Epidemiological and Molecular Investigation of the Heater–Cooler Unit (HCU)-Related Outbreak of Invasive Mycobacterium chimaera Infection Occurred in Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Epidemiological Investigation
- Suspected case: a patient who met clinical and exposure criteria, for whom no microbiological confirmation was available;
- Probable case: a patient who met the clinical and exposure criteria and had MC identified by direct PCR and Sanger sequencing in a significant biological sample, or a MAC strain isolated by culture or by direct PCR from a significant biological sample, or histopathological detection of nongaseous granuloma and foamy/swollen macrophages with the presence of alcohol-acid-fast bacilli in cardiac or vascular tissue or in a sternotomy wound specimen;
- Confirmed case: a patient who met the clinical and exposure criteria and had MC isolated by culture and identified by Sanger sequencing in a significant biological sample [49].
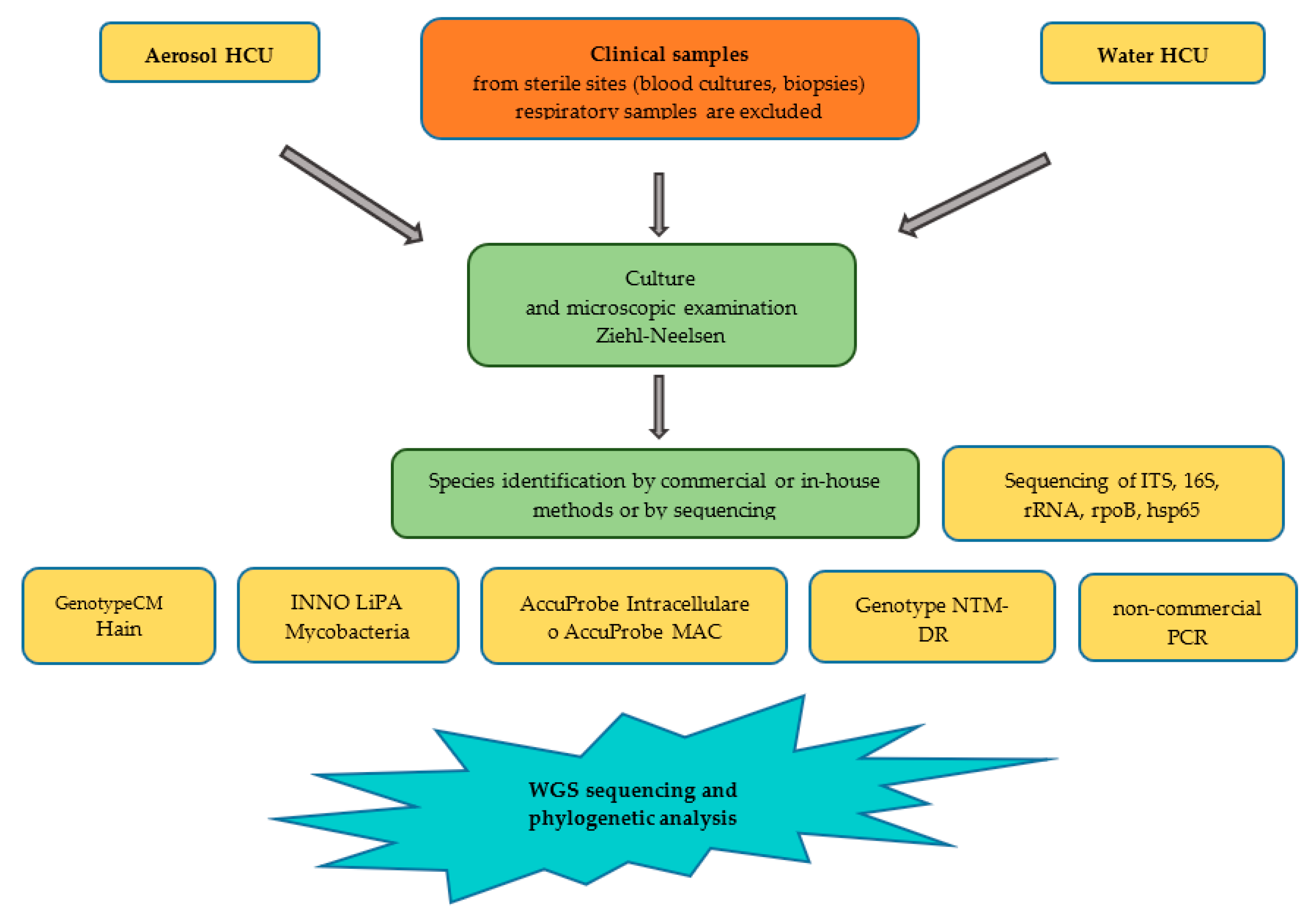
2.2. Molecular Analysis of Strains
3. Results
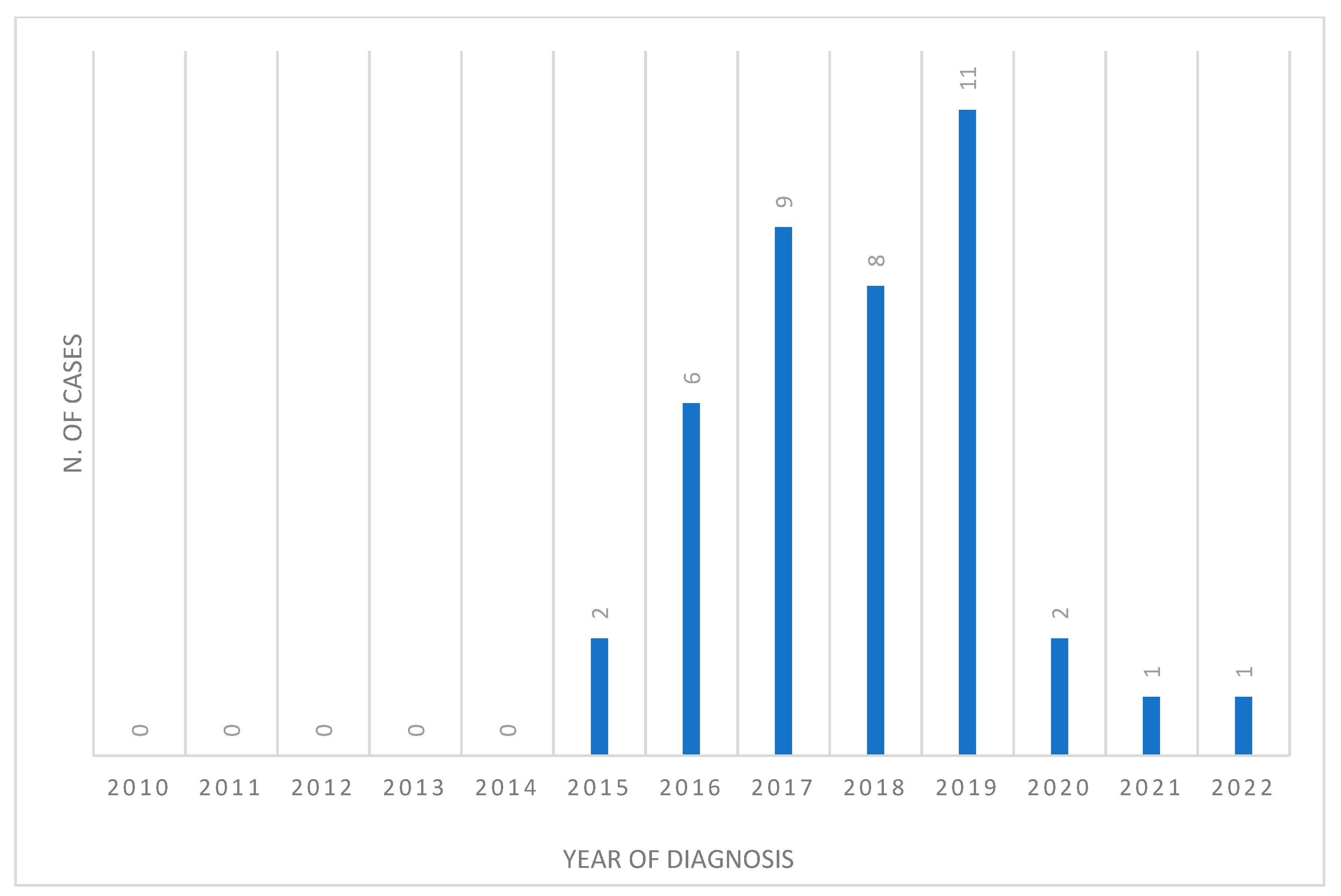
3.1. Demographic and Statistical Analysis
3.2. Laboratory Investigations
3.3. Contaminated HCU Analysis
4. Discussion
4.1. Public Health Response to Outbreak of MC Invasive Infection during Open Chest Surgery Occurred in Italy
- Identification of the subjects exposed by setting up a register of patients who had undergone HCU-assisted open chest surgery (including cardiac and/or pulmonary transplantation and aortic vascular transplantation) at the hospital level;
- Implementation of a local register of the HCUs used (where lacking), at the hospital level, in order to allow fast retrospective identification of patients at risk;
- Setting up regional/interregional reference centres for advice to medical staff and exposed subjects and follow-up of cases;
- Identification, where possible, of the general practitioners who cared for subjects potentially at risk to send them information for patients’ follow up (in addition to ministerial circular letters and any regional documents);
- Withdrawal of devices associated with one or more cases until microbiological proof of noncontamination.
