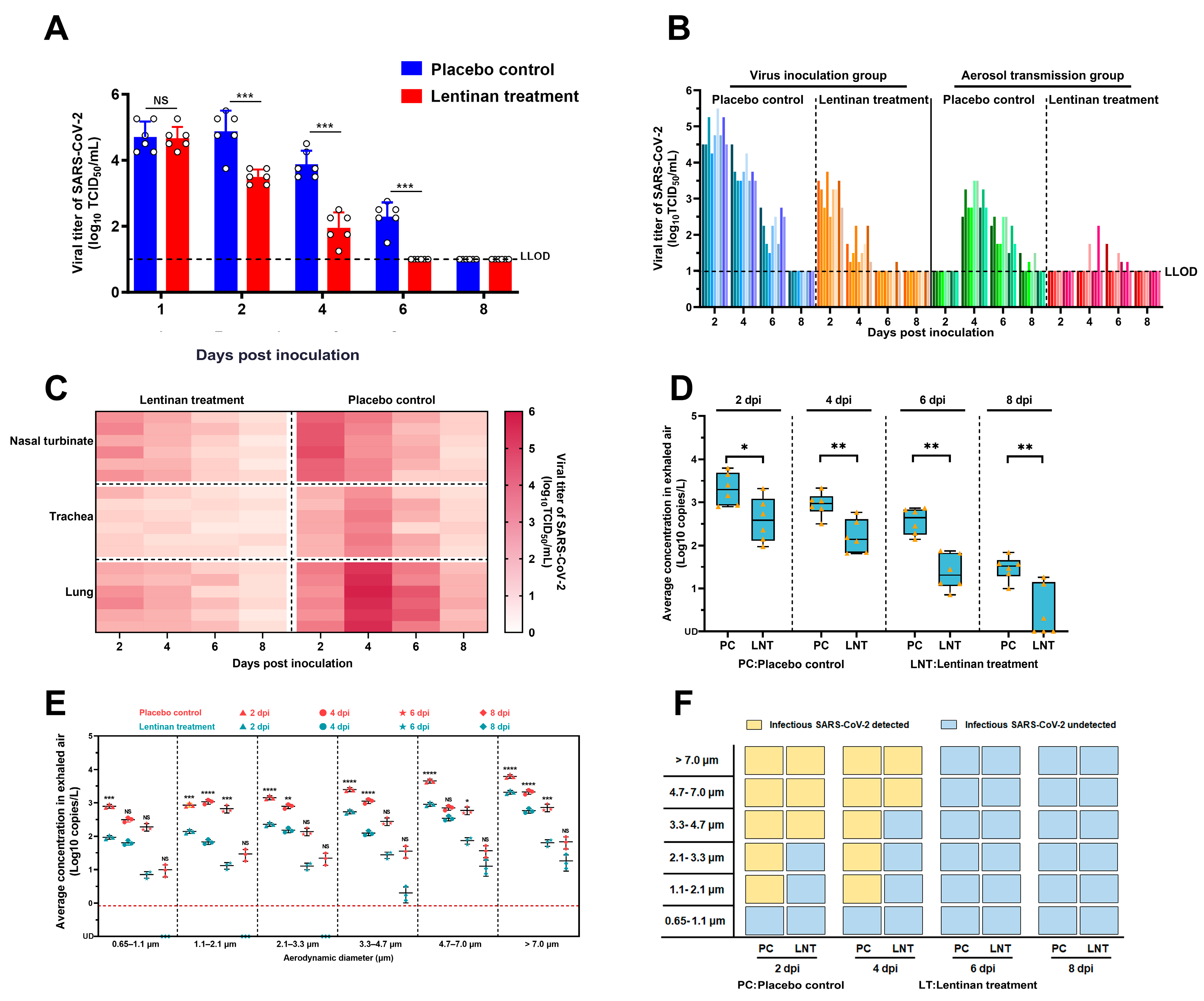
Lentinan Reduces Transmission Efficiency of COVID-19 by Changing Aerodynamic Characteristic of Exhaled SARS-CoV-2 Aerosols in Golden Hamsters
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Viruses and Cells
2.3. Hamsters
2.4. Source and Dosage of Lentinan
2.5. Viral Load and Tissue Distribution of SARS-CoV-2 in the Respiratory Tract of Hamsters
2.6. Collection of Exhaled Viral Aerosols from Hamsters
2.7. SARS-CoV-2 Airborne Transmission Studies in Hamsters
2.8. Viral Nucleic Acid Testing
2.9. Statistical Analysis
3. Results and Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guo, Z.D.; Wang, Z.Y.; Zhang, S.F.; Li, X.; Li, L.; Li, C.; Cui, Y.; Fu, R.B.; Dong, Y.Z.; Chi, X.Y.; et al. Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China, 2020. Emerg. Infect. Dis. 2020, 26, 1583–1591. [Google Scholar] [CrossRef] [PubMed]
- Morawska, L.; Milton, D.K. It Is Time to Address Airborne Transmission of Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 2020, 71, 2311–2313. [Google Scholar] [CrossRef]
- Zheng, J.; Wang, Z.; Li, J.; Zhang, Y.; Jiang, L.; Fu, Y.; Jin, Y.; Cheng, H.; Li, J.; Chen, Z.; et al. High amounts of SARS-CoV-2 in aerosols exhaled by patients with Omicron variant infection. J. Infect. 2022, 84, e126–e128. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, J.; Jiang, L.; Chen, Q.; Fu, Y.; Jin, Y.; Chen, Z.; Tang, F.; Zeng, X.; Wen, H.; et al. Comparison of SARS-CoV-2 aerosol emission from patients with Omicron BA.1 or BA.2 subvariant infection. J. Infect. 2022, 85, e37–e39. [Google Scholar] [CrossRef] [PubMed]
- Mao, X.; Hu, H.; Xiao, X.; Chen, D.; Yu, B.; He, J.; Yu, J.; Zheng, P.; Luo, J.; Luo, Y.; et al. Lentinan administration relieves gut barrier dysfunction induced by rotavirus in a weaned piglet model. Food Funct. 2019, 10, 2094–2101. [Google Scholar] [CrossRef]
- Kuang, Z.; Jin, T.; Wu, C.; Zong, Y.; Yin, P.; Dong, W.; Lin, X.; You, W.; Zhang, C.; Wang, L.; et al. Lentinan Attenuates Damage of the Small Intestinal Mucosa, Liver, and Lung in Mice with Gut-Origin Sepsis. J. Immunol. Res. 2021, 2021, 2052757. [Google Scholar] [CrossRef]
- Volman, J.J.; Ramakers, J.D.; Plat, J. Dietary modulation of immune function by beta-glucans. Physiol. Behav. 2008, 94, 276–284. [Google Scholar] [CrossRef]
- Ren, G.; Li, K.; Hu, Y.; Yu, M.; Qu, J.; Xu, X. Optimization of selenizing conditions for Seleno-Lentinan and its characteristics. Int. J. Biol. Macromol. 2015, 81, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhang, Y.; Zhang, L.; Tian, Q. Mushroom polysaccharide lentinan for treating different types of cancers: A review of 12 years clinical studies in China. Prog. Mol. Biol. Transl. Sci. 2019, 163, 297–328. [Google Scholar]
