sosa, A.; Molins-Bengoetxea, A.; El-Kholy, M.A.; Hernandez, M.; Abad, D.; Shawky, S.M.; Alkorta, I.; Gallego, L. Molecular Characterization of Multidrug Resistant Acinetobacter Baumannii Clinical Isolates from Alexandria, Egypt. Front. Cell. Infect. Microbiol. 2023, 13, 1208046. [Google Scholar] [CrossRef]
- Genteluci, G.L.; de Souza, P.A.; Gomes, D.B.C.; Sousa, V.S.; de Souza, M.J.; Abib, J.R.L.; de Castro, E.A.R.; Rangel, K.; Villas Bôas, M.H.S. Polymyxin B Heteroresistance and Adaptive Resistance in Multidrug- and Extremely Drug-Resistant Acinetobacter Baumannii. Curr. Microbiol. 2020, 77, 2300–2306. [Google Scholar] [CrossRef]
- Meschiari, M.; Lòpez-Lozano, J.-M.; Di Pilato, V.; Gimenez-Esparza, C.; Vecchi, E.; Bacca, E.; Orlando, G.; Franceschini, E.; Sarti, M.; Pecorari, M.; et al. A Five-Component Infection Control Bundle to Permanently Eliminate a Carbapenem-Resistant Acinetobacter Baumannii Spreading in an Intensive Care Unit. Antimicrob. Resist. Infect. Control 2021, 10, 123. [Google Scholar] [CrossRef] [PubMed]
- Moghnieh, R.A.; Kanafani, Z.A.; Tabaja, H.Z.; Sharara, S.L.; Awad, L.S.; Kanj, S.S. Epidemiology of Common Resistant Bacterial Pathogens in the Countries of the Arab League. Lancet Infect. Dis. 2018, 18, e379–e394. [Google Scholar] [CrossRef]
- Hsu, L.-Y.; Apisarnthanarak, A.; Khan, E.; Suwantarat, N.; Ghafur, A.; Tambyah, P.A. Carbapenem-Resistant Acinetobacter Baumannii and Enterobacteriaceae in South and Southeast Asia. Clin. Microbiol. Rev. 2017, 30, 1–22. [Google Scholar] [CrossRef]
- Wareth, G.; Linde, J.; Nguyen, N.H.; Nguyen, T.N.M.; Sprague, L.D.; Pletz, M.W.; Neubauer, H. WGS-Based Analysis of Carbapenem-Resistant Acinetobacter Baumannii in Vietnam and Molecular Characterization of Antimicrobial Determinants and MLST in Southeast Asia. Antibiotics 2021, 10, 563. [Google Scholar] [CrossRef]
- Aldali, J.A. Acinetobacter Baumannii: A Multidrug-Resistant Pathogen, Has Emerged in Saudi Arabia. Saudi Med. J. 2023, 44, 732–744. [Google Scholar] [CrossRef]
- Falcone, M.; Tiseo, G.; Carbonara, S.; Marino, A.; Di Caprio, G.; Carretta, A.; Mularoni, A.; Mariani, M.F.; Maraolo, A.E.; Scotto, R.; et al. Mortality Attributable to Bloodstream Infections Caused by Different Carbapenem-Resistant Gram-Negative Bacilli: Results From a Nationwide Study in Italy (ALARICO Network). Clin. Infect. Dis. 2023, 76, 2059–2069. [Google Scholar] [CrossRef] [PubMed]
- Goic-Barisic, I.; Music, M.S.; Drcelic, M.; Tuncbilek, S.; Akca, G.; Jakovac, S.; Tonkić, M.; Hrenovic, J. Molecular Characterisation of Colistin and Carbapenem-Resistant Clinical Isolates of Acinetobacter Baumannii from Southeast Europe. J. Glob. Antimicrob. Resist. 2023, 33, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Humphries, R.M.; Janssen, H.; Hey-Hadavi, J.H.; Hackel, M.; Sahm, D. Multidrug-Resistant Gram-Negative Bacilli Recovered from Respiratory and Blood Specimens from Adults: The ATLAS Surveillance Program in European Hospitals, 2018–2020. Int. J. Antimicrob. Agents 2023, 61, 106724. [Google Scholar] [CrossRef]