4.2. Operating Procedures to Contain the Spread of Infections
5. Limitations of this Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tortoli, E.; Rindi, L.; Garcia, M.J.; Chiaradonna, P.; Dei, R.; Garzelli, C.; Kroppenstedt, R.M.; Lari, N.; Mattei, R.; Mariottini, A.; et al. Proposal to elevate the genetic variant MAC-A, included in the Mycobacterium avium complex, to species rank as Mycobacterium chimaera sp. nov. Int. J. Syst. Evol. Microbiol. 2004, 54, 1277–1285. [Google Scholar] [CrossRef] [PubMed]
- Bills, N.D.; Hinrichs, S.H.; Aden, T.A.; Wickert, R.S.; Iwen, P.C. Molecular identification of Mycobacterium chimaera as a cause of infection in a patient with chronic obstructive pulmonary disease. Diagn. Microbiol. Infect. Dis. 2009, 63, 292–295. [Google Scholar] [CrossRef] [PubMed]
- Kasperbauer, S.H.; Daley, C.L. Mycobacterium chimaera Infections Related to the Heater-Cooler Unit Outbreak: A Guide to Diagnosis and Management. Clin. Infect. Dis. 2019, 68, 1244–1250. [Google Scholar] [CrossRef]
- van Ingen, J.; Kohl, T.A.; Kranzer, K.; Hasse, B.; Keller, P.M.; Katarzyna Szafranska, A.; Hillemann, D.; Chand, M.; Schreiber, P.W.; Sommerstein, R.; et al. Global outbreak of severe Mycobacterium chimaera disease after cardiac surgery: A molecular epidemiological study. Lancet. Infect. Dis. 2017, 17, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Struelens, M.J.; Plachouras, D. Mycobacterium chimaera infections associated with heater-cooler units (HCU): Closing another loophole in patient safety. Euro Surveill. 2016, 21, 30397. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Achermann, Y.; Rossle, M.; Hoffmann, M.; Deggim, V.; Kuster, S.; Zimmermann, D.R.; Bloemberg, G.; Hombach, M.; Hasse, B. Prosthetic valve endocarditis and bloodstream infection due to Mycobacterium Chimaera. J. Clin. Microbiol. 2013, 51, 1769–1773. [Google Scholar] [CrossRef]
- Tan, N.; Sampath, R.; Abu Saleh, O.M.; Tweet, M.S.; Jevremovic, D.; Alniemi, S.; Wengenack, N.L.; Sampathkumar, P.; Badley, A.D. Disseminated Mycobacterium chimaera Infection after Cardiothoracic Surgery. Open Forum Infect. Dis. 2016, 3, ofw131. [Google Scholar] [CrossRef]
- Scriven, J.E.; Scobie, A.; Verlander, N.Q.; Houston, A.; Collyns, T.; Cajic, V.; Kon, O.M.; Mitchell, T.; Rahama, O.; Robinson, A.; et al. Mycobacterium chimaera infection following cardiac surgery in the United Kingdom: Clinical features and outcome of the first 30 cases. Clin. Microbiol. Infect. 2018, 24, 1164–1170. [Google Scholar] [CrossRef]
- Kohler, P.; Kuster, S.P.; Bloemberg, G.; Schulthess, B.; Frank, M.; Tanner, F.C.; Rossle, M.; Boni, C.; Falk, V.; Wilhelm, M.J.; et al. Healthcare-associated prosthetic heart valve, aortic vascular graft, and disseminated Mycobacterium chimaera infections subsequent to open heart surgery. Eur. Heart J. 2015, 36, 2745–2753. [Google Scholar] [CrossRef]
- Zweifel, S.A.; Mihic-Probst, D.; Curcio, C.A.; Barthelmes, D.; Thielken, A.; Keller, P.M.; Hasse, B.; Boni, C. Clinical and Histopathologic Ocular Findings in Disseminated Mycobacterium chimaera Infection after Cardiothoracic Surgery. Ophthalmology 2017, 124, 178–188. [Google Scholar] [CrossRef]
- Gasch, O.; Meije, Y.; Espasa, M.; Font, B.; Jimenez, S.; Fernandez-Hidalgo, N. Disseminated Infection Due to Mycobacterium chimaera After Aortic Valve Replacement. Rev. Esp. Cardiol. 2019, 72, 502–503. [Google Scholar] [CrossRef] [PubMed]
- Lau, D.; Cooper, R.; Chen, J.; Sim, V.L.; McCombe, J.A.; Tyrrell, G.J.; Bhargava, R.; Adam, B.; Chapman, E.; Croxen, M.A.; et al. Mycobacterium chimaera Encephalitis Following Cardiac Surgery: A New Syndrome. Clin. Infect. Dis. 2020, 70, 692–695. [Google Scholar] [CrossRef] [PubMed]
- Cantillon, D.; Goff, A.; Taylor, S.; Salehi, E.; Fidler, K.; Stoneham, S.; Waddell, S.J. Searching for new therapeutic options for the uncommon pathogen Mycobacterium chimaera: An open drug discovery approach. Lancet. Microbe 2022, 3, e382–e391. [Google Scholar] [CrossRef]
- Mason, M.; Gregory, E.; Foster, K.; Klatt, M.; Zoubek, S.; Eid, A.J. Pharmacologic Management of Mycobacterium chimaera Infections: A Primer for Clinicians. Open Forum Infect. Dis. 2022, 9, ofac287. [Google Scholar] [CrossRef] [PubMed]
- Asadi, T.; Mullin, K.; Roselli, E.; Johnston, D.; Tan, C.D.; Rodriguez, E.R.; Gordon, S. Disseminated Mycobacterium chimaera infection associated with heater-cooler units after aortic valve surgery without endocarditis. J. Thorac. Cardiovasc. Surg. 2018, 155, 2369–2374. [Google Scholar] [CrossRef]
- Cappabianca, G.; Paparella, D.; D’Onofrio, A.; Caprili, L.; Minniti, G.; Lanzafame, M.; Parolari, A.; Musumeci, F.; Beghi, C. Mycobacterium chimaera infections following cardiac surgery in Italy: Results from a National Survey Endorsed by the Italian Society of Cardiac Surgery. J. Cardiovasc. Med. 2018, 19, 748–755. [Google Scholar] [CrossRef]
