Longitudinal Outcomes Following Mitral Valve Repair for Infective Endocarditis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Statistical Analysis
3. Results
3.1. Preoperative Demographics
3.2. Causative Microorganisms
3.3. Surgical Indication and Technique
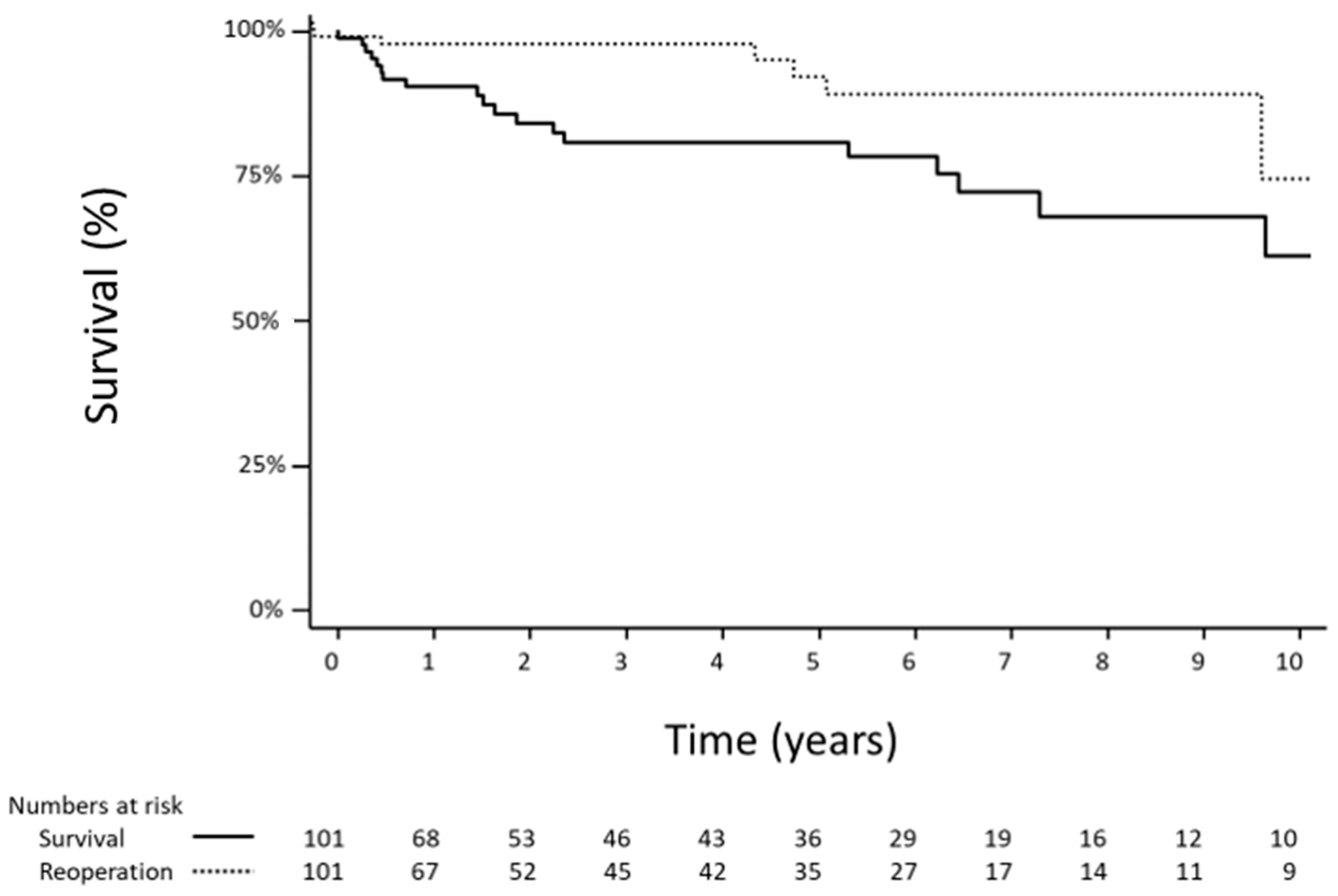
3.4. Short- and Long-Term Survival
3.5. Reoperation
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Hadji-Turdeghal, K.; Jensen, A.D.; Bruun, N.E.; Iversen, K.K.; Bundgaard, H.; Smerup, M.; Kober, L.; Østergaard, L.; Fosbøl, E.L. Temporal trends in the incidence of infective endocarditis in patients with a prosthetic heart valve. Open Heart 2023, 10, e002269. [Google Scholar] [CrossRef]
- Gatti, G.; Sponga, S.; Peghin, M.; Givone, F.; Ferrara, V.; Benussi, B.; Mazzaro, E.; Perrotti, A.; Bassetti, M.; Luzzati, R.; et al. Risk scores and surgery for infective endocarditis: In search of a good predictive score. Scand. Cardiovasc. J. 2019, 53, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Sellés, M.; Muñoz, P. Epidemiology, Diagnosis, Treatment, and Prognosis of Infective Endocarditis. J. Clin. Med. 2023, 12, 5705. [Google Scholar] [CrossRef]
- Palis, H.; Barocas, J.A.; Moe, J.; Scow, M.; Sedgemore, K.; Slaunwhite, A.K.; Buxton, J.A. Rising rates of infective endocarditis in North America: An urgent need for attentio to the rapidly changing unregulated drug supply. Int. J. Drug Policy 2023, 118, 104110. [Google Scholar] [CrossRef] [PubMed]
- Jamil, M.; Sultan, I.; Gleason, T.G.; Navid, F.; Fallert, M.A.; Suffoletto, M.S.; Kilic, A. Infective endocarditis: Trends, surgical outcomes, and controversies. J. Thorac. Dis. 2019, 11, 4875–4885. [Google Scholar] [CrossRef]
- Defauw, R.J.; Tomšič, A.; van Brakel, T.J.; Marsan, N.A.; Klautz, R.J.M.; Palmen, M. A structured approach to native mitral valve infective endocarditis: Is repair better than replacement? Eur. J. Cardiothorac. Surg. 2020, 58, 544–550. [Google Scholar] [CrossRef] [PubMed]
- Di Bacco, L.; D’Alonzo, M.; Di Mauro, M.; Petruccelli, R.D.; Baudo, M.; Palacios, C.M.; Benussi, S.; Muneretto, C.; Rosati, F. Mitral valve surgery in acute infective endocarditis: Long-term outcomes of mitral valve repair versus replacement. J. Cardiovasc. Med. 2024, 25, 30. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.K.; Wilson, K.; Elnagar, M.A.; Elbadawy, M.A.; Fathy, M.H. To repair or to replace in mitral valve infective endocarditis? an updated meta-analysis. J. Cardiothorac. Surg. 2024, 19, 247. [Google Scholar] [CrossRef]
- Scheggi, V.; Olivotto, I.; Del Pace, S.; Zoppetti, N.; Brunetto, A.; Marchionni, N.; Cerillo, A.; Stefàno, P.L. Feasibility and outcome of mitral valve repair in patients with infective endocarditis. Cardiothorac. Surg. 2020, 28, 27. [Google Scholar] [CrossRef]