- Reich, S.; Adler, A. Introduction and Spread of NDM-Producing Enterobacterales and Acinetobacter Baumannii into Middle Eastern Countries: A Molecular-Based Hypothesis. Expert. Rev. Anti Infect. Ther. 2023, 21, 749–758. [Google Scholar] [CrossRef]
- Sandfort, M.; Hans, J.B.; Fischer, M.A.; Reichert, F.; Cremanns, M.; Eisfeld, J.; Pfeifer, Y.; Heck, A.; Eckmanns, T.; Werner, G.; et al. Increase in NDM-1 and NDM-1/OXA-48-Producing Klebsiella Pneumoniae in Germany Associated with the War in Ukraine, 2022. Euro Surveill. 2022, 27, 2200926. [Google Scholar] [CrossRef]


| Microbiological Data of Patients | ||||||
|---|---|---|---|---|---|---|
| Case | Age | Sex (M/F) * | Date of First Isolation | Sample | Diagnostic/Colonization | Clinical Ward Where the Sample Was Obtained |
| 1 | 72 | M | 7 July 2022 | Biopsy | Diagnostic | Vascular surgery |
| 2 | 89 | M | 14 July 2022 | Abscess/Pus | Diagnostic | Vascular surgery |
| 3 | 35 | M | 6 August 2022 | Burn exudate | Colonization | Burn unit |
| 4 | 24 | M | 6 August 2022 | Tracheal aspirate | Diagnostic | Burn unit |
| 5 | 19 | M | 14 August 2022 | Tracheal aspirate | Diagnostic | Burn unit |
| 6 | 32 | M | 15 August 2022 | Tracheal aspirate | Diagnostic | Burn unit |
| 7 | 50 | M | 17 August 2022 | Catheter | Diagnostic | Plastic surgery |
| 8 | 50 | M | 25 August 2022 | Catheter | Diagnostic | Plastic surgery |
| 9 | 78 | M | 25 August 2022 | Blood | Diagnostic | Intensive care unit |
| 10 | 68 | M | 5 September 2022 | Burn exudate | Diagnostic | Plastic surgery |
| 11 | 84 | F | 9 September 2022 | Aspirate puncture | Diagnostic | Intensive care unit |
| 12 | 82 | F | 11 September 2022 | Surgical wound exudate | Diagnostic | Emergency |
| 13 | 90 | M | 28 September 2022 | Blood | Diagnostic | Intensive care unit |
| 14 | 46 | F | 13 October 2022 | Rectal swab | Colonization | General and digestive surgery |
| 15 | 78 | M | 19 October 2022 | Abscess/Pus | Diagnostic | Otolaryngology |
| 16 | 79 | F | 21 October 2022 | Rectal swab | Colonization | Plastic surgery |
| 17 | 63 | F | 27 October 2022 | Rectal swab | Colonization | Otolaryngology |
| 18 | 61 | F | 3 November 2022 | Rectal swab | Colonization | Burn unit |
| 19 | 43 | F | 6 November 2022 | Skin and soft tissue exudate | Diagnostic | Emergency |
| 20 | 19 | F | 24 November 2022 | Rectal swab | Colonization | Internal medicine |
| 21 | 57 | F | 1 December 2022 | Non-surgical wound exudate | Diagnostic | Vascular surgery |
| 22 | 52 | F | 21 February 2023 | Rectal swab | Colonization | Intensive care unit |
| 23 | 78 | M | 28 February 2023 | Tracheal aspirate | Diagnostic | Intensive care unit |
| 24 | 64 | F | 3 March 2023 | Tracheal aspirate | Diagnostic | Intensive care unit |
| Isolate | Pasteur ST | Oxford ST | Acquired β-Lactamase | Chromosomal β-Lactamase | |
|---|---|---|---|---|---|
| Carbapenemase | Carbapenemase | AmpC | |||
| 1 | 2 | 218 | blaOXA-72 | blaOXA-66 | blaADC-30 |
| 2 | 2 | 218 | blaOXA-72 | blaOXA-66 | blaADC-30 |
| 3 | 136 | 460 | blaOXA-23 | blaOXA-409 | blaADC-88 |
| 4 | 136 | 460 | blaOXA-23 | blaOXA-409 | blaADC-88 |
| 5 | 136 | 460 | blaOXA-23 | blaOXA-409 | blaADC-88 |