- O’Neil, C.R.; Taylor, G.; Smith, S.; Joffe, A.M.; Antonation, K.; Shafran, S.; Kunimoto, D. Mycobacterium chimaera Infection After Aortic Valve Replacement Presenting With Aortic Dissection and Pseudoaneurysm. Open Forum Infect. Dis. 2018, 5, ofy018. [Google Scholar] [CrossRef]
- Overton, K.; Mennon, V.; Mothobi, N.; Neild, B.; Martinez, E.; Masters, J.; Grant, P.; Akhunji, Z.; Su, W.Y.; Torda, A.; et al. Cluster of invasive Mycobacteria chimaera infections following cardiac surgery demonstrating novel clinical features and risks of aortic valve replacement. Intern. Med. J. 2018, 48, 1514–1520. [Google Scholar] [CrossRef]
- Shafizadeh, N.; Hale, G.; Bhatnagar, J.; Alshak, N.S.; Nomura, J. Mycobacterium chimaera Hepatitis: A New Disease Entity. Am. J. Surg. Pathol. 2019, 43, 244–250. [Google Scholar] [CrossRef]
- Lecorche, E.; Daniau, C.; La, K.; Mougari, F.; Benmansour, H.; Kumanski, S.; Robert, J.; Fournier, S.; Lebreton, G.; Carbonne, A.; et al. Mycobacterium chimaera Genomics With Regard to Epidemiological and Clinical Investigations Conducted for an Open Chest Postsurgical Mycobacterium chimaera Infection Outbreak. Open Forum Infect. Dis. 2021, 8, ofab192. [Google Scholar] [CrossRef]
- Nomura, J.; Rieg, G.; Bluestone, G.; Tsai, T.; Lai, A.; Terashita, D.; Bercovici, S.; Hong, D.K.; Lee, B.P. Rapid detection of invasive Mycobacterium chimaera disease via a novel plasma-based next-generation sequencing test. BMC Infect. Dis. 2019, 19, 371. [Google Scholar] [CrossRef]
- Epperson, L.E.; Timke, M.; Hasan, N.A.; Godo, P.; Durbin, D.; Helstrom, N.K.; Shi, G.; Kostrzewa, M.; Strong, M.; Salfinger, M. Evaluation of a Novel MALDI Biotyper Algorithm to Distinguish Mycobacterium intracellulare from Mycobacterium chimaera. Front. Microbiol. 2018, 9, 3140. [Google Scholar] [CrossRef]
- Ditommaso, S.; Giacomuzzi, M.; Memoli, G.; Garlasco, J.; Curtoni, A.; Iannaccone, M.; Zotti, C.M. A New Culture Method for the Detection of Non-Tuberculous Mycobacteria in Water Samples from Heater-Cooler Units and Extracorporeal Membrane Oxygenation Machines. Int. J. Environ. Res. Public Health 2022, 19, 10645. [Google Scholar] [CrossRef]
- Bagnarino, J.; Barbarini, D.; Russello, G.; Siciliano, M.; Monzillo, V.; Baldanti, F.; Carretto, E. Mycobacterium chimaera Identification Using MALDI-TOF MS Technology: A Practical Approach for the Clinical Microbiology Laboratories. Microorganisms 2022, 10, 1184. [Google Scholar] [CrossRef] [PubMed]
- Zoccola, R.; Di Blasio, A.; Bossotto, T.; Pontei, A.; Angelillo, M.; Dondo, A.; Goria, M.; Zoppi, S. Validation of a Novel Diagnostic Approach Combining the VersaTREK System for Recovery and Real-Time PCR for the Identification of Mycobacterium chimaera in Water Samples. Microorganisms 2021, 9, 1031. [Google Scholar] [CrossRef] [PubMed]
- Ditommaso, S.; Giacomuzzi, M.; Memoli, G.; Zotti, C.M. Failure to eradicate non-tuberculous mycobacteria upon disinfection of heater-cooler units: Results of a microbiological investigation in northwestern Italy. J. Hosp. Infect. 2020, 106, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Siddam, A.D.; Zaslow, S.J.; Wang, Y.; Phillips, K.S.; Silverman, M.D.; Regan, P.M.; Amarasinghe, J.J. Characterization of Biofilm Formation by Mycobacterium chimaera on Medical Device Materials. Front. Microbiol. 2020, 11, 586657. [Google Scholar] [CrossRef]
- Schlotthauer, U.; Hennemann, K.; Gartner, B.C.; Schafers, H.J.; Becker, S.L. Microbiological Surveillance of Heater-Cooler Units Used in Cardiothoracic Surgery for Detection of Mycobacterium chimaera. Thorac. Cardiovasc. Surg. 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Sommerstein, R.; Hasse, B.; Marschall, J.; Sax, H.; Genoni, M.; Schlegel, M.; Widmer, A.F. Global Health Estimate of Invasive Mycobacterium chimaera Infections Associated with Heater-Cooler Devices in Cardiac Surgery. Emerg. Infect. Dis. 2018, 24, 576–578. [Google Scholar] [CrossRef]
- Wetzstein, N.; Kohl, T.A.; Diricks, M.; Mas-Peiro, S.; Holubec, T.; Kessel, J.; Graf, C.; Koch, B.; Herrmann, E.; Vehreschild, M.; et al. Clinical characteristics and outcome of Mycobacterium chimaera infections after cardiac surgery: Systematic review and meta-analysis of 180 heater-cooler unit-associated cases. Clin. Microbiol. Infect. 2023, 29, 1008–1014. [Google Scholar] [CrossRef]
- Sax, H.; Bloemberg, G.; Hasse, B.; Sommerstein, R.; Kohler, P.; Achermann, Y.; Rossle, M.; Falk, V.; Kuster, S.P.; Bottger, E.C.; et al. Prolonged Outbreak of Mycobacterium chimaera Infection After Open-Chest Heart Surgery. Clin. Infect. Dis. 2015, 61, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.B.; Yuh, D.D.; Schwartz, S.B.; Lange, R.A.; Hopkins, R.; Bauer, K.; Marders, J.A.; Delgado Donayre, J.; Milligan, N.; Wentz, C. Nontuberculous Mycobacterium Infections Associated With Heater-Cooler Devices. Ann. Thorac. Surg. 2017, 104, 1237–1242. [Google Scholar] [CrossRef] [PubMed]