- Sun, M.; Zhao, W.; Xie, Q.; Zhan, Y.; Wu, B. Lentinan reduces tumor progression by enhancing gemcitabine chemotherapy in urothelial bladder cancer. Surg. Oncol. 2015, 24, 28–34. [Google Scholar] [CrossRef]
- Cui, H.; Zhang, C.; Zhang, C.; Cai, Z.; Chen, L.; Chen, Z.; Zhao, K.; Qiao, S.; Wang, Y.; Meng, L.; et al. Anti-Influenza Effect and Mechanisms of Lentinan in an ICR Mouse Model. Front. Cell. Infect. Microbiol. 2022, 12, 892864. [Google Scholar] [CrossRef] [PubMed]
- Ren, G.; Xu, L.; Lu, T.; Yin, J. Structural characterization and antiviral activity of lentinan from Lentinus edodes mycelia against infectious hematopoietic necrosis virus. Int. J. Biol. Macromol. 2018, 115, 1202–1210. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Okubo, A.; Yamazaki, S.; Suzuki, K.; Mitsuya, H.; Toda, S. Inhibition of the infectivity and cytopathic effect of human immunodeficiency virus by water-soluble lignin in an extract of the culture medium of Lentinus edodes mycelia (LEM). Biochem. Biophys. Res. Commun. 1989, 160, 367–373. [Google Scholar] [CrossRef]
- Sarkar, S.; Koga, J.; Whitley, R.J.; Chatterjee, S. Antiviral effect of the extract of culture medium of Lentinus edodes mycelia on the replication of herpes simplex virus type 1. Antivir. Res. 1993, 20, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Fan, W.; You, B.; Wang, X.; Zheng, X.; Xu, A.; Liu, Y.; Peng, H.; Yin, W.; Xu, M.; Dong, X.; et al. Safety and efficacy of lentinan nasal drops in patients infected with the variant of COVID-19: A randomized, placebo-controlled trial. Front. Pharmacol. 2023, 14, 1292479. [Google Scholar] [CrossRef]
- Sia, S.F.; Yan, L.M.; Chin, A.W.H.; Fung, K.; Choy, K.T.; Wong, A.Y.L.; Kaewpreedee, P.; Perera, R.A.P.M.; Poon, L.L.M.; Nicholls, J.M.; et al. Pathogenesis and transmission of SARS-CoV-2 in golden hamsters. Nature 2020, 583, 834–838. [Google Scholar] [CrossRef]
- Chan, J.F.; Zhang, A.J.; Yuan, S.; Poon, V.K.; Chan, C.C.; Lee, A.C.; Chan, W.M.; Fan, Z.; Tsoi, H.W.; Wen, L.; et al. Simulation of the Clinical and Pathological Manifestations of Coronavirus Disease 2019 (COVID-19) in a Golden Syrian Hamster Model: Implications for Disease Pathogenesis and Transmissibility. Clin. Infect. Dis. 2020, 71, 2428–2446. [Google Scholar] [CrossRef]