- El Gabry, M.; Haidari, Z.; Mourad, F.; Nowak, J.; Tsagakis, K.; Thielmann, M.; Wendt, D.; Jakob, H.; Shehada, S.-E. Outcomes of mitral valve repair in acute native mitral valve infective endocarditis. Interact. Cardiovasc. Thorac. Surg. 2019, 29, 823–829. [Google Scholar] [CrossRef]
- Pettersson, G.B.; Hussain, S.T.; Shrestha, N.K.; Gordon, S.; Fraser, T.G.; Ibrahim, K.S.; Blackstone, E.H. Infective endocarditis: An atlas of disease progression for describing, staging, coding, and understanding the pathology. J. Thorac. Cardiovasc. Surg. 2014, 147, 1142–1149.e2. [Google Scholar] [CrossRef] [PubMed]
- Delgado, V.; Ajmone Marsan, N.; de Waha, S.; Bonaros, N.; Brida, M.; Burri, H.; Caselli, S.; Doenst, T.; Ederhy, S.; Erba, P.A.; et al. 2023 ESC Guidelines for the management of endocarditis: Developed by the task force on the management of endocarditis of the European Society of Cardiology (ESC) Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS) and the European Association of Nuclear Medicine (EANM). Eur. Heart J. 2023, 44, 3948–4042. [Google Scholar] [CrossRef] [PubMed]
- de Kerchove, L.; Vanoverschelde, J.-L.; Poncelet, A.; Glineur, D.; Rubay, J.; Zech, F.; Noirhomme, P.; El Khoury, G. Reconstructive surgery in active mitral valve endocarditis: Feasibility, safety and durability. Eur. J. Cardiothorac. Surg. 2007, 31, 592–599. [Google Scholar] [CrossRef]
- Toyoda, N.; Itagaki, S.; Egorova, N.N.; Tannous, H.; Anyanwu, A.C.; El-Eshmawi, A.; Adams, D.H.; Chikwe, J. Real-world outcomes of surgery for native mitral valve endocarditis. J. Thorac. Cardiovasc. Surg. 2017, 154, 1906–1912.e9. [Google Scholar] [CrossRef] [PubMed]
- Arjomandi Rad, A.; Zubarevich, A.; Osswald, A.; Vardanyan, R.; Magouliotis, D.E.; Ansaripour, A.; Kourliouros, A.; Sá, M.P.; Rassaf, T.; Ruhparwar, A.; et al. The Surgical Treatment of Infective Endocarditis: A Comprehensive Review. Diagnostics 2024, 14, 464. [Google Scholar] [CrossRef]
- Chan, V.; Ruel, M.; Chaudry, S.; Lambert, S.; Mesana, T.G. Clinical and echocardiographic outcomes after repair of mitral valve bileaflet prolapse due to myxomatous disease. J. Thorac. Cardiovasc. Surg. 2012, 143, S8–S11. [Google Scholar] [CrossRef]
- Fowler, V.G.; Durack, D.T.; Selton-Suty, C.; Athan, E.; Bayer, A.S.; Chamis, A.L.; Dahl, A.; DiBernardo, L.; Durante-Mangoni, E.; Duval, X.; et al. The 2023 Duke-International Society for Cardiovascular Infectious Diseases Criteria for Infective Endocarditis: Updating the Modified Duke Criteria. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2023, 77, 518–526. [Google Scholar] [CrossRef]
- Okada, Y.; Nakai, T.; Muro, T.; Ito, H.; Shomura, Y. Mitral valve repair for infective endocarditis: Kobe experience. Asian Cardiovasc. Thorac. Ann. 2020, 28, 384–389. [Google Scholar] [CrossRef]