- Inojosa, W.O.; Giobbia, M.; Muffato, G.; Minniti, G.; Baldasso, F.; Carniato, A.; Farina, F.; Forner, G.; Rossi, M.C.; Formentini, S.; et al. Mycobacterium chimaera infections following cardiac surgery in Treviso Hospital, Italy, from 2016 to 2019: Cases report. World J. Clin. Cases 2019, 7, 2776–2786. [Google Scholar] [CrossRef] [PubMed]
- Quintas Viqueira, A.; Perez Romero, C.; Toro Rueda, C.; Sanchez Calles, A.M.; Blazquez Gonzalez, J.A.; Alejandre Leyva, M. Mycobacterium chimaera in heater-cooler devices: An experience in a tertiary hospital in Spain. New Microbes New Infect. 2021, 39, 100757. [Google Scholar] [CrossRef]
- Xu, K.; Finn, L.E.; Geist, R.L.; Prestel, C.; Moulton-Meissner, H.; Kim, M.; Stacey, B.; McAllister, G.A.; Gable, P.; Kamali, T.; et al. Mycobacterium chimaera infections among cardiothoracic surgery patients associated with heater-cooler devices-Kansas and California, 2019. Infect. Control Hosp. Epidemiol. 2022, 43, 1333–1338. [Google Scholar] [CrossRef]
- Natanti, A.; Palpacelli, M.; Valsecchi, M.; Tagliabracci, A.; Pesaresi, M. Mycobacterium chimaera: A report of 2 new cases and literature review. Int. J. Leg. Med. 2021, 135, 2667–2679. [Google Scholar] [CrossRef]
- Zabost, A.T.; Szturmowicz, M.; Brzezinska, S.A.; Klatt, M.D.; Augustynowicz-Kopec, E.M. Mycobacterium chimaera as an Underestimated Cause of NTM Lung Diseases in Patients Hospitalized in Pulmonary Wards. Pol. J. Microbiol. 2021, 70, 315–320. [Google Scholar] [CrossRef]
- Schreiber, P.W.; Kohl, T.A.; Kuster, S.P.; Niemann, S.; Sax, H. The global outbreak of Mycobacterium chimaera infections in cardiac surgery-a systematic review of whole-genome sequencing studies and joint analysis. Clin. Microbiol. Infect. 2021, 27, 1613–1620. [Google Scholar] [CrossRef]
- Chandrasekar, H.; Hoganson, D.M.; Lachenauer, C.S.; Newburger, J.W.; Sandora, T.J.; Saleeb, S.F. Mycobacterium chimaera Outbreak Management and Outcomes at a Large Pediatric Cardiac Surgery Center. Ann. Thorac. Surg. 2022, 114, 552–559. [Google Scholar] [CrossRef]
- Veenis, A.; Haghnegahdar, M.; Ajlan, R. Mycobacterium chimaera chorioretinitis preceding central nervous system lesions: A case report and review of the literature. BMC Ophthalmol. 2022, 22, 316. [Google Scholar] [CrossRef]
- Chand, M.; Lamagni, T.; Kranzer, K.; Hedge, J.; Moore, G.; Parks, S.; Collins, S.; Del Ojo Elias, C.; Ahmed, N.; Brown, T.; et al. Insidious Risk of Severe Mycobacterium chimaera Infection in Cardiac Surgery Patients. Clin. Infect. Dis. 2017, 64, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Perkins, K.M.; Lawsin, A.; Hasan, N.A.; Strong, M.; Halpin, A.L.; Rodger, R.R.; Moulton-Meissner, H.; Crist, M.B.; Schwartz, S.; Marders, J.; et al. Notes from the Field: Mycobacterium chimaera Contamination of Heater-Cooler Devices Used in Cardiac Surgery—United States. MMWR. Morb. Mortal. Wkly. Rep. 2016, 65, 1117–1118. [Google Scholar] [CrossRef] [PubMed]
- Diekema, D.J. Mycobacterium Chimaera Infections after Cardiovascular Surgery: Lessons from a Global Outbreak. Trans. Am. Clin. Climatol. Assoc. 2019, 130, 136–144. [Google Scholar]
- Lyman, M.M.; Grigg, C.; Kinsey, C.B.; Keckler, M.S.; Moulton-Meissner, H.; Cooper, E.; Soe, M.M.; Noble-Wang, J.; Longenberger, A.; Walker, S.R.; et al. Invasive Nontuberculous Mycobacterial Infections among Cardiothoracic Surgical Patients Exposed to Heater-Cooler Devices. Emerg. Infect. Dis. 2017, 23, 796–805. [Google Scholar] [CrossRef] [PubMed]
- Kuehl, R.; Banderet, F.; Egli, A.; Keller, P.M.; Frei, R.; Dobele, T.; Eckstein, F.; Widmer, A.F. Different Types of Heater-Cooler Units and Their Risk of Transmission of Mycobacterium chimaera during Open-Heart Surgery: Clues from Device Design. Infect. Control Hosp. Epidemiol. 2018, 39, 834–840. [Google Scholar] [CrossRef]
- Sommerstein, R.; Ruegg, C.; Kohler, P.; Bloemberg, G.; Kuster, S.P.; Sax, H. Transmission of Mycobacterium chimaera from Heater-Cooler Units during Cardiac Surgery despite an Ultraclean Air Ventilation System. Emerg. Infect. Dis. 2016, 22, 1008–1013. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.T.; Lamagni, T.; Chand, M. Evidence that Mycobacterium chimaera aerosols penetrate laminar airflow and result in infections at the surgical field. Lancet. Infect. Dis. 2017, 17, 1019. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bolcato, M.; Rodriguez, D.; Aprile, A. Risk Management in the New Frontier of Professional Liability for Nosocomial Infection: Review of the Literature on Mycobacterium chimaera. Int. J. Environ. Res. Public Health 2020, 17, 7328. [Google Scholar] [CrossRef] [PubMed]
- ECDC. Invasive Cardiovascular Infection by Mycobacterium chimaera Potentially Assocated with Heater-Cooler Units during Cardiac Surgery. 2015. Available online: https://www.ecdc.europa.eu/en/publications-data/invasive-cardiovascular-infection-mycobacterium-chimaera-potentially-associated (accessed on 23 June 2023).