- Imai, M.; Iwatsuki-Horimoto, K.; Hatta, M.; Loeber, S.; Halfmann, P.J.; Nakajima, N.; Watanabe, T.; Ujie, M.; Takahashi, K.; Ito, M.; et al. Syrian hamsters as a small animal model for SARS-CoV-2 infection and countermeasure development. Proc. Natl. Acad. Sci. USA 2020, 117, 16587–16595. [Google Scholar] [CrossRef]
- Yahalom-Ronen, Y.; Tamir, H.; Melamed, S.; Politi, B.; Shifman, O.; Achdout, H.; Vitner, E.B.; Israeli, O.; Milrot, E.; Stein, D.; et al. A single dose of recombinant VSV-∆G-spike vaccine provides protection against SARS-CoV-2 challenge. Nat. Commun. 2020, 11, 6402. [Google Scholar] [CrossRef]
- Rogers, T.F.; Zhao, F.; Huang, D.; Beutler, N.; Burns, A.; He, W.T.; Limbo, O.; Smith, C.; Song, G.; Woehl, J.; et al. Isolation of potent SARS-CoV-2 neutralizing antibodies and protection from disease in a small animal model. Science 2020, 369, 956–963. [Google Scholar] [CrossRef]
- Tortorici, M.A.; Beltramello, M.; Lempp, F.A.; Pinto, D.; Dang, H.V.; Rosen, L.E.; McCallum, M.; Bowen, J.; Minola, A.; Jaconi, S.; et al. Ultrapotent human antibodies protect against SARS-CoV-2 challenge via multiple mechanisms. Science 2020, 370, 950–957. [Google Scholar] [CrossRef] [PubMed]
- Kreye, J.; Reincke, S.M.; Kornau, H.C.; Sánchez-Sendin, E.; Corman, V.M.; Liu, H.; Yuan, M.; Wu, N.C.; Zhu, X.; Lee, C.D.; et al. A Therapeutic Non-self-reactive SARS-CoV-2 Antibody Protects from Lung Pathology in a COVID-19 Hamster Model. Cell 2020, 183, 1058–1069.e19. [Google Scholar] [CrossRef]
- Zhang, C.; Cui, H.; Li, E.; Guo, Z.; Wang, T.; Yan, F.; Liu, L.; Li, Y.; Chen, D.; Meng, K.; et al. The SARS-CoV-2 B.1.351 Variant Can Transmit in Rats But Not in Mice. Front. Immunol. 2022, 13, 869809. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Zhang, C.; Zhang, C.; Cui, H.; Chen, Z.; Jiang, X.; Wang, T.; Li, Y.; Liu, J.; Wan, Z.; et al. SARS-CoV-2-related pangolin coronavirus exhibits similar infection characteristics to SARS-CoV-2 and direct contact transmissibility in hamsters. iScience 2022, 25, 104350. [Google Scholar] [CrossRef]
- Jin, Y.; Cui, H.; Jiang, L.; Zhang, C.; Li, J.; Cheng, H.; Chen, Z.; Zheng, J.; Zhang, Y.; Fu, Y.; et al. Evidence for human infection with avian influenza A(H9N2) virus via environmental transmission inside live poultry market in Xiamen, China. J. Med. Virol. 2023, 95, e28242. [Google Scholar] [CrossRef]
- Guo, W.; Fu, Y.; Jia, R.; Guo, Z.; Su, C.; Li, J.; Zhao, X.; Jin, Y.; Li, P.; Fan, J.; et al. Visualization of the infection risk assessment of SARS-CoV-2 through aerosol and surface transmission in a negative-pressure ward. Environ. Int. 2022, 162, 107153. [Google Scholar] [CrossRef]