- Iung, B.; Rousseau-Paziaud, J.; Cormier, B.; Garbarz, E.; Fondard, O.; Brochet, E.; Acar, C.; Couëtil, J.P.; Hvass, U.; Vahanian, A. Contemporary results of mitral valve repair for infective endocarditis. J. Am. Coll. Cardiol. 2004, 43, 386–392. [Google Scholar] [CrossRef]
- Kanemitsu, H.; Nakamura, K.; Fukunaga, N.; Koyama, T. Long-Term Outcomes of Mitral Valve Repair for Active Endocarditis. Circ. J. Off. J. Jpn. Circ. Soc. 2016, 80, 1148–1152. [Google Scholar] [CrossRef]
- Rostagno, C.; Carone, E.; Stefàno, P.L. Role of mitral valve repair in active infective endocarditis: Long term results. J. Cardiothorac. Surg. 2017, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Zegdi, R.; Debièche, M.; Latrémouille, C.; Lebied, D.; Chardigny, C.; Grinda, J.-M.; Chauvaud, S.; Deloche, A.; Carpentier, A.; Fabiani, J.-N. Long-Term Results of Mitral Valve Repair in Active Endocarditis. Circulation 2005, 111, 2532–2536. [Google Scholar] [CrossRef]
- Ruttmann, E.; Legit, C.; Poelzl, G.; Mueller, S.; Chevtchik, O.; Cottogni, M.; Ulmer, H.; Pachinger, O.; Laufer, G.; Mueller, L.C. Mitral valve repair provides improved outcome over replacement in active infective endocarditis. J. Thorac. Cardiovasc. Surg. 2005, 130, 765–771. [Google Scholar] [CrossRef]
- Harky, A.; Hof, A.; Garner, M.; Froghi, S.; Bashir, M. Mitral valve repair or replacement in native valve endocarditis? Systematic review and meta-analysis. J. Card. Surg. 2018, 33, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Fathy, M.H.; Elnagar, M.A.; Elbadawi, M.A.; Awad, A.K. Infective endocarditis of mitral valve, valve replacement or repair?- a meta-analysis of 10,965 patients. Eur. Heart J. 2022, 43, ehac544.2122. [Google Scholar] [CrossRef]
- Cuerpo, G.P.; Valerio, M.; Pedraz, A.; Rodríguez-Abella, H.; Mestres, C.A.; Obrador, E.Q.; González-Calle, A.; Rodríguez Álvarez, R.; García, P.M.; Bouza, E.; et al. Mitral valve repair in infective endocarditis is not inferior to valve replacement: Results from a Spanish nationwide prospective registry. Gen. Thorac. Cardiovasc. Surg. 2019, 67, 585–593. [Google Scholar] [CrossRef]
- Hussain, S.T.; Blackstone, E.H.; Pettersson, G.B. Tell it like it is: Experience in mitral valve surgery does matter for improved outcomes in mitral valve infective endocarditis. J. Thorac. Cardiovasc. Surg. 2017, 154, 1904–1905.e1. [Google Scholar] [CrossRef]
- Wiens, E.J.; Kawa, K.; Kass, M.; Shah, A.H. Impact of biological sex on valvular heart disease, interventions, and outcomes. Can. J. Physiol. Pharmacol. 2024. [Google Scholar] [CrossRef]