- Ministero Della Salute. Infezione da Mycobacterium chimaera, Indicazioni Operative. 2019. Available online: https://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=null&id=3705 (accessed on 10 July 2023).
- Andrews, S. FastQC: A Quality Control Tool for High throughput Sequence Data. 2010. Available online: https://www.bioinformatics.babraham.ac.uk/projects/fastqc/ (accessed on 16 January 2023).
- Bisognin, F.; Messina, F.; Butera, O.; Nisii, C.; Mazzarelli, A.; Cristino, S.; Pascale, M.R.; Lombardi, G.; Cannas, A.; Dal Monte, P. Investigating the Origin of Mycobacterium chimaera Contamination in Heater-Cooler Units: Integrated Analysis with Fourier Transform Infrared Spectroscopy and Whole-Genome Sequencing. Microbiol. Spectr. 2022, 10, e0289322. [Google Scholar] [CrossRef]
- Garrison, E.; Marth, G. Haplotype-basedvariant detection from short-read sequencing. arXiv 2012, arXiv:1207.3907. [Google Scholar]
- Hasse, B.; Hannan, M.M.; Keller, P.M.; Maurer, F.P.; Sommerstein, R.; Mertz, D.; Wagner, D.; Fernandez-Hidalgo, N.; Nomura, J.; Manfrin, V.; et al. International Society of Cardiovascular Infectious Diseases Guidelines for the Diagnosis, Treatment and Prevention of Disseminated Mycobacterium chimaera Infection Following Cardiac Surgery with Cardiopulmonary Bypass. J. Hosp. Infect. 2020, 104, 214–235. [Google Scholar] [CrossRef]
- Chiesi, S.; Piacentini, D.; Salerno, N.D.; Luise, D.; Peracchi, M.; Concia, E.; Cazzadori, A.; Piovan, E.; Lanzafame, M. Disseminated Mycobacterium chimaera infection after open heart surgery in an Italian woman: A case report and a review of the literature. Infez. Med. 2017, 25, 267–269. [Google Scholar]
- Mokhles, M.M.; Soloukey Tbalvandany, S.; Siregar, S.; Versteegh, M.I.M.; Noyez, L.; van Putte, B.; Vonk, A.B.A.; Roos-Hesselink, J.W.; Bogers, A.; Takkenberg, J.J.M. Male-female differences in aortic valve and combined aortic valve/coronary surgery: A national cohort study in the Netherlands. Open Heart 2018, 5, e000868. [Google Scholar] [CrossRef] [PubMed]
- Cicchetti, A.; Gasbarrini, A. The healthcare service in Italy: Regional variability. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 1–3. [Google Scholar] [PubMed]
- Ministero Della Salute. Infezioni Causate da Mycobacterium Chimaera in Pazienti Sottoposti a Interventi Chirurgici a “Cuore Aperto” con Sistemi di Riscaldamento—Raffreddamento, Raccomandazioni per Operatori. 2019. Available online: https://www.salute.gov.it/portale/dispositiviMedici/dettaglioNotizieDispositiviMedici.jsp?lingua=italiano&menu=notizie&p=dalministero&id=3556 (accessed on 10 July 2023).