- Murphy, E.J.; Masterson, C.; Rezoagli, E.; O’Toole, D.; Major, I.; Stack, G.D.; Lynch, M.; Laffey, J.G.; Rowan, N.J. β-Glucan extracts from the same edible shiitake mushroom Lentinus edodes produce differential in-vitro immunomodulatory and pulmonary cytoprotective effects—Implications for coronavirus disease (COVID-19) immunotherapies. Sci. Total Environ. 2020, 732, 139330. [Google Scholar] [CrossRef]
- Zhou, S.; Sun, H. Prognostic model for gastric cancer patients with COVID-19 and network pharmacology study on treatment by lentinan. Sci. Rep. 2024, 14, 24645. [Google Scholar] [CrossRef] [PubMed]
- Brogna, C.; Brogna, B.; Bisaccia, D.R.; Lauritano, F.; Marino, G.; Montano, L.; Cristoni, S.; Prisco, M.; Piscopo, M. Could SARS-CoV-2 Have Bacteriophage Behavior or Induce the Activity of Other Bacteriophages? Vaccines 2022, 10, 708. [Google Scholar] [CrossRef]
- Ji, X.; Su, L.; Zhang, P.; Yue, Q.; Zhao, C.; Sun, X.; Li, K.; Liu, X.; Zhang, S.; Zhao, L. Lentinan improves intestinal inflammation and gut dysbiosis in antibiotics-induced mice. Sci. Rep. 2022, 12, 19609. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, L.; Khan, A.I.; Rehman, A.U.; Khinsar, K.H.; Xin, Y. Lentinan’s effect on gut microbiota and inflammatory cytokines in 5-FU-induced mucositis mice. AMB Express 2025, 15, 11. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, C.; Li, J.; Cui, H.; Jin, Y.; Chen, Z.; Zhang, L.; Song, S.; Lu, B.; Wang, Z.; Guo, Z. Lentinan Reduces Transmission Efficiency of COVID-19 by Changing Aerodynamic Characteristic of Exhaled SARS-CoV-2 Aerosols in Golden Hamsters. Microorganisms 2025, 13, 597. https://doi.org/10.3390/microorganisms13030597
Zhang C, Li J, Cui H, Jin Y, Chen Z, Zhang L, Song S, Lu B, Wang Z, Guo Z. Lentinan Reduces Transmission Efficiency of COVID-19 by Changing Aerodynamic Characteristic of Exhaled SARS-CoV-2 Aerosols in Golden Hamsters. Microorganisms. 2025; 13(3):597. https://doi.org/10.3390/microorganisms13030597
Chicago/Turabian StyleZhang, Cheng, Jiaming Li, Huan Cui, Yifei Jin, Zhaoliang Chen, Lei Zhang, Sihui Song, Bing Lu, Zhongyi Wang, and Zhendong Guo. 2025. "Lentinan Reduces Transmission Efficiency of COVID-19 by Changing Aerodynamic Characteristic of Exhaled SARS-CoV-2 Aerosols in Golden Hamsters" Microorganisms 13, no. 3: 597. https://doi.org/10.3390/microorganisms13030597
APA StyleZhang, C., Li, J., Cui, H., Jin, Y., Chen, Z., Zhang, L., Song, S., Lu, B., Wang, Z., & Guo, Z. (2025). Lentinan Reduces Transmission Efficiency of COVID-19 by Changing Aerodynamic Characteristic of Exhaled SARS-CoV-2 Aerosols in Golden Hamsters. Microorganisms, 13(3), 597. https://doi.org/10.3390/microorganisms13030597