| 6 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 7 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 8 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 9 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 10 | 136 | 460 | blaOXA-23 | blaOXA-409 | blaADC-88 |
| 11 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 12 | 78 | 944 | blaOXA-72 | blaOXA-90 | blaADC-152 |
| 13 | 136 | 460 | blaOXA-23 | blaOXA-409 | blaADC-88 |
| 14 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 15 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 16 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 17 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 18 | 315 | 231 | blaOXA-23 | blaOXA-69 | blaADC-79 |
| 19 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 20 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 21 | 2 | 218 | blaOXA-23 | blaOXA-69 | blaADC-30 |
| 22 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 23 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| 24 | 1 | 231 | blaOXA-23blaNDM-1 | blaOXA-69 | blaADC-191 |
| Antibiotics. | * S% Total Isolates (n) | * I% Total Isolates (n) | * R% Total Isolates (n) | *** MIC50 | *** MIC90 |
|---|---|---|---|---|---|
| Amikacin | 4.2 (1) | - | 95.8 (23) | 32 | 32 |
| Cefiderocol ** | 83.3 (20) | - | 16.7 (4) | - | - |
| Ceftazidime | 0 | - | 100 (24) | >16 | >16 |
| Ciprofloxacin | 0 | - | 100 (24) | >2 | >2 |
| Colistin | 91.6 (22) | - | 8.3 (2) | 1 | 1 |
| Gentamicin | 0 | - | 100 (24) | >8 | >8 |
| Imipenem | 0 | - | 100 (24) | >16 | >16 |
| Meropenem | 0 | - | 100 (24) | >16 | >16 |
| Piperaciclin/Tazobactam | 0 | - | 100 (24) | >32/4 | >32/4 |
| Tobramycin | 0 | - | 100 (24) | >8 | >8 |
| Trimethoprim-Sulfamethoxazole | 0 | 12.5 (3) | 87.5 (21) | >8/152 | >8/152 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hidalgo, E.; Sotelo, J.; Pérez-Vázquez, M.; Iniesta, Á.; Cañada-García, J.E.; Valiente, O.; Aracil, B.; Arana, D.M.; Oteo-Iglesias, J. Emergence of NDM-1- and OXA-23-Co-Producing Acinetobacter baumannii ST1 Isolates from a Burn Unit in Spain. Microorganisms 2025, 13, 1149. https://doi.org/10.3390/microorganisms13051149
Hidalgo E, Sotelo J, Pérez-Vázquez M, Iniesta Á, Cañada-García JE, Valiente O, Aracil B, Arana DM, Oteo-Iglesias J. Emergence of NDM-1- and OXA-23-Co-Producing Acinetobacter baumannii ST1 Isolates from a Burn Unit in Spain. Microorganisms. 2025; 13(5):1149. https://doi.org/10.3390/microorganisms13051149
Chicago/Turabian StyleHidalgo, Elena, Jared Sotelo, María Pérez-Vázquez, Ángela Iniesta, Javier E. Cañada-García, Olga Valiente, Belén Aracil, David M. Arana, and Jesús Oteo-Iglesias. 2025. "Emergence of NDM-1- and OXA-23-Co-Producing Acinetobacter baumannii ST1 Isolates from a Burn Unit in Spain" Microorganisms 13, no. 5: 1149. https://doi.org/10.3390/microorganisms13051149
APA StyleHidalgo, E., Sotelo, J., Pérez-Vázquez, M., Iniesta, Á., Cañada-García, J. E., Valiente, O., Aracil, B., Arana, D. M., & Oteo-Iglesias, J. (2025). Emergence of NDM-1- and OXA-23-Co-Producing Acinetobacter baumannii ST1 Isolates from a Burn Unit in Spain. Microorganisms, 13(5), 1149. https://doi.org/10.3390/microorganisms13051149