- Gotting, T.; Klassen, S.; Jonas, D.; Benk, C.; Serr, A.; Wagner, D.; Ebner, W. Heater-cooler units: Contamination of crucial devices in cardiothoracic surgery. J. Hosp. Infect. 2016, 93, 223–228. [Google Scholar] [CrossRef]
- Buchanan, R.; Agarwal, A.; Mathai, E.; Cherian, B.P. Mycobacterium chimaera: A novel pathogen with potential risk to cardiac surgical patients. Natl. Med. J. India 2020, 33, 284–287. [Google Scholar] [CrossRef] [PubMed]
- Puis, L.; Milojevic, M.; Boer, C.; De Somer, F.; Gudbjartsson, T.; van den Goor, J.; Jones, T.J.; Lomivorotov, V.; Merkle, F.; Ranucci, M.; et al. 2019 EACTS/EACTA/EBCP guidelines on cardiopulmonary bypass in adult cardiac surgery. Interact. Cardiovasc. Thorac. Surg. 2020, 30, 161–202. [Google Scholar] [CrossRef]
| Total Cases (n = 40) | Absolute Number (%) |
|---|---|
| Demographics and risk factors | |
| Male | 35 (87.5) |
| Geographical area: Northern Italy | 37 (92.5) |
| Geographical area: Central Italy | 0 |
| Geographical area: Southern Italy | 3 (7.5) |
| Geographical area: Islands | 0 |
| Main symptoms (n = 14) | |
| Fever | 8 (10.8) |
| Leukopenia/thrombocytopenia | 7 (9.5) |
| Endocarditis | 6 (8.1) |
| Hepatitis | 6 (8.1) |
| Asthenia | 5 (6.8) |
| Weight loss | 5 (6.8) |
| Night sweats | 5 (6.8) |
| Multiple granulomas | 4 (5.4) |
| Nephritis | 4 (5.4) |
| Lung involvement/pneumonia | 4 (5.4) |
| Splenomegaly | 4 (5.4) |
| Nausea | 3 (4.1) |
| Bacteraemia | 2 (2.7) |
| Death | 21 (52.5) |
| Mean; median age (range) | 64.9; 66 (35–82 years) |
| Mean; median time between surgery and diagnosis (range, n = 37) | 4.6; 4 (2–8 years) |
| Mean; median time between diagnosis and death (range, n = 16) | 2.1; 1.5 (0.5–9.5 years) |
| (A) | ||
|---|---|---|
| ID | SNPs [4] | Classification |
| 1 | 113518G>A; 209278G>A | 1.1 |
| 2 | 113518G>A; 209278G>A | 1.1 |
| 3 | 113518G>A; 209278G>A | 1.1 |
| 4 | 1611282G>C; 2366314G>A | 1.8 |
| 5 | 113518G>A; 209278G>A | 1.1 |
| 6 | 113518G>A; 209278G>A | 1.1 |
| 7 | 113518G>A; 209278G>A | 1.1 |
| 8 | 113518G>A; 209278G>A | 1.1 |
| 9 | 113518G>A; 209278G>A | 1.1 |
| 10 | 113518G>A; 209278G>A | 1.1 |
| 11 | 113518G>A; 209278G>A | 1.1 |
| 12 | 113518G>A; 209278G>A | 1.1 |
| 13 | 113518G>A; 209278G>A | 1.1 |
| 14 | 113518G>A; 209278G>A | 1.1 |
| 15 | 1611282G>C; 2366314G>A | 1.8 |
| 16 | 1611282G>C; 2366314G>A | 1.8 |
| 17 | 113518G>A; 209278G>A | 1.1 |
| 18 | 113518G>A; 209278G>A | 1.1 |
| 19 | 1611282G>C; 2366314G>A | 1.8 |
| 20 | 113518G>A; 209278G>A | 1.1 |
| 21 | 113518G>A; 209278G>A | 1.1 |
| 22 | 113518G>A; 209278G>A | 1.1 |
| 23 | 1611282G>C; 2366314G>A | 1.8 |
| 24 | 113518G>A; 209278G>A | 1.1 |
| 25 | 113518G>A; 209278G>A | 1.1 |
| 26 | 113518G>A; 209278G>A | 1.1 |
| 27 | 113518G>A; 209278G>A | 1.1 |
| 28 | 113518G>A; 209278G>A | 1.1 |
| 29 | 113518G>A; 209278G>A | 1.1 |
| 30 | 113518G>A; 209278G>A | 1.1 |
| 31 | 113518G>A; 209278G>A | 1.1 |
| 32 | 113518G>A; 209278G>A | 1.1 |
| 33 | 113518G>A; 209278G>A | 1.1 |
| 34 | 113518G>A; 209278G>A | 1.1 |
| 35 | 113518G>A; 209278G>A | 1.1 |
| 36 | 1611282G>C; 2366314G>A | 1.8 |
| (B) | ||
| ID | SNPs [4] | Classification |
| 1 | 4977262T>C | ungrouped |
| 2 | 4977262T>C | ungrouped |
| 3 | ungrouped | |
| 4 | ungrouped | |
| 5 | 5003561A>G | Branch 2 |
| 6 | 4977262T>C | Branch 1 |
| 7 | 4977262T>C | Branch 1 |
| 8 | ungrouped | |
| 9 | 5003561A>G | Branch 2 |
| 10 | ungrouped | |
| 11 | ungrouped | |
| 12 | 4977262T>C | Branch 1 |
| 13 | ungrouped | |
| 14 | 5003561A>G | Branch 2 |
| 15 | Roseomonas mucosa | |
| 16 | ungrouped | |
| 17 | 4977262T>C | Branch 1 |
| 18 | 4977262T>C | Branch 1 |
| 19 | 4977262T>C | Branch 1 |
| 20 | 4977262T>C | Branch 1 |
| 21 | ungrouped | |
| ID | SNPs [4] | Classification |
|---|---|---|
| 1 | 3022332T>C; 5709901T>C; 3406341C>T; 1828053C>T | 2 |
| 2 | 113518G>A; 209278G>A | 1.1 |
| 3 | 113518G>A; 209278G>A | 1.1 |
| 4 | ungrouped | |
| 5 | ungrouped | |
| 6 | ungrouped | |
| 7 | 113518G>A; 209278G>A | 1.1 |
| 8 | 113518G>A; 209278G>A | 1.1 |
| 9 | 5003561A>G; 2339764C>T | Branch 2 |
| 10 | 5003561A>G | Branch 2 |