- DesJardin, J.T.; Chikwe, J.; Hahn, R.T.; Hung, J.W.; Delling, F.N. Sex Differences and Similarities in Valvular Heart Disease. Circ. Res. 2022, 130, 455–473. [Google Scholar] [CrossRef]
- Fukui, M.; Cavalcante, J.L.; Ahmed, A.; Bae, R.; Bapat, V.N.; Gössl, M.; Garcia, S.; Enriquez-Sarano, M.; Sorajja, P. Clinical Outcomes of Mitral Valve Disease with Mitral Annular Calcification. Am. J. Cardiol. 2022, 174, 107–113. [Google Scholar] [CrossRef]
- Avierinos, J.-F.; Inamo, J.; Grigioni, F.; Gersh, B.; Shub, C.; Enriquez-Sarano, M. Sex Differences in the Morphology and Outcomes of Mitral Valve Prolapse: A Cohort study. Ann. Intern. Med. 2008, 149, 787–795. [Google Scholar] [CrossRef]
- Tersalvi, G.; Gaiero, L.; Capriolo, M.; Cristoforetti, Y.; Salizzoni, S.; Senatore, G.; Pedrazzini, G.; Biasco, L. Sex Differences in Epidemiology, Morphology, Mechanisms, and Treatment of Mitral Valve Regurgitation. Medicina 2023, 59, 1017. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, F.; Clavel, M.-A.; Michelena, H.I.; Suri, R.M.; Schaff, H.V.; Enriquez-Sarano, M. Comprehensive Imaging in Women With Organic Mitral Regurgitation: Implications for Clinical Outcome. JACC Cardiovasc. Imaging 2016, 9, 388–396. [Google Scholar] [CrossRef]
- Slouha, E.; Al-Geizi, H.; Albalat, B.R.; Burle, V.S.; Clunes, L.A.; Kollias, T.F. Sex Differences in Infective Endocarditis: A Systematic Review. Cureus 2023, 15, e49815. [Google Scholar] [CrossRef] [PubMed]
- Polishchuk, I.; Stavi, V.; Awesat, J.; Ben Baruch Golan, Y.; Bartal, C.; Sagy, I.; Jotkowitz, A.; Barski, L. Sex Differences in Infective Endocarditis. Am. J. Med. Sci. 2021, 361, 83–89. [Google Scholar] [CrossRef]
- Curlier, E.; Hoen, B.; Alla, F.; Selton-Suty, C.; Schubel, L.; Doco-Lecompte, T.; Minary, L.; Erpelding, M.-L.; Duval, X.; Chirouze, C.; et al. Relationships between sex, early valve surgery and mortality in patients with left-sided infective endocarditis analysed in a population-based cohort study. Heart Br. Card. Soc. 2014, 100, 1173–1178. [Google Scholar] [CrossRef] [PubMed]
- Leterrier, J.; Iung, B.; de Tymoski, C.; Deconinck, L.; Para, M.; Duval, X.; Provenchere, S.; Mesnier, J.; Delhomme, C.; Haviari, S.; et al. Sex differences and outcomes in surgical infective endocarditis. Eur. J. Cardiothorac. Surg. 2024, 65, ezae114. [Google Scholar] [CrossRef]
- Afshar, Z.M.; Sabzi, F.; Shirvani, M.; Salehi, N.; Nemati, N.; Kheradmand, W.; Torbati, H.; Rouzbahani, M. Sex-Based Differences in One-Year Outcomes after Mitral Valve Repair for Infective Endocarditis. Braz. J. Cardiovasc. Surg. 2023, 38, e20210333. [Google Scholar] [CrossRef]
- Bansal, A.; Cremer, P.C.; Jaber, W.A.; Rampersad, P.; Menon, V. Sex Differences in the Utilization and Outcomes of Cardiac Valve Replacement Surgery for Infective Endocarditis: Insights from the National Inpatient Sample. J. Am. Heart Assoc. 2021, 10, e020095. [Google Scholar] [CrossRef]