| 11 | 5003561A>G; 2339764C>T | Branch 2 |
| 12 | 5003561A>G; 2339764C>T | Branch 2 |
| 13 | 113518G>A; 209278G>A | 1.1 |
| 14 | 113518G>A; 209278G>A | 1.1 |
| 15 | 113518G>A; 209278G>A | 1.1 |
| 16 | 113518G>A; 209278G>A | 1.1 |
| 17 | 113518G>A; 209278G>A | 1.1 |
| 18 | ungrouped | |
| 19 | 113518G>A; 209278G>A | 1.1 |
| 20 | 4977262T>C | Branch 2 |
| 21 | ungrouped | |
| 22 | ungrouped | |
| 23 | 113518G>A; 209278G>A | 1.1 |
| 24 | ungrouped | |
| 25 | 4977262T>C | Branch 2 |
| 26 | ungrouped | |
| 27 | 4977262T>C | Branch 1 |
| 28 | ungrouped | |
| 29 | 113518G>A; 209278G>A | 1.1 |
| 30 | ungrouped | |
| 31 | 4977262T>C | Branch 1 |
| 32 | 113518G>A; 209278G>A | 1.1 |
| 33 | Sphingomonas paucimobilis | |
| 34 | 113518G>A; 209278G>A | 1.1 |
| 35 | 4977262T>C | Branch 1 |
| 36 | 4977262T>C | Branch 1 |
| 37 | Oligotropha carboxidovorans | |
| 38 | 4977262T>C | Branch 1 |
| 39 | M. paragordonae | |
| 40 | 113518G>A; 209278G>A | 1.1 |
| 41 | Branch 2 | |
| 42 | ungrouped | |
| 43 | ungrouped | |
| 44 | 113518G>A; 209278G>A | 1.1 |
| 45 | ungrouped | |
| 46 | ungrouped | |
| 47 | ungrouped | |
| 48 | 113518G>A; 209278G>A | 1.1 |
| 49 | 3022332T>C; 3406341C>T; 1828053C>T | 2.1 |
| 50 | 5003561A>G | Branch 2 |
| 51 | 5003561A>G | Branch 2 |
| 52 | 5003561A>G | Branch 2 |
| 53 | 5003561A>G | Branch 2 |
| 54 | 5003561A>G | Branch 2 |
| 55 | 5003561A>G | Branch 2 |
| 56 | 5003561A>G | Branch 2 |
| 57 | 5003561A>G | Branch 2 |
| 58 | 113518G>A; 209278G>A | 1.1 |
| 59 | 113518G>A; 209278G>A | 1.1 |
| 60 | ungrouped | |
| 61 | ungrouped | |
| 62 | ungrouped | |
| 63 | 2339764C>T | Branch 2 |
| 64 | ungrouped | |
| 65 | ungrouped | |
| 66 | ungrouped | |
| 67 | ungrouped | |
| 68 | ungrouped | |
| 69 | ungrouped | |
| 70 | ungrouped | |
| 71 | 3406341C>T; 1828053C>T; 2329494C>T | 2.1 |
| 72 | 1611282G>C; 2366314G>A | 1.8 |
| 73 | 3022332T>C; 3406341C>T; 1828053C>T | 2.1 |
| 74 | 113518G>A; 209278G>A | 1.1 |
| 75 | 113518G>A; 209278G>A | 1.1 |
| 76 | 5003561A>G | Branch 2 |
| 77 | 5003561A>G | Branch 2 |
| 78 | 5003561A>G | Branch 2 |
| 79 | 113518G>A; 209278G>A | 1.1 |
| 80 | 2329494C>T; 5709901T>C | 2 |
| 81 | 113518G>A; 209278G>A | 1.1 |
| 82 | 113518G>A; 209278G>A | 1.1 |
| 83 | 113518G>A; 209278G>A | 1.1 |
| 84 | 113518G>A; 209278G>A | 1.1 |
| 85 | 2329494T>C; 3022332T>C; 3949608A>G; 5709901T>C | 2 |
| 86 | 4977262T>C | Branch 1 |
| 87 | 113518G>A; 209278G>A | 1.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannas, A.; Campanale, A.; Minella, D.; Messina, F.; Butera, O.; Nisii, C.; Mazzarelli, A.; Fontana, C.; Lispi, L.; Maraglino, F.; et al. Epidemiological and Molecular Investigation of the Heater–Cooler Unit (HCU)-Related Outbreak of Invasive Mycobacterium chimaera Infection Occurred in Italy. Microorganisms 2023, 11, 2251. https://doi.org/10.3390/microorganisms11092251
Cannas A, Campanale A, Minella D, Messina F, Butera O, Nisii C, Mazzarelli A, Fontana C, Lispi L, Maraglino F, et al. Epidemiological and Molecular Investigation of the Heater–Cooler Unit (HCU)-Related Outbreak of Invasive Mycobacterium chimaera Infection Occurred in Italy. Microorganisms. 2023; 11(9):2251. https://doi.org/10.3390/microorganisms11092251
Chicago/Turabian StyleCannas, Angela, Antonella Campanale, Daniela Minella, Francesco Messina, Ornella Butera, Carla Nisii, Antonio Mazzarelli, Carla Fontana, Lucia Lispi, Francesco Maraglino, and et al. 2023. "Epidemiological and Molecular Investigation of the Heater–Cooler Unit (HCU)-Related Outbreak of Invasive Mycobacterium chimaera Infection Occurred in Italy" Microorganisms 11, no. 9: 2251. https://doi.org/10.3390/microorganisms11092251
APA StyleCannas, A., Campanale, A., Minella, D., Messina, F., Butera, O., Nisii, C., Mazzarelli, A., Fontana, C., Lispi, L., Maraglino, F., Di Caro, A., & Sabbatucci, M. (2023). Epidemiological and Molecular Investigation of the Heater–Cooler Unit (HCU)-Related Outbreak of Invasive Mycobacterium chimaera Infection Occurred in Italy. Microorganisms, 11(9), 2251. https://doi.org/10.3390/microorganisms11092251