| Variables | Total (N = 101) |
|---|---|
| Age (years) | 55.3 ± 14.2 |
| Sex (% female) | 33 (33%) |
| Atrial fibrillation | 13 (13%) |
| NYHA III/IV | 13 (13%) |
| STS risk of mortality (%) | 1.6 ± 2.1 |
| LVEF (%) | 61.5 ± 10.6 |
| Mitral perforation | 8 (7.9%) |
| Mitral regurgitation grade III/IV | 83 (82%) |
| Concomitant coronary artery disease requiring CABG | 9 (8.9%) |
| Microorganism | Total (N = 101) |
|---|---|
| Streptococcus viridans | 21 (21%) |
| Methicillin-susceptible Staphylococcus aureus (MSSA) | 2 (2.0%) |
| Staphylococcus aureus (susceptibility unspecified) | 5 (5.0%) |
| Streptococcus gallolyticus | 1 (1.0%) |
| Streptococcus (species unspecified) | 2 (2.0%) |
| Enterococcus (species unspecified) | 2 (2.0%) |
| Enterococcus durans | 1 (1.0%) |
| MSSA + Enterococcus faecalis | 1 (1.0%) |
| Haemophilus parainfluenzae | 1 (1.0%) |
| Cardiobacterium hominis | 1 (1.0%) |
| Escherichia coli | 1 (1.0%) |
| Histoplasma capsulatum | 1 (1.0%) |
| Corynebacterium | 1 (1.0%) |
| Coagulase-negative Staphylococci | 2 (2.0%) |
| Negative blood cultures | 22 (22%) |
| Not reported | 37 (37%) |
| Surgical Indication | Total (N = 101) |
|---|---|
| Heart failure with mitral regurgitation | 89 (88%) |
| Persistent infection | 2 (2.0%) |
| Locally uncontrolled | 6 (5.9%) |
| Septic emboli | 4 (4.0%) |
| Surgical Technique | N |
|---|---|
| Neochords | 25 |
| Posterior leaflet resection | 25 |
| Anterior leaflet resection | 13 |
| Chordal transfer | 21 |
| Annuloplasty | |
| Futureband | 95 |
| Duran | 1 |
| Physio | 4 |
| Cosgrove | 1 |
| Annuloplasty size (mm) | 30 ± 3 |
| Median: 30 (IQR 28–32) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qiu, Y.; Lau, L.; Khan, Z.; Messika-Zeitoun, D.; Ruel, M.; Chan, V. Longitudinal Outcomes Following Mitral Valve Repair for Infective Endocarditis. Microorganisms 2024, 12, 1809. https://doi.org/10.3390/microorganisms12091809
Qiu Y, Lau L, Khan Z, Messika-Zeitoun D, Ruel M, Chan V. Longitudinal Outcomes Following Mitral Valve Repair for Infective Endocarditis. Microorganisms. 2024; 12(9):1809. https://doi.org/10.3390/microorganisms12091809
Chicago/Turabian StyleQiu, Yuan, Lawrence Lau, Zaim Khan, David Messika-Zeitoun, Marc Ruel, and Vincent Chan. 2024. "Longitudinal Outcomes Following Mitral Valve Repair for Infective Endocarditis" Microorganisms 12, no. 9: 1809. https://doi.org/10.3390/microorganisms12091809
APA StyleQiu, Y., Lau, L., Khan, Z., Messika-Zeitoun, D., Ruel, M., & Chan, V. (2024). Longitudinal Outcomes Following Mitral Valve Repair for Infective Endocarditis. Microorganisms, 12(9), 1809. https://doi.org/10.3390/microorganisms12091809






